Point-of-care coagulation testing US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Point-of-care coagulation testing. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Point-of-care coagulation testing US Medical PG Question 1: A 35-year-old patient is brought into the emergency department post motor vehicle crash. Stabilization of the patient in the trauma bay requires endotracheal intubation. The patient has a laceration on the femoral artery from shrapnel and seems to have lost large quantities of blood. The patient is transfused with 13 units of packed red blood cells. His vitals are T 96.5, HR 150, BP 90/40. Even with the direct pressure on the femoral artery, the patient continues to bleed. Results of labs drawn within the last hour are pending. Which of the following is most likely to stop the bleeding in this patient?
- A. Normal saline
- B. Fresh frozen plasma and platelets (Correct Answer)
- C. Whole blood
- D. Dextrose
- E. Cryoprecipitate
Point-of-care coagulation testing Explanation: ***Fresh frozen plasma and platelets***
- This patient is experiencing **dilutional coagulopathy** due to massive transfusion of packed red blood cells, which lack clotting factors and platelets.
- **Fresh frozen plasma (FFP)** provides essential clotting factors, while **platelets** directly address thrombocytopenia, both crucial for **hemostasis**.
- This represents **standard component therapy** readily available in emergency departments.
*Normal saline*
- Administering normal saline would further dilute the remaining clotting factors and platelets, potentially **worsening the coagulopathy**.
- While essential for **volume resuscitation**, it does not provide any clotting components needed to stop bleeding.
*Whole blood*
- While **whole blood** contains red blood cells, plasma, and platelets in physiologic ratios, it is **not readily available** in most civilian trauma centers.
- Modern practice uses **component therapy** (FFP + platelets + PRBCs) which is more widely accessible and allows for targeted resuscitation.
- Low-titer O whole blood programs exist in some centers but are not universally available.
*Dextrose*
- **Dextrose solutions** primarily provide free water and glucose, used for hydration and hypoglycemia.
- It has **no hemostatic properties** and would further dilute clotting factors, exacerbating the bleeding.
*Cryoprecipitate*
- **Cryoprecipitate** is rich in **fibrinogen, factor VIII, factor XIII, and von Willebrand factor**.
- While useful for specific factor deficiencies or when fibrinogen is critically low in massive transfusions, it **does not replace all clotting factors or platelets** comprehensively as FFP and platelets would.
- Typically used as **adjunctive therapy** when fibrinogen levels are known to be low.
Point-of-care coagulation testing US Medical PG Question 2: An otherwise healthy 23-year-old man comes to the physician because of a 3-day history of mild persistent bleeding from the site of a tooth extraction. He has no prior history of medical procedures or surgeries and no history of easy bruising. He appears well. Vital signs are within normal limits. Laboratory studies show:
Hemoglobin 12.4 g/dL
Platelets 200,000/mm3
Serum
Prothrombin time 25 seconds
Partial thromboplastin time (activated) 35 seconds
Deficiency of which of the following coagulation factors is the most likely cause of this patient’s condition?
- A. Factor II
- B. Factor XIII
- C. Factor X
- D. Factor VII (Correct Answer)
- E. Factor V
Point-of-care coagulation testing Explanation: ***Factor VII***
- An **isolated prolonged PT** with a normal aPTT, platelets, and hemoglobin points to a defect in the **extrinsic pathway** of coagulation.
- **Factor VII** is the sole coagulation factor exclusively in the extrinsic pathway, making its deficiency the most likely cause.
*Factor II*
- **Factor II (prothrombin)** is a common pathway factor, so its deficiency would prolong both PT and aPTT.
- The patient's aPTT is normal, ruling out a significant deficiency of Factor II.
*Factor XIII*
- **Factor XIII** is responsible for stabilizing the fibrin clot but does not affect PT or aPTT.
- A deficiency would present with delayed bleeding or poor wound healing, not a prolonged PT.
*Factor X*
- **Factor X** is a common pathway factor, and its deficiency would prolong both PT and aPTT.
- The normal aPTT in this patient makes Factor X deficiency unlikely.
*Factor V*
- **Factor V** is a common pathway factor, and its deficiency would result in prolongation of both PT and aPTT.
