Gastric surgery procedures US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Gastric surgery procedures. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Gastric surgery procedures US Medical PG Question 1: A 54-year-old man comes to the physician because of generalized fatigue and numbness of his legs and toes for 5 months. He has hypertension and hypercholesterolemia. He underwent a partial gastrectomy for peptic ulcer disease 15 years ago. Current medications include amlodipine and atorvastatin. He is a painter. His temperature is 37°C (98.6°F), pulse is 101/min, respirations are 17/min, and blood pressure is 122/82 mm Hg. Examination shows conjunctival pallor and glossitis. Sensation to vibration and position is absent over the lower extremities. He has a broad-based gait. The patient sways when he stands with his feet together and closes his eyes. His hemoglobin concentration is 10.1 g/dL, leukocyte count is 4300/mm3, and platelet count is 110,000/mm3. Which of the following laboratory findings is most likely to be seen in this patient?
- A. Oligoclonal bands in cerebrospinal fluid
- B. Elevated methylmalonic acid levels (Correct Answer)
- C. Positive rapid plasma reagin test
- D. Decreased serum iron levels
- E. Basophilic stippling on peripheral smear
Gastric surgery procedures Explanation: ***Elevated methylmalonic acid levels***
- The patient's history of **partial gastrectomy**, followed by **fatigue**, **neurological symptoms** (numbness, gait instability, absent vibration/position sensation, positive Romberg sign), **conjunctival pallor**, **glossitis**, and **pancytopenia** (anemia, leukopenia, thrombocytopenia) are all classic signs of **vitamin B12 deficiency**.
- **Methylmalonic acid (MMA)** and **homocysteine** are biochemical markers that accumulate when vitamin B12 is deficient, as vitamin B12 acts as a cofactor in their metabolism. Elevated MMA is a more specific indicator of vitamin B12 deficiency than homocysteine.
*Oligoclonal bands in cerebrospinal fluid*
- **Oligoclonal bands** in the CSF are characteristic of **multiple sclerosis** and other inflammatory disorders of the central nervous system, which do not align with this patient's clinical presentation, particularly the history of gastrectomy and pancytopenia.
- While the patient has neurological symptoms, they are more consistent with a metabolic neuropathy secondary to vitamin B12 deficiency rather than demyelinating disease.
*Positive rapid plasma reagin test*
- A **positive rapid plasma reagin (RPR) test** indicates **syphilis**, which can cause neurological symptoms (neurosyphilis).
- However, the patient's **pancytopenia**, **glossitis**, and history of **gastrectomy** are not typical features of syphilis.
*Decreased serum iron levels*
- **Decreased serum iron levels** would suggest **iron deficiency anemia**. While iron deficiency can cause fatigue and pallor, it typically does not lead to the specific neurological symptoms (demyelinating neuropathy) seen here or pancytopenia.
- The patient's **glossitis** can be seen in both iron and B12 deficiency, but the neurological signs point specifically to B12 deficiency.
*Basophilic stippling on peripheral smear*
- **Basophilic stippling** on a peripheral smear is a classic finding in **lead poisoning** or other conditions causing ribosomal precipitation, such as **thalassemia** or **sideroblastic anemia**.
- While lead poisoning can cause neuropathy and anemia, it would not typically present with the specific history of gastrectomy or the pronounced pancytopenia seen in this patient.
Gastric surgery procedures US Medical PG Question 2: A 2-month-old girl is brought to the physician for a well-child examination. She was born at 32 weeks' gestation and weighed 1616 g (3 lb 9 oz); she currently weighs 2466 g (5 lb 7 oz). She is exclusively breastfed and receives vitamin D supplementation. Physical examination shows no abnormalities apart from low height and weight. This patient is at increased risk for which of the following complications?
