Small bowel resection and anastomosis US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Small bowel resection and anastomosis. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Small bowel resection and anastomosis US Medical PG Question 1: A 72-year-old female presents to the emergency department complaining of severe abdominal pain and several days of bloody diarrhea. Her symptoms began with intermittent bloody diarrhea five days ago and have worsened steadily. For the last 24 hours, she has complained of fevers, chills, and abdominal pain. She has a history of ulcerative colitis, idiopathic hypertension, and hypothyroidism. Her medications include hydrochlorothiazide, levothyroxine, and sulfasalazine.
In the ED, her temperature is 39.1°C (102.4°F), pulse is 120/min, blood pressure is 90/60 mmHg, and respirations are 20/min. On exam, the patient is alert and oriented to person and place, but does not know the day. Her mucus membranes are dry. Heart and lung exam are not revealing. Her abdomen is distended with marked rebound tenderness. Bowel sounds are hyperactive.
Serum:
Na+: 142 mEq/L
Cl-: 107 mEq/L
K+: 3.3 mEq/L
HCO3-: 20 mEq/L
BUN: 15 mg/dL
Glucose: 92 mg/dL
Creatinine: 1.2 mg/dL
Calcium: 10.1 mg/dL
Hemoglobin: 11.2 g/dL
Hematocrit: 30%
Leukocyte count: 14,600/mm^3 with normal differential
Platelet count: 405,000/mm^3
What is the next best step in management?
- A. Emergent colonoscopy
- B. Contrast enema
- C. Colectomy
- D. Plain abdominal radiograph
- E. Abdominal CT with IV contrast (Correct Answer)
Small bowel resection and anastomosis Explanation: ***Abdominal CT with IV contrast***
- The patient presents with **severe abdominal pain, bloody diarrhea, fever, hypotension, tachycardia, abdominal distension, rebound tenderness, and leukocytosis**, all suggestive of **toxic megacolon** complicating her ulcerative colitis.
- An **abdominal CT with IV contrast** is the most appropriate next step to confirm the diagnosis, assess the extent of colonic dilation and inflammation, and rule out complications like perforation.
*Emergent colonoscopy*
- **Colonoscopy** is generally **contraindicated** in suspected toxic megacolon due to the high risk of **perforation** of the severely inflamed and dilated colon.
- While it can diagnose ulcerative colitis, the current acute, severe presentation makes it too risky.
*Contrast enema*
- A **contrast enema** is also **contraindicated** in setting of potential **toxic megacolon** or suspected colonic perforation.
- The pressure from the contrast agent could worsen dilation or cause perforation in an already compromised colon.
*Colectomy*
- **Colectomy** is a surgical intervention reserved for cases of **toxic megacolon** that **fail medical management** or when there is evidence of **perforation** or **ischemia**.
- It is not the *immediate* next step in management without further imaging and attempts at medical stabilization.
*Plain abdominal radiograph*
- A plain abdominal radiograph can show colonic dilation and air-fluid levels, which are indicative of toxic megacolon; however, it has **limited ability to assess the extent of inflammation**, detect complications like **perforation**, or rule out other intra-abdominal pathologies.
- It might be a useful initial screen but is not as comprehensive as a CT scan, especially when a definitive diagnosis and management plan is needed.
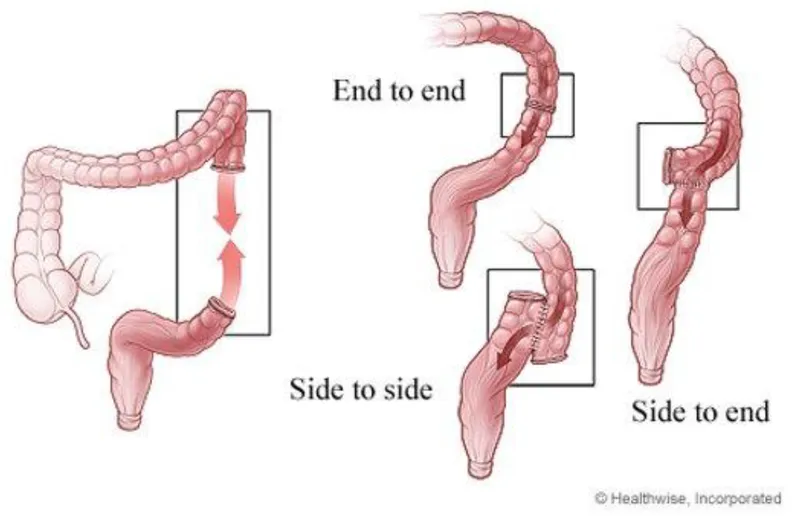
Small bowel resection and anastomosis US Medical PG Question 2: A 69-year-old male presents to the Emergency Department with bilious vomiting that started within the past 24 hours. His medical history is significant for hypertension, hyperlipidemia, and a myocardial infarction six months ago. His past surgical history is significant for a laparotomy 20 years ago for a perforated diverticulum. Most recently he had some dental work done and has been on narcotic pain medicine for the past week. He reports constipation and obstipation. He is afebrile with a blood pressure of 146/92 mm Hg and a heart rate of 116/min. His abdominal exam reveals multiple well-healed scars with distension but no tenderness. An abdominal/pelvic CT scan reveals dilated small bowel with a transition point to normal caliber bowel distally. When did the cause of his pathology commence?