- The normal aPTT makes a Factor V deficiency improbable.
Point-of-care coagulation testing US Medical PG Question 3: A 6-month-old male presents to the emergency department with his parents after his three-year-old brother hit him on the arm with a toy truck. His parents are concerned that the minor trauma caused an unusual amount of bruising. The patient has otherwise been developing well and meeting all his milestones. His parents report that he sleeps throughout the night and has just started to experiment with solid food. The patient’s older brother is in good health, but the patient’s mother reports that some members of her family have an unknown blood disorder. On physical exam, the patient is agitated and difficult to soothe. He has 2-3 inches of ecchymoses and swelling on the lateral aspect of the left forearm. The patient has a neurological exam within normal limits and pale skin with blue irises. An ophthalmologic evaluation is deferred.
Which of the following is the best initial step?
- A. Genetic testing
- B. Complete blood count and coagulation panel (Correct Answer)
- C. Ensure the child's safety and alert the police
- D. Peripheral blood smear
- E. Hemoglobin electrophoresis
Point-of-care coagulation testing Explanation: ***Complete blood count and coagulation panel***
- The unusual amount of **bruising** after minor trauma, along with a family history of an unknown blood disorder, strongly suggests a potential **bleeding disorder**. A **CBC** and a **coagulation panel** (PT, aPTT, fibrinogen) are essential initial steps to evaluate for abnormalities in platelets, clotting factors, or other hematologic conditions.
- These tests can help narrow down the differential diagnosis between **platelet dysfunction**, **coagulopathies** (like hemophilia or von Willebrand disease), or other less common bleeding disorders, guiding further specific investigations.
- **Important consideration:** The presence of **blue sclera** (described as "blue irises") raises concern for **osteogenesis imperfecta (OI)**, a connective tissue disorder causing bone fragility. However, initial hematologic screening is still appropriate given the family history of blood disorder and presentation of excessive bruising. If coagulation studies are normal, imaging and further workup for OI would be indicated.
*Genetic testing*
- While a genetic component is plausible given the patient's family history and clinical presentation (blue sclera may suggest osteogenesis imperfecta), **genetic testing** is typically performed *after* initial laboratory workup has identified a specific type of bleeding or inherited disorder.
- Starting with genetic testing without basic hematologic parameters is not the most efficient or cost-effective initial diagnostic approach.
*Ensure the child's safety and alert the police*
- While child abuse should always be considered in cases of unexplained or excessive bruising, the presence of a **family history of a blood disorder** and the **blue sclera** (suggesting possible osteogenesis imperfecta) make **medical causes** more immediate concerns for initial investigation.
- Pursuing a medical workup first often clarifies whether abuse is the primary explanation, although child protective services should be notified if suspicion remains high after medical evaluation.
*Peripheral blood smear*
- A **peripheral blood smear** provides information on red blood cell morphology, platelet size and number, and white blood cell differential. While useful in assessing for some hematologic conditions, it is often performed *after* a CBC has indicated abnormalities or in conjunction with specialized testing.
- It would not be the *best initial step* as it doesn't directly assess clotting factor function, which is critical in evaluating significant bruising severity.
*Hemoglobin electrophoresis*
- **Hemoglobin electrophoresis** is used to diagnose **hemoglobinopathies** like sickle cell anemia or thalassemia.
- The patient's symptoms (easy bruising) are not characteristic of hemoglobinopathies, and while he has pale skin, this test would not be the initial step to investigate a bleeding disorder.
Point-of-care coagulation testing US Medical PG Question 4: A 59-year-old woman comes to the physician because of left leg swelling that started after a transcontinental flight. A duplex ultrasound of the left leg shows a noncompressible popliteal vein. A drug is prescribed that inhibits the coagulation cascade. Two weeks later, laboratory studies show:
Platelet count 210,000/mm3
Partial thromboplastin time 28 seconds (normal: 25-35)
Prothrombin time 12 seconds (normal: 11-13)
Thrombin time 15 seconds (control: 15 seconds)
Which of the following drugs was most likely prescribed?