- A. Iron deficiency anemia (Correct Answer)
- B. Hemorrhage
- C. Scurvy
- D. Subacute combined degeneration
- E. Intussusception
Gastric surgery procedures Explanation: ***Iron deficiency anemia***
- Preterm infants have **lower iron stores** at birth due to reduced placental transfer in the third trimester.
- Their rapid growth rate and exclusive breastfeeding (breast milk has low iron content) further increase their risk of **iron deficiency anemia**.
*Hemorrhage*
- While preterm infants are at higher risk for certain hemorrhages (e.g., intraventricular hemorrhage), this typically occurs in the **immediate neonatal period** and risk significantly decreases by 2 months of age.
- Hemorrhage is not a common long-term complication unique to a 2-month-old preterm infant without additional risk factors.
*Scurvy*
- Scurvy is caused by **vitamin C deficiency**, which is typically not a concern in breastfed infants as breast milk provides adequate vitamin C.
- The primary deficiency risk addressed by supplementation in breastfed infants is vitamin D, not vitamin C.
*Subacute combined degeneration*
- This condition is caused by **vitamin B12 deficiency**, leading to demyelination of the spinal cord.
- While possible in infants of vegan mothers, it is unlikely in a breastfed infant without specific dietary restrictions in the mother.
*Intussusception*
- Intussusception is a condition where one segment of the intestine telescopes into another, usually occurring between **3 months and 3 years of age**.
- It is not specifically linked to prematurity or low birth weight as an increased long-term risk.
Gastric surgery procedures US Medical PG Question 3: A 22-year-old primigravid woman comes to the physician for her initial prenatal visit at 12 weeks' gestation. She has had generalized fatigue and shortness of breath over the past 2 months. She has also had a tingling sensation in her toes for the past month. Three years ago, she was treated for gonorrhea. She follows a strict vegan diet since the age of 13 years. Her temperature is 37°C (98.6°F), pulse is 111/min, and blood pressure is 122/80 mm Hg. Examination shows pale conjunctivae and a shiny tongue. Muscle tone and strength is normal. Deep tendon reflexes are 2+ bilaterally. Sensation to vibration and position is decreased over the upper and lower extremities. When asked to stand, hold her arms in front of her, and close her eyes, she loses her balance and takes a step backward. Which of the following is most likely to have prevented this patient's condition?
- A. Calcium supplementation
- B. Thyroxine supplementation
- C. Vitamin B12 supplementation (Correct Answer)
- D. Iron supplementation
- E. Penicillin G therapy
Gastric surgery procedures Explanation: ***Vitamin B12 supplementation***
- The patient's symptoms, including **fatigue**, **shortness of breath**, **tingling sensation in toes** (paresthesias), **pale conjunctivae**, **shiny tongue** (glossitis), decreased **vibration and position sensation**, and **ataxia** (losing balance with eyes closed), are classic signs of **vitamin B12 deficiency**.
- A **strict vegan diet** since age 13 significantly increases the risk of vitamin B12 deficiency, as B12 is primarily found in animal products. Supplementation would have prevented these symptoms.
*Calcium supplementation*
- **Calcium** is essential for bone health, muscle function, and nerve transmission, but deficiency typically causes symptoms like **osteoporosis**, **muscle cramps**, or **tetany**, not the specific neurological and hematological signs seen here.
- While important in pregnancy, calcium deficiency does not explain the patient's array of symptoms, especially the neurological presentation.
*Thyroxine supplementation*
- **Thyroxine** (thyroid hormone) deficiency (hypothyroidism) can cause fatigue, but symptoms typically also include **weight gain**, constipation, cold intolerance, and dry skin, which are not mentioned.
- It does not cause the specific neurological signs like **paresthesias**, loss of **vibration sensation**, or **ataxia**, nor does it explain the **shiny tongue**.
*Iron supplementation*
- **Iron deficiency** is a common cause of fatigue, shortness of breath, and pale conjunctivae (due to anemia). However, it does not typically cause the **neurological symptoms** described (tingling, sensory loss, ataxia) or the **shiny tongue**.