- A. One week ago
- B. Six months ago
- C. 20 years ago (Correct Answer)
- D. At birth
- E. 24 hours ago
Small bowel resection and anastomosis Explanation: ***20 years ago***
- The patient's history of a **laparotomy 20 years ago** for a perforated diverticulum is the most likely cause of his current small bowel obstruction. **Adhesions** from prior abdominal surgery are the leading cause of small bowel obstruction.
- The CT scan finding of **dilated small bowel** with a **transition point** confirms a mechanical obstruction, and the operative scarring supports adhesions as the etiology.
*One week ago*
- While **narcotic pain medicine** can cause constipation and ileus, it typically leads to a more diffuse distention without a clear transition point characteristic of a mechanical obstruction.
- The development of a clear transition point on CT after only one week of narcotic use makes a mechanical obstruction from adhesions more likely than a pure narcotic-induced ileus.
*Six months ago*
- A **myocardial infarction** six months ago is not directly related to the development of a small bowel obstruction.
- While cardiac events can sometimes lead to mesenteric ischemia, the CT findings of a transition point are more indicative of a mechanical obstruction rather than ischemia.
*At birth*
- Congenital conditions causing small bowel obstruction, such as **atresia** or **malrotation**, typically present in infancy or early childhood.
- Given the patient's age and history of prior abdominal surgery, a congenital cause is highly unlikely.
*24 hours ago*
- The onset of symptoms within the past 24 hours describes the **acute presentation** of the obstruction, not its underlying cause.
- The obstruction itself developed over time due to a predisposing factor from his past medical history.
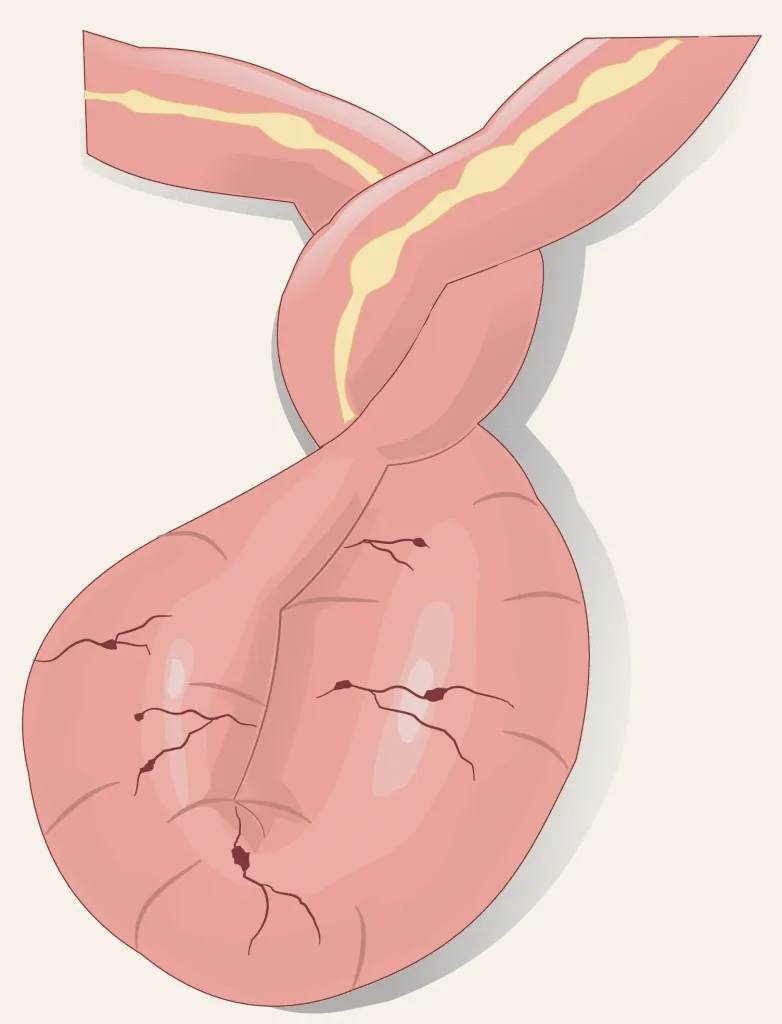
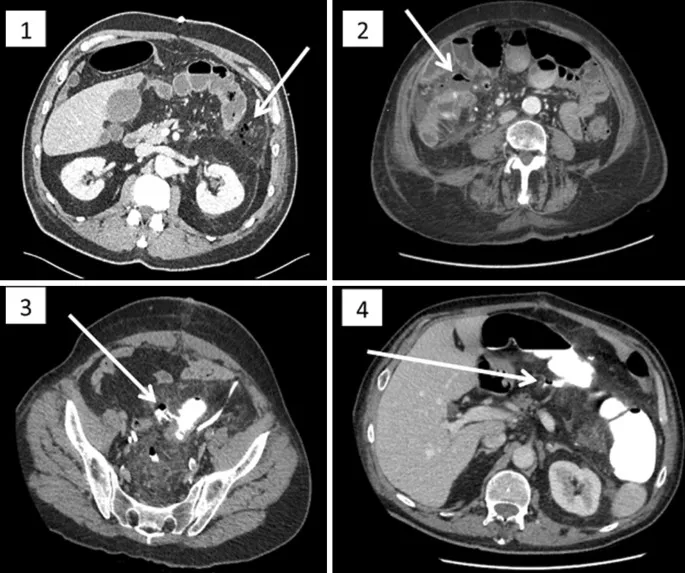
Small bowel resection and anastomosis US Medical PG Question 3: A 76-year-old female is brought to the emergency department after being found unresponsive in her room at her nursing facility. Past medical history is significant for Alzheimer's disease, hypertension, and diabetes. Surgical history is notable for an open cholecystectomy at age 38 and multiple cesarean sections. On arrival, she is non-responsive but breathing by herself, and her vital signs are T 102.9 F, HR 123 bpm, BP 95/64, RR 26/min, and SaO2 97% on 6L nasal cannula. On physical exam the patient has