Whipple procedure indications US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Whipple procedure indications. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Whipple procedure indications US Medical PG Question 1: A 62-year-old woman referred to the cardiology clinic for the evaluation of fatigue and dyspnea for 4 months. She also has loose stools (2–4 per day), palpitations, and non-pitting edema up to her mid-calf. On examination, vital signs are unremarkable, but she appears to be flushed with mild bilateral wheezes can be heard on chest auscultation. Cardiovascular examination reveals a grade 2/6 holosystolic murmur at the left mid-sternal area, which is louder during inspiration. Basic laboratory investigations are unremarkable. Echocardiography reveals moderate to severe right ventricular dilatation with severe right ventricular systolic dysfunction. A CT of the chest and abdomen reveals a solid, non-obstructing 2 cm mass in the small intestine and a solid 1.5 cm mass in the liver. What is the most likely cause of her symptoms?
- A. Carcinoid tumor (Correct Answer)
- B. Bronchial asthma
- C. Irritable bowel syndrome
- D. Systemic mastocytosis
- E. Whipple’s disease
Whipple procedure indications Explanation: ***Carcinoid tumor***
- The patient's symptoms of **fatigue, dyspnea, flushing, loose stools, palpitations, non-pitting edema**, and **wheezing** are all classic manifestations of **carcinoid syndrome**. The finding of a solid mass in the **small intestine** with **liver metastasis** in conjunction with right-sided heart valve involvement (holosystolic murmur louder on inspiration, right ventricular dilatation and dysfunction) is highly suggestive of a neuroendocrine tumor producing vasoactive substances.
- **Right-sided cardiac involvement** is a hallmark of **carcinoid syndrome**, as the vasoactive substances are typically metabolized by the lungs, protecting the left side of the heart.
*Bronchial asthma*
- While **wheezing** is present, it is usually the primary and often isolated respiratory symptom in asthma. Other systemic symptoms like **flushing, diarrhea, and right heart failure** are not characteristic of bronchial asthma.
- Asthma is not associated with **gastrointestinal masses** or structural **cardiac abnormalities** like right ventricular dilation and dysfunction.
*Irritable bowel syndrome*
- While **loose stools** are seen in IBS, the presence of **flushing, wheezing, palpitations, and significant cardiac pathology** makes IBS an unlikely diagnosis.
- IBS is a functional disorder and does not cause **solid masses** in the intestine or liver, nor does it lead to **right ventricular dysfunction**.
*Systemic mastocytosis*
- This condition can cause **flushing, diarrhea, and cardiac symptoms (tachycardia, hypotension)**, similar to carcinoid syndrome, due to the release of histamine and other mediators from mast cells.
- However, characteristic features of systemic mastocytosis include **urticaria pigmentosa (cutaneous mastocytomas)**, bone pain, and elevated serum tryptase, which are not described in this patient. The presence of **solid intestinal and liver masses** is also more consistent with a tumor than mastocytosis.
*Whipple’s disease*
- This disease can cause **diarrhea, malabsorption, weight loss, and fatigue**, but it is also commonly associated with **arthralgias, lymphadenopathy, and neurological symptoms**.
- **Whipple's disease** does not typically cause **flushing, wheezing, or discrete solid masses** in the intestine and liver, nor does it directly lead to **right-sided heart valve dysfunction** in this manner.
Whipple procedure indications US Medical PG Question 2: A 55-year-old female presents to the emergency room complaining of severe abdominal pain. She reports a six-month history of worsening dull mid-epigastric pain that she had attributed to stress at work. She has lost fifteen pounds over that time. She also reports that her stools have become bulky, foul-smelling, and greasy. Over the past few days, her abdominal pain acutely worsened and seemed to radiate to her back. She also developed mild pruritus and yellowing of her skin. Her temperature is 101°F (38.3°C), blood pressure is 145/85 mmHg, pulse is 110/min, and respirations are 20/min. On examination, her skin appears yellowed and she is tender to palpation in her mid-epigastrium and right upper quadrant. She is subsequently sent for imaging. If a mass is identified, what would be the most likely location of the mass?