- Although iron deficiency anemia might coexist, the neurological findings strongly point away from it as the primary cause of all symptoms.
*Penicillin G therapy*
- **Penicillin G** is used to treat bacterial infections, including syphilis and gonorrhea. While the patient was treated for gonorrhea, this current presentation is not indicative of an active infection.
- The symptoms are characteristic of a nutritional deficiency, not a bacterial infection or a complication of prior gonorrhea without current active infection.
Gastric surgery procedures US Medical PG Question 4: A 47-year-old man comes to the physician for gradual onset of fatigue for the last 4 months. He also reports shortness of breath and difficulty concentrating. His friends have told him that he appears pale. He has smoked one pack of cigarettes daily for the last 20 years. He does not drink alcohol. His vital signs are within normal limits. Neurological examination shows reduced sensation to light touch and pinprick in the toes bilaterally. Laboratory studies show:
Hemoglobin 8.2 g/dL
Mean corpuscular volume 108 μm3
Leukocyte count 4,200/mm3
Serum
Thyroid-stimulating hormone 2.6 μU/mL
Iron 67 μg/dL
Vitamin B12 (cyanocobalamin) 51 ng/L (N = 170–900)
Folic acid 13 ng/mL (N = 5.4–18)
An oral dose of radiolabeled vitamin B12 is administered, followed by an intramuscular injection of nonradioactive vitamin B12. A 24-hour urine sample is collected and urine vitamin B12 levels are unchanged. The procedure is repeated with the addition of oral intrinsic factor, and 24-hour urine vitamin B12 levels increase. The patient is at increased risk for which of the following?
- A. Type 2 diabetes mellitus
- B. Gastric carcinoma (Correct Answer)
- C. Celiac disease
- D. Colorectal carcinoma
- E. De Quervain thyroiditis
Gastric surgery procedures Explanation: ***Gastric carcinoma***
- The patient's presentation, including **macrocytic anemia**, neurological symptoms (reduced sensation), and particularly the **Schilling test results** (correction with intrinsic factor), points to **pernicious anemia**.
- **Pernicious anemia** significantly increases the risk of developing **gastric carcinoma** due to the associated **chronic atrophic gastritis** and **intestinal metaplasia**.
*Type 2 diabetes mellitus*
- While common, there is nothing in the patient's presentation (including laboratory values) that specifically suggests an increased risk for **type 2 diabetes mellitus**.
- **Pernicious anemia** does not directly increase the risk of developing diabetes.
*Celiac disease*
- **Celiac disease** is an autoimmune condition triggered by **gluten**, leading to malabsorption. It typically presents with **iron deficiency anemia** (microcytic), not macrocytic anemia.
- The Schilling test results indicating **intrinsic factor deficiency** are not characteristic of celiac disease.
*Colorectal carcinoma*
- Although **colorectal carcinoma** is a common malignancy, there are no specific symptoms (e.g., changes in bowel habits, rectal bleeding) or lab findings (e.g., iron deficiency anemia, which can occur with chronic blood loss) in this patient to suggest an elevated risk for this condition.
- **Pernicious anemia** does not directly predispose individuals to colorectal cancer.
*De Quervain thyroiditis*
- **De Quervain thyroiditis** is a subacute thyroiditis typically characterized by **painful thyroid enlargement** and transient hyperthyroidism followed by hypothyroidism.
- The patient's **TSH level is normal**, and there are no symptoms or signs pointing toward thyroid inflammation in this case.
Gastric surgery procedures US Medical PG Question 5: A 57-year-old woman presents to her primary care physician with a chief complaint of epigastric pain that has worsened over the past three weeks. She describes it as sudden “gnawing” sensations that last for up to half a minute before subsiding. She finds some relief after a glass of water, but does not associate relief or exacerbation around mealtimes. The patient denies any radiation of the pain, fever, weight loss, fatigue, or change in stool color and quality. She does not take any medications, and says her diet includes lots of spicy and smoked foods. The physician refers her for an upper endoscopy, which reveals evidence of duodenal ulcers and mild gastroesophageal reflux. The pathology report reveals focal intestinal metaplasia and gastric dysplasia in the stomach, but no Helicobacter pylori infection. How should the physician advise this patient?
