Fluid management in special populations US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Fluid management in special populations. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Fluid management in special populations US Medical PG Question 1: A 7-day-old male infant presents to the pediatrician for weight loss. There is no history of excessive crying, irritability, lethargy, or feeding difficulty. The parents deny any history of fast breathing, bluish discoloration of lips/nails, fever, vomiting, diarrhea, or seizures. He was born at full term by vaginal delivery without any perinatal complications and his birth weight was 3.6 kg (8 lb). Since birth he has been exclusively breastfed and passes urine six to eight times a day. His physical examination, including vital signs, is completely normal. His weight is 3.3 kg (7.3 lb); length and head circumference are normal for his age and sex. Which of the following is the next best step in the management of the infant?
- A. Reassurance of parents (Correct Answer)
- B. Evaluation of the mother for malnutrition
- C. Admission of the infant in the NICU to treat with empiric intravenous antibiotics
- D. Emphasize the need to clothe the infant warmly to prevent hypothermia
- E. Supplementation of breastfeeding with an appropriate infant formula
Fluid management in special populations Explanation: ***Reassurance of parents***
- A **weight loss of 8.3%** (300g from 3.6kg) is within the expected range for a 7-day-old exclusively breastfed infant, which can be up to 7-10% in the first week.
- The infant's normal physical exam, good urine output, and lack of other symptoms suggest **adequate feeding** and overall well-being.
*Evaluation of the mother for malnutrition*
- The mother's nutritional status is not directly indicative of the infant's weight loss within the normal physiological range in this scenario.
- There is no information to suggest the mother is malnourished or that it would directly impact the quality or quantity of breast milk to cause pathological weight loss.
*Admission of the infant in the NICU to treat with empiric intravenous antibiotics*
- This is an overly aggressive intervention as there are **no signs or symptoms of infection** (e.g., fever, lethargy, poor feeding) and the infant appears well.
- Empiric antibiotics are not warranted in an otherwise healthy, full-term infant with normal physiological weight loss.
*Emphasize the need to clothe the infant warmly to prevent hypothermia*
- The infant's **vital signs are normal**, indicating no hypothermia, and there is no clinical evidence to support this as a primary concern.
- While maintaining warmth is important, it is not the next best step for addressing this specific presentation of physiological weight loss.
*Supplementation of breastfeeding with an appropriate infant formula*
- Supplementation is typically not needed for physiological weight loss in an otherwise healthy, exclusively breastfed infant with **adequate urine output** and no signs of dehydration.
- Encouraging continued exclusive breastfeeding and providing support for proper latch and feeding techniques would be more appropriate if there were concerns about inadequate milk intake.
Fluid management in special populations US Medical PG Question 2: A physician at an internal medicine ward notices that several of his patients have hyponatremia without any associated symptoms. Severe hyponatremia, often defined as < 120 mEq/L, is associated with altered mental status, coma, and seizures, and warrants treatment with hypertonic saline. Because some patients are chronically hyponatremic, with serum levels < 120 mEq/L, but remain asymptomatic, the physician is considering decreasing the cutoff for severe hyponatremia to < 115 mEq/L. Changing the cutoff to < 115 mEq/L would affect the validity of serum sodium in predicting severe hyponatremia requiring hypertonic saline in which of the following ways?
- A. Increased sensitivity and decreased positive predictive value
- B. Increased specificity and decreased positive predictive value
- C. Decreased specificity and increased negative predictive value
- D. Increased specificity and decreased negative predictive value (Correct Answer)
- E. Decreased sensitivity and decreased positive predictive value
Fluid management in special populations Explanation: ***Increased specificity and decreased negative predictive value***
- **Increasing the cutoff from <120 to <115 mEq/L makes the diagnostic criteria MORE STRINGENT** (fewer patients classified as "severe").
- **Specificity INCREASES**: With a stricter cutoff, fewer patients without true severe disease (asymptomatic chronic hyponatremia) will be falsely labeled as "severe" and unnecessarily treated with hypertonic saline. Specificity measures the ability to correctly identify patients who do NOT have the target condition (symptomatic severe hyponatremia requiring treatment).
- **Negative Predictive Value (NPV) DECREASES**: Patients with sodium levels between 115-120 mEq/L will now test "negative" for severe hyponatremia (falling above the new threshold), but some of these patients may still develop symptoms requiring treatment. Therefore, a "negative" test result (Na >115) becomes less reliable at ruling out the need for future treatment, decreasing NPV.
- **Note**: Sensitivity will DECREASE (more symptomatic patients with Na 115-120 will be missed), and PPV will INCREASE (those identified as severe are more likely to truly need treatment).
*Increased sensitivity and decreased positive predictive value*
- Moving the cutoff to a more stringent value (<115 mEq/L) would **decrease sensitivity**, not increase it, because patients with sodium 115-120 mEq/L who have symptoms would be missed.
- The positive predictive value would **increase**, not decrease, because patients classified as "severe" under the stricter criteria are more likely to truly require hypertonic saline.
*Increased specificity and decreased positive predictive value*
- **Increased specificity** is correct, as explained above.
- However, **PPV would increase**, not decrease, with a more stringent cutoff. When fewer patients are classified as "severe," those who meet the stricter criteria are more likely to truly have severe disease requiring treatment.
*Decreased specificity and increased negative predictive value*
- Specificity would **increase**, not decrease, with stricter diagnostic criteria (fewer false positives).
- NPV would **decrease**, not increase, because patients just above the new threshold (Na 115-120) who test "negative" may still require treatment.
*Decreased sensitivity and decreased positive predictive value*
- **Decreased sensitivity** is correct—the stricter cutoff will miss symptomatic patients with sodium 115-120 mEq/L.