- A. Pancreatic duct
- B. Common hepatic duct
- C. Cystic duct
- D. Common bile duct
- E. Ampulla of Vater (Correct Answer)
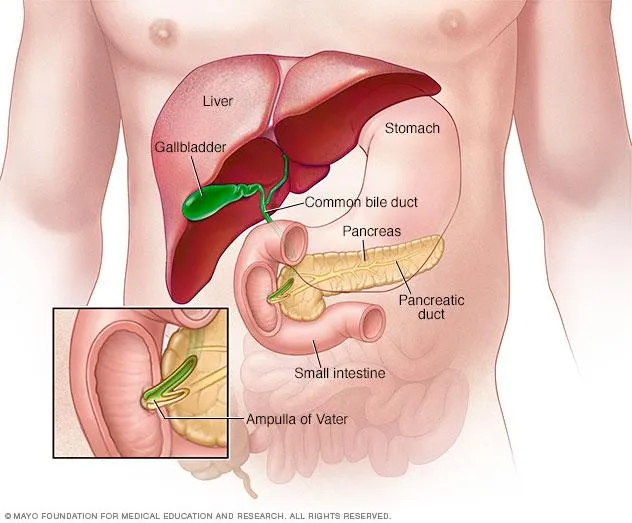
Whipple procedure indications Explanation: ***Ampulla of Vater***
- The patient's presentation represents classic **periampullary obstruction** with **"double duct" involvement** affecting both the pancreatic duct and common bile duct.
- **Steatorrhea** and **epigastric pain radiating to the back** indicate pancreatic duct obstruction causing exocrine pancreatic insufficiency and chronic pancreatitis.
- **Jaundice** and **pruritus** indicate common bile duct obstruction causing cholestasis.
- A mass at the **ampulla of Vater** (where the pancreatic duct and common bile duct merge before entering the duodenum) explains the entire clinical picture, including the **painless progressive jaundice** with a palpable gallbladder (Courvoisier's sign).
*Pancreatic duct*
- An obstruction solely in the **pancreatic duct** (e.g., in the body or tail of the pancreas) would cause steatorrhea, weight loss, and pain from pancreatic insufficiency and pancreatitis.
- However, it would **not cause jaundice or pruritus** unless the mass grew large enough to secondarily compress the common bile duct, which would be a late finding rather than a presenting feature.
*Common hepatic duct*
- Obstruction of the **common hepatic duct** would cause jaundice and pruritus from biliary obstruction.
- However, it would **not cause steatorrhea** or the chronic pancreatic pain radiating to the back that results from pancreatic duct obstruction.
- This location does not explain the pancreatic insufficiency symptoms that are prominent in this case.
*Cystic duct*
- Obstruction of the **cystic duct** leads to **acute cholecystitis** and biliary colic, not the chronic progressive symptoms described.
- It would **not cause jaundice** (the cystic duct only drains the gallbladder, not the hepatic bile flow) unless a stone migrated to the common bile duct.
- It does not explain the **steatorrhea** or pancreatic-type pain radiating to the back.
*Common bile duct*
- A mass in the **common bile duct** (proximal to the ampulla) could cause jaundice and pruritus by obstructing bile flow.
- However, it would **not directly obstruct the pancreatic duct**, so it would not explain the **steatorrhea** and **pancreatic pain radiating to the back** that are prominent features in this case.
- Only at the ampulla, where both ducts converge, would a single mass cause both sets of symptoms simultaneously.
Whipple procedure indications US Medical PG Question 3: A 52-year-old man presents with 2 months of diarrhea, abdominal pain, and fatigue. He reports a weight loss of 4 kg (8 lb). He also says his joints have been hurting recently, as well. Past medical history is unremarkable. Review of systems is significant for problems with concentration and memory. Physical examination is unremarkable. A GI endoscopy is performed with a biopsy of the small bowel. Which of the following histologic finding would most likely be seen in this patient?
- A. PAS positive macrophages (Correct Answer)
- B. Non-caseating granulomas in the small intestine
- C. Absence of nerves in the myenteric plexus
- D. Blunting of the villi
- E. Crypt hyperplasia with increased intraepithelial lymphocytes
Whipple procedure indications Explanation: **PAS positive macrophages**
- The clinical presentation with **diarrhea**, abdominal pain, weight loss, joint pain, and **neurological symptoms** (problems with concentration and memory) is classic for **Whipple's disease**.
- **Whipple's disease** is caused by the bacterium **Tropheryma whipplei**, which is characterized histologically by **foamy macrophages** in the lamina propria that stain **positive with Periodic Acid-Schiff (PAS)** due to undigested bacterial cell wall material.