- A. Intestinal metaplasia and gastric dysplasia are best managed with acid suppression and repeat endoscopy.
- B. Intestinal metaplasia requires no specific treatment, while gastric dysplasia requires immediate surgery.
- C. Intestinal metaplasia and gastric dysplasia are irreversible and untreatable.
- D. Intestinal metaplasia may regress with treatment of underlying cause; gastric dysplasia requires monitoring and possible intervention. (Correct Answer)
- E. Both intestinal metaplasia and gastric dysplasia require endoscopic surveillance.
Gastric surgery procedures Explanation: ***Correct: Intestinal metaplasia may regress with treatment of underlying cause; gastric dysplasia requires monitoring and possible intervention.***
- **Intestinal metaplasia (IM)**, especially without *H. pylori*, may resolve or improve if the underlying cause like **GERD** or chronic irritation (spicy/smoked foods) is treated.
- **Gastric dysplasia** is a **precancerous lesion** that warrants close surveillance and possible endoscopic removal or other interventions depending on its grade and extent to prevent progression to gastric cancer.
- This is the most comprehensive and medically accurate approach to managing both findings.
*Incorrect: Intestinal metaplasia and gastric dysplasia are best managed with acid suppression and repeat endoscopy.*
- While **acid suppression (PPI therapy)** is beneficial for **duodenal ulcers** and **GERD**, it is not the primary or sole management for **intestinal metaplasia** and **gastric dysplasia**.
- **Repeat endoscopy** is part of surveillance, but this option doesn't address treatment of underlying causes or the need for active intervention for dysplasia.
*Incorrect: Intestinal metaplasia requires no specific treatment, while gastric dysplasia requires immediate surgery.*
- **Intestinal metaplasia** does benefit from identifying and managing underlying causes (GERD, dietary factors) to prevent progression.
- **Gastric dysplasia** does not always require **immediate surgery**; management depends on the grade (low-grade vs. high-grade) and can include endoscopic resection before considering surgery.
*Incorrect: Intestinal metaplasia and gastric dysplasia are irreversible and untreatable.*
- This statement is factually incorrect; **intestinal metaplasia** can regress with treatment of underlying causes.
- **Gastric dysplasia** is treatable, with interventions ranging from surveillance to **endoscopic resection** or surgery to prevent progression to cancer.
*Incorrect: Both intestinal metaplasia and gastric dysplasia require endoscopic surveillance.*
- Although **endoscopic surveillance** is crucial for both conditions, especially for **gastric dysplasia**, this option doesn't encompass the complete management strategy.
- It fails to mention treatment of underlying causes (GERD, dietary modification) for intestinal metaplasia and active intervention (endoscopic resection) for dysplasia.
- Surveillance alone is insufficient; comprehensive management is required.
Gastric surgery procedures US Medical PG Question 6: A CT scan of the abdomen reveals a mass in the pancreatic uncinate process. Which of the following structures is most likely to be compressed by this mass?
- A. Common bile duct
- B. Portal vein
- C. Splenic vein
- D. Superior mesenteric vein (Correct Answer)
Gastric surgery procedures Explanation: ***Superior mesenteric vein***
- The **uncinate process** of the pancreas hooks around the **superior mesenteric vessels**. Therefore, a mass in this region would most directly compress the **superior mesenteric vein (SMV)** and artery (SMA).
- Compression of the SMV can lead to **venous outflow obstruction** from the small intestine, potentially causing **bowel ischemia** or edema.
*Common bile duct*
- The **common bile duct** passes through the **head of the pancreas**, not typically the uncinate process.
