Esophageal surgery procedures US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Esophageal surgery procedures. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Esophageal surgery procedures US Medical PG Question 1: A 23-year-old college senior visits the university health clinic after vomiting large amounts of blood. He has been vomiting for the past 36 hours after celebrating his team’s win at the national hockey championship with his varsity friends while consuming copious amounts of alcohol. His personal medical history is unremarkable. His blood pressure is 129/89 mm Hg while supine and 100/70 mm Hg while standing. His pulse is 98/min, strong and regular, with an oxygen saturation of 98%. His body temperature is 36.5°C (97.7°F), while the rest of the physical exam is normal. Which of the following is associated with this patient’s condition?
- A. Esophageal tear (Correct Answer)
- B. Portal hypertension
- C. Esophageal metaplasia
- D. Esophageal varices
- E. Esophageal perforation
Esophageal surgery procedures Explanation: ***Esophageal tear***
- This patient's presentation of **hematemesis** after prolonged, forceful vomiting, especially following substantial alcohol consumption, is highly characteristic of a **Mallory-Weiss tear**.
- A Mallory-Weiss tear is a **longitudinal mucosal laceration** at the gastroesophageal junction, caused by the sudden increase in **intra-abdominal and intra-gastric pressure** during retching or vomiting.
*Portal hypertension*
- While portal hypertension can lead to upper GI bleeding from **esophageal varices**, there is no clinical evidence of **chronic liver disease** (e.g., jaundice, ascites, spider angiomata) in this otherwise healthy young man.
- The patient's unremarkable medical history and acute onset of symptoms after an episode of severe vomiting are not typical for a new presentation of chronic **portal hypertension**.
*Esophageal metaplasia*
- **Esophageal metaplasia (Barrett's esophagus)** is a change in the lining of the esophagus from squamous to columnar epithelium, usually due to chronic gastroesophageal reflux disease (GERD).
- It is an asymptomatic precursor to adenocarcinoma and does not cause acute, massive hematemesis without associated ulceration or malignancy.
*Esophageal varices*
- **Esophageal varices** are dilated veins in the lower esophagus that can rupture and cause life-threatening bleeding, typically due to **portal hypertension** from cirrhosis or other liver diseases.
- The patient's lack of a history of liver disease and the context of excessive vomiting make variceal bleeding less likely than a Mallory-Weiss tear.
*Esophageal perforation*
- **Esophageal perforation (Boerhaave syndrome)** is a transmural tear of the esophagus, also associated with severe vomiting, but it presents with more severe symptoms.
- Key differentiating features include **severe retrosternal chest pain**, **dyspnea**, **subcutaneous emphysema**, and potentially **septic shock** due to mediastinitis, none of which are described in this patient.
Esophageal surgery procedures US Medical PG Question 2: A previously healthy 55-year-old man comes to the physician because of a 5-month history of progressively worsening substernal chest pain after meals. The pain occurs almost daily, is worst after eating spicy food or drinking coffee, and often wakes him up from sleep at night. He has not had any weight loss. He has smoked 1 pack of cigarettes daily for 35 years and he drinks 1 to 2 glasses of wine daily with dinner. Physical examination is unremarkable. Esophagogastroduodenoscopy shows erythema of the distal esophagus with two small mucosal erosions. Biopsy specimens obtained from the esophagus show no evidence of metaplasia. Without treatment, this patient is at greatest risk for which of the following complications?
- A. Esophageal squamous cell carcinoma
- B. Esophageal adenocarcinoma
- C. Esophageal stricture (Correct Answer)
- D. Sliding hiatal hernia
- E. Pyloric stenosis
Esophageal surgery procedures Explanation: ***Esophageal stricture***
- Chronic inflammation from **gastroesophageal reflux disease (GERD)** can lead to **fibrosis and scar tissue formation** in the esophagus, resulting in the narrowing of the esophageal lumen.
- While not immediately life-threatening, **esophageal strictures** can cause **dysphagia** and require endoscopic dilation.