*Non-caseating granulomas in the small intestine*
- **Non-caseating granulomas** are characteristic of **Crohn's disease**, which typically presents with abdominal pain, diarrhea, and weight loss, but **neurological symptoms** are not a primary feature.
- While Crohn's disease can cause joint pain (arthritis), the combination of GI and neurological symptoms points away from it.
*Absence of nerves in the myenteric plexus*
- An **absence of nerves in the myenteric plexus** is the hallmark of **Hirschsprung's disease**, which is a congenital disorder primarily affecting neonates and infants, causing intestinal obstruction and chronic constipation.
- This finding is inconsistent with the patient's age and presenting symptoms of diarrhea and neurological issues.
*Blunting of the villi*
- **Villi blunting** is characteristic of **celiac disease** (gluten-sensitive enteropathy), which presents with malabsorption symptoms like diarrhea, weight loss, and abdominal pain.
- However, **celiac disease** typically does not involve **neurological symptoms** like concentration and memory problems as a prominent feature, and the PAS-positive macrophages are specific to Whipple's.
*Crypt hyperplasia with increased intraepithelial lymphocytes*
- **Crypt hyperplasia** and **increased intraepithelial lymphocytes (IELs)** are seen in various small bowel pathologies, including **celiac disease** and **microscopic colitis**.
- While these findings suggest intestinal inflammation, they are not specific to **Whipple's disease** and do not account for the characteristic neurological involvement.
Whipple procedure indications US Medical PG Question 4: A 50-year-old Caucasian man is admitted to the ER with an 8-hour history of intense abdominal pain that radiates to the back, nausea, and multiple episodes of vomiting. Past medical history is insignificant. His blood pressure is 90/60 mm Hg, pulse is 120/min, respirations are 20/min, and body temperature is 37.8°C (100°F). Upon examination, he has significant epigastric tenderness, and hypoactive bowel sounds. Serum lipase and amylase are elevated and the patient rapidly deteriorates, requiring transfer to the intensive care unit for a month. After being stabilized, he is transferred to the general medicine floor with an abdominal computed tomography (CT) reporting a well-circumscribed collection of fluid of homogeneous density. Which of the following best describes the condition this patient has developed?
- A. Acute necrotic collection
- B. Fistula formation
- C. Walled-off necrosis
- D. Pancreatic pseudocyst (Correct Answer)
- E. Pancreatic cancer
Whipple procedure indications Explanation: ***Pancreatic pseudocyst***
- The patient experienced an episode of **severe acute pancreatitis**, followed by the development of a well-circumscribed collection of fluid with homogeneous density, which is characteristic of a **pancreatic pseudocyst**.
- **Pseudocysts** are collections of pancreatic fluid and inflammatory exudates that become encapsulated by a fibrous wall, typically appearing around 4 weeks after an episode of acute pancreatitis.
*Acute necrotic collection*
- An **acute necrotic collection** is an early phase (within 4 weeks) of peripancreatic fluid collection that contains both fluid and non-viable pancreatic or peripancreatic tissue, which is not described as homogeneous in density.
- This term usually refers to the initial, unorganized collection of necrotic material, prior to the development of a well-defined wall.
*Fistula formation*
- **Fistula formation** involves an abnormal connection between two epithelialized organs or between an organ and the skin, which is not described by a well-circumscribed fluid collection.
- While it can be a complication of pancreatitis, the CT finding of a homogeneous fluid collection does not directly indicate a fistula.
*Walled-off necrosis*
- **Walled-off necrosis (WON)** is a mature collection (typically >4 weeks) of pancreatic and/or peripancreatic necrotic tissue that has developed a well-defined inflammatory wall but contains a significant solid/necrotic component.
- The CT description of a "homogeneous density" fluid collection does not align with WON, which would typically show heterogeneous density due to solid necrotic debris.
*Pancreatic cancer*
- **Pancreatic cancer** is an abnormal growth of cells within the pancreas and would typically present as a mass lesion, often with tissue invasion.
- While a pseudocyst can sometimes mimic a cystic tumor, the history of acute pancreatitis and the specific CT description of a homogeneous fluid collection make pancreatic cancer less likely in this context.
