GDFT Principles - Don't Just Guess, Assess!
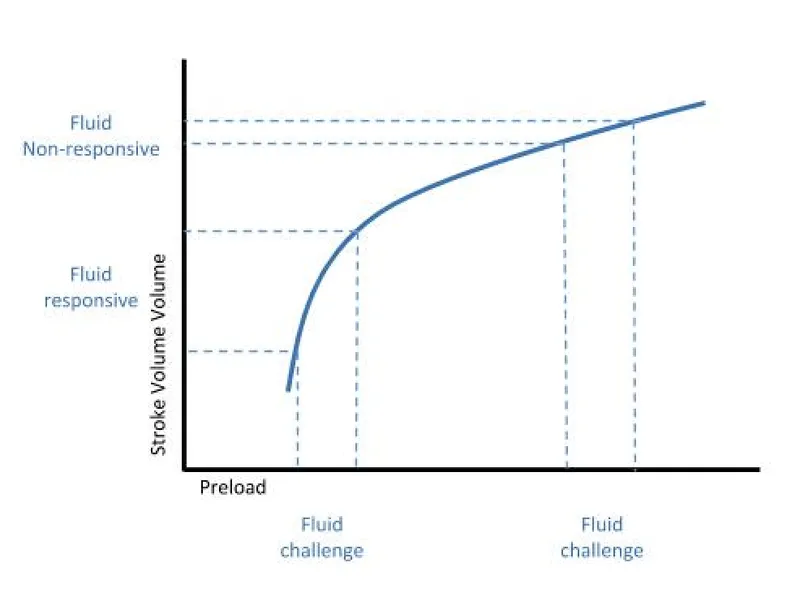
Goal-Directed Fluid Therapy (GDFT) shifts focus from static measures (e.g., CVP, PAOP) to dynamic assessments to predict fluid responsiveness. The goal is to administer fluids only to patients who will respond with an increase in stroke volume (SV), avoiding fluid overload.
- Dynamic Parameters:
- Stroke Volume Variation (SVV) / Pulse Pressure Variation (PPV): Variations > 10-15% in mechanically ventilated patients suggest fluid responsiveness.
- Passive Leg Raise (PLR): A reversible "fluid challenge." A significant ↑ in SV or cardiac output predicts responsiveness.
⭐ SVV and PPV are reliable only in controlled mechanical ventilation (tidal volume ≥ 8 mL/kg), sinus rhythm, and a closed chest. They are unreliable with spontaneous breathing or arrhythmias.
GDFT Monitoring - The Body's Dashboard
- Core Principle: Shift from static measures to dynamic assessments of fluid responsiveness.
| Parameter | Type | Utility in GDFT |
|---|---|---|
| CVP, PAOP | Static | Poor predictor of fluid responsiveness. |
| SVV, PPV | Dynamic | >10-15% suggests fluid responsiveness. |
| PLR, EEo | Dynamic | Assesses preload reserve without fluid bolus. |
| CO, SV | Dynamic | Direct measure of cardiac performance. |
| %%{init: {'flowchart': {'htmlLabels': true}}}%% | ||
| flowchart TD |
Start["📋 Assess Hemodynamics
• Evaluate stability• Initial check"]
Decision["📋 SVV/PPV > 13%?
• Fluid responsive?• Check variability"]
Fluid["💊 Administer Fluids
• Give fluid bolus• Increase preload"]
Pressors["💊 Pressors/Inotropes
• Consider vasopressors• Support contractility"]
Reassess["👁️ Re-assess SV/CO
• Check stroke volume• Cardiac output"]
Start --> Decision Decision -->|Yes| Fluid Decision -->|No| Pressors Fluid --> Reassess Pressors --> Reassess
style Start fill:#FEF8EC, stroke:#FBECCA, stroke-width:1.5px, rx:12, ry:12, color:#854D0E style Decision fill:#FEF8EC, stroke:#FBECCA, stroke-width:1.5px, rx:12, ry:12, color:#854D0E style Fluid fill:#F1FCF5, stroke:#BEF4D8, stroke-width:1.5px, rx:12, ry:12, color:#166534 style Pressors fill:#F1FCF5, stroke:#BEF4D8, stroke-width:1.5px, rx:12, ry:12, color:#166534 style Reassess fill:#EEFAFF, stroke:#DAF3FF, stroke-width:1.5px, rx:12, ry:12, color:#0369A1
> ⭐ **Exam Favorite:** Dynamic parameters (SVV, PPV, PLR) are superior to static pressures (CVP, PAOP) in predicting which patients will respond to a fluid challenge with an increase in stroke volume.
