Colorectal cancer resection principles US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Colorectal cancer resection principles. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Colorectal cancer resection principles US Medical PG Question 1: A 53-year-old woman comes to the emergency department because of weakness and abdominal pain for 24 hours. She has had three bowel movements with dark stool during this period. She has not had vomiting and has never had such episodes in the past. She underwent a tubal ligation 15 years ago. She has chronic lower extremity lymphedema, osteoarthritis, and type 2 diabetes mellitus. Her father died of colon cancer at the age of 72 years. Current medications include metformin, naproxen, and calcium with vitamin D3. She had a screening colonoscopy at 50 years of age which was normal. She appears pale and diaphoretic. Her temperature is 36°C (96.8°F), pulse is 110/min, respirations are 20/min, and blood pressure is 90/50 mm Hg. Pulse oximetry on room air shows an oxygen saturation of 98%. The abdomen is soft and nondistended with mild epigastric tenderness. Rectal exam shows tarry stool. Two large bore IV lines are placed and fluid resuscitation with normal saline is initiated. Which of the following is the most appropriate next step in management?
- A. Esophagogastroduodenoscopy (Correct Answer)
- B. CT scan of the abdomen with contrast
- C. Flexible sigmoidoscopy
- D. Diagnostic laparoscopy
- E. Colonoscopy
Colorectal cancer resection principles Explanation: ***Esophagogastroduodenoscopy***
- The patient presents with symptoms highly suggestive of an **upper GI bleed**, including **melena (dark, tarry stools)**, weakness, abdominal pain, and signs of **hemodynamic instability** (tachycardia, hypotension, pallor, diaphoresis).
- An EGD is the **most appropriate initial diagnostic and therapeutic procedure** for suspected upper GI bleeding, allowing for direct visualization, diagnosis of the source (e.g., peptic ulcer, esophagitis, varices), and immediate intervention (e.g., endoscopic hemostasis).
*CT scan of the abdomen with contrast*
- A CT scan is not the first-line investigation for acute GI bleeding because it is generally less sensitive than endoscopy for active bleeding and does not allow for immediate therapeutic intervention.
- While it can identify some causes of GI bleeding, such as tumors or vascular malformations, it is usually reserved for cases where endoscopy is inconclusive or contraindicated.
*Flexible sigmoidoscopy*
- Flexible sigmoidoscopy visualizes only the **rectum and sigmoid colon**, which is insufficient to evaluate the entire colon for a lower GI bleed, and completely misses the upper GI tract.
- Given the tarry stools (melena), an upper GI bleed is far more likely than a lower GI bleed.
*Diagnostic laparoscopy*
- Diagnostic laparoscopy is an invasive surgical procedure used to explore the abdominal cavity for conditions that cause pain or internal bleeding, but it is not the initial diagnostic choice for **GI bleeding**.
- It would expose the patient to unnecessary surgical risks without first attempting less invasive and highly effective endoscopic methods.
*Colonoscopy*
- While a colonoscopy is the gold standard for evaluating the **lower GI tract**, the patient's symptoms (melena, epigastric tenderness) strongly indicate an **upper GI bleed**.
- Performing a colonoscopy first would delay the diagnosis and treatment of a potentially life-threatening upper GI bleed.
Colorectal cancer resection principles US Medical PG Question 2: A 26-year-old white man comes to the physician because of increasing generalized fatigue for 6 months. He has been unable to work out at the gym during this period. He has also had cramping lower abdominal pain and diarrhea for the past 5 weeks that is occasionally bloody. His father was diagnosed with colon cancer at the age of 65. He has smoked half a pack of cigarettes daily for the past 10 years. He drinks 1–2 beers on social occasions. His temperature is 37.3°C (99.1°F), pulse is 88/min, and blood pressure is 116/74 mm Hg. Physical examination shows dry mucous membranes. The abdomen is soft and nondistended with slight tenderness to palpation over the lower quadrants bilaterally. Rectal examination shows stool mixed with blood. His hemoglobin concentration is 13.5 g/dL, leukocyte count is 7,500/mm3, and platelet count is 480,000/mm3. Urinalysis is within normal limits. Which of the following is the most appropriate next step in management?
