Maintenance fluid requirements US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Maintenance fluid requirements. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Maintenance fluid requirements US Medical PG Question 1: A 61-year-old female with congestive heart failure and type 2 diabetes is brought to the emergency room by her husband because of an altered mental status. He states he normally helps her be compliant with her medications, but he had been away for several days. On physical exam, her temperature is 37.2 C, BP 85/55, and HR 130. Serum glucose is 500 mg/dL. Which of the following is the first step in the management of this patient?
- A. IV ½ NS
- B. IV insulin
- C. Subcutaneous insulin injection
- D. IV NS (Correct Answer)
- E. IV D5W
Maintenance fluid requirements Explanation: ***IV NS***
- The patient presents with **hypotension (85/55 mmHg)** and **tachycardia (130 bpm)**, indicating significant **volume depletion** despite a history of congestive heart failure.
- **Isotonic intravenous fluids (e.g., normal saline)** are crucial in the initial management of **diabetic ketoacidosis (DKA)** or **hyperosmolar hyperglycemic state (HHS)** to restore intravascular volume and improve tissue perfusion.
*IV ½ NS*
- **Hypotonic solutions** such as IV ½ NS are typically used later in DKA/HHS management, once the patient's **hemodynamic stability** has been achieved and serum sodium levels are stable or elevated.
- Administering hypotonic fluids to an already **hypotensive and volume-depleted patient** could worsen hypotension and potentially lead to cerebral edema if not carefully monitored.
*IV insulin*
- While insulin is essential for correcting hyperglycemia, it is administered **after or concurrently with fluid resuscitation** to avoid worsening hypovolemia as it drives glucose and potassium into cells, potentially causing **hypokalemia** and further **hemoconcentration**.
- **Fluid resuscitation** should always precede or be initiated simultaneously with insulin therapy, especially in cases of hemodynamic instability.
*Subcutaneous insulin injection*
- **Subcutaneous insulin** is not appropriate for initial management in this critically ill patient due to its **slower onset of action** and potentially **erratic absorption** in hypotensive and poorly perfused states.
- **Intravenous insulin** is preferred in DKA/HHS for its rapid, titratable effect.
*IV D5W*
- **Dextrose 5% in water (D5W)** is a hypotonic solution primarily used when **blood glucose levels fall below 250 mg/dL** during DKA/HHS treatment to prevent hypoglycemia.
- Administering D5W in a patient with a **serum glucose of 500 mg/dL** would further elevate blood sugar and worsen the hyperosmolar state.
Maintenance fluid requirements US Medical PG Question 2: A 45-year-old woman comes to the physician because of a 3-month history of worsening fatigue, loss of appetite, itching of the skin, and progressive leg swelling. Although she has been drinking 2–3 L of water daily, she has been passing only small amounts of urine. She has type 1 diabetes mellitus, chronic kidney disease, hypertension, and diabetic polyneuropathy. Her current medications include insulin, torasemide, lisinopril, and synthetic erythropoietin. Her temperature is 36.7°C (98°F), pulse is 87/min, and blood pressure is 138/89 mm Hg. She appears pale. There is 2+ pitting edema in the lower extremities. Sensation to pinprick and light touch is decreased over the feet and legs bilaterally. Laboratory studies show:
Hemoglobin 11.4 g/dL
Leukocyte count 6000/mm3
Platelet count 280,000/mm3
Serum
Na+ 137 mEq/L
K+ 5.3 mEq/L
Cl− 100 mEq/L
HCO3− 20 mEq/L
Urea nitrogen 85 mg/dL
Creatinine 8 mg/dL
pH 7.25
Which of the following long-term treatments would best improve quality of life and maximize survival in this patient?
- A. Peritoneal dialysis
- B. Living donor kidney transplant (Correct Answer)
- C. Cadaveric kidney transplant
- D. Hemofiltration
- E. Fluid restriction
Maintenance fluid requirements Explanation: ***Living donor kidney transplant***
- A **living donor kidney transplant** offers the best outcomes for **quality of life and survival** in eligible patients with end-stage renal disease (ESRD), particularly when compared to dialysis, due to better graft survival rates and reduced complications.