*Esophageal squamous cell carcinoma*
- This type of cancer is more commonly associated with **tobacco and alcohol use**, but generally does not directly result from GERD.
- There is no mention of **dysphagia to solids** or other typical symptoms of esophageal cancer.
*Esophageal adenocarcinoma*
- This complication is typically preceded by **Barrett's esophagus**, which involves **intestinal metaplasia** of the esophageal lining.
- The biopsy results explicitly state **no evidence of metaplasia**, making this an unlikely immediate risk.
*Sliding hiatal hernia*
- A **sliding hiatal hernia** is a common anatomical predisposition for GERD, and it may contribute to the patient's symptoms but is not a complication *of* GERD itself.
- It involves the **protrusion of the stomach into the chest cavity** through the diaphragm.
*Pyloric stenosis*
- **Pyloric stenosis** affects the **pylorus**, the opening between the stomach and the small intestine, and is not a direct complication of esophageal reflux disease.
- It usually presents with **projectile vomiting** and typically occurs in infants or, less commonly, in adults due to other causes like chronic ulcers or tumors.
Esophageal surgery procedures US Medical PG Question 3: A 58-year-old man comes to the physician for the evaluation of intermittent dysphagia for 6 months. He states that he drinks a lot of water during meals to help reduce discomfort he has while swallowing food. He has hypertension and gastroesophageal reflux disease. He has smoked one half-pack of cigarettes daily for 32 years. He does not drink alcohol. Current medications include hydrochlorothiazide and ranitidine. He is 173 cm (5 ft 8 in) tall and weighs 101 kg (222 lb); BMI is 33.7 kg/m2. His temperature is 37°C (98.6°F), pulse is 75/min, and blood pressure is 125/75 mm Hg. The lungs are clear to auscultation. Cardiac examination shows no murmurs, rubs, or gallops. The abdomen is soft and nontender. A barium esophagogram shows a smooth, circumferential narrowing at the distal esophagus. An upper endoscopy shows a sliding hiatal hernia and a thin mucosal ring at the gastroesophageal junction. Biopsies from the area show normal squamous and columnar epithelium with no dysplasia or malignancy. Which of the following is the most appropriate next step in the management of this patient?
- A. Mechanical dilation (Correct Answer)
- B. Iron supplementation
- C. Esophageal stent
- D. Esophagectomy
- E. Nissen fundoplication
Esophageal surgery procedures Explanation: ***Mechanical dilation***
- The patient's presentation with **intermittent dysphagia to solids**, a thin mucosal ring at the gastroesophageal junction on endoscopy, and a **smooth circumferential narrowing** on barium study is diagnostic of a **Schatzki ring** (B ring).
- Biopsies showing **no dysplasia or malignancy** confirm this is a benign condition.
- **Mechanical dilation** (pneumatic or bougie dilation) is the **first-line treatment** for symptomatic Schatzki rings, with success rates exceeding 90% and providing immediate symptom relief.
- The procedure is safe, minimally invasive, and can be repeated if symptoms recur.
*Iron supplementation*
- **Plummer-Vinson syndrome** (iron deficiency anemia with esophageal webs in the upper esophagus) presents differently from this patient's distal esophageal ring.
- There is no evidence of anemia in this case, and iron supplementation would not address the **mechanical obstruction**.
*Esophageal stent*
- Esophageal stents are reserved for **malignant strictures** or **refractory benign strictures** that fail multiple dilations.
- This would be inappropriate as **first-line therapy** for a benign Schatzki ring and carries higher complication risks (migration, perforation).
*Esophagectomy*
- **Esophagectomy** is a major surgical procedure indicated for **esophageal cancer** or end-stage benign disease (e.g., severe caustic injury, refractory achalasia with megaesophagus).
- This is **grossly excessive** for a benign Schatzki ring, which responds well to simple dilation.