- A. D-xylose absorption test
- B. CT scan of the abdomen and pelvis with contrast
- C. Capsule endoscopy
- D. Colonoscopy (Correct Answer)
- E. Flexible sigmoidoscopy
Colorectal cancer resection principles Explanation: ***Colonoscopy***
- The patient presents with **bloody diarrhea** and **lower abdominal pain**, which are classic symptoms of inflammatory bowel disease (IBD), particularly **Crohn's disease** or **ulcerative colitis**. A colonoscopy allows for direct visualization of the colonic and terminal ileal mucosa, **biopsy collection** for histological confirmation, and assessment of disease extent and severity.
- While the patient's hemoglobin is currently normal, the presence of bloody stools indicates potential ongoing blood loss, and the history of fatigue suggests chronic inflammation. **Colonoscopy is the gold standard** for diagnosing and differentiating types of IBD.
*D-xylose absorption test*
- This test is used to assess **small bowel mucosal function** and carbohydrate absorption, typically in cases of suspected malabsorption like **celiac disease**.
- While malabsorption can cause fatigue, the patient's primary symptoms of bloody diarrhea and abdominal pain are not typical for isolated malabsorption, and a d-xylose test would not identify the source of bleeding.
*CT scan of the abdomen and pelvis with contrast*
- A CT scan can identify **extraintestinal manifestations** of IBD, abscesses, or bowel wall thickening, but it is **less sensitive** than colonoscopy for direct mucosal evaluation and cannot obtain biopsies for definitive diagnosis.
- It might be considered after colonoscopy for assessing transmural involvement or complications but is not the initial diagnostic step for primary luminal symptoms.
*Capsule endoscopy*
- Capsule endoscopy is primarily used to evaluate the **small bowel** for lesions beyond the reach of standard upper endoscopy and colonoscopy, such as obscure GI bleeding or suspected Crohn's disease confined to the small bowel.
- Given the patient's symptoms of **lower abdominal pain** and bloody diarrhea, the pathology is likely in the colon or terminal ileum, making colonoscopy more appropriate for initial evaluation. A capsule endoscopy does not visualize the colon.
*Flexible sigmoidoscopy*
- A flexible sigmoidoscopy visualizes the **rectum and a portion of the sigmoid colon**, which might be affected in ulcerative colitis.
- However, it would miss lesions in the more proximal colon or terminal ileum, which are common sites for Crohn's disease and some forms of ulcerative colitis, thus potentially leading to an incomplete diagnosis.
Colorectal cancer resection principles US Medical PG Question 3: A 64-year-old woman has progressively worsening abdominal pain 5 hours after an open valve replacement with cardiopulmonary bypass. The pain is crampy and associated with an urge to defecate. The patient reports having had 2 bloody bowel movements in the last hour. Her operation was complicated by significant intraoperative blood loss, which prolonged the operation and necessitated 2 transfusions of red blood cells. She has hypercholesterolemia and type 2 diabetes mellitus. The patient received prophylactic perioperative antibiotics and opioid pain management during recovery. Her temperature is 37.9°C (98.9°F), pulse is 95/min, and blood pressure is 115/69 mm Hg. Examination shows a soft abdomen with mild tenderness to palpation in the left quadrants but no rebound tenderness or guarding. Bowel sounds are decreased. Rectal examination shows blood on the examining finger. Which of the following is the most likely underlying cause of this patient's symptoms?
- A. Embolization of superior mesenteric artery
- B. Atherosclerotic narrowing of the intestinal vessels
- C. Small outpouchings in the sigmoid wall
- D. Infection with Clostridioides difficile
- E. Decreased blood flow to the splenic flexure (Correct Answer)
Colorectal cancer resection principles Explanation: ***Decreased blood flow to the splenic flexure***
- This patient's symptoms are highly suggestive of **ischemic colitis**, which often affects the **splenic flexure** due to its "watershed" area vulnerability. **Cardiopulmonary bypass** and significant **intraoperative blood loss** (leading to hypotension and hypoperfusion) are major risk factors for this condition.