Whipple procedure indications US Medical PG Question 5: A 51-year-old woman presents to her primary care doctor with diarrhea. She has had 3-10 malodorous and loose bowel movements daily for the last 6 months, though she recalls that her bowel movements started increasing in frequency nearly 2 years ago. She was otherwise healthy until 2 years ago, when she had multiple elevated fasting blood glucose levels and was diagnosed with type 2 diabetes mellitus. She was also hospitalized once 6 months ago for epigastric pain that was determined to be due to cholelithiasis. She is an avid runner and runs 3-4 marathons per year. She is a vegetarian and takes all appropriate supplements. Her body mass index is 19 kg/m^2. She has lost 10 pounds since her last visit 18 months ago. On exam, she has dry mucous membranes and decreased skin turgor. A high-resolution spiral computerized tomography scan demonstrates a 5-cm enhancing lesion in the head of the pancreas. Additional similar lesions are found in the liver. Further laboratory workup confirms the diagnosis. The patient is offered surgery but refuses as she reportedly had a severe complication from anesthesia as a child. This patient should be treated with a combination of octreotide, 5-fluorouracil, and which other medication?
- A. Paclitaxel
- B. Glucagon
- C. Streptozotocin (Correct Answer)
- D. Insulin
- E. Methotrexate
Whipple procedure indications Explanation: ***Streptozotocin***
- The patient's presentation with **diarrhea**, **weight loss**, **new-onset diabetes**, and a **pancreatic mass with liver metastases** is highly suggestive of a **neuroendocrine tumor**, specifically a **VIPoma** or **gastrinoma** with potential for glucagonoma given the diabetes. Given the recommended treatment with octreotide and 5-fluorouracil, **streptozotocin** is a key cytotoxic chemotherapy agent used in the treatment of metastatic pancreatic neuroendocrine tumors.
- **Streptozotocin** is an **alkylating agent** that targets pancreatic islet cells and is effective in combination with 5-fluorouracil for advanced, well-differentiated neuroendocrine tumors, especially those that are functional and causing symptoms.
*Paclitaxel*
- **Paclitaxel** is a **microtubule inhibitor** primarily used in breast, ovarian, and lung cancers. It is not a standard chemotherapy agent for pancreatic neuroendocrine tumors in combination with octreotide and 5-fluorouracil.
- While sometimes used in other pancreatic malignancies (e.g., pancreatic adenocarcinoma), it is **not indicated** for the specific context of this neuroendocrine tumor treatment regimen.
*Glucagon*
- **Glucagon** is a hormone that **raises blood glucose levels** and would be contraindicated in a patient with new-onset diabetes and a pancreatic tumor, potentially exacerbating hyperglycemia.
- It is a **hormone**, not a chemotherapy agent, and has no role in treating the underlying pancreatic neuroendocrine tumor.
*Insulin*
- **Insulin** treats hyperglycemia, which is a symptom in this patient due to likely a **glucagonoma** or other neuroendocrine tumor affecting glucose metabolism. However, it does not treat the underlying tumor.
- While necessary for managing diabetes, **insulin** is a supportive treatment and not the chemotherapy agent required to combine with octreotide and 5-fluorouracil for directly targeting the tumor.
*Methotrexate*
- **Methotrexate** is an **antimetabolite** primarily used in various cancers like leukemia, lymphoma, and autoimmune diseases. It is not part of the standard chemotherapy regimen for pancreatic neuroendocrine tumors.
- Its mechanism of action and efficacy profile do not align with the treatment of well-differentiated metastatic pancreatic neuroendocrine tumors in this context.
Whipple procedure indications US Medical PG Question 6: A CT scan of the abdomen reveals a mass in the pancreatic uncinate process. Which of the following structures is most likely to be compressed by this mass?
- A. Common bile duct
- B. Portal vein
- C. Splenic vein
- D. Superior mesenteric vein (Correct Answer)
Whipple procedure indications Explanation: ***Superior mesenteric vein***
- The **uncinate process** of the pancreas hooks around the **superior mesenteric vessels**. Therefore, a mass in this region would most directly compress the **superior mesenteric vein (SMV)** and artery (SMA).
- Compression of the SMV can lead to **venous outflow obstruction** from the small intestine, potentially causing **bowel ischemia** or edema.
*Common bile duct*
- The **common bile duct** passes through the **head of the pancreas**, not typically the uncinate process.