marked abdominal distension and is tympanic to percussion. Laboratory studies are notable for a lactic acidosis. An upright abdominal radiograph and CT abdomen/pelvis with contrast are shown in Figures A and B respectively. She is started on IV fluids and a nasogastric tube is placed to suction which returns green bilious fluid. Repeat vitals 1 hour later are T 101F, HR 140 bpm, BP 75/44, RR 30/min, and SaO2 is 100% on the ventilator after she is intubated for airway concerns. What is the next best step in management?
- A. Sigmoidoscopy, attempted derotation and rectal tube placement
- B. Continue IV fluid hydration, nasogastric suction, NPO
- C. Pneumatic enema
- D. Immediate laparotomy and surgical management (Correct Answer)
- E. Therapy with levofloxacin and metronidazole
Small bowel resection and anastomosis Explanation: ***Immediate laparotomy and surgical management***
- The patient presents with **signs of shock** (hypotension, tachycardia, tachypnea, fever, lactic acidosis) and **peritoneal signs** (marked abdominal distension, tympany) along with imaging findings (not provided but implied by the clinical picture) consistent with **bowel obstruction complicated by ischemia or perforation**. **Laparotomy** is urgently needed to address the underlying surgical emergency.
- Given the patient's deteriorating vital signs despite initial resuscitation, and the likelihood of **severe bowel compromise**, medical management or less invasive procedures are insufficient and would delay definitive treatment.
*Sigmoidoscopy, attempted derotation and rectal tube placement*
- This approach is typically used for **uncomplicated sigmoid volvulus** in a stable patient without signs of perforation or peritonitis.
- Given the patient's **septic shock** and **lactic acidosis**, there is a high suspicion of bowel ischemia or perforation, making endoscopic derotation contraindicated and dangerous.
*Continue IV fluid hydration, nasogastric suction, NPO*
- While important initial steps for any bowel obstruction, these measures alone are **insufficient** given the patient's rapidly deteriorating condition and evidence of **organ damage** (lactic acidosis suggests tissue hypoperfusion/ischemia).
- These are supportive measures, not definitive treatment for a **surgical emergency** like complicated bowel obstruction.
*Pneumatic enema*
- **Pneumatic enema** is primarily used for the reduction of **intussusception**, usually in pediatric patients.