- The presentation with **crampy abdominal pain**, **urgent defecation**, and **bloody bowel movements** shortly after cardiac surgery points to colonic ischemia.
*Embolization of superior mesenteric artery*
- While an acute **SMA embolism** could cause severe abdominal pain and bloody stools, it typically presents with **more diffuse and severe abdominal tenderness**, often with marked tenderness disproportionate to examination findings early on, and rapid progression to peritonitis.
- The patient's history of valvular disease and hypercholesterolemia increases the risk of embolization, but the **mild tenderness confined to left quadrants** and decreased bowel sounds are less typical of an acute SMA occlusion.
*Atherosclerotic narrowing of the intestinal vessels*
- This describes **chronic mesenteric ischemia**, which typically causes **postprandial abdominal pain** (intestinal angina) and weight loss, not acute abdominal pain and bloody diarrhea in the immediate postoperative period.
- While the patient has risk factors for atherosclerosis (hypercholesterolemia, diabetes), the acute onset of symptoms following cardiac surgery points to an acute ischemic event rather than chronic narrowing.
*Small outpouchings in the sigmoid wall*
- This refers to **diverticulitis** or **diverticular bleeding**. While diverticular bleeding can cause painless or painful bleeding, and diverticulitis can cause abdominal pain, the acute onset post-cardiac surgery in the setting of hypoperfusion makes ischemic colitis a more likely diagnosis.
- Diverticulitis typically presents with **localized left lower quadrant pain**, fever, and leukocytosis, but the systemic context of recent cardiac surgery and hypoperfusion strongly favors ischemia.
*Infection with Clostridioides difficile*
- **_Clostridioides difficile_ infection** typically causes **watery diarrhea**, often after antibiotic use, and usually takes several days to develop symptoms after exposure or antibiotic initiation.
- Although the patient received perioperative antibiotics, the onset of symptoms within hours of surgery and the presence of **frank bloody stools** are less characteristic of _C. difficile_ infection, which is more commonly associated with non-bloody diarrhea.
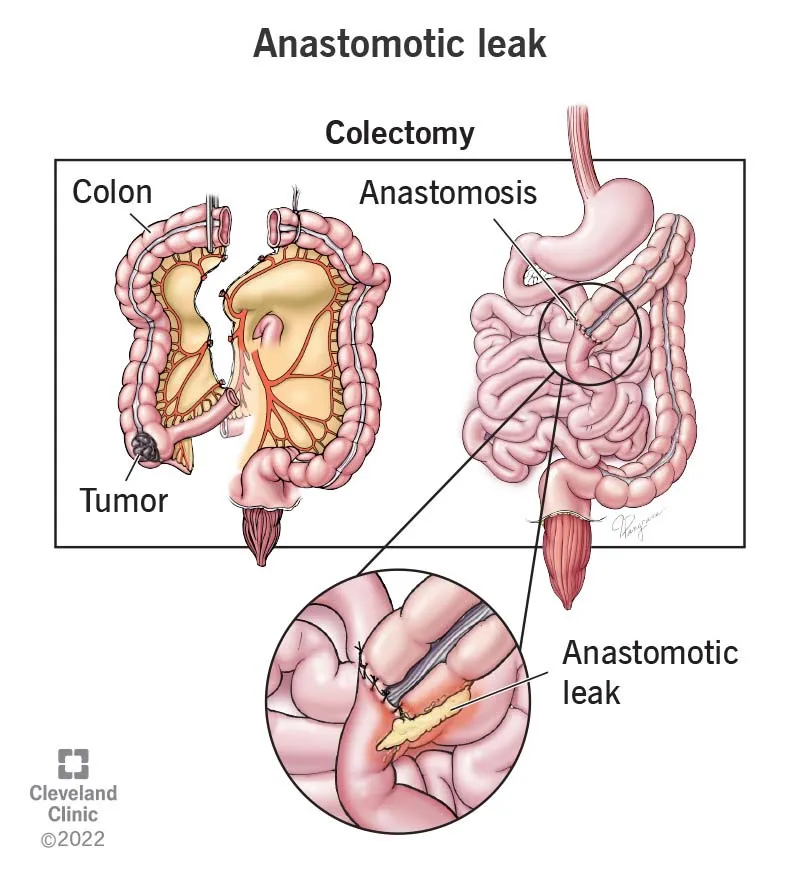
Colorectal cancer resection principles US Medical PG Question 4: Five days after undergoing an open colectomy and temporary colostomy for colon cancer, a 73-year-old man develops severe pain and swelling of the left calf. He was diagnosed with colon cancer 3 months ago. He has hypothyroidism and hypertension. His father died of colon cancer at the age of 68. He does not smoke. Prior to admission, his medications included levothyroxine, amlodipine, and carvedilol. Since the surgery, he has also been receiving unfractionated heparin, morphine, and piperacillin-tazobactam. He is 172 cm (5 ft 8 in) tall and weighs 101 kg (223 lb); BMI is 34.1 kg/m2. He appears uncomfortable. His temperature is 38.1°C (100.6°F), pulse is 103/min, and blood pressure is 128/92 mm Hg. Examination shows multiple necrotic lesions over bilateral thighs. The left calf is erythematous, tender, and swollen. Dorsiflexion of the left foot elicits pain behind the knee. The abdomen is soft and nontender. There is a healing midline incision and the colostomy is healthy and functioning. The remainder of the examination shows no abnormalities. Laboratory studies show:
Hemoglobin 13.6 g/dL
Leukocyte count 12,100/mm3
Platelet count 78,000/mm3
Prothrombin time 18 seconds (INR = 1.1)
Activated partial thromboplastin time 46 seconds
Serum
Na+ 138 mEq/L
Cl- 103 mEq/L
K+ 4.1 mEq/L
Urea nitrogen 18 mg/dL
Glucose 101 mg/dL
Creatinine 1.1 mg/dL
Which of the following is the most appropriate next step in management?
- A. Switch from unfractionated heparin to warfarin therapy
- B. Transfuse platelet concentrate
- C. Administer vitamin K
- D. Switch from unfractionated heparin to argatroban therapy (Correct Answer)
- E. Administer fresh frozen plasma
Colorectal cancer resection principles Explanation: ***Switch from unfractionated heparin to argatroban therapy***
- The patient's presentation with new **thrombosis (severe pain and swelling of the left calf)**, **thrombocytopenia (platelet count 78,000/mm3)**, and recent exposure to **unfractionated heparin (UFH)** is highly suggestive of **Heparin-Induced Thrombocytopenia (HIT) with thrombosis (HITT)**.
- In suspected or confirmed HIT, UFH must be immediately discontinued, and a **direct thrombin inhibitor (DTI)** like **argatroban** should be initiated to prevent further thrombosis.
*Switch from unfractionated heparin to warfarin therapy*
- While warfarin is used for long-term anticoagulation, it should **not be initiated as monotherapy in acute HIT** due to the risk of **venous limb gangrene** and further thrombosis during the initial phase of warfarin action (due to initial procoagulant effect).
- Warfarin can only be started **after platelet counts have recovered** and a non-heparin anticoagulant (like a DTI) has been administered for at least 5 days, given there is an overlap period.
*Transfuse platelet concentrate*
- Platelet transfusions are generally **contraindicated in HIT** because they can worsen the prothrombotic state by providing more substrate for platelet activation, potentially exacerbating thrombosis.
- Platelet transfusions are reserved for **life-threatening bleeding** in patients with HIT, which is not the case here.
*Administer vitamin K*
- Vitamin K is the antidote for **warfarin** overdose and has no role in the management of HIT. The patient's PT/INR is only mildly elevated, likely due to heparin and not warfarin, as he was not on warfarin.
- Administering vitamin K would not address the underlying pathology of HIT and would not be beneficial.
*Administer fresh frozen plasma*
- Fresh frozen plasma (FFP) contains clotting factors and is used to reverse coagulopathy in cases of **severe bleeding or factor deficiencies**, or for rapid reversal of warfarin.