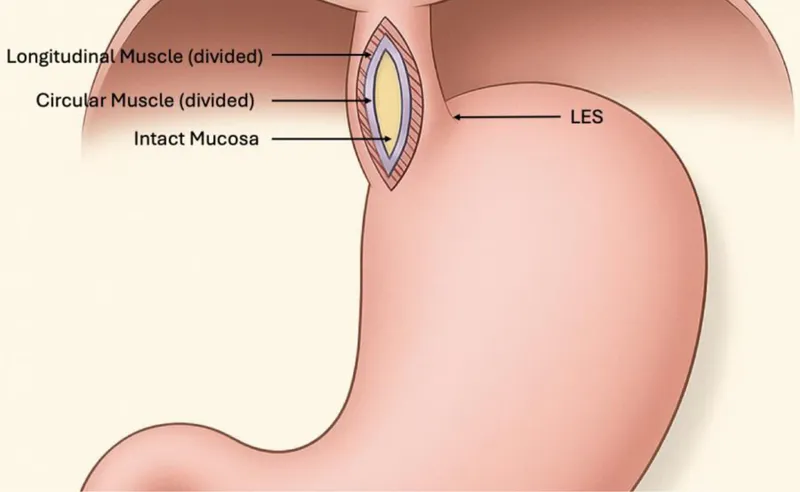
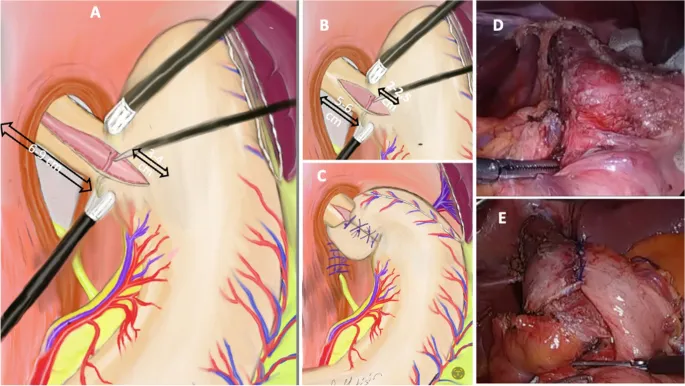
*Nissen fundoplication*
- **Nissen fundoplication** treats **severe GERD** by creating an anti-reflux barrier, but does not address an existing **mechanical stricture or ring**.
- While the patient has GERD (a risk factor for Schatzki rings), the immediate problem is the obstructing ring itself, which requires dilation first.
- Some patients may benefit from fundoplication after dilation if severe reflux persists, but this is not the next step.
Esophageal surgery procedures US Medical PG Question 4: A 62-year-old man is referred to a gastroenterologist because of difficulty swallowing for the past 5 months. He has difficulty swallowing both solid and liquid foods, but there is no associated pain. He denies any shortness of breath or swelling in his legs. He immigrated from South America 10 years ago. He is a non-smoker and does not drink alcohol. His physical examination is unremarkable. A barium swallow study was ordered and the result is given below. Esophageal manometry confirms the diagnosis. What is the most likely underlying cause of this patient’s condition?
- A. Pharyngoesophageal diverticulum
- B. Chagas disease (Correct Answer)
- C. Esophageal rupture
- D. Gastroesophageal reflux disease
- E. Squamous cell carcinoma of the esophagus
Esophageal surgery procedures Explanation: ***Chagas disease***
- The patient's history of living in **South America** and presenting with **dysphagia for both solids and liquids** (suggesting a motility disorder), along with the **barium swallow image showing esophageal dilation and a 'bird's beak' appearance** at the gastroesophageal junction, are highly characteristic of achalasia caused by Chagas disease.
- Chagas disease, caused by *Trypanosoma cruzi*, leads to the destruction of **myenteric plexus neurons** in the esophagus, resulting in achalasia (failure of the lower esophageal sphincter to relax) and megaesophagus.
*Pharyngoesophageal diverticulum*
- This typically presents as **Zenker's diverticulum**, causing **difficulty initiating a swallow**, regurgitation of undigested food, and sometimes halitosis, which is different from the described dysphagia for both solids and liquids.