- Compression of the common bile duct would more commonly be associated with masses in the **head of the pancreas**, leading to **jaundice**.
*Portal vein*
- The **portal vein** is formed by the union of the **splenic vein** and the **superior mesenteric vein**, generally posterior to the neck of the pancreas.
- While pancreatic masses can affect the portal vein, a mass specifically in the uncinate process would more directly impinge on the SMV before significantly affecting the main portal vein, which is superior and posterior to the uncinate process.
*Splenic vein*
- The **splenic vein** runs along the **posterior aspect of the body and tail of the pancreas**.
- A mass in the uncinate process, located at the inferior margin of the head, is relatively distant from the splenic vein.
Gastric surgery procedures US Medical PG Question 7: A 45-year-old bank manager is brought to the emergency department by ambulance after vomiting bright red blood while at work. He is also complaining of abdominal pain that is 10/10 in intensity, stabbing, and relentless. He had a similar yet less severe abdominal pain off and on for the last 2 weeks. Eating food and drinking milk seemed to make the pain a little more tolerable. When he arrives at the hospital his heart rate is 115/min, and blood pressure is 100/70 mm Hg. On physical exam, he appears pale. A nasogastric tube is placed and removes 30 ml of bright red fluid from his stomach. An intravenous line is started and a bolus of fluids is administered. After stabilizing the patient, an esophagogastroduodenoscopy (EGD) is performed. There is a fair amount of residual blood in the stomach but no other abnormalities are noted. However, a bleeding duodenal ulcer is found on the posteromedial wall of the second portion of the duodenum. Which vessels listed below is the most likely blood supply to this section of the duodenum?
- A. Dorsal pancreatic artery
- B. Left gastroepiploic artery
- C. Gastroduodenal artery (Correct Answer)
- D. Inferior pancreaticoduodenal artery
- E. Greater pancreatic artery
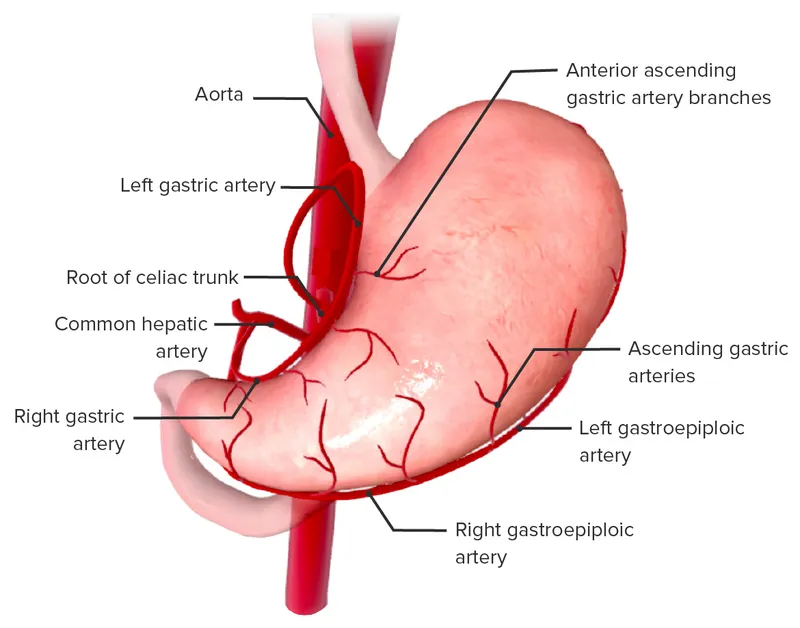
Gastric surgery procedures Explanation: ***Gastroduodenal artery***
- The **gastroduodenal artery** courses posterior to the first part of the duodenum and often supplies the **second part of the duodenum** via its branches, the anterior and posterior superior pancreaticoduodenal arteries.
- An ulcer in the **posteromedial wall of the second portion of the duodenum** is most likely to erode into the gastroduodenal artery, leading to significant hemorrhage as seen in this patient.