- The patient's symptoms (fatigue, itching, leg swelling, oliguria, high urea nitrogen, creatinine, hyperkalemia, metabolic acidosis) are consistent with **ESRD**, and while she has several comorbidities, she is not explicitly stated to have contraindications for transplantation.
*Peritoneal dialysis*
- While an effective treatment for ESRD, **dialysis generally provides lower quality of life** and survival benefits compared to successful kidney transplantation.
- She already has significant fluid overload symptoms and **oliguria**, making adequate fluid removal through peritoneal dialysis potentially challenging without strict management and impacting her overall well-being.
*Cadaveric kidney transplant*
- A **cadaveric kidney transplant** is a viable option and offers better outcomes than dialysis, but it generally has **poorer graft survival** and a longer wait time compared to a living donor transplant due to delayed graft function and cold ischemia time.
- Given the option, a **living donor transplant is superior** in terms of long-term outcomes and reduces the time spent on dialysis.
*Hemofiltration*
- **Hemofiltration is a form of renal replacement therapy**, similar to hemodialysis, often used in acute settings or for critically ill patients with severe fluid overload or electrolyte imbalances.
- While it can manage her symptoms, it is not a long-term treatment that **improves quality of life or maximizes survival** better than transplantation for ESRD.
*Fluid restriction*
- **Fluid restriction** is a supportive measure to manage fluid overload in patients with ESRD; however, it addresses symptoms rather than the underlying progressive renal failure.
- While necessary as part of supportive care, it does not offer a definitive long-term solution or improve survival for ESRD, which requires **renal replacement therapy or transplantation**.
Maintenance fluid requirements US Medical PG Question 3: A 23-year-old man presents to the emergency department for altered mental status after a finishing a marathon. He has a past medical history of obesity and anxiety and is not currently taking any medications. His temperature is 104°F (40°C), blood pressure is 147/88 mmHg, pulse is 200/min, respirations are 33/min, and oxygen saturation is 99% on room air. Physical exam reveals dry mucous membranes, hot flushed skin, and inappropriate responses to the physician's questions. Laboratory values are ordered as seen below.
Hemoglobin: 15 g/dL
Hematocrit: 44%
Leukocyte count: 8,500/mm^3 with normal differential
Platelet count: 199,000/mm^3
Serum:
Na+: 165 mEq/L
Cl-: 100 mEq/L
K+: 4.0 mEq/L
HCO3-: 22 mEq/L
BUN: 30 mg/dL
Glucose: 133 mg/dL
Creatinine: 1.5 mg/dL
Ca2+: 10.2 mg/dL
AST: 12 U/L
ALT: 10 U/L
Which of the following is the best next step in management?
- A. Lactated ringer
- B. Hypotonic saline
- C. 50% normal saline 50% dextrose
- D. Normal saline (Correct Answer)
- E. Dextrose solution
Maintenance fluid requirements Explanation: ***Normal saline***
- The patient presents with **heat stroke** (temperature 104°F, altered mental status after marathon) complicated by **severe hypernatremia (Na+ 165 mEq/L)** and **hypovolemia** (elevated BUN/Cr ratio, tachycardia, dry mucous membranes).
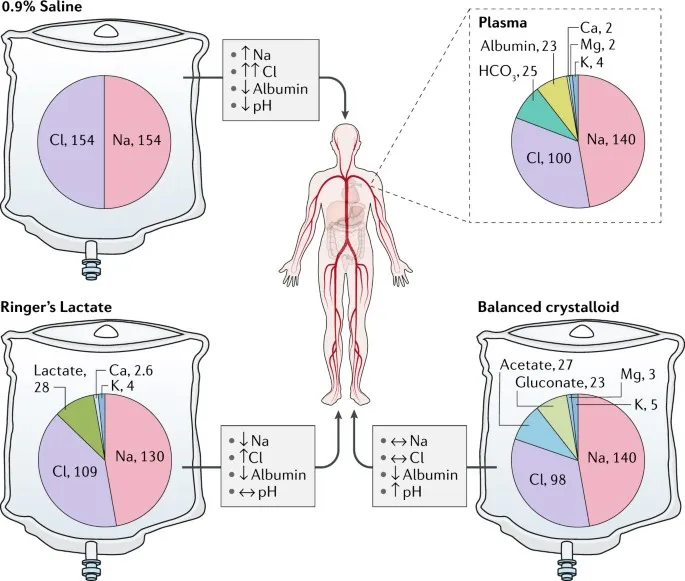
- In **hypovolemic hypernatremia**, the best initial step is to restore **intravascular volume** with **isotonic crystalloid** (normal saline or lactated Ringer's) to stabilize hemodynamics and organ perfusion.
