Inflammatory bowel disease surgical management US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Inflammatory bowel disease surgical management. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Inflammatory bowel disease surgical management US Medical PG Question 1: A 22-year-old woman comes to the physician because of abdominal pain and diarrhea for 2 months. The pain is intermittent, colicky and localized to her right lower quadrant. She has anorexia and fears eating due to the pain. She has lost 4 kg (8.8 lb) during this time. She has no history of a serious illness and takes no medications. Her temperature is 37.8°C (100.0°F), blood pressure 125/65 mm Hg, pulse 75/min, and respirations 14/min. An abdominal examination shows mild tenderness of the right lower quadrant on deep palpation without guarding. Colonoscopy shows small aphthous-like ulcers in the right colon and terminal ileum. Biopsy from the terminal ileum shows noncaseating granulomas in all layers of the bowel wall. Which of the following is the most appropriate pharmacotherapy at this time?
- A. Budesonide (Correct Answer)
- B. Azathioprine
- C. Ciprofloxacin
- D. Metronidazole
- E. Rectal mesalamine
Inflammatory bowel disease surgical management Explanation: ***Budesonide***
- This patient presents with symptoms and findings (RLQ pain, aphthous ulcers, noncaseating granulomas in the terminal ileum) consistent with **Crohn's disease** isolated to the **ileum and right colon**.
- **Budesonide** is a glucocorticoid with high first-pass metabolism, making it effective for localized ileal and right colonic Crohn's disease with fewer systemic side effects than prednisone.
*Azathioprine*
- **Azathioprine** is an immunomodulator used for maintaining remission in moderate to severe Crohn's disease, not typically for acute exacerbations as first-line monotherapy.
- Its onset of action is slow (several weeks to months), making it unsuitable for immediate symptom control.
*Ciprofloxacin*
- **Ciprofloxacin** is an antibiotic mainly used when there is concern for bacterial overgrowth, abscess, or perianal disease in Crohn's, none of which are explicitly indicated here.
- There is no evidence suggesting a primary bacterial infection as the cause of her current symptoms.
*Metronidazole*
- **Metronidazole** is an antibiotic often used for Crohn's disease with perianal involvement or fistulas, and sometimes for active colonic disease, but less effective for ileal involvement.
- Like ciprofloxacin, it's not the primary treatment for uncomplicated flare of ileocolonic Crohn's.
*Rectal mesalamine*
- **Rectal mesalamine** is an aminosalicylate primarily used for mild to moderate **ulcerative colitis**, particularly proctitis or left-sided colitis due to its topical action.
- It is ineffective for Crohn's disease involving the terminal ileum and right colon, as it would not reach this location in sufficient concentration.
Inflammatory bowel disease surgical management US Medical PG Question 2: A 27-year-old female has a history of periodic bloody diarrhea over several years. Colonoscopy shows sigmoid colon inflammation, and the patient complains of joint pain in her knees and ankles. You suspect inflammatory bowel disease. Which of the following would suggest a diagnosis of Crohn disease:
- A. Jaundice
- B. Mucosal and submucosal ulcerations
- C. Perianal fistula (Correct Answer)
- D. Loss of large bowel haustra
- E. Left lower quadrant pain
Inflammatory bowel disease surgical management Explanation: ***Perianal fistula***
- The presence of a **perianal fistula** is highly characteristic of **Crohn disease** due to its **transmural inflammation**, which can extend through the bowel wall and form tracts to the skin.
- While other inflammatory bowel disease (IBD) symptoms like bloody diarrhea and joint pain are present, a fistula specifically points towards Crohn disease rather than ulcerative colitis.
*Jaundice*
- **Jaundice** is not a typical manifestation of Crohn disease itself, though it can occur as a complication if there is associated **primary sclerosing cholangitis (PSC)**, which is more commonly linked with **ulcerative colitis**.
- It would suggest a primary liver issue or biliary obstruction, rather than directly supporting a diagnosis of Crohn disease.
*Mucosal and submucosal ulcerations*
- While **ulcerations** are a feature of both ulcerative colitis and Crohn disease, the description of **mucosal and submucosal ulcerations** is not specific enough to differentiate between them.
- In Crohn disease, ulcers tend to be **scattered** and **deep ("cobblestoning")**, potentially extending transmurally, whereas in ulcerative colitis, they are typically more **superficial** and **continuous**.