- A Zenker's diverticulum would appear as a **pouch-like protrusion** in the posterior pharynx, not the diffuse esophageal dilation seen in the image.
*Esophageal rupture*
- Esophageal rupture (Boerhaave syndrome) is an acute, life-threatening condition associated with **severe chest pain, vomiting, and crepitus**, not a chronic, progressive dysphagia without pain.
- Imaging would reveal **extravasation of contrast** into the mediastinum or pleural space, not the smooth dilation and distal narrowing observed.
*Gastroesophageal reflux disease*
- While chronic GERD can lead to **strictures** and dysphagia, it typically causes **heartburn**, regurgitation, and sometimes odynophagia, and the dysphagia is usually progressive for solids first.
- The barium swallow would show reflux or a stricture, not the **classic achalasia findings** of a dilated esophagus tapering to a narrow distal segment.
*Squamous cell carcinoma of the esophagus*
- Squamous cell carcinoma usually presents with **progressive dysphagia, initially for solids**, and is often associated with weight loss, smoking, and alcohol use, none of which are present in this patient.
- A tumor would typically appear as an **irregular, focal narrowing or mass** on barium swallow, not the smooth, diffuse dilation seen in this image.
Esophageal surgery procedures US Medical PG Question 5: A 48-year-old man presents to an urgent care center with epigastric discomfort following meals and an occasional dry cough worse in the morning, both of which have increased in frequency over the past several months. He is otherwise healthy and has no additional complaints. Past medical history is significant for major depressive disease, anxiety, and hypothyroidism. Physical exam is unremarkable. Given the following options, what is the most appropriate next step in patient management?
- A. Fluoroscopic barium swallow
- B. Lifestyle modifications
- C. EGD with esophageal biopsy
- D. Electrocardiogram
- E. Begin Omeprazole therapy (Correct Answer)
Esophageal surgery procedures Explanation: ***Begin Omeprazole therapy***
- **Epigastric discomfort after meals** and **dry cough worse in the morning** are classic symptoms of **gastroesophageal reflux disease (GERD)**.
- For **typical GERD symptoms without alarm features**, the most appropriate next step is an **empirical trial of PPI therapy** (proton pump inhibitor such as omeprazole) for 4-8 weeks.
- **Current guidelines** from the American College of Gastroenterology recommend **PPI therapy as first-line treatment** for typical GERD, as lifestyle modifications alone are often insufficient.
- The patient has had symptoms increasing over several months, warranting pharmacologic intervention.
*Lifestyle modifications*
- While lifestyle modifications (weight loss, avoiding late meals, elevating head of bed, avoiding trigger foods) are **important adjunctive measures**, they are **not sufficient as monotherapy** for established GERD.
- These should be recommended **in addition to PPI therapy**, not as a standalone initial treatment for symptomatic GERD.
*Fluoroscopic barium swallow*
- This study is useful for evaluating **dysphagia**, esophageal strictures, or motility disorders, which are not the primary complaints here.
- It is generally not indicated for uncomplicated GERD without structural concerns.
*EGD with esophageal biopsy*
- **Esophagogastroduodenoscopy (EGD)** with biopsy is indicated for **alarm symptoms** such as dysphagia, odynophagia, weight loss, anemia, or **failure of empirical PPI therapy** after 4-8 weeks.
- The patient presents with typical GERD symptoms without alarm features, making diagnostic endoscopy premature before a therapeutic trial.
*Electrocardiogram*
- While chest pain can sometimes mimic cardiac pain, this patient's symptoms are primarily **epigastric and postprandial** with a **chronic cough**.
- There are no concerning cardiac symptoms such as exertional chest pain, diaphoresis, dyspnea, or radiation to the arm/jaw that would warrant ECG evaluation.