- **Normal saline (0.9% NaCl, 154 mEq/L Na+)** is hypotonic relative to the patient's serum (165 mEq/L), so it will begin **gradual correction** of hypernatremia while providing volume resuscitation.
- After volume restoration, hypotonic fluids (0.45% saline or D5W) may be used for further correction, but they should NOT be given initially to a volume-depleted patient due to risk of worsening hypotension.
- Correction rate should be **≤10-12 mEq/L per 24 hours** to avoid cerebral edema.
*Hypotonic saline*
- While hypotonic saline (0.45% NaCl) is used to correct hypernatremia, it should **not** be the first-line choice in a **hypovolemic** patient.
- Administering hypotonic fluids to a volume-depleted patient can worsen hypotension and compromise organ perfusion before adequately restoring intravascular volume.
- Hypotonic saline is appropriate **after** volume status has been restored with isotonic fluids.
*Lactated ringer*
- **Lactated Ringer's solution** is an isotonic crystalloid (130 mEq/L Na+) and would be an equally acceptable choice for initial volume resuscitation.
- It is slightly more hypotonic than normal saline, which could provide marginally faster correction of hypernatremia.
- Either normal saline or lactated Ringer's is appropriate for initial management; normal saline is more commonly cited in USMLE resources for hypernatremia management.
*50% normal saline 50% dextrose*
- This mixture would create a **hypertonic solution** that could worsen hypernatremia rather than correct it.
- The patient's glucose is normal (133 mg/dL), so dextrose supplementation is not indicated.
- This option is inappropriate for managing hypernatremia.
*Dextrose solution*
- **D5W (5% dextrose in water)** provides free water and would correct hypernatremia by diluting serum sodium.
- However, in a **volume-depleted** patient, giving free water without adequate sodium can lead to rapid osmotic shifts, worsening hypotension, and potentially causing cerebral edema if correction occurs too rapidly.
- D5W is reserved for **euvolemic or hypervolemic hypernatremia**, not hypovolemic hypernatremia.
Maintenance fluid requirements US Medical PG Question 4: A 48-year-old woman is transferred from her primary care physician's office to the emergency department for further evaluation of hypokalemia to 2.5 mEq/L. She was recently diagnosed with hypertension 2 weeks ago and started on medical therapy. The patient said that she enjoys all kinds of food and exercises regularly, but has not been able to complete her workouts as she usually does. Her temperature is 97.7°F (36.5°C), blood pressure is 107/74 mmHg, pulse is 80/min, respirations are 15/min, and SpO2 is 94% on room air. Her physical exam is unremarkable. Peripheral intravenous (IV) access is obtained. Her basic metabolic panel is obtained below.
Serum:
Na+: 135 mEq/L
Cl-: 89 mEq/L
K+: 2.2 mEq/L
HCO3-: 33 mEq/L
BUN: 44 mg/dL
Glucose: 147 mg/dL
Creatinine: 2.3 mg/dL
Magnesium: 2.0 mEq/L
What is the next best step in management?
- A. Obtain an electrocardiogram (Correct Answer)
- B. Obtain urine sodium and creatinine
- C. Administer isotonic saline 1 liter via peripheral IV
- D. Administer potassium chloride 40mEq via peripheral IV
- E. Administer potassium bicarbonate 50mEq per oral
Maintenance fluid requirements Explanation: ***Obtain an electrocardiogram***
- The patient has severe **hypokalemia** (K+ 2.2 mEq/L), which requires urgent assessment for cardiac complications before initiating treatment.
- An **ECG is the mandatory first step** in severe hypokalemia (K+ <2.5 mEq/L) to evaluate for life-threatening arrhythmias and ECG changes including U waves, T wave flattening, ST depression, and QT prolongation.
- The patient is **hemodynamically stable** with only mild symptoms (exercise intolerance), so immediate potassium administration is not required before obtaining an ECG.
- ECG findings will guide the urgency and route of potassium repletion and determine the need for cardiac monitoring during treatment.