- Compression of the common bile duct would more commonly be associated with masses in the **head of the pancreas**, leading to **jaundice**.
*Portal vein*
- The **portal vein** is formed by the union of the **splenic vein** and the **superior mesenteric vein**, generally posterior to the neck of the pancreas.
- While pancreatic masses can affect the portal vein, a mass specifically in the uncinate process would more directly impinge on the SMV before significantly affecting the main portal vein, which is superior and posterior to the uncinate process.
*Splenic vein*
- The **splenic vein** runs along the **posterior aspect of the body and tail of the pancreas**.
- A mass in the uncinate process, located at the inferior margin of the head, is relatively distant from the splenic vein.
Whipple procedure indications US Medical PG Question 7: A 45-year-old woman comes to see you for a second opinion regarding an upcoming surgery for pancreatic insulinoma. While taking a surgical history, she tells you she previously had a pituitary tumor resected. For which additional neoplasms might you consider testing her?
- A. Parathyroid adenoma (Correct Answer)
- B. Medullary thyroid carcinoma
- C. Mucosal neuroma
- D. Multiple myeloma
- E. Pheochromocytoma
Whipple procedure indications Explanation: ***Parathyroid adenoma***
- The patient's history of a **pituitary tumor** and a **pancreatic insulinoma** strongly suggests **Multiple Endocrine Neoplasia Type 1 (MEN1)**.
- **Parathyroid adenomas** are the most common manifestation of MEN1, affecting over 90% of patients, and should be screened for.
*Medullary thyroid carcinoma*
- This is a characteristic component of **Multiple Endocrine Neoplasia Type 2 (MEN2)**.
- MEN2 includes medullary thyroid carcinoma, pheochromocytoma, and parathyroid hyperplasia, which is distinct from the patient's presentation.
*Mucosal neuroma*
- **Mucosal neuromas** are associated with **Multiple Endocrine Neoplasia Type 2B (MEN2B)**, a subtype of MEN2.
- MEN2B also typically involves medullary thyroid carcinoma and pheochromocytoma, which do not align with the patient's current tumors.
*Multiple myeloma*
- This is a **hematologic malignancy** involving plasma cells and is not typically associated with the type of endocrine tumors seen in this patient.
- There is no direct link between multiple myeloma and pituitary or pancreatic neuroendocrine tumors.
*Pheochromocytoma*
- **Pheochromocytoma** is a tumor of the adrenal medulla and is a hallmark of **Multiple Endocrine Neoplasia Type 2 (MEN2)**.
- While it is an endocrine tumor, it is not part of the triad seen in MEN1 (pituitary, parathyroid, and pancreatic tumors).
Whipple procedure indications US Medical PG Question 8: A 64-year-old woman presents to the physician’s office to find out the results of her recent abdominal CT. She had been complaining of fatigue, weight loss, and jaundice for 6 months prior to seeing the physician. The patient has a significant medical history of hypothyroidism, generalized anxiety disorder, and hyperlipidemia. She takes levothyroxine, sertraline, and atorvastatin. The vital signs are stable today. On physical examination, her skin shows slight jaundice, but no scleral icterus is present. The palpation of the abdomen reveals no tenderness, guarding, or masses. The CT results shows a 3 x 3 cm mass located at the head of the pancreas. Which of the following choices is most appropriate for delivering bad news to the patient?
- A. Refer the patient to an oncologist without informing the patient of their cancer
- B. Ask that a spouse or close relative come to the appointment, explain to them the bad news, and see if they will tell the patient since they have a closer relationship
- C. Set aside an appropriate amount of time in your schedule, and ensure you will not have any interruptions as you explain the bad news to the patient (Correct Answer)
- D. Call the patient over the phone to break the bad news, and tell them they can make an office visit if they prefer
- E. Train one of the nursing staff employees on this matter, and delegate this duty as one of their job responsibilities
Whipple procedure indications Explanation: ***Set aside an appropriate amount of time in your schedule, and ensure you will not have any interruptions as you explain the bad news to the patient***
- Delivering bad news requires a **dedicated, uninterrupted environment** to allow for clear communication, emotional support, and time for the patient to process the information and ask questions.
- Adequate time ensures that the physician can address immediate concerns, explore the patient's understanding, and collaboratively plan the next steps, fostering **trust and patient-centered care**.