*Dorsal pancreatic artery*
- The **dorsal pancreatic artery** typically arises from the splenic artery or hepatic artery and supplies the **pancreas**, particularly the neck and body.
- It is not a primary blood supply to the **duodenum**, and its erosion due to a duodenal ulcer is highly unlikely.
*Left gastroepiploic artery*
- The **left gastroepiploic artery** (also known as the left gastro-omental artery) primarily supplies the **greater curvature of the stomach** and the **greater omentum**.
- Its location and distribution make it an improbable source of bleeding for an ulcer located in the **duodenum**.
*Inferior pancreaticoduodenal artery*
- The **inferior pancreaticoduodenal artery** typically arises from the superior mesenteric artery and supplies the **head of the pancreas** and the **third and fourth parts of the duodenum**.
- While it supplies the duodenum, it is less likely to be eroded by an ulcer in the **second portion of the duodenum** compared to the gastroduodenal artery.
*Greater pancreatic artery*
- The **greater pancreatic artery** (also known as the artery of the pancreatic magna) is a branch of the **splenic artery** and supplies the **pancreatic body and tail**.
- This artery is exclusively involved in the blood supply of the **pancreas** and is not a direct or likely source of bleeding from a **duodenal ulcer**.
Gastric surgery procedures US Medical PG Question 8: A 63-year-old woman comes to the physician because of diarrhea and weakness after her meals for 2 weeks. She has the urge to defecate 15–20 minutes after a meal and has 3–6 bowel movements a day. She also has palpitations, sweating, and needs to lie down soon after eating. One month ago, she underwent a distal gastrectomy for gastric cancer. She had post-operative pneumonia, which was treated with cefotaxime. She returned from a vacation to Brazil 6 weeks ago. Her immunizations are up-to-date. She is 165 cm (5 ft 5 in) tall and weighs 51 kg (112 lb); BMI is 18.6 kg/m2. Vital signs are within normal limits. Examination shows a well-healed abdominal midline surgical scar. The abdomen is soft and nontender. Bowel sounds are hyperactive. Rectal examination is unremarkable. Which of the following is the most appropriate next step in management?
- A. Dietary modifications (Correct Answer)
- B. Stool PCR test
- C. Octreotide therapy
- D. Metronidazole therapy
- E. Stool microscopy
Gastric surgery procedures Explanation: ***Dietary modifications***
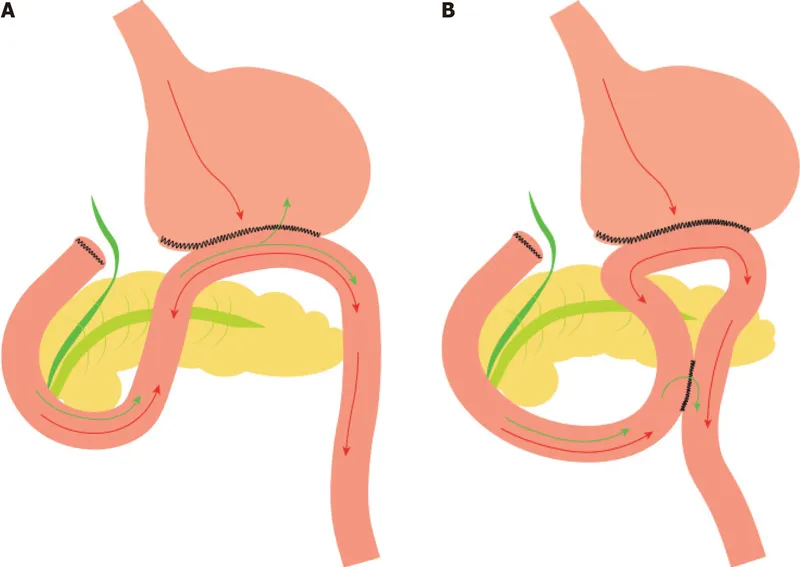
- This patient's symptoms (diarrhea, weakness, palpitations, sweating, and urge to defecate soon after meals) following a **distal gastrectomy** are classic for **dumping syndrome**. **Dietary modification** is the first-line treatment.