*Administer potassium chloride 40mEq via peripheral IV*
- While **IV potassium chloride** will be needed for repletion, it should be administered after ECG assessment in a stable patient.
- IV potassium administration carries risks including phlebitis, infiltration, and potential cardiac complications if given too rapidly without monitoring.
- In severe hypokalemia without cardiac arrest or documented life-threatening arrhythmias, obtaining an ECG first is standard practice.
*Obtain urine sodium and creatinine*
- Measuring **urine electrolytes** helps identify the cause of hypokalemia (likely diuretic-induced given recent hypertension treatment with metabolic alkalosis and hypochloremia).
- However, this diagnostic workup should follow the immediate assessment and treatment of severe hypokalemia.
- While useful for long-term management, it does not take priority over assessing cardiac risk with an ECG.
*Administer potassium bicarbonate 50mEq per oral*
- **Potassium bicarbonate** is contraindicated in this patient with **metabolic alkalosis** (HCO3- 33 mEq/L), as it would worsen the alkalosis.
- The correct form for repletion in metabolic alkalosis is **potassium chloride**, which addresses both the hypokalemia and hypochloremia.
- Oral repletion is also too slow for severe hypokalemia and may cause gastrointestinal side effects.
*Administer isotonic saline 1 liter via peripheral IV*
- While the patient shows signs of volume depletion (elevated BUN/Cr ratio, likely prerenal azotemia from diuretic use), the immediate priority is assessing the cardiac impact of severe hypokalemia.
- **Isotonic saline** without potassium supplementation could potentially worsen hypokalemia through dilution and increased renal potassium excretion.
- Volume resuscitation should be considered after ECG assessment and in conjunction with potassium repletion.
Maintenance fluid requirements US Medical PG Question 5: A 69-year-old male presents to the emergency department for slurred speech and an inability to use his right arm which occurred while he was eating dinner. The patient arrived at the emergency department within one hour. A CT scan was performed of the head and did not reveal any signs of hemorrhage. The patient is given thrombolytics and is then managed on the neurology floor. Three days later, the patient is recovering and is stable. He seems depressed but is doing well with his symptoms gradually improving as compared to his initial presentation. The patient complains of neck pain that has worsened slowly over the past few days for which he is being given ibuprofen. Laboratory values are ordered and return as indicated below:
Serum:
Na+: 130 mEq/L
K+: 3.7 mEq/L
Cl-: 100 mEq/L
HCO3-: 24 mEq/L
Urea nitrogen: 7 mg/dL
Glucose: 70 mg/dL
Creatinine: 0.9 mg/dL
Ca2+: 9.7 mg/dL
Urine:
Appearance: dark
Glucose: negative
WBC: 0/hpf
Bacterial: none
Na+: 320 mEq/L/24 hours
His temperature is 99.5°F (37.5°C), pulse is 95/min, blood pressure is 129/70 mmHg, respirations are 10/min, and oxygen saturation is 98% on room air. Which of the following is the best next step in management?
- A. Demeclocycline
- B. Fluid restriction (Correct Answer)
- C. Oral salt tablets
- D. Continue conservative management
- E. Conivaptan
Maintenance fluid requirements Explanation: ***Fluid restriction***
- The patient presents with **hyponatremia** (Na+ 130 mEq/L) and elevated urine sodium (320 mEq/L/24 hours) in the setting of recent stroke and possible SIADH (**Syndrome of Inappropriate Antidiuretic Hormone secretion**).
- **Fluid restriction** is the initial and most crucial step in managing euvolemic hyponatremia due to SIADH, reducing water intake to allow the kidney to excrete excess water and correct serum sodium.
*Demeclocycline*
- **Demeclocycline** is a tetracycline derivative that inhibits the action of ADH on renal tubules, used in chronic or refractory cases of SIADH.
- It is *not* the first-line treatment for acute, moderate hyponatremia, especially when fluid restriction has not yet been attempted.
*Oral salt tablets*
- **Oral salt tablets** would increase the solute load but would also draw water, potentially worsening hyponatremia if unrestricted fluid intake persists in SIADH.
- This intervention is generally not appropriate for **euvolemic hyponatremia** where the primary issue is excess free water.