- A. Unfractionated heparin
- B. Apixaban
- C. Aspirin
- D. Warfarin
- E. Low molecular weight heparin (Correct Answer)
Point-of-care coagulation testing Explanation: ***Low molecular weight heparin***
- **LMWH (e.g., enoxaparin) is the first-line treatment for acute DVT** in ambulatory patients and is the most likely drug prescribed in this outpatient scenario
- LMWH enhances **antithrombin activity primarily against Factor Xa** (more than Factor IIa/thrombin), which is why it has **minimal effect on routine coagulation tests** (PT, PTT, TT)
- **Monitoring of LMWH is done via anti-Xa levels**, not PTT, PT, or TT, explaining why all these values remain normal two weeks after initiation
- The normal coagulation studies are **expected and consistent** with therapeutic LMWH use
*Unfractionated heparin*
- Unfractionated heparin (UFH) acts by enhancing **antithrombin activity against both Factor Xa and Factor IIa (thrombin)**, which significantly **prolongs PTT** (typically 1.5-2x control when therapeutic)
- UFH requires **IV administration and hospital monitoring**, making it unlikely for this ambulatory post-flight DVT patient
- If the patient were currently on UFH, the **PTT would be prolonged** (not normal as shown); if discontinued, this wouldn't be "the drug prescribed" for ongoing DVT treatment
*Apixaban*
- Apixaban is a **direct Factor Xa inhibitor** that would cause **mild prolongation of PT** and possibly PTT at therapeutic levels
- While it's a reasonable outpatient DVT treatment, the completely normal PT argues against current apixaban use
- Apixaban doesn't require routine monitoring, but when measured, coagulation times would typically show some abnormality
*Warfarin*
- Warfarin is a **vitamin K antagonist** that inhibits synthesis of factors II, VII, IX, and X, causing **significant PT/INR prolongation** (target INR 2-3 for DVT)
- The **normal PT (12 seconds) excludes warfarin** as the current medication
- Warfarin requires regular INR monitoring and would not show normal values at therapeutic doses
*Aspirin*
- Aspirin is an **antiplatelet agent** (COX-1 inhibitor) that affects platelet aggregation, **not the coagulation cascade**
- It has **no effect on PT, PTT, or TT** and is **inadequate monotherapy for DVT treatment**
- While it may have a role in extended VTE prevention, it would not be the primary drug prescribed for acute DVT
Point-of-care coagulation testing US Medical PG Question 5: A 71-year-old woman is brought to the emergency department following a syncopal episode. Earlier in the day, the patient had multiple bowel movements that filled the toilet bowl with copious amounts of bright red blood. Minutes later, she felt dizzy and lightheaded and collapsed into her daughter's arms. The patient has a medical history of diabetes mellitus and hypertension. Her temperature is 99.0°F (37.2°C), blood pressure is 155/94 mmHg, pulse is 82/min, respirations are 15/min, and oxygen saturation is 99% on room air. The patient's exam is notable for fecal occult blood positivity on rectal exam; however, the patient is no longer having bloody bowel movements. The patient's lungs are clear to auscultation and her abdomen is soft and nontender. Labs are ordered as seen below.
Hemoglobin: 7.1 g/dL
Hematocrit: 25%
Leukocyte count: 5,300/mm^3 with normal differential
Platelet count: 182,500/mm^3
Two large bore IV's are placed and the patient is given normal saline. What is the best next step in management?
- A. Packed red blood cells
- B. Type and screen (Correct Answer)
- C. Fresh frozen plasma
- D. CT abdomen
- E. Colonoscopy
Point-of-care coagulation testing Explanation: ***Type and screen***
- The patient has experienced a **significant colonic bleed** with associated **syncopal episode** and a **hemoglobin drop** to 7.1 g/dL. Before administering blood products, **blood typing and cross-matching** must be performed to ensure compatibility.
- This step is critical for **patient safety** to prevent transfusion reactions, especially given the likelihood of needing a transfusion soon.
- In the **sequence of acute blood loss management**, type and screen must be completed **before** packed red blood cells can be safely administered, making it the immediate next step after initial resuscitation with IV fluids.
*Packed red blood cells*
- While the patient will likely need **packed red blood cells (PRBCs)** due to severe anemia (Hb 7.1 g/dL) and hemodynamic instability (syncopal episode), PRBCs cannot be administered safely without first performing a **type and screen** to ensure compatibility.