- It is **not indicated** for the management of suspected bowel obstruction with signs of ischemia or perforation in an elderly patient and could be harmful.
*Therapy with levofloxacin and metronidazole*
- While **antibiotics** are crucial in managing septic shock due to an abdominal source, they are an **adjunctive treatment** and not the primary step for a surgical emergency.
- Antibiotics alone will not resolve the underlying mechanical obstruction or address compromised bowel, which requires **surgical intervention**.
Small bowel resection and anastomosis US Medical PG Question 4: A 64-year-old woman has progressively worsening abdominal pain 5 hours after an open valve replacement with cardiopulmonary bypass. The pain is crampy and associated with an urge to defecate. The patient reports having had 2 bloody bowel movements in the last hour. Her operation was complicated by significant intraoperative blood loss, which prolonged the operation and necessitated 2 transfusions of red blood cells. She has hypercholesterolemia and type 2 diabetes mellitus. The patient received prophylactic perioperative antibiotics and opioid pain management during recovery. Her temperature is 37.9°C (98.9°F), pulse is 95/min, and blood pressure is 115/69 mm Hg. Examination shows a soft abdomen with mild tenderness to palpation in the left quadrants but no rebound tenderness or guarding. Bowel sounds are decreased. Rectal examination shows blood on the examining finger. Which of the following is the most likely underlying cause of this patient's symptoms?
- A. Embolization of superior mesenteric artery
- B. Atherosclerotic narrowing of the intestinal vessels
- C. Small outpouchings in the sigmoid wall
- D. Infection with Clostridioides difficile
- E. Decreased blood flow to the splenic flexure (Correct Answer)
Small bowel resection and anastomosis Explanation: ***Decreased blood flow to the splenic flexure***
- This patient's symptoms are highly suggestive of **ischemic colitis**, which often affects the **splenic flexure** due to its "watershed" area vulnerability. **Cardiopulmonary bypass** and significant **intraoperative blood loss** (leading to hypotension and hypoperfusion) are major risk factors for this condition.
- The presentation with **crampy abdominal pain**, **urgent defecation**, and **bloody bowel movements** shortly after cardiac surgery points to colonic ischemia.
*Embolization of superior mesenteric artery*
- While an acute **SMA embolism** could cause severe abdominal pain and bloody stools, it typically presents with **more diffuse and severe abdominal tenderness**, often with marked tenderness disproportionate to examination findings early on, and rapid progression to peritonitis.
- The patient's history of valvular disease and hypercholesterolemia increases the risk of embolization, but the **mild tenderness confined to left quadrants** and decreased bowel sounds are less typical of an acute SMA occlusion.
*Atherosclerotic narrowing of the intestinal vessels*
- This describes **chronic mesenteric ischemia**, which typically causes **postprandial abdominal pain** (intestinal angina) and weight loss, not acute abdominal pain and bloody diarrhea in the immediate postoperative period.
- While the patient has risk factors for atherosclerosis (hypercholesterolemia, diabetes), the acute onset of symptoms following cardiac surgery points to an acute ischemic event rather than chronic narrowing.
*Small outpouchings in the sigmoid wall*
- This refers to **diverticulitis** or **diverticular bleeding**. While diverticular bleeding can cause painless or painful bleeding, and diverticulitis can cause abdominal pain, the acute onset post-cardiac surgery in the setting of hypoperfusion makes ischemic colitis a more likely diagnosis.
- Diverticulitis typically presents with **localized left lower quadrant pain**, fever, and leukocytosis, but the systemic context of recent cardiac surgery and hypoperfusion strongly favors ischemia.
*Infection with Clostridioides difficile*
- **_Clostridioides difficile_ infection** typically causes **watery diarrhea**, often after antibiotic use, and usually takes several days to develop symptoms after exposure or antibiotic initiation.
- Although the patient received perioperative antibiotics, the onset of symptoms within hours of surgery and the presence of **frank bloody stools** are less characteristic of _C. difficile_ infection, which is more commonly associated with non-bloody diarrhea.
Small bowel resection and anastomosis US Medical PG Question 5: A 47-year-old woman presents to the emergency department with abdominal pain. The patient states that she felt this pain come on during dinner last night. Since then, she has felt bloated, constipated, and has been vomiting. Her current medications include metformin, insulin, levothyroxine, and ibuprofen. Her temperature is 99.0°F (37.2°C), blood pressure is 139/79 mmHg, pulse is 95/min, respirations are 12/min, and oxygen saturation is 98% on room air. On physical exam, the patient appears uncomfortable. Abdominal exam is notable for hypoactive bowel sounds, abdominal distension, and diffuse tenderness in all four quadrants. Cardiac and pulmonary exams are within normal limits. Which of the following is the best next step in management?