Esophageal surgery procedures US Medical PG Question 6: A 58-year-old man comes to the physician for recurrent heartburn for 12 years. He has also developed a cough for a year, which is worse at night. He has smoked a pack of cigarettes daily for 30 years. His only medication is an over-the-counter antacid. He has not seen a physician for 8 years. He is 175 cm (5 ft 9 in) tall and weighs 95 kg (209 lb); BMI is 31 kg/m2. Vital signs are within normal limits. There is no lymphadenopathy. The abdomen is soft and nontender. The remainder of the examination shows no abnormalities. A complete blood count is within the reference range. An upper endoscopy shows columnar epithelium 2 cm from the gastroesophageal junction. Biopsies from the columnar epithelium show low-grade dysplasia and intestinal metaplasia. Which of the following is the most appropriate next step in management?
- A. Endoscopic therapy (Correct Answer)
- B. Nissen fundoplication
- C. Repeat endoscopy in 18 months
- D. External beam radiotherapy
- E. Omeprazole, clarithromycin, and metronidazole therapy
Esophageal surgery procedures Explanation: ***Endoscopic therapy***
- The presence of **low-grade dysplasia** and **intestinal metaplasia** in **Barrett's esophagus** significantly increases the risk of progression to high-grade dysplasia or esophageal adenocarcinoma. Endoscopic therapy, such as **endoscopic mucosal resection (EMR)** or **radiofrequency ablation (RFA)**, is recommended to eradicate the dysplastic tissue.
- This approach aims to prevent malignant transformation and has been shown to be more effective than surveillance alone for low-grade dysplasia.
*Nissen fundoplication*
- This is a **surgical procedure** primarily used to treat severe **gastroesophageal reflux disease (GERD)** symptoms that are refractory to medical management.
- While the patient has GERD, fundoplication does not directly address the **dysplastic changes** already identified in the esophageal lining and is not the primary treatment for dysplasia.
*Repeat endoscopy in 18 months*
- For **Barrett's esophagus without dysplasia**, surveillance endoscopy is typically performed every 3-5 years. For **low-grade dysplasia**, surveillance intervals are often shorter (e.g., 6-12 months) if immediate endoscopic therapy is not pursued or if there is uncertainty about the biopsy findings.
- However, with confirmed **low-grade dysplasia** and **intestinal metaplasia**, active eradication via endoscopic therapy is generally preferred over watchful waiting with delayed surveillance, given the risk of progression.
*External beam radiotherapy*
- **External beam radiotherapy** is a treatment for established **esophageal cancer**, not for precancerous conditions like low-grade dysplasia in Barrett's esophagus.
- It carries significant side effects and is overly aggressive for the current findings.
*Omeprazole, clarithromycin, and metronidazole therapy*
- This is a standard **triple therapy regimen** for eradicating **Helicobacter pylori infection**.
- While the patient has chronic GERD, there is no mention of H. pylori infection, and treating H. pylori would not resolve the **dysplastic changes** in the esophageal epithelium.
Esophageal surgery procedures US Medical PG Question 7: A 63-year-old man presents to the ambulatory medical clinic with symptoms of dysphagia and ‘heartburn’, which he states have become more troublesome over the past year. Past medical history is significant for primary hypertension. On physical exam, he is somewhat tender to palpation over his upper abdomen. The vital signs include: temperature 36.7°C (98.0°F), blood pressure 126/74 mm Hg, heart rate 74/min, and respiratory rate 14/min. Barium swallow fluoroscopy demonstrates a subdiaphragmatic gastroesophageal junction, with herniation of the gastric fundus into the left hemithorax. Given the following options, what is the most appropriate next step in the management of this patient’s underlying condition?
- A. Lifestyle modification
- B. Antacid therapy
- C. Cimetidine
- D. Surgical gastropexy (Correct Answer)
- E. Omeprazole
Esophageal surgery procedures Explanation: ***Surgical gastropexy***
- This patient has a **paraesophageal hiatal hernia** (Type II or III), evidenced by the barium swallow showing a **subdiaphragmatic gastroesophageal junction** with **herniation of the gastric fundus into the left hemithorax**.