*Loss of large bowel haustra*
- **Loss of haustra**, also known as **"lead pipe" appearance**, is a characteristic finding in chronic **ulcerative colitis** due to continuous inflammation and fibrosis, leading to a straightened appearance of the colon.
- This finding is less typical for Crohn disease, which often has **skip lesions** and can involve any part of the gastrointestinal tract.
*Left lower quadrant pain*
- **Left lower quadrant pain** can be associated with inflammation in the **descending or sigmoid colon**, which can occur in both Crohn disease and ulcerative colitis.
- Therefore, this symptom is **non-specific** and does not help to differentiate between the two conditions.
Inflammatory bowel disease surgical management US Medical PG Question 3: An 18-year-old man presents with bloody diarrhea and weight loss. He undergoes endoscopic biopsy which shows pseudopolyps. Biopsies taken during the endoscopy show inflammation only involving the mucosa and submucosa. He is diagnosed with an inflammatory bowel disease. Which of the following characteristics was most likely present?
- A. Cobblestone mucosa
- B. Skip lesions
- C. Fistulas and strictures
- D. Noncaseating granuloma
- E. Rectal involvement (Correct Answer)
Inflammatory bowel disease surgical management Explanation: **_Rectal involvement_**
- The description of **bloody diarrhea** and **pseudopolyps** on endoscopy, along with inflammation limited to the **mucosa and submucosa**, is highly characteristic of **ulcerative colitis (UC)**. UC invariably involves the rectum and extends proximally in a continuous fashion.
- The presence of **pseudopolyps** is common in UC due to cycles of mucosal ulceration and regeneration.
*Cobblestone mucosa*
- **Cobblestone mucosa** is a classic endoscopic finding in **Crohn's disease**, resulting from deep ulcerations interspersed with islands of edematous, non-ulcerated mucosa.
- This feature points to a transmural pattern of inflammation, which is inconsistent with the superficial inflammation confined to the **mucosa and submucosa** described.
*Skip lesions*
- **Skip lesions** refer to discontinuous areas of inflammation separated by healthy tissue, a hallmark feature of **Crohn's disease**.
- **Ulcerative colitis** (implied by the superficial inflammation) is characterized by continuous inflammation extending proximally from the rectum without skipped areas.
*Fistulas and strictures*
- **Fistulas** (abnormal connections between organs or to the skin) and **strictures** (narrowing of the intestinal lumen) are complications typically associated with **Crohn's disease**, due to its **transmural inflammation**.
- These are rare in **ulcerative colitis**, which primarily affects the superficial layers of the colon.
*Noncaseating granuloma*
- The presence of **noncaseating granulomas** on biopsy is a key histological feature distinguishing **Crohn's disease** from ulcerative colitis.
- The inflammation described as restricted to the **mucosa and submucosa** makes granulomas less likely, as they often imply a transmural process.
Inflammatory bowel disease surgical management US Medical PG Question 4: A 64-year-old woman has progressively worsening abdominal pain 5 hours after an open valve replacement with cardiopulmonary bypass. The pain is crampy and associated with an urge to defecate. The patient reports having had 2 bloody bowel movements in the last hour. Her operation was complicated by significant intraoperative blood loss, which prolonged the operation and necessitated 2 transfusions of red blood cells. She has hypercholesterolemia and type 2 diabetes mellitus. The patient received prophylactic perioperative antibiotics and opioid pain management during recovery. Her temperature is 37.9°C (98.9°F), pulse is 95/min, and blood pressure is 115/69 mm Hg. Examination shows a soft abdomen with mild tenderness to palpation in the left quadrants but no rebound tenderness or guarding. Bowel sounds are decreased. Rectal examination shows blood on the examining finger. Which of the following is the most likely underlying cause of this patient's symptoms?
- A. Embolization of superior mesenteric artery
- B. Atherosclerotic narrowing of the intestinal vessels
- C. Small outpouchings in the sigmoid wall
- D. Infection with Clostridioides difficile
- E. Decreased blood flow to the splenic flexure (Correct Answer)
Inflammatory bowel disease surgical management Explanation: ***Decreased blood flow to the splenic flexure***
- This patient's symptoms are highly suggestive of **ischemic colitis**, which often affects the **splenic flexure** due to its "watershed" area vulnerability. **Cardiopulmonary bypass** and significant **intraoperative blood loss** (leading to hypotension and hypoperfusion) are major risk factors for this condition.