- Administering PRBCs before compatibility testing is generally reserved for **life-threatening emergencies** with ongoing massive hemorrhage where there is no time for even an immediate cross-match (in which case O-negative blood would be used).
- This patient, while anemic, is currently **hemodynamically stable** (normal BP and pulse), allowing time for proper type and screen.
*Fresh frozen plasma*
- **Fresh frozen plasma (FFP)** is used to replace clotting factors in patients with **coagulopathies** or significant bleeding, often observed in massive transfusions or liver disease.
- This patient's **platelet count is normal** and there is no information to suggest a coagulopathy, thus FFP is not indicated as the immediate next step.
*CT abdomen*
- A **CT scan of the abdomen** may be useful later to identify the cause of the lower GI bleed, such as diverticulosis or angiodysplasia.
- However, the immediate priority is to **stabilize the patient hemodynamically** and address the acute blood loss before pursuing diagnostic imaging.
*Colonoscopy*
- A **colonoscopy** is the definitive diagnostic and potentially therapeutic procedure for a lower GI bleed.
- However, before performing a colonoscopy, the patient must be **hemodynamically stable**, which includes addressing their **anemia** and ensuring adequate blood product availability.
Point-of-care coagulation testing US Medical PG Question 6: A 65-year-old man presents to the emergency department by ambulance following a motor vehicle accident. He was a restrained passenger. At the hospital, he is bleeding heavily from a large wound in his left leg. A review of medical records reveals a history of atrial fibrillation for which he takes warfarin. His international normalized ratio (INR) 2 days ago was 2.6. On physical exam he is cool and clammy. The vital signs include: heart rate 130/min and blood pressure 96/54 mm Hg. Aggressive resuscitation with intravenous normal saline is begun. Which of the following is the next best step to correct this patient's underlying coagulopathy?
- A. Give platelets
- B. Give intravenous vitamin K
- C. Give fresh frozen plasma (FFP) (Correct Answer)
- D. Give cryoprecipitate
- E. Give packed red blood cells
Point-of-care coagulation testing Explanation: ***Give fresh frozen plasma (FFP)***
- This patient is in **hemorrhagic shock** due to severe bleeding while on **warfarin**, evidenced by tachycardia (HR 130), hypotension (BP 96/54), and cool/clammy skin with an INR of 2.6.
- **Fresh frozen plasma (FFP)** contains all vitamin K-dependent clotting factors (II, VII, IX, X) and is the best option **among those listed** to immediately reverse warfarin's effects in this life-threatening hemorrhage.
- FFP provides rapid reversal within minutes to hours, though it requires large volumes (10-15 mL/kg) and carries risk of transfusion-associated circulatory overload (TACO).
- **Note:** In modern practice, **4-factor prothrombin complex concentrate (PCC)** is preferred over FFP for warfarin reversal (faster, smaller volume, fewer complications), but it is not listed among the options here.
*Give intravenous vitamin K*
- **Vitamin K** reverses warfarin by enabling synthesis of vitamin K-dependent clotting factors (II, VII, IX, X).
- However, it takes **6-24 hours** to produce clinical effect, making it unsuitable as monotherapy for **life-threatening acute bleeding**.
- Vitamin K should be given as **adjunct therapy** alongside FFP, but cannot be the sole intervention in hemorrhagic shock.
*Give platelets*
- **Platelets** are indicated for **thrombocytopenia** (typically <50,000 in active bleeding) or **platelet dysfunction**.
- Warfarin affects **clotting factors**, not platelet count or function, so platelets will not reverse the coagulopathy.
- No indication of thrombocytopenia is mentioned in this case.
*Give cryoprecipitate*
- **Cryoprecipitate** contains **fibrinogen, Factor VIII, Factor XIII, von Willebrand factor, and fibronectin**.
- It does **not contain** the vitamin K-dependent factors (II, VII, IX, X) depleted by warfarin.
- Cryoprecipitate is used for **hypofibrinogenemia** (fibrinogen <100 mg/dL) in massive transfusion or DIC, not for warfarin reversal.