*Continue conservative management*
- With a sodium level of 130 mEq/L, this is considered **mild to moderate hyponatremia** and requires active intervention to prevent potential neurological complications.
- Simply continuing conservative management without addressing the underlying **hyponatremia** or its cause would be inadequate and potentially harmful.
*Conivaptan*
- **Conivaptan** is an ADH receptor antagonist that can be used for persistent or significant hyponatremia in SIADH.
- It is typically reserved for more severe or refractory cases of hyponatremia and is usually administered intravenously, making it less suitable as a first-line outpatient management strategy.
Maintenance fluid requirements US Medical PG Question 6: A 35-year-old woman is brought to the emergency department 45 minutes after being rescued from a house fire. On arrival, she appears confused and has shortness of breath. The patient is 165 cm (5 ft 5 in) tall and weighs 55 kg (121 lb); BMI is 20 kg/m2. Her pulse is 125/min, respirations are 29/min, and blood pressure is 105/65 mm Hg. Pulse oximetry on room air shows an oxygen saturation of 97%. Examination shows second and third-degree burns over the anterior surfaces of the chest and abdomen, and the anterior surface of the upper extremities. There is black debris in the mouth and nose. There are coarse breath sounds over the lung bases. Cardiac examination shows no murmurs, rubs, or gallop. Femoral and pedal pulses are palpable bilaterally. Which of the following is the most appropriate fluid regimen for this patient according to the Parkland formula?
- A. Administer 4 liters of intravenous colloids over the next 8 hours
- B. Administer 5 liters of intravenous colloids over the next 6 hours
- C. Administer 5 liters of intravenous crystalloids over the next 6 hours
- D. Administer 8 liters of intravenous colloids over the next 12 hours
- E. Administer 6 liters of intravenous crystalloids over the next 24 hours (Correct Answer)
Maintenance fluid requirements Explanation: ***Administer 6 liters of intravenous crystalloids over the next 24 hours***
- The **Parkland formula** is 4 mL × weight (kg) × %TBSA burn. The patient's weight is 55 kg. The burns cover the anterior chest (9%), anterior abdomen (9%), and anterior surfaces of both upper extremities (4.5% + 4.5% = 9%), totaling **27% TBSA**.
- Calculation: 4 mL × 55 kg × 27% = **5,940 mL ≈ 6 liters**. Half is given in the first 8 hours (approximately 3 L), and the remaining half over the next 16 hours (approximately 3 L). Total fluid in 24 hours is approximately **6 liters of crystalloids**.
*Administer 4 liters of intravenous colloids over the next 8 hours*
- The Parkland formula primarily uses **crystalloids** (lactated Ringer's solution) for initial fluid resuscitation in burn patients, not colloids.
- Administering only 4 liters would be insufficient given the patient's 27% TBSA burn, and colloids are not first-line.
*Administer 5 liters of intravenous colloids over the next 6 hours*
- **Colloids** are not the first-line fluid for initial burn resuscitation under the Parkland formula; crystalloids are used.
- The timing of 6 hours does not align with the Parkland formula's 24-hour resuscitation period (half in first 8 hours, half in next 16 hours).
*Administer 5 liters of intravenous crystalloids over the next 6 hours*
- While **crystalloids** are appropriate, 5 liters over 6 hours represents an inappropriately rapid infusion rate that does not follow the Parkland formula timing.
- The first 8 hours should receive approximately 3 liters, not 5 liters over 6 hours, which could lead to complications such as **pulmonary edema or compartment syndrome**.
*Administer 8 liters of intravenous colloids over the next 12 hours*
- This option incorrectly specifies **colloids** instead of crystalloids as the primary fluid for burn resuscitation according to the Parkland formula.
- The volume of 8 liters exceeds the calculated requirement of 6 liters for this patient's 27% TBSA burn.
Maintenance fluid requirements US Medical PG Question 7: An 80-year-old male with known metastatic prostate cancer presents to your office with vague complaints of "achy bones." Strangely, he refers to you using the name of another physician. On physical exam, he is afebrile, but mildly tachycardic at 100 beats/min. Mucous membranes are dry. Cardiac exam shows regular rhythm and no murmurs. The patient has diffuse, nonfocal abdominal pain. He cannot articulate the correct date. You check the patient's serum calcium level, which is found to be 15.3 mg/dL. What is the best next step in management?