- It is **not indicated for HIT**, as HIT is a prothrombotic condition involving platelet activation, not a deficiency in clotting factors that would be corrected by FFP.
Colorectal cancer resection principles US Medical PG Question 5: A 25-year-old woman presents to a physician for a new patient physical exam. Aside from occasional shin splints, she has a relatively unremarkable medical history. She takes oral contraceptive pills as scheduled and a multivitamin daily. She reports no known drug allergies. All of her age appropriate immunizations are up to date. Her periods have been regular, occurring once every 28 to 30 days with normal flow. She is sexually active with two partners, who use condoms routinely. She works as a cashier at the local grocery store. Her mother has diabetes and coronary artery disease, and her father passed away at age 45 after being diagnosed with colon cancer at age 40. Her grand-aunt underwent bilateral mastectomies after being diagnosed with breast cancer at age 60. Her physical exam is unremarkable. Which of the following is the best recommendation for this patient?
- A. Colonoscopy in 10 years
- B. Mammogram now
- C. Pap smear now
- D. Pap smear in 5 years
- E. HPV DNA testing now (Correct Answer)
Colorectal cancer resection principles Explanation: ***HPV DNA testing now***
- This 25-year-old patient is due for cervical cancer screening and this is the best recommendation.
- **ACOG (2021)** recommends **primary HPV testing every 5 years** for women aged 25-65 as the preferred screening method.
- Although USPSTF guidelines recommend starting HPV testing at age 30, ACOG's updated guidelines support initiating primary HPV testing at age 25, making this the most current evidence-based recommendation.
- Given she is presenting for a new patient physical and cervical cancer screening is due now, initiating HPV testing is appropriate.
*Colonoscopy in 10 years*
- While the patient's father was diagnosed with colon cancer at age 40, this option is **incorrectly timed**.
- Guidelines recommend screening beginning at age 40 OR 10 years before the youngest affected first-degree relative's diagnosis (age 30 for this patient), whichever comes first.
- Since this patient is 25, she would need colonoscopy at age 30 (in 5 years), not in 10 years (age 35).
- However, cervical cancer screening is the more immediate priority right now.
*Mammogram now*
- The patient's grand-aunt had breast cancer at age 60, but this is a **second-degree relative** with late-onset disease.
- This does not meet criteria for early mammography screening at age 25.
- Routine mammography typically begins at age 40 (per ACOG) or age 50 (per USPSTF), unless there is a strong family history in first-degree relatives or genetic mutations (BRCA1/2).
*Pap smear now*
- Pap smear (cytology) is an acceptable screening option for cervical cancer.
- **USPSTF (2018)** recommends cytology alone every 3 years for women ages 21-29, or starting HPV-based testing at age 30.
- However, **ACOG (2021)** supports primary HPV testing starting at age 25 as the preferred method.
- While Pap smear now would not be incorrect, HPV DNA testing is the preferred and more current guideline-based approach for this age group.
*Pap smear in 5 years*
- This represents inappropriate delay in initiating cervical cancer screening.
- Screening should begin now, not be deferred for 5 years.
- The 5-year interval applies to primary HPV testing once initiated, not to delaying the start of screening.
Colorectal cancer resection principles US Medical PG Question 6: A 36-year-old man undergoes ileocecal resection after a gunshot injury. The resected ileocecal segment is sent for histological evaluation. One of the slides derived from the specimen is shown in the image. Which of the following statements regarding the structure marked within the red circle is correct?
- A. This structure can be only found in the colon.
- B. These structures mostly contain M-cells.
- C. This structure can become a site of entry of certain microorganisms including S. typhi. (Correct Answer)
- D. This structure only appears in case of bacterial infection.
- E. Infants have the largest amount of these structures within their intestinal wall.
Colorectal cancer resection principles Explanation: ***This structure can become a site of entry of certain microorganisms including S. typhi.***
- The image illustrates **Peyer's patches**, which are lymphoid follicles found primarily in the ileum. These structures are rich in **M-cells**, which sample antigens from the intestinal lumen.