- In paraesophageal hernias, the GE junction remains in relatively normal position while the gastric fundus herniates through the diaphragmatic hiatus alongside the esophagus.
- **Symptomatic paraesophageal hernias** warrant **surgical repair** (fundoplication with hernia reduction and hiatal repair) due to significant risk of complications including **gastric volvulus, strangulation, incarceration**, and **ischemia**.
- The patient's progressive dysphagia and year-long symptoms indicate this is not an incidental finding but a symptomatic hernia requiring definitive surgical management.
*Omeprazole*
- **Proton pump inhibitors** are first-line medical therapy for **sliding hiatal hernias (Type I)** where the GE junction migrates above the diaphragm, causing GERD symptoms.
- In **paraesophageal hernias**, the primary pathophysiology is **mechanical** (herniation and potential obstruction/strangulation), not acid-related, so PPIs address symptoms but not the underlying structural problem.
- While PPIs may provide some symptomatic relief, they do **not prevent the serious mechanical complications** of paraesophageal hernias and are insufficient as definitive management.
*Lifestyle modification*
- **Lifestyle modifications** are appropriate adjunctive measures for GERD and sliding hiatal hernias but do not address the mechanical nature and complication risk of paraesophageal hernias.
- They cannot prevent gastric volvulus or strangulation, which are life-threatening complications unique to paraesophageal hernias.
*Antacid therapy*
- **Antacids** provide temporary symptom relief but have no role in managing the structural abnormality or preventing complications of paraesophageal hernia.
- They are even less effective than PPIs for acid suppression and similarly fail to address the mechanical problem.
*Cimetidine*
- **H2-receptor antagonists** like cimetidine reduce gastric acid production but are less potent than PPIs.
- Like PPIs, they may provide some symptomatic relief but do not address the **mechanical herniation** or prevent the serious complications that make surgical repair necessary for paraesophageal hernias.
Esophageal surgery procedures US Medical PG Question 8: A 63-year-old man is brought to the emergency department, 30 minutes after being involved in a high-speed motor vehicle collision. He is obtunded on arrival. He is intubated and mechanical ventilation is begun. The ventilator is set at a FiO2 of 60%, tidal volume of 440 mL, and positive end-expiratory pressure of 4 cm H2O. On the third day of intubation, his temperature is 37.3°C (99.1°F), pulse is 91/min, and blood pressure is 103/60 mm Hg. There are decreased breath sounds over the left lung base. Cardiac examination shows no abnormalities. The abdomen is soft and not distended. Arterial blood gas analysis shows:
pH 7.49
pCO2 29 mm Hg
pO2 73 mm Hg
HCO3- 20 mEq/L
O2 saturation 89%
Monitoring shows a sudden increase in the plateau airway pressure. An x-ray of the chest shows deepening of the costophrenic angle on the left side. Which of the following is the most appropriate next step in management?
- A. CT scan of the chest
- B. Administer levofloxacin
- C. Close observation
- D. Increase the PEEP
- E. Insertion of a chest tube (Correct Answer)
Esophageal surgery procedures Explanation: ***Insertion of a chest tube***
- The sudden increase in **plateau airway pressure**, decreased breath sounds over the left lung base, worsening hypoxemia (O2 sat 89%) despite high FiO2, and **deepening of the costophrenic angle on the left side** indicate a **traumatic hemothorax**.
- Deepening of the costophrenic angle on chest X-ray is a classic sign of **pleural fluid accumulation** (hemothorax or pleural effusion), not pneumothorax.
- In a trauma patient (high-speed motor vehicle collision) on day 3 of mechanical ventilation, this represents a **delayed hemothorax** requiring immediate drainage.
- **Chest tube insertion** is the definitive management to evacuate blood, re-expand the lung, and improve ventilation and oxygenation.
*CT scan of the chest*
- While CT scan would provide detailed anatomical information, the clinical presentation with sudden respiratory decompensation and clear chest X-ray findings of hemothorax requires **immediate intervention**.