- Recommended modifications include **smaller, more frequent meals**, avoiding high-sugar foods, increasing protein and fiber, and separating solids from liquids during meals.
*Stool PCR test*
- While diarrhea is present, the patient's symptoms are strongly linked to her recent gastrectomy and meal ingestion rather than an infectious cause.
- A stool PCR test would be appropriate if there were other signs of infection, such as fever or severe abdominal pain, or if dietary modifications failed to resolve symptoms.
*Octreotide therapy*
- **Octreotide**, a somatostatin analog, is reserved for **severe cases of dumping syndrome** that do not respond to dietary modifications.
- It works by inhibiting the release of gastrointestinal hormones and slowing gastric emptying, but it is not the initial management step.
*Metronidazole therapy*
- **Metronidazole** is an antibiotic used to treat bacterial and parasitic infections. There is no evidence suggesting an infection in this patient.
- The timing of symptoms immediately post-meal points away from an infection and towards post-gastrectomy complications.
*Stool microscopy*
- Similar to a stool PCR, **stool microscopy** is used to identify parasites or other pathogens.
- Given the classic presentation of dumping syndrome following gastrectomy, an infectious cause is less likely, and other diagnostic tests should be pursued if dietary measures fail.
Gastric surgery procedures US Medical PG Question 9: A 44-year-old woman presents to the emergency department with confusion starting this morning. Her husband states that she initially complained of abdominal pain, diarrhea, and fatigue after eating. She has vomited 3 times and progressively became more confused. Her past medical history is notable for morbid obesity, diabetes, hypertension, dyslipidemia, a sleeve gastrectomy 1 month ago, and depression with multiple suicide attempts. Her temperature is 98.0°F (36.7°C), blood pressure is 104/54 mmHg, pulse is 120/min, respirations are 15/min, and oxygen saturation is 98% on room air. Her physical exam is notable for generalized confusion. Laboratory values are ordered as seen below.
Serum:
Na+: 139 mEq/L
Cl-: 100 mEq/L
K+: 3.9 mEq/L
HCO3-: 24 mEq/L
BUN: 22 mg/dL
Glucose: 41 mg/dL
Creatinine: 1.1 mg/dL
Ca2+: 10.2 mg/dL
C-peptide level: normal
Which of the following is the most likely diagnosis?
- A. Propranolol overdose
- B. Dumping syndrome (Correct Answer)
- C. Malnutrition
- D. Insulin overdose
- E. Glipizide overdose
Gastric surgery procedures Explanation: ***Dumping syndrome***
- The patient's recent **sleeve gastrectomy** and symptoms of **abdominal pain, diarrhea, fatigue, vomiting**, and subsequent **confusion** (due to hypoglycemia) after eating are classic for **late dumping syndrome**.
- **Late dumping syndrome** occurs 1-3 hours after eating due to rapid gastric emptying causing hyperglycemia, which triggers excessive insulin release, followed by reactive hypoglycemia.
- The **low glucose of 41 mg/dL** after a meal, alongside a **normal C-peptide**, confirms reactive hypoglycemia from endogenous insulin surge (not exogenous insulin).
*Propranolol overdose*
- While propranolol overdose can cause **hypoglycemia** and confusion, the patient's other symptoms of gastrointestinal distress directly following a meal are not typical.
- Propranolol overdose would also typically cause **bradycardia**, whereas the patient is tachycardic (120/min).
*Malnutrition*
- Malnutrition is a chronic condition and typically wouldn't present with acute, post-prandial symptoms like sudden abdominal pain, diarrhea, vomiting, and acute severe hypoglycemia leading to confusion.