- A. Metoclopramide
- B. Nasogastric tube, NPO, and IV fluids (Correct Answer)
- C. Stool guaiac
- D. Emergency surgery
- E. IV antibiotics and steroids
Small bowel resection and anastomosis Explanation: ***Nasogastric tube, NPO, and IV fluids***
- The patient's symptoms (abdominal pain, bloating, constipation, vomiting, distension, and hypoactive bowel sounds) are highly suggestive of a **bowel obstruction**.
- **Nasogastric tube decompression** relieves pressure, **NPO status** prevents further bowel distension, and **intravenous fluids** address dehydration and electrolyte imbalances, stabilizing the patient for further evaluation.
*Metoclopramide*
- This is a **prokinetic agent** that increases gastrointestinal motility.
- Using it in the context of a suspected bowel obstruction could worsen the condition by increasing pressure against the obstruction and potentially leading to **perforation**.
*Stool guaiac*
- A stool guaiac test detects the presence of **occult blood in the stool**, which is useful for evaluating gastrointestinal bleeding.
- While it can be part of a complete workup, it is not the immediate priority for a patient presenting with symptoms of **acute bowel obstruction** requiring stabilization.
*Emergency surgery*
- While surgery may ultimately be required for a bowel obstruction, it is not the immediate first step unless there are clear signs of **perforation**, **ischemia**, or **strangulation**, which are not specified here.
- Initial management involves **stabilization** with NG decompression, NPO, and IV fluids.
*IV antibiotics and steroids*
- **IV antibiotics** are indicated for suspected infection (e.g., appendicitis, diverticulitis with perforation), but the primary presentation here is mechanical obstruction, not infection.
- **Steroids** are typically used for inflammatory conditions or adrenal insufficiency, neither of which is indicated given the patient's symptoms.
Small bowel resection and anastomosis US Medical PG Question 6: A 55-year-old man is brought to the emergency department by his friends after he was found vomiting copious amounts of blood. According to his friends, he is a chronic alcoholic and lost his family and job because of his drinking. The admission vital signs were as follows: blood pressure is 100/75 mm Hg, heart rate is 95/min, respiratory rate is 15/min, and oxygen saturation is 97% on room air. He is otherwise alert and oriented to time, place, and person. The patient was stabilized with intravenous fluids and a nasogastric tube was inserted. He is urgently prepared for endoscopic evaluation. An image from the procedure is shown. Which of the following sets of pathologies with the portacaval anastomoses is paired correctly?
- A. Caput medusae | Caval (systemic): epigastric veins | Portal (hepatic): paraumbilical vein
- B. External hemorrhoids | Caval (systemic): middle and inferior rectal veins | Portal (hepatic): superior rectal vein
- C. Internal hemorrhoids | Caval (systemic): retroperitoneal veins | Portal (hepatic): colic veins
- D. Anorectal varices | Caval (systemic): inferior rectal vein | Portal (hepatic): middle rectal vein
- E. Esophageal varices | Caval (systemic): azygos vein | Portal (hepatic): left gastric vein (Correct Answer)
Small bowel resection and anastomosis Explanation: ***Esophageal varices | Caval (systemic): azygos vein | Portal (hepatic): left gastric vein***
- The clinical presentation of a **chronic alcoholic with hematemesis** and findings on **endoscopy** is classic for **esophageal varices** due to portal hypertension from cirrhosis.
- **Esophageal varices** form when the **left gastric vein** (portal system) becomes engorged and anastomoses with **esophageal tributaries** that drain into the **azygos and hemiazygos veins** (systemic circulation).
- This is one of the most clinically significant portacaval anastomoses, as rupture leads to life-threatening upper GI bleeding.
*Caput medusae | Caval (systemic): epigastric veins | Portal (hepatic): paraumbilical vein*
- **Caput medusae** results from dilation of **paraumbilical veins** (portal) anastomosing with **superficial and inferior epigastric veins** (systemic) around the umbilicus.
- While this pairing is anatomically correct, it presents as **visible dilated periumbilical veins** on physical exam, not hematemesis.
- This does not match the clinical scenario of acute upper GI bleeding.
*External hemorrhoids | Caval (systemic): middle and inferior rectal veins | Portal (hepatic): superior rectal vein*
- **External hemorrhoids** involve the **inferior rectal veins** draining into the internal pudendal vein (systemic → systemic).