- The presentation with **crampy abdominal pain**, **urgent defecation**, and **bloody bowel movements** shortly after cardiac surgery points to colonic ischemia.
*Embolization of superior mesenteric artery*
- While an acute **SMA embolism** could cause severe abdominal pain and bloody stools, it typically presents with **more diffuse and severe abdominal tenderness**, often with marked tenderness disproportionate to examination findings early on, and rapid progression to peritonitis.
- The patient's history of valvular disease and hypercholesterolemia increases the risk of embolization, but the **mild tenderness confined to left quadrants** and decreased bowel sounds are less typical of an acute SMA occlusion.
*Atherosclerotic narrowing of the intestinal vessels*
- This describes **chronic mesenteric ischemia**, which typically causes **postprandial abdominal pain** (intestinal angina) and weight loss, not acute abdominal pain and bloody diarrhea in the immediate postoperative period.
- While the patient has risk factors for atherosclerosis (hypercholesterolemia, diabetes), the acute onset of symptoms following cardiac surgery points to an acute ischemic event rather than chronic narrowing.
*Small outpouchings in the sigmoid wall*
- This refers to **diverticulitis** or **diverticular bleeding**. While diverticular bleeding can cause painless or painful bleeding, and diverticulitis can cause abdominal pain, the acute onset post-cardiac surgery in the setting of hypoperfusion makes ischemic colitis a more likely diagnosis.
- Diverticulitis typically presents with **localized left lower quadrant pain**, fever, and leukocytosis, but the systemic context of recent cardiac surgery and hypoperfusion strongly favors ischemia.
*Infection with Clostridioides difficile*
- **_Clostridioides difficile_ infection** typically causes **watery diarrhea**, often after antibiotic use, and usually takes several days to develop symptoms after exposure or antibiotic initiation.
- Although the patient received perioperative antibiotics, the onset of symptoms within hours of surgery and the presence of **frank bloody stools** are less characteristic of _C. difficile_ infection, which is more commonly associated with non-bloody diarrhea.
Inflammatory bowel disease surgical management US Medical PG Question 5: A 31-year-old woman comes to the emergency department because of a 4-day history of fever and diarrhea. She has abdominal cramps and frequent bowel movements of small quantities of stool with blood and mucus. She has had multiple similar episodes over the past 8 months. Her temperature is 38.1°C (100.6°F), pulse is 75/min, and blood pressure is 130/80 mm Hg. Bowel sounds are normal. The abdomen is soft. There is tenderness to palpation in the left lower quadrant with guarding and no rebound. She receives appropriate treatment and recovers. Two weeks later, colonoscopy shows polypoid growths flanked by linear ulcers. A colonic biopsy specimen shows mucosal edema with distorted crypts and inflammatory cells in the lamina propria. Which of the following is the most appropriate recommendation for this patient?
- A. Obtain genetic studies now
- B. Obtain barium follow-through radiography in 1 year
- C. Obtain glutamate dehydrogenase antigen immunoassay now
- D. Start annual magnetic resonance cholangiopancreatography screening in 10 years
- E. Start annual colonoscopy starting in 8 years (Correct Answer)
Inflammatory bowel disease surgical management Explanation: ***Start annual colonoscopy starting in 8 years***
- The patient's presentation with bloody diarrhea, abdominal cramps, and repetitive episodes is consistent with <b>inflammatory bowel disease (IBD)</b>, specifically likely <b>ulcerative colitis</b> given the left lower quadrant tenderness and colonic biopsy findings (distorted crypts, inflammatory cells in lamina propria).
- Patients with IBD, particularly ulcerative colitis affecting a significant portion of the colon and diagnosed at a younger age, are at increased risk for <b>colorectal cancer</b>. Annual colonoscopy screening is recommended 8–10 years after diagnosis for early detection and prevention.
*Obtain genetic studies now*
- While genetic factors play a role in IBD susceptibility, <b>genetic studies are not routinely indicated for diagnosis or management</b> of inflammatory bowel disease, nor do they guide current screening recommendations for colorectal cancer in IBD patients.