- While M-cells are crucial for initiating immune responses, some pathogens like *Salmonella typhi* exploit them to **translocate across the intestinal barrier** and disseminate, leading to systemic infection.
*This structure can be only found in the colon.*
- The structure shown is a **Peyer's patch**, which is predominantly found in the **ileum** of the small intestine, not exclusively in the colon.
- While lymphoid tissue is present throughout the GI tract, these large aggregated lymphoid nodules are characteristic of the ileum.
*These structures mostly contain M-cells.*
- While **M-cells (microfold cells)** are indeed present in the dome epithelium overlying Peyer's patches and are critical for antigen sampling, they constitute a minority of the cells within the entire structure.
- The bulk of Peyer's patches consists of **lymphocytes** (B cells, T cells), macrophages, and dendritic cells, forming lymphoid follicles and interfollicular areas.
*This structure only appears in case of bacterial infection.*
- **Peyer's patches** are a normal and permanent component of the gut-associated lymphoid tissue (GALT) and are present in healthy individuals.
- They serve as crucial sites for **immune surveillance** and the induction of adaptive immune responses to both commensal bacteria and pathogens, even in the absence of an active infection.
*Infants have the largest amount of these structures within their intestinal wall.*
- Peyer's patches are **well-developed at birth** and continue to increase in size and number during childhood and adolescence.
- They tend to **atrophy with age**, meaning that young adults and adolescents typically have the most prominent and numerous Peyer's patches, not infants.
Colorectal cancer resection principles US Medical PG Question 7: A 55-year-old woman is being managed on the surgical floor after having a total abdominal hysterectomy as a definitive treatment for endometriosis. On day 1 after the operation, the patient complains of fevers. She has no other complaints other than aches and pains from lying in bed as she has not moved since the procedure. She is currently receiving ondansetron, acetaminophen, and morphine. Her temperature is 101°F (38.3°C), blood pressure is 127/68 mmHg, pulse is 100/min, respirations are 17/min, and oxygen saturation is 94% on room air. Her abdominal exam is within normal limits and cardiopulmonary exam is only notable for mild crackles. Which of the following is the most likely etiology of this patient’s fever?
- A. Deep vein thrombosis
- B. Abscess formation
- C. Inflammatory stimulus of surgery (Correct Answer)
- D. Urinary tract infection
- E. Wound infection
Colorectal cancer resection principles Explanation: ***Inflammatory stimulus of surgery***
- Postoperative fever occurring within the first 24-48 hours after surgery, especially a major abdominal procedure, is most commonly due to the **systemic inflammatory response** to tissue trauma and stress from the surgery itself.
- The temperature of 101°F (38.3°C) is a common reactive fever. In this timeframe, **atelectasis** (part of the inflammatory response to surgery) is the classic cause, supported by the patient's **immobility since surgery** and **mild crackles** on exam.
- The patient has no other specific signs of infection, making this the most likely cause.
*Deep vein thrombosis*
- While DVT is a concern post-surgery, it typically presents with **leg pain, swelling, and tenderness**, not primarily as fever alone on day 1.
- A fever from DVT would usually indicate a more advanced complication like pulmonary embolism, which is inconsistent with the mild crackles and stable oxygen saturation.
*Abscess formation*
- Abscesses usually take several days to form and present with significant fevers, localized pain, and possibly purulent drainage, not typically within the first **24 hours post-op**.
- The abdominal exam is noted as within normal limits, making an abscess unlikely at this early stage.
*Urinary tract infection*
- UTIs are common post-op, especially with catheterization, but typically present with **dysuria, frequency, urgency**, and sometimes suprapubic pain, which are absent here.
- While fever can be a symptom, the lack of urinary complaints makes it a less likely primary diagnosis on day 1.
*Wound infection*
- Wound infections rarely develop within the first **24-48 hours** post-surgery, as bacteria require time to proliferate and cause inflammatory signs.
- Typical signs include **erythema, warmth, tenderness, and purulent drainage** at the incision site, which are not mentioned.