*Give packed red blood cells*
- **Packed red blood cells (PRBCs)** replace blood volume and improve oxygen-carrying capacity in hemorrhagic shock.
- While PRBCs are critical for managing hypovolemia, they **do not contain clotting factors** and will not correct the **warfarin-induced coagulopathy**.
- PRBCs should be transfused in this patient, but they must be combined with FFP to address the underlying bleeding disorder.
Point-of-care coagulation testing US Medical PG Question 7: A 58-year-old cirrhotic man with ascites undergoes large volume paracentesis (6 liters removed). Four hours later, he becomes hypotensive (BP 80/50 mmHg) and tachycardic (HR 115/min). Labs show: Cr 2.1 mg/dL (baseline 1.0), Na+ 128 mEq/L, Hct 38%. What is the most appropriate immediate management?
- A. 5% albumin 6-8 grams per liter of ascites removed (Correct Answer)
- B. Normal saline bolus 2 liters
- C. Octreotide and midodrine for hepatorenal syndrome
- D. Vasopressors to maintain blood pressure
- E. Re-infusion of filtered ascitic fluid
Point-of-care coagulation testing Explanation: ***5% albumin 6-8 grams per liter of ascites removed***
- This patient is experiencing **post-paracentesis circulatory dysfunction (PPCD)**, characterized by hypotension and **acute kidney injury** (doubled creatinine) following a large volume paracentesis (>5L).
- Administration of **intravenous albumin** is the gold standard treatement to expand the **effective arterial blood volume** and prevent further deterioration into hepatorenal syndrome.
*Normal saline bolus 2 liters*
- In cirrhotic patients, **crystalloids** are less effective as they rapidly redistribute into the **interstitial space** (third-spacing) and can worsen ascites/edema.
- Saline does not provide the **oncotic pressure** required to counteract the splanchnic vasodilation typical of PPCD.
*Octreotide and midodrine for hepatorenal syndrome*
- While these agents are used for **Hepatorenal Syndrome (HRS)**, the immediate priority in post-procedure hypotension is **volume expansion** to correct the circulatory dysfunction.
- These medications are typically reserved for patients who do not respond to **volume expansion with albumin** or meet specific criteria for type 1 HRS.
*Vasopressors to maintain blood pressure*
- Vasopressors like **norepinephrine** are generally considered after fluid resuscitation with **albumin** has failed to restore hemodynamic stability.
- Using pressors alone ignores the underlying **intravascular volume deficit** caused by the fluid shift after paracentesis.
*Re-infusion of filtered ascitic fluid*
- This is not a standard or recommended clinical practice due to risks of **infection**, **coagulopathy**, and lack of evidence for efficacy.
- The specific requirement in this pathology is **concentrated albumin** to maintain oncotic pressure, which ascitic fluid does not provide efficiently.
Point-of-care coagulation testing US Medical PG Question 8: A 42-year-old woman with prolonged vomiting from gastroparesis is admitted with weakness. Labs show: K+ 2.1 mEq/L, pH 7.51, HCO3- 42 mEq/L, Mg2+ 1.4 mg/dL. She receives 80 mEq of IV potassium chloride over 24 hours, but repeat K+ is 2.3 mEq/L. What explains the refractory hypokalemia?
- A. Secondary hyperaldosteronism from volume depletion
- B. Insufficient potassium replacement dose
- C. Ongoing losses from continued vomiting
- D. Metabolic alkalosis promoting intracellular potassium shift
- E. Hypomagnesemia preventing potassium retention (Correct Answer)
Point-of-care coagulation testing Explanation: ***Hypomagnesemia preventing potassium retention***
- Low **intracellular magnesium** inhibits **ROMK channels** in the renal collecting duct; without magnesium inhibition, these channels allow excessive **potassium secretion** into the urine.
- **Magnesium** is also a necessary cofactor for the **Na+/K+-ATPase pump**, which is required to transport potassium into the cells and maintain serum levels.
*Secondary hyperaldosteronism from volume depletion*
- While **volume depletion** triggers the **Renin-Angiotensin-Aldosterone System (RAAS)**, leading to potassium loss, it does not typically cause absolute refraction to supplementation in the presence of adequate IV fluids.