- Delaying treatment to obtain CT imaging in an unstable ventilated patient could worsen hypoxemia and lead to cardiovascular compromise.
- CT scan may be obtained later if needed to evaluate for ongoing bleeding or other injuries.
*Administer levofloxacin*
- Antibiotics would be appropriate for **pneumonia or empyema**, but the patient has no clear signs of infection (afebrile at 37.3°C, acute presentation over hours not days).
- The primary problem is **mechanical compression** from pleural fluid accumulation, not infection.
- Antibiotics do not address the life-threatening respiratory compromise from hemothorax.
*Close observation*
- Close observation is inappropriate given the acute deterioration with increased plateau pressures and worsening hypoxemia.
- The patient requires urgent intervention to prevent further respiratory failure and potential cardiovascular collapse.
- Expectant management would be negligent in this clinical scenario.
*Increase the PEEP*
- Increasing **Positive End-Expiratory Pressure (PEEP)** would worsen the situation by increasing intrathoracic pressure against an already compressed lung.
- Higher PEEP could impair venous return, decrease cardiac output, and potentially convert a simple hemothorax to a tension physiology.
- PEEP adjustments do not address the underlying problem of pleural space fluid accumulation requiring drainage.
Esophageal surgery procedures US Medical PG Question 9: A 68-year-old man is brought to the emergency department because of fever, progressive weakness, and cough for the past five days. He experienced a similar episode 2 months ago, for which he was hospitalized for 10 days while visiting his son in Russia. He states that he has never fully recovered from that episode. He felt much better after being treated with antibiotics, but he still coughs often during meals. He sometimes also coughs up undigested food after eating. For the last 5 days, his coughing has become more frequent and productive of yellowish-green sputum. He takes hydrochlorothiazide for hypertension and pantoprazole for the retrosternal discomfort that he often experiences while eating. He has smoked half a pack of cigarettes daily for the last 30 years and drinks one shot of vodka every day. The patient appears thin. His temperature is 40.1°C (104.2°F), pulse is 118/min, respirations are 22/min, and blood pressure is 125/90 mm Hg. Auscultation of the lungs shows right basal crackles. There is dullness on percussion at the right lung base. The remainder of the physical examination shows no abnormalities. Laboratory studies show:
Hemoglobin 15.4 g/dL
Leukocyte count 17,000/mm3
Platelet count 350,000/mm3
Na+ 139 mEq/L
K+
4.6 mEq/L
Cl- 102 mEq/L
HCO3- 25 mEq/L
Urea Nitrogen 16 mg/dL
Creatinine 1.3 mg/dL
An x-ray of the chest shows a right lower lobe infiltrate. Which of the following is the most likely explanation for this patient's symptoms?
- A. Weak tone of the lower esophageal sphincter
- B. Unrestricted growth of pneumocytes with invasion of the surrounding tissue
- C. Uncoordinated contractions of the esophagus
- D. Formation of a tissue cavity containing necrotic debris
- E. Outpouching of the hypopharynx (Correct Answer)
Esophageal surgery procedures Explanation: ***Outpouching of the hypopharynx***
- The patient's history of coughing up undigested food and coughing during meals suggests **dysphagia** and potential **aspiration**, which can be caused by a **Zenker's diverticulum** (an outpouching of the hypopharynx).
- This condition creates a pouch that can trap food, leading to regurgitation and repeated aspiration pneumonia, as evidenced by his recurrent pneumonia and current symptoms.
- Zenker's diverticulum is the **underlying explanation** that accounts for *all* of this patient's symptoms: the regurgitation of undigested food, dysphagia, and recurrent aspiration pneumonia.
*Weak tone of the lower esophageal sphincter*
- A weak lower esophageal sphincter (LES) primarily causes **gastroesophageal reflux disease (GERD)**, often associated with heartburn and regurgitation of stomach contents, not undigested food.
- While GERD can cause aspiration, the coughing up of *undigested food* is more indicative of a proximal esophageal issue or pharyngeal problem.