- These are **not a true portacaval anastomosis** and would present with rectal bleeding or perianal discomfort, not hematemesis.
*Internal hemorrhoids | Caval (systemic): retroperitoneal veins | Portal (hepatic): colic veins*
- **Internal hemorrhoids** (anorectal varices) involve the **superior rectal vein** (portal) anastomosing with **middle and inferior rectal veins** (systemic).
- The vessels listed here (retroperitoneal veins and colic veins) are **incorrect** for this anastomosis.
- Would present with hematochezia (lower GI bleeding), not hematemesis.
*Anorectal varices | Caval (systemic): inferior rectal vein | Portal (hepatic): middle rectal vein*
- **Anorectal varices** involve the **superior rectal vein** (portal) anastomosing with **middle and inferior rectal veins** (systemic).
- The pairing here is **incorrect**: the middle rectal vein is part of the systemic circulation (drains to internal iliac vein), not portal.
- This would present with rectal bleeding, not hematemesis.
Small bowel resection and anastomosis US Medical PG Question 7: Four days after undergoing a total abdominal hysterectomy for atypical endometrial hyperplasia, a 59 year-old woman reports abdominal bloating and discomfort. She has also had nausea without vomiting. She has no appetite despite not having eaten since the surgery and drinking only sips of water. Her postoperative pain has been well controlled on a hydromorphone patient-controlled analgesia (PCA) pump. Her foley was removed on the second postoperative day and she is now voiding freely. Although she lays supine in bed for most of the day, she is able to walk around the hospital room with a physical therapist. Her temperature is 36.5°C (97.7°F), pulse is 84/min, respirations are 10/min, and blood pressure is 132/92 mm Hg. She is 175 cm (5 ft 9 in) tall and weighs 115 kg (253 lb); BMI is 37.55 kg/m2. Examination shows a mildly distended, tympanic abdomen; bowel sounds are absent. Laboratory studies are within normal limits. An x-ray of the abdomen shows uniform distribution of gas in the small bowel, colon, and rectum without air-fluid levels. Which of the following is the most appropriate next step in the management of this patient?
- A. Esophagogastroduodenoscopy
- B. Begin total parenteral nutrition
- C. Colonoscopy
- D. Gastrografin enema
- E. Reduce use of opioid therapy (Correct Answer)
Small bowel resection and anastomosis Explanation: ***Reduce use of opioid therapy***
- The patient's symptoms (bloating, discomfort, nausea, absent bowel sounds, diffuse gas on X-ray) after abdominal surgery are consistent with a **postoperative ileus**, which is often exacerbated by **opioid use**.
- Reducing opioids, if pain control allows, can help normalize gastrointestinal motility and resolve the ileus, as her vital signs are stable and there are no signs of obstruction or infection.
*Esophagogastroduodenoscopy*
- This procedure is primarily used to evaluate the **upper gastrointestinal tract** (esophagus, stomach, duodenum) for conditions like ulcers, inflammation, or obstruction.
- While the patient has nausea, there is no evidence suggesting an upper GI pathology that would warrant an EGD, especially with diffuse gas distribution on X-ray.
*Begin total parenteral nutrition*
- **Total parenteral nutrition (TPN)** is indicated when a patient cannot meet their nutritional needs via the enteral route for an extended period, typically more than 7-10 days, or in severe malnutrition.
- The patient has only been NPO for four days post-op, and addressing the underlying cause of her GI symptoms (likely ileus) is the priority before considering long-term nutritional support.
*Colonoscopy*
- **Colonoscopy** is used to visualize the large intestine for conditions such as polyps, cancer, or inflammatory bowel disease.
- There are no symptoms or signs (e.g., lower GI bleeding, chronic diarrhea) to suggest a need for colonoscopy in this acute postoperative setting.
*Gastrografin enema*
- A **Gastrografin enema** is a diagnostic and sometimes therapeutic study used to evaluate the colon and identify conditions like anastomotic leaks or obstructions, particularly in the context of recent surgery.
- The abdominal X-ray shows diffuse gas without air-fluid levels and the patient's symptoms are classic for an ileus, not a mechanical obstruction that would require a contrast study.
Small bowel resection and anastomosis US Medical PG Question 8: A 14-year-old boy is brought to the emergency department because of abdominal swelling and vomiting over the past 24 hours. He has generalized abdominal pain. He has no history of any serious illnesses and takes no medications. His temperature is 36.7°C (98.1°F), blood pressure is 115/70 mm/Hg, pulse is 88/min, and respirations are 16/min. Abdominal examination shows diffuse swelling with active bowel sounds. Mild generalized tenderness without guarding or rebound is noted. His leukocyte count is 8,000/mm3. An X-ray of the abdomen is shown. Intravenous fluids have been initiated. Which of the following is the most appropriate next step in management?