- Genetic studies would not provide immediate clinical benefit for this patient's acute symptoms or long-term management plan regarding cancer surveillance.
*Obtain barium follow-through radiography in 1 year*
- <b>Barium follow-through radiography</b> is primarily used to evaluate the small intestine, often in suspected Crohn's disease. This patient's symptoms and colonoscopy findings point towards colonic involvement, making this less appropriate.
- Furthermore, this imaging modality uses <b>ionizing radiation</b> and is less sensitive for detecting mucosal changes indicative of dysplasia or early cancer compared to colonoscopy.
*Obtain glutamate dehydrogenase antigen immunoassay now*
- <b>Glutamate dehydrogenase antigen immunoassay</b> is a test for <b><i>Clostridioides difficile</i> infection</b>. While C. difficile can cause severe diarrhea and colitis, the patient's history of recurrent episodes over 8 months and the specific colonoscopy findings (polypoid growths, linear ulcers, distorted crypts) are more characteristic of IBD.
- Although C. difficile infection can exacerbate IBD, it does not explain the chronic, recurrent nature of her illness or the long-term cancer surveillance needs.
*Start annual magnetic resonance cholangiopancreatography screening in 10 years*
- <b>MRCP screening</b> is used to monitor for <b>primary sclerosing cholangitis (PSC)</b>, a condition associated with IBD, particularly ulcerative colitis. However, PSC screening is performed <b>when clinically indicated</b> (e.g., elevated alkaline phosphatase, cholestatic symptoms), not as routine scheduled surveillance.
- This patient has no clinical features suggesting PSC at present, and there is no guideline recommending routine MRCP screening at a predetermined time interval for all IBD patients.
Inflammatory bowel disease surgical management US Medical PG Question 6: A 56-year-old woman is one week status post abdominal hysterectomy when she develops a fever of 101.4°F (38.6°C). Her past medical history is significant for type II diabetes mellitus and a prior history of alcohol abuse. The operative report and intraoperative cystoscopy indicate that the surgery was uncomplicated. The nurse reports that since the surgery, the patient has also complained of worsening lower abdominal pain. She has given the patient the appropriate pain medications with little improvement. The patient has tolerated an oral diet well and denies nausea, vomiting, or abdominal distension. Her blood pressure is 110/62 mmHg, pulse is 122/min, and respirations are 14/min. Since being given 1000 mL of intravenous fluids yesterday, the patient has excreted 800 mL of urine. On physical exam, she is uncomfortable, shivering, and sweating. The surgical site is intact, but the surrounding skin appears red. No drainage is appreciated. The abdominal examination reveals tenderness to palpation and hypoactive bowel sounds. Labs and a clean catch urine specimen are obtained as shown below:
Leukocyte count and differential:
Leukocyte count: 18,000/mm^3
Segmented neutrophils: 80%
Bands: 10%
Eosinophils: 1%
Basophils: < 1%
Lymphocytes: 5%
Monocytes: 4%
Platelet count: 300,000/mm^3
Hemoglobin: 12.5 g/dL
Hematocrit: 42%
Urine:
Epithelial cells: 15/hpf
Glucose: positive
RBC: 1/hpf
WBC: 2/hpf
Bacteria: 50 cfu/mL
Ketones: none
Nitrites: negative
Leukocyte esterase: negative
Which of the following is most likely the cause of this patient’s symptoms?
- A. Surgical error
- B. Post-operative ileus
- C. Wound infection (Correct Answer)
- D. Alcohol withdrawal
- E. Urinary tract infection
Inflammatory bowel disease surgical management Explanation: ***Wound infection***
- The patient presents with **fever**, worsening **lower abdominal pain**, **tachycardia**, and **local signs of inflammation** (redness around the surgical site, tenderness) one week post-hysterectomy, with a **leukocytosis and left shift** (elevated neutrophils and bands). These findings are highly characteristic of a common **post-surgical wound infection**.
- The lack of significant drainage initially does not rule out infection, and the symptoms are localized to the surgical area.
*Surgical error*
- The operative report and intraoperative cystoscopy indicated the surgery was **uncomplicated**, making an immediate post-operative surgical error less likely to be the primary cause of these symptoms.