## GDFT in Action - The Fluid Algorithm
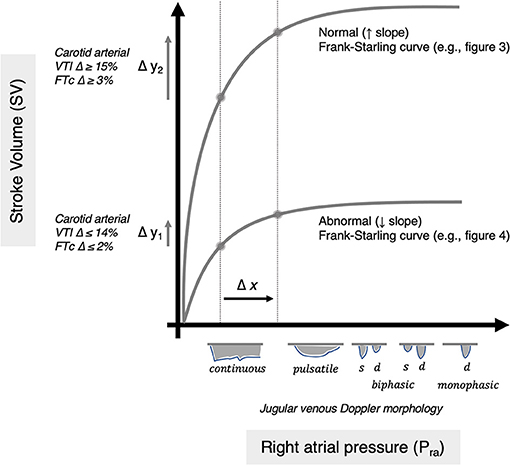
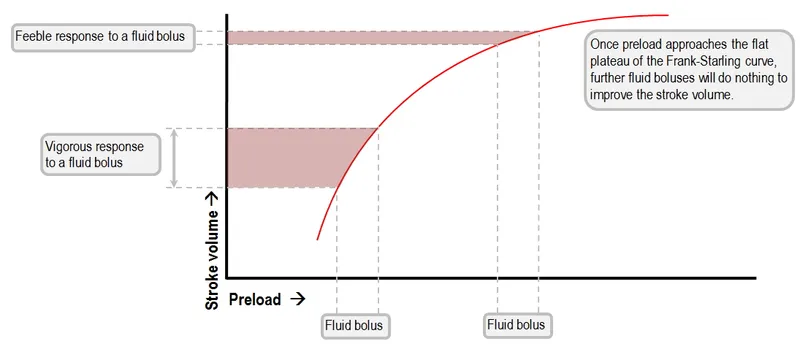
* **Core Principle:** Use dynamic assessments to guide fluid administration, avoiding both hypovolemia and fluid overload. The goal is to optimize cardiac output by placing the patient on the optimal portion of their Frank-Starling curve.
```mermaid
%%{init: {'flowchart': {'htmlLabels': true}}}%%
flowchart TD
Start["<b>⚠️ Hypotension</b><br><span style='display:block; text-align:left; color:#555'>• Hypoperfusion signs</span><span style='display:block; text-align:left; color:#555'>• Critical state</span>"]
Assess["<b>📋 Dynamic Assess</b><br><span style='display:block; text-align:left; color:#555'>• Fluid response</span><span style='display:block; text-align:left; color:#555'>• Hemodynamic check</span>"]
Check["<b>🔬 SVV or PPV?</b><br><span style='display:block; text-align:left; color:#555'>• SVV > 13 pct</span><span style='display:block; text-align:left; color:#555'>• PPV > 13 pct</span>"]
Fluid["<b>💊 Fluid Challenge</b><br><span style='display:block; text-align:left; color:#555'>• 250-500 mL IV</span><span style='display:block; text-align:left; color:#555'>• Use Crystalloid</span>"]
SVCheck["<b>🩺 Stroke Volume</b><br><span style='display:block; text-align:left; color:#555'>• SV ⬆️ by > 10 pct?</span><span style='display:block; text-align:left; color:#555'>• Measure output</span>"]
Pressors["<b>💊 Vasopressors</b><br><span style='display:block; text-align:left; color:#555'>• Consider pressors</span><span style='display:block; text-align:left; color:#555'>• Support pressure</span>"]
Goal["<b>✅ Target MAP</b><br><span style='display:block; text-align:left; color:#555'>• Maintain >= 65 mmHg</span><span style='display:block; text-align:left; color:#555'>• Final goal</span>"]
Start --> Assess
Assess --> Check
Check -->|YES| Fluid
Check -->|NO| Pressors
Fluid --> SVCheck
SVCheck -->|YES| Check
SVCheck -->|NO| Pressors
Pressors --> Goal
style Start fill:#FDF4F3, stroke:#FCE6E4, stroke-width:1.5px, rx:12, ry:12, color:#B91C1C