- A. Rectal tube
- B. IV antibiotics
- C. Endoscopy
- D. Close observation (Correct Answer)
- E. Colectomy
Small bowel resection and anastomosis Explanation: ***Close observation***
- This patient presents with signs of **partial or early bowel obstruction** (abdominal swelling, vomiting, diffuse pain) but remains **hemodynamically stable** with **no peritoneal signs** (no guarding or rebound tenderness), **normal vital signs**, and **normal leukocyte count**.
- The presence of **active bowel sounds** indicates the bowel is still viable and functional, suggesting this is not a complete obstruction with ischemia.
- **Initial management of bowel obstruction** in a stable patient without signs of perforation or strangulation is **conservative**: NPO status, NG tube decompression (if not already done), IV fluid resuscitation (already initiated), serial abdominal exams, and **close observation** to monitor for improvement or signs of deterioration.
- Many partial obstructions resolve with conservative management. Surgery is reserved for cases that fail to improve, develop peritoneal signs, or show evidence of bowel compromise.
- If diagnosis remains unclear or the patient worsens, **CT scan** would be the next imaging study, not endoscopy.
*Endoscopy*
- **Endoscopy is NOT indicated** for suspected mechanical small or large bowel obstruction in this age group and presentation.
- **Colonoscopy** with detorsion is used for **sigmoid volvulus** in elderly patients with a characteristic "coffee bean" sign on X-ray, not in adolescents with generalized obstruction.
- While **air or contrast enema under fluoroscopy** (not endoscopy) is used for **intussusception**, this condition typically affects infants and toddlers (peak age 6-36 months), not 14-year-olds.
- Performing endoscopy on an obstructed bowel carries risk of perforation and doesn't address the most likely anatomic locations of obstruction.
*Rectal tube*
- A **rectal tube** is used for **colonic decompression** in specific scenarios like sigmoid volvulus or Ogilvie syndrome (acute colonic pseudo-obstruction), typically in elderly patients.
- It provides no diagnostic information and is unlikely to relieve an obstruction in a 14-year-old, where small bowel obstruction or proximal large bowel pathology is more likely.
- This is not appropriate initial management without first establishing the location and nature of the obstruction.
*IV antibiotics*
- **Antibiotics are not indicated** as the initial next step in this stable patient without signs of infection or perforation.
- The patient is **afebrile**, has a **normal WBC count** (8,000/mm³), and has **no peritoneal signs** (no guarding or rebound).
- Antibiotics would be indicated if there were signs of **bowel ischemia, perforation, or peritonitis**, or if the patient was proceeding to surgery.
- Addressing the obstruction with conservative management is the priority.
*Colectomy*
- **Colectomy** is a major surgical intervention reserved for cases of **bowel necrosis, perforation, malignancy**, or when conservative/less invasive management fails.
- This is absolutely **not the initial management step** in a stable patient with suspected obstruction who has not yet been given a trial of conservative management.
- Surgery would only be considered after failed conservative management (24-48 hours) or if signs of peritonitis, ischemia, or complete obstruction with clinical deterioration develop.
Small bowel resection and anastomosis US Medical PG Question 9: One day after undergoing an open colectomy, a 65-year-old man with colon cancer experiences shivers. The procedure was originally scheduled to be done laparoscopically, but it was converted because of persistent bleeding. Besides the conversion, the operation was uneventful. Five years ago, he underwent renal transplantation because of cystic disease and has been taking prednisolone since then. He has a history of allergy to sulfonamides. He appears acutely ill. His temperature is 39.2°C (102.5°F), pulse is 120/min, respirations are 23/min, and blood pressure is 90/62 mm Hg. Abdominal examination shows a midline incision extending from the xiphisternum to the pubic symphysis. There is a 5-cm (2-in) area of purplish discoloration near the margin of the incision in the lower abdomen. Palpation of the abdomen produces severe pain and crackling sounds are heard. Laboratory studies show:
Hemoglobin 12.5 g/dL
Leukocyte count 18,600/mm3
Platelet count 228,000/mm3
Erythrocyte sedimentation rate 120 mm/h
Serum
Na+ 134 mEq/L
K+ 3.5 mEq/L
Cl- 98 mEq/L
HCO3- 22 mEq/L
Glucose 200 mg/dL
Urea nitrogen 60 mg/dL
Creatinine 3.2 mg/dL
Creatine kinase 750 U/L
Which of the following is the most appropriate next step in management?