- While complications can arise later, the current presentation points more directly to an infectious process rather than an unnoted immediate surgical complication.
*Post-operative ileus*
- Although bowel sounds are hypoactive, the patient is **tolerating an oral diet well** and denies nausea, vomiting, or abdominal distension, which are key symptoms of a clinically significant ileus.
- Her primary complaint is localized pain and systemic signs of infection, rather than generalized abdominal distension and inability to pass flatus or stool.
*Alcohol withdrawal*
- While the patient has a history of alcohol abuse, the primary symptoms (fever, localized abdominal pain, redness around the incision, leukocytosis) are more indicative of an **infectious process** than alcohol withdrawal.
- Alcohol withdrawal typically presents with tremors, agitation, hallucinations, and autonomic instability, and while some overlap (tachycardia) exists, the overall clinical picture doesn't fit.
*Urinary tract infection*
- The urine analysis shows **negative nitrites and leukocyte esterase**, with only 2 WBC/hpf, which makes a **urinary tract infection (UTI) highly unlikely** despite the presence of some bacteria (50 cfu/mL, which is often considered contamination in a clean catch).
- The patient's symptoms are also predominantly localized to the surgical wound area rather than dysuria, frequency, or urgency.
Inflammatory bowel disease surgical management US Medical PG Question 7: A 53 year-old woman with history of ulcerative colitis presents to the emergency department with a severe flare. The patient reports numerous bloody loose stools, and has been febrile for two days. Vital signs are: T 101.9 HR 98 BP 121/86 RR 17 Sat 100%. Abdominal exam is notable for markedly distended abdomen with tympani and tenderness to palpation without guarding or rebound. KUB is shown in figure A. CT scan shows markedly dilated descending and sigmoid colon with no perforations. What is the next best step in management for this patient?
- A. IV Ondansetron
- B. Rectal 5-ASA
- C. IV hydrocortisone (Correct Answer)
- D. Oral prednisone
- E. IV Metoclopramide
Inflammatory bowel disease surgical management Explanation: ***IV hydrocortisone***
- This patient has **toxic megacolon**, a life-threatening complication of ulcerative colitis requiring aggressive medical management alongside surgical consultation.
- High-dose **IV corticosteroids** (hydrocortisone 100mg IV q6-8h or methylprednisolone) are first-line medical therapy to rapidly suppress severe colonic inflammation.
- Medical management includes IV steroids, broad-spectrum antibiotics, bowel rest (NPO), IV fluid resuscitation, and nasogastric decompression while preparing for potential **emergent colectomy** if medical therapy fails within 24-72 hours.
- IV route ensures **rapid systemic delivery** in a critically ill patient with impaired GI absorption.
*IV Ondansetron*
- An antiemetic that treats nausea/vomiting symptoms but does **not address the underlying inflammatory process** or systemic toxicity.
- Does not modify disease course or reduce the risk of **perforation** in toxic megacolon.
*Rectal 5-ASA*
- **Contraindicated in toxic megacolon** due to risk of perforation with rectal manipulation and increased intraluminal pressure.
- Local therapy is ineffective for **systemic toxicity** (fever, hemodynamic instability) and extensive colonic involvement.
- Only appropriate for mild-to-moderate distal ulcerative colitis, not severe fulminant disease.
*Oral prednisone*
- Inadequate for **acute severe/fulminant colitis** requiring hospitalization due to delayed absorption and lower bioavailability.
- IV corticosteroids provide **immediate systemic effect** necessary for life-threatening toxic megacolon.
- Oral route inappropriate in patient with severe GI symptoms and potential ileus.
*IV Metoclopramide*
- A prokinetic agent that is **absolutely contraindicated in toxic megacolon** as it increases colonic motility and can precipitate perforation.
- Does not address the **inflammatory pathophysiology** of ulcerative colitis.
- Used for gastroparesis and nausea, not for managing inflammatory bowel disease complications.
Inflammatory bowel disease surgical management US Medical PG Question 8: A 31 year-old-man presents to an urgent care clinic with symptoms of lower abdominal pain, bloating, bloody diarrhea, and fullness, all of which have become more frequent over the last 3 months. Rectal examination reveals a small amount of bright red blood. His vital signs include: temperature 36.7°C (98.0°F), blood pressure 126/74 mm Hg, heart rate 74/min, and respiratory rate 14/min. Colonoscopy is performed, showing extensive mucosal erythema, induration, and pseudopolyps extending from the rectum to the splenic flexure. Given the following options, what is the most appropriate treatment to induce remission in this patient?