- While possible post-bariatric surgery, the acute timing and specific meal-related symptoms point away from general malnutrition as the primary cause of this acute episode.
*Insulin overdose*
- **Insulin overdose** would cause severe hypoglycemia and confusion, but the patient's **normal C-peptide level** makes exogenous insulin administration unlikely as the cause of hypoglycemia.
- Insulin overdose doesn't typically cause the preceding abdominal pain, diarrhea, and vomiting immediately after eating like dumping syndrome.
*Glipizide overdose*
- Glipizide, a sulfonylurea, would cause **hypoglycemia** and confusion by stimulating endogenous insulin release, leading to an **elevated C-peptide level**.
- The patient's **normal C-peptide level** rules out sulfonylurea overdose as the cause of her hypoglycemia.
Gastric surgery procedures US Medical PG Question 10: A 37-year-old man presents to the physician. He has been overweight since childhood. He has not succeeded in losing weight despite following different diet and exercise programs over the past several years. He has had diabetes mellitus for 2 years and severe gastroesophageal reflux disease for 9 years. His medications include metformin, aspirin, and pantoprazole. His blood pressure is 142/94 mm Hg, pulse is 76/min, and respiratory rate is 14/min. His BMI is 36.5 kg/m2. Laboratory studies show:
Hemoglobin A1C 6.6%
Serum
Fasting glucose 132 mg/dL
Which of the following is the most appropriate surgical management?
- A. No surgical management at this time
- B. Laparoscopic adjustable gastric banding
- C. Biliopancreatic diversion and duodenal switch (BPD-DS)
- D. Laparoscopic sleeve gastrectomy
- E. Laparoscopic Roux-en-Y gastric bypass (Correct Answer)
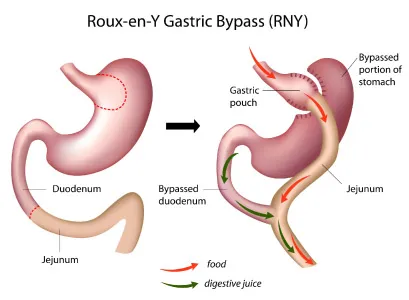
Gastric surgery procedures Explanation: ***Laparoscopic Roux-en-Y gastric bypass***
- This patient meets criteria for bariatric surgery with a **BMI of 36.5 kg/m2** along with significant **comorbidities** such as **type 2 diabetes** and **severe GERD**.
- Roux-en-Y gastric bypass is particularly effective for **diabetes remission** and is the most effective bariatric procedure for **resolving GERD**, making it the most appropriate choice given his symptoms.
*No surgical management at this time*
- The patient has a high BMI (36.5 kg/m2) with multiple obesity-related comorbidities including **diabetes mellitus** and **severe GERD** that have not improved with lifestyle changes and medication.
- Delaying surgical management would allow his obesity and related conditions to potentially worsen, despite his efforts to lose weight through diet and exercise.
*Laparoscopic adjustable gastric banding*
- This procedure typically results in **less weight loss** compared to other bariatric surgeries and is less effective at resolving comorbidities like diabetes and GERD.
- It carries a higher rate of **long-term complications** such as band erosion or slippage, and would not address the patient's severe GERD effectively.
*Biliopancreatic diversion and duodenal switch (BPD-DS)*
- While BPD-DS leads to the most significant weight loss and diabetes remission, it is associated with a **higher risk of surgical complications** and **severe nutritional deficiencies**.
- Given the patient's BMI and comorbidities, a less aggressive procedure like Roux-en-Y gastric bypass offers a better risk-benefit profile, especially for GERD.
*Laparoscopic sleeve gastrectomy*
- Sleeve gastrectomy is an effective weight-loss procedure, but it can **worsen or induce GERD** in some patients due to changes in gastric anatomy and pressure.
- As the patient has severe GERD, this procedure would not be the optimal choice and could exacerbate his symptoms.
More Gastric surgery procedures US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.