Colorectal cancer resection principles US Medical PG Question 8: A newborn boy born vaginally to a healthy 37-year-old G3P1 from a pregnancy complicated by hydramnios fails to pass meconium after 24 hours of life. The vital signs are within normal limits for his age. The abdomen is distended, the anus is patent, and the rectal examination reveals pale mucous with non-pigmented meconium. Based on a barium enema, the boy is diagnosed with sigmoid colonic atresia. Disruption of which structure during fetal development could lead to this anomaly?
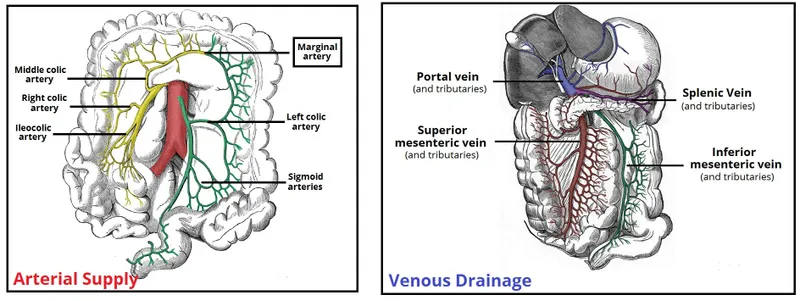
- A. Inferior mesenteric artery (Correct Answer)
- B. Superior mesenteric artery
- C. Vitelline duct
- D. Cloaca
- E. Celiac artery
Colorectal cancer resection principles Explanation: ***Inferior mesenteric artery***
- **Sigmoid colonic atresia**, as observed in this case, results from an ischemic event affecting the segment of the bowel supplied by the **inferior mesenteric artery** during fetal development.
- Interruption of blood flow to this region can lead to subsequent **atresia** as the affected part of the intestine necroses and is reabsorbed.
*Superior mesenteric artery*
- The **superior mesenteric artery** primarily supplies the midgut structures, including the small intestine and parts of the large intestine up to the transverse colon.
- Disruption of the superior mesenteric artery would typically lead to atresias higher up in the **gastrointestinal tract**, such as jejunal or ileal atresias, not sigmoid colonic atresia.
*Vitelline duct*
- The **vitelline duct** (also known as the omphalomesenteric duct) connects the midgut to the yolk sac during early fetal development.
- Persistent patency or partial obliteration of the vitelline duct can lead to anomalies like **Meckel's diverticulum** or vitelline cysts, which are distinct from colonic atresia.
*Cloaca*
- The **cloaca** is a common cavity for the digestive, urinary, and reproductive tracts during early embryonic development.
- Defects in cloacal development lead to complex malformations involving these systems, such as **imperforate anus** or persistent cloaca, rather than isolated colonic atresia with a patent anus.
*Celiac artery*
- The **celiac artery** supplies the foregut structures, including the stomach, duodenum, liver, and spleen.
- Disruption of the celiac artery during fetal development would result in malformations of these upper gastrointestinal organs, not the sigmoid colon.
Colorectal cancer resection principles US Medical PG Question 9: A 47-year-old woman is brought to the emergency department by her husband with the complaints of severe abdominal pain and discomfort. The pain began 2 days earlier, she describes it as radiating to her back and is associated with nausea. Her past medical history is significant for similar episodes of pain after fatty meals that resolved on its own. She drinks socially and has a 15 pack-year smoking history. Her pulse is 121/min, blood pressure is 121/71 mm Hg, and her temperature is 103.1°F (39.5°C). She has tenderness in the right upper quadrant and epigastrium with guarding and rebound tenderness. Bowel sounds are hypoactive. Part of a CBC is given below. What is the next best step in the management of this patient?