- A. Azathioprine
- B. Mesalamine
- C. Total proctocolectomy
- D. Sulfasalazine
- E. Systemic corticosteroids (Correct Answer)
Inflammatory bowel disease surgical management Explanation: ***Systemic corticosteroids***
- The patient presents with classic symptoms of an acute **ulcerative colitis flare**, including bloody diarrhea, abdominal pain, and colonoscopy findings of extensive inflammation from the rectum to the splenic flexure (consistent with **left-sided colitis**).
- **Systemic corticosteroids** such as prednisone or methylprednisolone are the **most appropriate treatment to induce remission** during active flares of moderate to severe ulcerative colitis due to their potent **anti-inflammatory effects** and rapid onset of action.
- This patient has moderate to severe disease based on extent and symptom severity, warranting systemic corticosteroids rather than topical or aminosalicylate therapy alone.
*Azathioprine*
- **Azathioprine** is an **immunomodulator** used for maintaining remission in inflammatory bowel disease, not for acute flare treatment.
- Its onset of action is slow (weeks to months), making it unsuitable for immediate symptom control in an acute flare.
*Mesalamine*
- **Mesalamine** (an aminosalicylate) is a **first-line therapy** for inducing and maintaining remission in **mild to moderate** ulcerative colitis, particularly for proctitis or left-sided colitis.
- However, for extensive disease with significant symptoms as seen in this patient, **systemic corticosteroids** are preferred due to greater potency and more rapid induction of remission in moderate to severe flares.
*Total proctocolectomy*
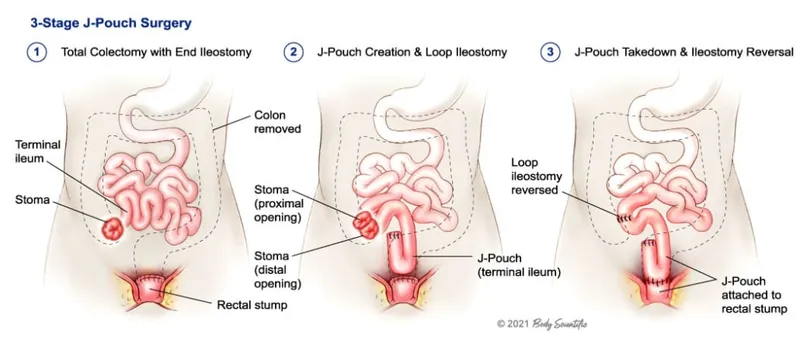
- **Total proctocolectomy** is a surgical procedure that provides a **definitive cure** for ulcerative colitis by removing the entire colon and rectum.
- However, surgery is reserved for cases of **refractory disease** (failure of medical therapy), severe complications (e.g., toxic megacolon, perforation, severe hemorrhage), or high risk of dysplasia/cancer.
- This patient is presenting with an acute flare and should be managed medically first; surgery is not the initial treatment approach.
*Sulfasalazine*
- **Sulfasalazine** is an aminosalicylate similar to mesalamine, used for inducing and maintaining remission in mild to moderate ulcerative colitis.
- While effective for mild disease, systemic corticosteroids are preferred for moderate to severe acute flares due to their stronger and more rapid anti-inflammatory action when the disease is extensive and symptomatic.
Inflammatory bowel disease surgical management US Medical PG Question 9: Three hours after undergoing open proctocolectomy for ulcerative colitis, a 42-year-old male complains of abdominal pain. The pain is localized to the periumbilical and hypogastric regions. A total of 20 mL of urine has drained from his urinary catheter since the end of the procedure. Temperature is 37.2°C (98.9°F), pulse is 92/min, respirations are 12/min, and blood pressure is 110/72 mm Hg. Pulse oximetry on room air shows an oxygen saturation of 99%. Physical examination shows a 20 cm vertical midline incision and an ileostomy in the right lower quadrant. There is no fluid drainage from the surgical wounds. The urinary catheter flushes easily and is without obstruction. Cardiopulmonary examination shows no abnormalities. Serum studies show a blood urea nitrogen of 30 mg/dL and a creatinine of 1.3 mg/dL. Which of the following is the most appropriate next step in management?