*Refer the patient to an oncologist without informing the patient of their cancer*
- This approach violates the principle of **patient autonomy** and the ethical obligation to provide complete and accurate information about their diagnosis.
- Patients have a right to know their medical status and actively participate in decisions regarding their care, which includes being informed of a **cancer diagnosis**.
*Ask that a spouse or close relative come to the appointment, explain to them the bad news, and see if they will tell the patient since they have a closer relationship*
- While involving family is important for support, the **primary responsibility** to deliver difficult medical news rests with the physician directly to the patient.
- This avoids potential miscommunication, ensures the patient receives accurate information from the medical professional, and respects the patient's individual right to hear their diagnosis without an intermediary.
*Call the patient over the phone to break the bad news, and tell them they can make an office visit if they prefer*
- Delivering significant bad news, especially a potential cancer diagnosis, over the phone is generally **inappropriate and insensitive**, as it lacks the personal presence and immediate support needed.
- A phone call does not allow for non-verbal cues, immediate emotional support, or a comprehensive discussion of complex medical information, making an **in-person consultation preferential**.
*Train one of the nursing staff employees on this matter, and delegate this duty as one of their job responsibilities*
- Delivering a new and serious medical diagnosis, such as cancer, is primarily the **responsibility of the treating physician** due to the complexity of the information and the need for medical expertise.
- While nurses play a crucial role in patient education and support, conveying initial diagnoses of this gravity falls outside their typical scope of practice and could erode **patient trust**.
Whipple procedure indications US Medical PG Question 9: A 66-year-old man comes to the physician because of yellowish discoloration of his eyes and skin, abdominal discomfort, and generalized fatigue for the past 2 weeks. He has had dark urine and pale stools during this period. He has had a 10-kg (22-lb) weight loss since his last visit 6 months ago. He has hypertension. He has smoked one pack of cigarettes daily for 34 years. He drinks three to four beers over the weekends. His only medication is amlodipine. His temperature is 37.3°C (99.1°F), pulse is 89/min, respirations are 14/min, and blood pressure is 114/74 mm Hg. Examination shows jaundice of the sclera and skin and excoriation marks on his trunk and extremities. The lungs are clear to auscultation. The abdomen is soft and nontender. The remainder of the examination shows no abnormalities. Laboratory studies show:
Hemoglobin 12 g/dL
Leukocyte count 5,000/mm3
Platelet count 400,000/mm3
Serum
Urea nitrogen 28 mg/dL
Creatinine 1.2 mg/dL
Bilirubin
Total 7.0 mg/dL
Direct 5.5 mg/dL
Alkaline phosphatase 615 U/L
Aspartate aminotransferase (AST, GOT) 170 U/L
Alanine aminotransferase (ALT, GPT) 310 U/L
γ-Glutamyltransferase (GGT) 592 U/L (N = 5–50 U/L)
An ultrasound shows extrahepatic biliary dilation. A CT scan of the abdomen shows a 2.5-cm (1-in) mass in the head of the pancreas with no abdominal lymphadenopathy. The patient undergoes biliary stenting. Which of the following is the most appropriate next step in the management of this patient?
- A. Gemcitabine and 5-fluorouracil therapy
- B. Stereotactic radiation therapy
- C. Central pancreatectomy
- D. Gastroenterostomy
- E. Pancreaticoduodenectomy (Correct Answer)
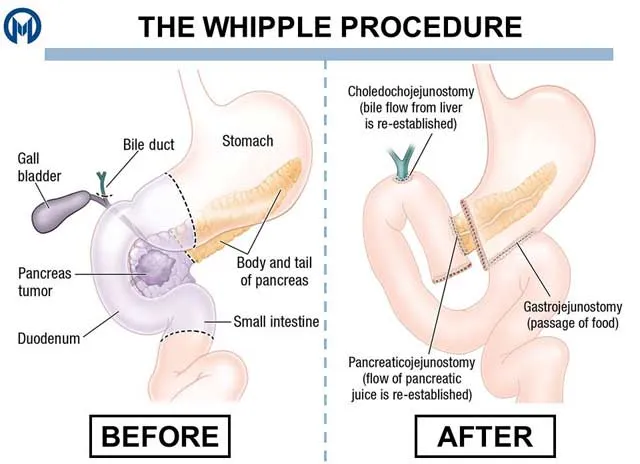
Whipple procedure indications Explanation: ***Pancreaticoduodenectomy***
- The patient presents with **obstructive jaundice**, a **pancreatic head mass** on CT, and **significant weight loss**, highly suggestive of **pancreatic adenocarcinoma**.