- Addressing the **volume status** alone will not fix the hypokalemia if the **magnesium deficiency** is still driving renal wasting.
*Insufficient potassium replacement dose*
- A dose of **80 mEq** over 24 hours is a significant amount of supplement for a patient who is hospitalized and being monitored.
- Failure to increase serum potassium by more than 0.2 mEq/L despite high-dose IV replacement suggests an **active wasting mechanism** rather than just an under-correction.
*Ongoing losses from continued vomiting*
- Although vomiting causes loss of **hydrochloric acid** and induces **metabolic alkalosis**, the gastric fluid itself contains relatively low concentrations of potassium.
- The primary cause of hypokalemia in vomiting is **renal loss** (due to alkalosis and RAAS) rather than direct loss of potassium from the stomach.
*Metabolic alkalosis promoting intracellular potassium shift*
- **Alkalosis** causes an intracellular shift of potassium as **hydrogen ions** exit cells to help buffer the serum pH.
- While this contributes to the initial low lab value, it does not explain why **exogenous IV potassium** fails to raise the serum concentration over a 24-hour period.
Point-of-care coagulation testing US Medical PG Question 9: A 65-year-old diabetic man with TURP syndrome presents with confusion, nausea, and seizures 2 hours post-operatively. Labs show: Na+ 115 mEq/L, serum osmolality 240 mOsm/kg. He weighs 70 kg. What is the target sodium correction rate and fluid management strategy?
- A. Conivaptan infusion for water diuresis
- B. Normal saline infusion with fluid restriction
- C. Rapid correction to 135 mEq/L with 3% hypertonic saline over 4 hours
- D. Increase sodium by 6-8 mEq/L in first 24 hours with 3% saline boluses
- E. 3% saline to increase sodium by 4-6 mEq/L in first 2-4 hours, then slower correction (Correct Answer)
Point-of-care coagulation testing Explanation: ***3% saline to increase sodium by 4-6 mEq/L in first 2-4 hours, then slower correction***
- For **acute symptomatic hyponatremia** (seizures, confusion) in **TURP syndrome**, a rapid initial rise of **4-6 mEq/L** is required to reverse cerebral edema and prevent herniation.
- After the initial stabilization, the rate is slowed to stay within **6-8 mEq/L per 24 hours** to mitigate the risk of **Osmotic Demyelination Syndrome (ODS)**.
*Conivaptan infusion for water diuresis*
- **Vaptans** are Vasopressin receptor antagonists typically used for **euvolemic hyponatremia** (SIADH) rather than acute, life-threatening hyponatremia.
- This treatment is too slow for a patient presenting with **seizures** and severe neurological compromise.
*Normal saline infusion with fluid restriction*
- **Normal saline (0.9%)** may worsen hyponatremia in high ADH states or be insufficient to rapidly increase sodium in a **hypervolemic** post-TURP state.
- **Fluid restriction** alone is an appropriate long-term strategy for mild cases but is contraindicated as primary therapy for **acute, symptomatic seizures**.
*Rapid correction to 135 mEq/L with 3% hypertonic saline over 4 hours*
- Correcting sodium to **normal levels (135 mEq/L)** too quickly represents an overcorrection that carries an extremely high risk of **pontine myelinolysis**.
- The goal of emergency treatment is **symptom reversal**, not immediate normalization of laboratory values.
*Increase sodium by 6-8 mEq/L in first 24 hours with 3% saline boluses*
- While 6-8 mEq/L is a safe 24-hour target, it does not prioritize the necessary **early rapid rise** needed in the first few hours for a patient having **seizures**.
- This approach lacks the specific **2-4 hour urgency** required to manage active intracranial pressure increases from acute hypotonicity.
Point-of-care coagulation testing US Medical PG Question 10: A 50-year-old man is 5 days post-operative from a Whipple procedure. He has had high nasogastric output (1500 mL/day) and has been NPO. Labs show: Na+ 132 mEq/L, K+ 2.9 mEq/L, Cl- 88 mEq/L, HCO3- 38 mEq/L, pH 7.52. Urine chloride is 8 mEq/L. What is the appropriate management?