Hb%: 11 gm/dL
Total count (WBC): 13,400/mm3
Differential count:
Neutrophils: 80%
Lymphocytes: 15%
Monocytes: 5%
ESR: 45 mm/hr
C-reactive protein: 9.9 mg/dL (Normal < 3.0 mg/dL)
- A. Serum lipase levels
- B. Ultrasound of the gallbladder (Correct Answer)
- C. Erect abdominal X-ray
- D. Upper GI endoscopy
- E. Ultrasound of the appendix
Colorectal cancer resection principles Explanation: ***Ultrasound of the gallbladder***
- The patient presents with classic symptoms of **acute cholecystitis**, including severe right upper quadrant pain radiating to the back, fever, leukocytosis, and a history of similar pain after fatty meals.
- An ultrasound of the gallbladder is the **gold standard** for diagnosing cholecystitis, as it can visualize gallstones, gallbladder wall thickening, pericholecystic fluid, and sonographic Murphy's sign.
*Serum lipase levels*
- While pancreatic involvement can occur, **serum lipase** is primarily used to diagnose **pancreatitis**, which typically presents with more severe epigastric pain and may or may not involve gallstones.
- The clinical picture here is more suggestive of cholecystitis, where gallbladder imaging is the priority.
*Erect abdominal X-ray*
- An **erect abdominal X-ray** is useful for detecting **free air under the diaphragm** in cases of bowel perforation or to assess for bowel obstruction.
- It is not the primary diagnostic tool for cholecystitis, as gallstones are often radiolucent and it does not provide detailed information about the gallbladder wall or surrounding structures.
*Upper GI endoscopy*
- **Upper GI endoscopy** is indicated for evaluating **esophageal, gastric, or duodenal pathologies**, such as ulcers, gastritis, or tumors.
- While peptic ulcer disease can cause epigastric pain, the patient's symptoms, especially the radiation to the back, fever, and history of pain after fatty meals, are more consistent with gallbladder disease, making endoscopy a less immediate diagnostic step.
*Ultrasound of the appendix*
- An **ultrasound of the appendix** is primarily used to diagnose **appendicitis**, which typically presents with periumbilical pain migrating to the right lower quadrant.
- The patient's pain is localized to the right upper quadrant and epigastrium, making appendicitis highly unlikely.
Colorectal cancer resection principles US Medical PG Question 10: A 39-year-old man presents with painless swelling of the right testis and a sensation of heaviness. The physical examination revealed an intra-testicular solid mass that could not be felt separately from the testis. After a thorough evaluation, he was diagnosed with testicular seminoma. Which of the following group of lymph nodes are most likely involved?
- A. Superficial inguinal lymph nodes (lateral group)
- B. Deep inguinal lymph nodes
- C. Superficial inguinal lymph nodes (medial group)
- D. Para-rectal lymph nodes
- E. Para-aortic lymph nodes (Correct Answer)
Colorectal cancer resection principles Explanation: ***Para-aortic lymph nodes***
- The **testes** develop in the abdomen and descend into the scrotum, retaining their original lymphatic drainage. Therefore, **testicular cancer** typically metastasizes to the **para-aortic** (or retroperitoneal) lymph nodes, which are located near the renal veins at the level of L1-L2.
- This is the primary lymphatic drainage pathway for the testes.
*Superficial inguinal lymph nodes (lateral group)*
- These lymph nodes primarily drain the skin of the **scrotum**, perineum, and lower limbs, but not the **testes** themselves.
- Involvement would suggest spread to the scrotal skin or compromised lymphatic flow due to prior scrotal surgery or infection, which is not indicated here.
*Deep inguinal lymph nodes*
- **Deep inguinal lymph nodes** drain structures deeper in the leg and gluteal region, as well as receiving efferent vessels from the superficial inguinal nodes.
- They are not the primary drainage site for the **testes**.
*Superficial inguinal lymph nodes (medial group)*
- Similar to the lateral group, the **medial superficial inguinal lymph nodes** primarily drain the external genitalia (excluding the testes), perineum, and lower abdominal wall.
- They are not the direct drainage route for **testicular cancer**.
*Para-rectal lymph nodes*
- **Para-rectal lymph nodes** are located near the rectum and are involved in the drainage of the rectum and lower sigmoid colon.
- They have no direct connection to the lymphatic drainage of the **testes**.
More Colorectal cancer resection principles US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.