- A. Surgical debridement (Correct Answer)
- B. Intravenous clindamycin therapy
- C. X-ray of the abdomen and pelvis
- D. Vacuum-assisted wound closure device
- E. CT scan of abdomen
Small bowel resection and anastomosis Explanation: ***Surgical debridement***
- The patient's presentation with **fever**, **tachycardia**, **hypotension**, **purplish discoloration**, **severe pain**, and **crepitus** (crackling sounds) near the incision after abdominal surgery is highly suggestive of **necrotizing fasciitis**.
- **Surgical debridement** is the most urgent and critical step to remove necrotic tissue, control the spread of infection, and improve outcomes in necrotizing soft tissue infections.
*Intravenous clindamycin therapy*
- While broad-spectrum antibiotics, including clindamycin, are essential in managing necrotizing fasciitis, they are **adjunctive to surgical debridement**, not a standalone primary treatment.
- Delaying surgery for antibiotic therapy alone would worsen the patient's prognosis and could lead to rapid progression of the infection.
*X-ray of the abdomen and pelvis*
- An X-ray might show subcutaneous **gas (crepitus)**, which is consistent with necrotizing fasciitis due to gas-producing bacteria.
- However, the clinical presentation is already highly indicative of the diagnosis, and waiting for imaging would **delay critical surgical intervention**.
*Vacuum-assisted wound closure device*
- **VAC therapy** is used for wound management to promote healing after debridement, by creating negative pressure.
- It is **not a primary treatment** for an active, spreading necrotizing infection and should only be considered after adequate surgical debridement has been performed.
*CT scan of abdomen*
- A CT scan can confirm the presence of **gas in the soft tissues** and assess the extent of the infection, providing valuable information.
- However, like X-rays, obtaining a CT scan would **delay immediate surgical intervention**, which is paramount given the rapid progression of necrotizing fasciitis.
Small bowel resection and anastomosis US Medical PG Question 10: A 75-year-old man is brought to the emergency department after 2 days of severe diffuse abdominal pain, nausea, vomiting, and lack of bowel movements, which has led him to stop eating. He has a history of type-2 diabetes mellitus, hypertension, and chronic obstructive pulmonary disease. Upon admission, his vital signs are within normal limits and physical examination shows diffuse abdominal tenderness, distention, lack of bowel sounds, and an empty rectal ampulla. After initial fluid therapy and correction of moderate hypokalemia, the patient's condition shows mild improvement. His abdominal plain film is taken and shown. Which of the following is the most appropriate concomitant approach?
- A. Exploratory surgery
- B. Initiate pain management with morphine
- C. Initiate intravenous metoclopramide
- D. Gastrografin enema
- E. Nasogastric decompression (Correct Answer)
Small bowel resection and anastomosis Explanation: ***Nasogastric decompression***
- The patient exhibits symptoms consistent with **bowel obstruction** (diffuse abdominal pain, distention, absent bowel sounds, empty rectal ampulla), which can lead to significant fluid and gas accumulation. **Nasogastric decompression** is crucial to relieve pressure, prevent aspiration, and stabilize the patient.
- This intervention helps manage symptoms, reduces the risk of complications, and provides time for further diagnostic workup while addressing fluid and electrolyte imbalances.
*Exploratory surgery*
- While surgery may be indicated for complete bowel obstruction, it is usually reserved for cases that fail conservative management or show signs of **strangulation** or **perforation**.
- Without evidence of these acute complications and given the patient's mild improvement after initial therapy, immediate surgery is not the most appropriate first step.
*Initiate pain management with morphine*
- While pain management is important, **opioids** like morphine can actually **reduce bowel motility** and worsen a bowel obstruction.
- Addressing the underlying obstruction through decompression should be prioritized before initiating pain medication that could exacerbate the condition.
*Initiate intravenous metoclopramide*
- **Metoclopramide** is a **prokinetic agent** that increases gastrointestinal motility.
- In a suspected bowel obstruction, stimulating motility can increase intraluminal pressure and potentially worsen the condition or increase the risk of perforation, making it contraindicated.
*Gastrografin enema*
- A **Gastrografin enema** is typically used to diagnose and sometimes treat **distal colonic obstructions**, or as a therapeutic trial for **meconium ileus** in infants.
- Given the diffuse abdominal pain and an empty rectal ampulla suggesting a more proximal or severe obstruction, an enema may not be appropriate and could even be dangerous if there's a risk of perforation.
More Small bowel resection and anastomosis US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.