style Assess fill:#FEF8EC, stroke:#FBECCA, stroke-width:1.5px, rx:12, ry:12, color:#854D0E
style Check fill:#FFF7ED, stroke:#FFEED5, stroke-width:1.5px, rx:12, ry:12, color:#C2410C
style Fluid fill:#F1FCF5, stroke:#BEF4D8, stroke-width:1.5px, rx:12, ry:12, color:#166534
style SVCheck fill:#F7F5FD, stroke:#F0EDFA, stroke-width:1.5px, rx:12, ry:12, color:#6B21A8
style Pressors fill:#F1FCF5, stroke:#BEF4D8, stroke-width:1.5px, rx:12, ry:12, color:#166534
style Goal fill:#F6F5F5, stroke:#E7E6E6, stroke-width:1.5px, rx:12, ry:12, color:#525252
⭐ Exam Favorite: Dynamic assessments of fluid responsiveness (e.g., Stroke Volume Variation (SVV), Pulse Pressure Variation (PPV), passive leg raise) are superior to static measures (e.g., Central Venous Pressure (CVP), Pulmonary Capillary Wedge Pressure (PCWP)) in predicting which patients will respond to a fluid bolus.
Evidence & Outcomes - The Proof is in the Pudding
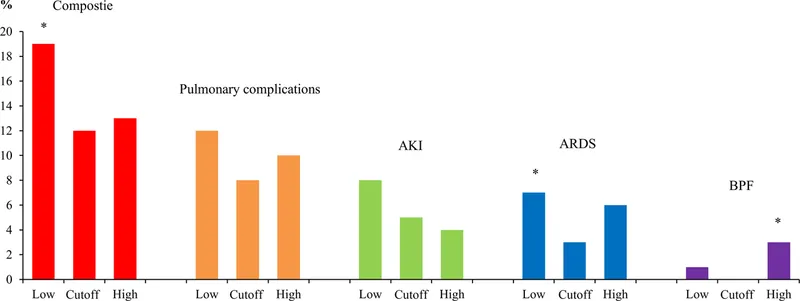
- GDFT significantly improves outcomes in major surgery and sepsis.
- Primary Benefits:
- ↓ Mortality rates
- ↓ Hospital length of stay
- ↓ Post-op complications (AKI, infections)
- Greatest impact in high-risk surgical patients and septic shock.
⭐ Studies show GDFT significantly reduces acute kidney injury (AKI) and surgical site infection (SSI) rates in patients undergoing major abdominal surgery.
High‑Yield Points - ⚡ Biggest Takeaways
- Goal-Directed Fluid Therapy (GDFT) titrates IV fluids to specific hemodynamic endpoints, moving beyond fixed-volume protocols.
- Its primary aim is to optimize oxygen delivery (DO₂) and prevent tissue hypoxia and end-organ damage.
- Utilizes dynamic parameters like stroke volume variation (SVV) or cardiac output to guide fluid administration.
- GDFT helps prevent both hypovolemia and deleterious fluid overload, improving patient outcomes.
- Key benefits include reduced postoperative complications, especially AKI and surgical site infections.
- Primarily indicated for high-risk surgical patients or those in septic shock.