- Given the mass is localized to the head of the pancreas without evidence of metastases or lymphadenopathy on CT, **surgical resection (Whipple procedure)** is the only potentially curative treatment.
*Gemcitabine and 5-fluorouracil therapy*
- This is a form of **chemotherapy** commonly used for **advanced or metastatic pancreatic cancer**, or as adjuvant therapy after surgical resection.
- It is not the most appropriate *initial* step for a potentially resectable tumor, as surgery offers the best chance for cure.
*Stereotactic radiation therapy*
- **Radiation therapy** is typically used for **locally advanced, unresectable pancreatic cancer** to control tumor growth and symptoms, or as an adjunct to chemotherapy.
- It is not a primary curative treatment for resectable pancreatic head masses.
*Central pancreatectomy*
- **Central pancreatectomy** is a less common procedure typically reserved for tumors in the **neck or body of the pancreas**, aiming to preserve the pancreatic head and tail.
- It is not appropriate for a mass located in the **head of the pancreas** that is causing biliary obstruction.
*Gastroenterostomy*
- **Gastroenterostomy** is a **palliative surgical procedure** used to bypass an obstructed duodenum, often due to an **unresectable pancreatic head mass** causing gastric outlet obstruction.
- While the patient has obstructive jaundice, the primary goal here is to resect the tumor, not merely bypass the obstruction, especially since it appears resectable.
Whipple procedure indications US Medical PG Question 10: A 27-year-old-man is brought to the emergency department 30 minutes after being involved in a motorcycle accident. He lost control at high speed and was thrown forward onto the handlebars. On arrival, he is alert and responsive. He has abdominal pain and superficial lacerations on his left arm. Vital signs are within normal limits. Examination shows a tender, erythematous area over his epigastrium. The abdomen is soft and non-distended. A CT scan of the abdomen shows no abnormalities. Treatment with analgesics is begun, the lacerations are cleaned and dressed, and the patient is discharged home after 2 hours of observation. Four days later, the patient returns to the emergency department with gradually worsening upper abdominal pain, fever, poor appetite, and vomiting. His pulse is 91/min and blood pressure is 135/82 mm Hg. Which of the following is the most likely diagnosis?
- A. Abdominal compartment syndrome
- B. Aortic dissection
- C. Splenic rupture
- D. Pancreatic ductal injury (Correct Answer)
- E. Diaphragmatic rupture
Whipple procedure indications Explanation: ***Pancreatic ductal injury***
- A forceful impact to the **epigastrium** (e.g., falling onto handlebars) can cause **pancreatic injury**, particularly a **ductal transection**, due to the pancreas being compressed against the vertebral column.
- Initial CT scans can be normal because the injury to the **ductal system** takes time to manifest, leading to delayed symptoms like **worsening abdominal pain, fever, vomiting**, and **poor appetite** several days later due to **pancreatitis** or a **pseudocyst** formation.
*Abdominal compartment syndrome*
- This typically presents with **acute abdominal distension**, increased intra-abdominal pressure, and organ dysfunction (e.g., oliguria, respiratory compromise), which are not described here.
- It's an immediate complication of severe trauma or fluid resuscitation, not a delayed presentation like described.
*Aortic dissection*
- Characterized by **sudden-onset, severe, tearing chest or back pain** and often involves hypertension or Marfan syndrome.
- It would manifest immediately with hemodynamic instability and distinct pain, not a delayed presentation of progressive abdominal symptoms.
*Splenic rupture*
- Often causes **left upper quadrant pain**, **Kehr's sign** (referred shoulder pain), and **hemodynamic instability** due to significant blood loss.
- While possible in trauma, a normal initial CT scan makes this less likely, and its symptoms usually appear earlier or are more severe.
*Diaphragmatic rupture*
- Can present with **dyspnea, shoulder pain**, or signs of **herniated abdominal organs** into the chest.
- It causes more immediate respiratory distress or gastrointestinal obstruction symptoms, and the abdominal symptoms described are not typical for this injury.
More Whipple procedure indications US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.