- A. Discontinue nasogastric suction only
- B. Normal saline with potassium chloride (Correct Answer)
- C. Acetazolamide to promote bicarbonate excretion
- D. Half-normal saline with potassium supplementation
- E. Hydrochloric acid infusion
Point-of-care coagulation testing Explanation: ***Normal saline with potassium chloride***
- The patient has **hypochloremic, hypokalemic metabolic alkalosis** due to high-output gastric suctioning; a **urine chloride <10 mEq/L** confirms it is **chloride-responsive**.
- Administering **Isotonic Saline (0.9% NaCl)** restores volume and provides the chloride needed to promote renal **bicarbonate excretion**, while **KCl** corrects the hypokalemia that maintains alkalosis.
*Discontinue nasogastric suction only*
- While suctioning is the source of acid loss, stopping it alone does not address the existing **volume depletion** or the severe **electrolyte imbalances** already present.
- The kidneys require exogenous **chloride replacement** to effectively reverse the metabolic alkalosis and restore acid-base balance.
*Acetazolamide to promote bicarbonate excretion*
- This carbonic anhydrase inhibitor can lower bicarbonate but may worsen **hypokalemia** and contributes to further **volume depletion**.
- It is generally reserved for patients with severe volume overload who cannot tolerate saline, which is not the case for this **hypovolemic** patient.
*Half-normal saline with potassium supplementation*
- **0.45% Saline** provides less sodium and chloride than required for rapid volume expansion and correction of **contraction alkalosis**.
- **Isotonic 0.9% saline** is preferred to reliably expand the **extracellular fluid volume** and suppress the renin-angiotensin-aldosterone system.
*Hydrochloric acid infusion*
- This is an extreme measure reserved for life-threatening **metabolic alkalosis (pH >7.55-7.60)** that is refractory to standard saline and potassium replacement.
- It requires **central venous access** due to its caustic nature and is not indicated as initial management for **chloride-responsive** states.
More Point-of-care coagulation testing US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.
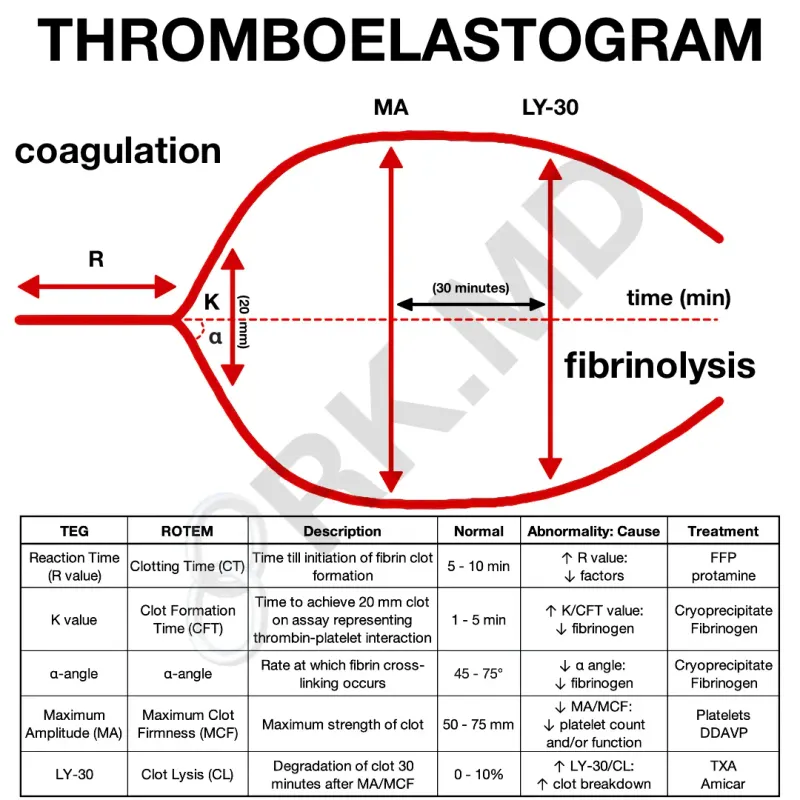 tracing with parameters R, K, alpha-angle, MA, and LY30 labeled)
tracing with parameters R, K, alpha-angle, MA, and LY30 labeled)