- A. Calcitonin
- B. Intravenous normal saline (Correct Answer)
- C. Furosemide
- D. Pamidronate
- E. Hemodialysis
Maintenance fluid requirements Explanation: ***Intravenous normal saline***
- The patient exhibits classic symptoms of **hypercalcemia** (vague bone aches, confusion, dry mucous membranes, tachycardia, diffuse nonfocal abdominal pain) in the context of metastatic prostate cancer and a severely elevated serum calcium level of 15.3 mg/dL.
- **Volume expansion with intravenous normal saline** is the initial and most crucial step in managing severe hypercalcemia, as it helps to restore hydration and promote renal calcium excretion.
*Calcitonin*
- **Calcitonin** can rapidly lower serum calcium by inhibiting osteoclastic bone resorption and increasing renal calcium excretion, but its effect is typically transient and less potent than initial hydration.
- It is often used as an adjunct to saline and bisphosphonates, especially in cases where a rapid but temporary decrease in calcium is needed.
*Furosemide*
- **Furosemide** (a loop diuretic) should only be considered *after* adequate volume repletion has been achieved, as it can worsen dehydration and electrolyte abnormalities if given prematurely.
- It works by inhibiting calcium reabsorption in the loop of Henle, but **dehydration must be corrected first** to ensure effective GFR and avoid electrolyte imbalance.
*Pamidronate*
- **Pamidronate** (a bisphosphonate) is a potent inhibitor of osteoclast-mediated bone resorption and is effective in long-term management of hypercalcemia of malignancy.
- However, its onset of action is slow (2-4 days) and therefore it is not the best *initial step* for acutely symptomatic and severely hypercalcemic patients.
*Hemodialysis*
- **Hemodialysis** is reserved for severe, refractory hypercalcemia, particularly in patients with **renal failure** who cannot handle large fluid loads or excrete calcium effectively.
- While effective, it is an invasive procedure and not typically the first-line treatment for hypercalcemia of malignancy in a patient with presumably intact renal function capable of responding to hydration.
Maintenance fluid requirements US Medical PG Question 8: On morning labs, a patient's potassium comes back at 5.9 mEq/L. The attending thinks that this result is spurious, and asks the team to repeat the electrolytes. Inadvertently, the medical student, intern, and resident all repeat the electrolytes that same morning. The following values are reported: 4.3 mEq/L, 4.2 mEq/L, and 4.2 mEq/L. What is the median potassium value for that patient that day including the first value?
- A. 4.3 mEq/L
- B. 4.65 mEq/L
- C. 4.25 mEq/L (Correct Answer)
- D. 1.7 mEq/L
- E. 4.2 mEq/L
Maintenance fluid requirements Explanation: ***4.25 mEq/L***
- The question asks for the median including **all four potassium values**: 5.9, 4.3, 4.2, and 4.2 mEq/L.
- To find the **median**, first arrange the values in ascending order: **4.2, 4.2, 4.3, 5.9**.
- With an **even number of values (4)**, the median is the **average of the two middle numbers**: (4.2 + 4.3) / 2 = **4.25 mEq/L**.
- This correctly represents the **central tendency** of all laboratory values obtained that day.
*4.3 mEq/L*
- This is the **third value** in the sorted dataset (4.2, 4.2, 4.3, 5.9).
- This would be the median if there were an **odd number of values**, where you would simply take the middle value.
- With an even number of data points, you must **average the two middle values** (4.2 and 4.3), not select just one.
*4.65 mEq/L*
- This value (4.65) would result from incorrectly averaging **4.3 and 5.9**, perhaps by mistakenly identifying these as the two middle values.
- This could also result from averaging the **minimum (4.2) and maximum (5.9)** values: (4.2 + 5.9) / 2 = 5.05, though neither calculation yields exactly 4.65.
- The median requires proper sorting and identification of the **true middle position(s)** in the dataset.
*1.7 mEq/L*
- This value has **no mathematical relationship** to the given data (5.9, 4.3, 4.2, 4.2 mEq/L).
- This is a distractor representing **severe hypokalemia**, which is not supported by any of the laboratory values obtained.
- This might represent the **range** (5.9 - 4.2 = 1.7), though range is typically reported as a difference, not a standalone value.