- A. Administer tamsulosin
- B. Administer intravenous furosemide
- C. Obtain an abdominal CT
- D. Start ciprofloxacin
- E. Administer intravenous fluids (Correct Answer)
Inflammatory bowel disease surgical management Explanation: ***Administer intravenous fluids***
- The patient's **oliguria** (20 mL urine over 3 hours, ~7 mL/hour) post-surgery, elevated **BUN (30 mg/dL)**, and **creatinine (1.3 mg/dL)** with a **BUN:Cr ratio >20:1** suggest **prerenal acute kidney injury** due to **hypovolemia**.
- Post-operative fluid losses from **third-spacing**, blood loss, and insensible losses commonly cause hypovolemia after major abdominal surgery.
- **Intravenous fluids** are the most appropriate initial step to restore intravascular volume and improve renal perfusion.
*Administer tamsulosin*
- **Tamsulosin** is an alpha-blocker used to relax smooth muscle in the prostate and bladder neck, primarily for **urinary retention** due to benign prostatic hyperplasia.
- This patient's oliguria is due to **prerenal azotemia** from hypovolemia, not prostatic obstruction, and the catheter flushes easily without obstruction.
*Administer intravenous furosemide*
- **Furosemide** is a loop diuretic that increases urine output, but administering it in the context of **prerenal acute kidney injury** can worsen hypovolemia and further compromise renal function.
- Diuretics are generally contraindicated in oliguria due to hypovolemia and should only be considered after volume resuscitation.
*Obtain an abdominal CT*
- While an abdominal CT can diagnose surgical complications, there are no immediate signs of a surgical emergency like **anastomotic leak** or **bowel obstruction**.
- Addressing the likely **hypovolemia** is more urgent and should precede further imaging in this scenario.
*Start ciprofloxacin*
- The patient does not show signs of infection, such as fever or localized signs of bacterial peritonitis, making **antibiotics** like ciprofloxacin inappropriate as the initial management step.
- The elevated BUN and creatinine are more indicative of volume depletion than infection.
Inflammatory bowel disease surgical management US Medical PG Question 10: A 45-year-old man is brought to the emergency department because of severe abdominal pain for the past 2 hours. He has a 2-year history of burning epigastric pain that gets worse with meals. His pulse is 120/min, respirations are 22/min, and blood pressure is 60/40 mm Hg. Despite appropriate lifesaving measures, he dies. At autopsy, examination shows erosion of the right gastric artery. Perforation of an ulcer in which of the following locations most likely caused this patient's findings?
- A. Anterior duodenum
- B. Posterior duodenum
- C. Lesser curvature of the stomach (Correct Answer)
- D. Greater curvature of the stomach
- E. Fundus of the stomach
Inflammatory bowel disease surgical management Explanation: ***Lesser curvature of the stomach***
- Erosion of the **right gastric artery** by a gastric ulcer is characteristic of an ulcer located on the **lesser curvature of the stomach**.
- Ulcers in this location can erode into adjacent blood vessels, leading to **severe hemorrhage** as evidenced by the patient's **hypotension** and subsequent death.
*Anterior duodenum*
- Ulcers in the **anterior duodenum** typically present with **perforation into the peritoneal cavity**, leading to generalized peritonitis, not primarily hemorrhage from a major artery.
- While bleeding can occur, it's usually from smaller duodenal arteries and less commonly involves large arteries like the right gastric artery.
*Posterior duodenum*
- Ulcers in the **posterior duodenum** are known to erode into the **gastroduodenal artery**, leading to massive upper gastrointestinal bleeding.
- This is a distinct arterial involvement compared to the erosion of the right gastric artery.
*Greater curvature of the stomach*
- Ulcers on the **greater curvature of the stomach** are less common and often associated with malignancy.
- If they bleed, it would typically involve branches of the **gastroepiploic arteries**, not the right gastric artery.
*Fundus of the stomach*
- Ulcers in the **fundus** are rare.
- If a vessel were involved, it would typically be a short gastric artery, not the right gastric artery which courses along the lesser curvature.
More Inflammatory bowel disease surgical management US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.