*Unrestricted growth of pneumocytes with invasion of the surrounding tissue*
- This describes **lung cancer**, which can present with cough, weight loss, and recurrent pneumonia due to bronchial obstruction.
- However, the symptom of coughing up *undigested food* is not typical of primary lung malignancy, and the history strongly points to a swallowing disorder.
*Uncoordinated contractions of the esophagus*
- This refers to esophageal motility disorders like **achalasia** or **diffuse esophageal spasm**, which can cause dysphagia and regurgitation.
- While these can lead to aspiration, the specific complaint of coughing up *undigested food* *after eating* is more characteristic of a pharyngeal pouch (Zenker's diverticulum) rather than general esophageal dysmotility.
*Formation of a tissue cavity containing necrotic debris*
- This describes a **lung abscess**, which is a possible *complication* of aspiration pneumonia, accounting for the fever, productive cough, and infiltrate.
- However, the question asks for the **most likely explanation** for this patient's symptoms—a lung abscess is a *sequela* of aspiration, not the *underlying cause* of the repeated aspiration events.
- It does not explain the pathognomonic finding of coughing up undigested food after eating, which points to Zenker's diverticulum as the root cause.
Esophageal surgery procedures US Medical PG Question 10: A 68-year-old man comes to the physician because of a 6-month history of difficulty swallowing pieces of meat and choking frequently during meal times. He also sometimes regurgitates foul-smelling, undigested food particles. Examination shows a 3 x 3 cm soft cystic, immobile mass in the upper third of the left side of his neck anterior to the left sternocleidomastoid muscle that becomes prominent when he coughs. A barium swallow shows an accumulation of contrast on the lateral aspect of the neck at the C5 level. Which of the following is the most likely underlying cause for this patient's condition?
- A. Remnant of the embryological omphalomesenteric duct
- B. Inadequate relaxation of lower esophageal sphincter
- C. Remnant of the thyroglossal duct
- D. Increased intrapharyngeal pressure (Correct Answer)
- E. Remnant of the second branchial cleft
Esophageal surgery procedures Explanation: ***Increased intrapharyngeal pressure***
- The symptoms of **dysphagia**, **regurgitation of undigested food**, and a **neck mass prominent with coughing** are classic for a **Zenker's diverticulum**, which results from increased intrapharyngeal pressure causing herniation of mucosa through Killian's triangle.
- The barium swallow showing **contrast accumulation** and the location of the mass further support this diagnosis, as Zenker's diverticula are pseudo-diverticula caused by pulsion from high pressure during swallowing.
*Remnant of the embryological omphalomesenteric duct*
- An **omphalomesenteric duct remnant** typically presents as a **Meckel's diverticulum** in the small intestine or an umbilical fistula, not as a neck mass with swallowing difficulties.
- This embryological anomaly is related to the midgut development and has no connection to pharyngeal issues.
*Inadequate relaxation of lower esophageal sphincter*
- **Inadequate relaxation of the lower esophageal sphincter** (LES) is characteristic of **achalasia**, which causes dysphagia and regurgitation, but typically of *fermented* rather than *undigested* food, and does not present with a palpable neck mass as described.
- Achalasia involves the distal esophagus and does not lead to a pharyngeal outpouching.
*Remnant of the thyroglossal duct*
- A **thyroglossal duct cyst** is a midline neck mass that moves with swallowing and tongue protrusion, which is not consistent with the lateral, pulsion-type mass that becomes prominent with coughing.
- While it can be found in the upper third of the neck, its embryological origin and presentation differ significantly from a Zenker's diverticulum.
*Remnant of the second branchial cleft*
- A **second branchial cleft cyst** is typically a lateral neck mass, often located anterior to the sternocleidomastoid muscle, but it is congenital and does not typically present with progressive dysphagia and regurgitation of undigested food in adulthood, nor does it typically become prominent with coughing due to increased intrapharyngeal pressure.
- These cysts are usually asymptomatic unless infected and are not directly related to swallowing mechanics.
More Esophageal surgery procedures US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.