*4.2 mEq/L*
- This is the **mode** of the dataset (the most frequently occurring value, appearing three times).
- While mode is a valid measure of central tendency, the question specifically asks for the **median**, not the mode.
- The median of this dataset (4.2, 4.2, 4.3, 5.9) is **4.25 mEq/L**, not 4.2 mEq/L.
Maintenance fluid requirements US Medical PG Question 9: In a randomized controlled trial studying a new treatment, the primary endpoint (mortality) occurred in 14.4% of the treatment group and 16.7% of the control group. Which of the following represents the number of patients needed to treat to save one life, based on the primary endpoint?
- A. 1/(0.144 - 0.167)
- B. 1/(0.167 - 0.144) (Correct Answer)
- C. 1/(0.300 - 0.267)
- D. 1/(0.267 - 0.300)
- E. 1/(0.136 - 0.118)
Maintenance fluid requirements Explanation: ***1/(0.167 - 0.144)***
- The **Number Needed to Treat (NNT)** is calculated as **1 / Absolute Risk Reduction (ARR)**.
- The **Absolute Risk Reduction (ARR)** is the difference between the event rate in the control group (16.7%) and the event rate in the treatment group (14.4%), which is **0.167 - 0.144**.
*1/(0.144 - 0.167)*
- This calculation represents 1 divided by the **Absolute Risk Increase**, which would be relevant if the treatment increased mortality.
- The **NNT should always be a positive value**, indicating the number of patients to treat to prevent one adverse event.
*1/(0.300 - 0.267)*
- This option uses arbitrary numbers (0.300 and 0.267) that do not correspond to the given **mortality rates** in the problem.
- It does not reflect the correct calculation for **absolute risk reduction** based on the provided data.
*1/(0.267 - 0.300)*
- This option also uses arbitrary numbers not derived from the problem's data, and it would result in a **negative value** for the denominator.
- The difference between event rates of 0.267 and 0.300 is not present in the given information for this study.
*1/(0.136 - 0.118)*
- This calculation uses arbitrary numbers (0.136 and 0.118) that are not consistent with the reported **mortality rates** of 14.4% and 16.7%.
- These values do not represent the **Absolute Risk Reduction** required for calculating NNT in this specific scenario.
Maintenance fluid requirements US Medical PG Question 10: A boy with diabetic ketoacidosis is admitted to the pediatric intensive care unit for closer monitoring. Peripheral venous access is established. He is treated with IV isotonic saline and started on an insulin infusion. This patient is at the highest risk for which of the following conditions in the next 24 hours?
- A. Cerebral edema (Correct Answer)
- B. Intrinsic kidney injury
- C. Cognitive impairment
- D. Hyperkalemia
- E. Deep venous thrombosis
Maintenance fluid requirements Explanation: ***Cerebral edema***
- **Cerebral edema** is a severe and potentially fatal complication of **diabetic ketoacidosis (DKA)** treatment, particularly in children.
- It results from a rapid decrease in serum osmolality during treatment, causing water to shift into brain cells.
*Intrinsic kidney injury*
- While dehydration in DKA can lead to **prerenal acute kidney injury**, **intrinsic kidney injury** is less common as an acute risk directly from DKA treatment in the first 24 hours.
- Initial fluid resuscitation often improves renal perfusion, reducing the risk of intrinsic damage unless other predisposing factors are present.
*Cognitive impairment*
- Cognitive impairment after DKA is more commonly observed in the long term, potentially due to recurrent episodes or severe DKA with cerebral edema.
- It is not the most immediate and highest risk acute complication in the short-term (next 24 hours).
*Hyperkalemia*
- Patients with DKA typically present with **hyperkalemia** due to acidosis and insulin deficiency, which resolves with insulin therapy as potassium shifts back into cells.
- The more immediate risk during treatment, especially after initial fluid resuscitation and insulin, is **hypokalemia**, not hyperkalemia, due to the intracellular shift of potassium.
*Deep venous thrombosis*
- **Dehydration** and **hyperviscosity** associated with DKA can increase the risk of **thrombosis**, but **deep venous thrombosis** is not the highest or most immediate acute risk in the next 24 hours.
- **Cerebral edema** is a more specific and life-threatening complication directly related to the treatment of DKA in children.
More Maintenance fluid requirements US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.