- However, **PPV would increase**, not decrease. With stricter criteria, patients identified as "severe" are more likely to truly have severe disease requiring hypertonic saline.
Fluid management in special populations US Medical PG Question 3: A 23-year-old man presents to the emergency department for altered mental status after a finishing a marathon. He has a past medical history of obesity and anxiety and is not currently taking any medications. His temperature is 104°F (40°C), blood pressure is 147/88 mmHg, pulse is 200/min, respirations are 33/min, and oxygen saturation is 99% on room air. Physical exam reveals dry mucous membranes, hot flushed skin, and inappropriate responses to the physician's questions. Laboratory values are ordered as seen below.
Hemoglobin: 15 g/dL
Hematocrit: 44%
Leukocyte count: 8,500/mm^3 with normal differential
Platelet count: 199,000/mm^3
Serum:
Na+: 165 mEq/L
Cl-: 100 mEq/L
K+: 4.0 mEq/L
HCO3-: 22 mEq/L
BUN: 30 mg/dL
Glucose: 133 mg/dL
Creatinine: 1.5 mg/dL
Ca2+: 10.2 mg/dL
AST: 12 U/L
ALT: 10 U/L
Which of the following is the best next step in management?
- A. Lactated ringer
- B. Hypotonic saline
- C. 50% normal saline 50% dextrose
- D. Normal saline (Correct Answer)
- E. Dextrose solution
Fluid management in special populations Explanation: ***Normal saline***
- The patient presents with **heat stroke** (temperature 104°F, altered mental status after marathon) complicated by **severe hypernatremia (Na+ 165 mEq/L)** and **hypovolemia** (elevated BUN/Cr ratio, tachycardia, dry mucous membranes).
- In **hypovolemic hypernatremia**, the best initial step is to restore **intravascular volume** with **isotonic crystalloid** (normal saline or lactated Ringer's) to stabilize hemodynamics and organ perfusion.
- **Normal saline (0.9% NaCl, 154 mEq/L Na+)** is hypotonic relative to the patient's serum (165 mEq/L), so it will begin **gradual correction** of hypernatremia while providing volume resuscitation.
- After volume restoration, hypotonic fluids (0.45% saline or D5W) may be used for further correction, but they should NOT be given initially to a volume-depleted patient due to risk of worsening hypotension.
- Correction rate should be **≤10-12 mEq/L per 24 hours** to avoid cerebral edema.
*Hypotonic saline*
- While hypotonic saline (0.45% NaCl) is used to correct hypernatremia, it should **not** be the first-line choice in a **hypovolemic** patient.
- Administering hypotonic fluids to a volume-depleted patient can worsen hypotension and compromise organ perfusion before adequately restoring intravascular volume.
- Hypotonic saline is appropriate **after** volume status has been restored with isotonic fluids.
*Lactated ringer*
- **Lactated Ringer's solution** is an isotonic crystalloid (130 mEq/L Na+) and would be an equally acceptable choice for initial volume resuscitation.
- It is slightly more hypotonic than normal saline, which could provide marginally faster correction of hypernatremia.
- Either normal saline or lactated Ringer's is appropriate for initial management; normal saline is more commonly cited in USMLE resources for hypernatremia management.
*50% normal saline 50% dextrose*
- This mixture would create a **hypertonic solution** that could worsen hypernatremia rather than correct it.
- The patient's glucose is normal (133 mg/dL), so dextrose supplementation is not indicated.
- This option is inappropriate for managing hypernatremia.
*Dextrose solution*
- **D5W (5% dextrose in water)** provides free water and would correct hypernatremia by diluting serum sodium.
- However, in a **volume-depleted** patient, giving free water without adequate sodium can lead to rapid osmotic shifts, worsening hypotension, and potentially causing cerebral edema if correction occurs too rapidly.
- D5W is reserved for **euvolemic or hypervolemic hypernatremia**, not hypovolemic hypernatremia.
Fluid management in special populations US Medical PG Question 4: The serum brain natriuretic peptide and N-terminal pro-BNP are elevated. A diagnosis of heart failure with preserved ejection fraction is made. In addition to supplemental oxygen therapy, which of the following is the most appropriate initial step in management?
- A. Intravenous dobutamine
- B. Intravenous furosemide therapy (Correct Answer)
- C. Intravenous morphine therapy
- D. Thoracentesis
- E. Intermittent hemodialysis
Fluid management in special populations Explanation: ***Intravenous furosemide therapy***
- Heart failure with **preserved ejection fraction (HFpEF)** often presents with **pulmonary congestion** due to elevated filling pressures.
- **Furosemide**, a loop diuretic, effectively reduces fluid overload and associated symptoms by increasing renal excretion of sodium and water.
*Intravenous dobutamine*
- **Dobutamine** is an inotropic agent that increases myocardial contractility and heart rate.
- It is typically used for **acute decompensated heart failure with low cardiac output** and is generally avoided in HFpEF unless there is significant hypoperfusion, as it can worsen myocardial oxygen demand and diastolic dysfunction.
*Intravenous morphine therapy*
- **Morphine** can be used in acute heart failure to reduce preload and anxiety, but it is not a primary treatment for the underlying fluid overload.
- It can cause respiratory depression and hypotension, and its use is typically reserved for patients with severe pain or dyspnea not adequately managed by other therapies.
*Thoracentesis*
- **Thoracentesis** is indicated for symptomatic **pleural effusions** causing respiratory distress.
- While pleural effusions can occur in heart failure, initial management of generalized fluid overload typically involves diuretics, making thoracentesis a secondary intervention if diuretic therapy is insufficient.
*Intermittent hemodialysis*
- **Intermittent hemodialysis** is an invasive procedure primarily used for severe renal failure or refractory fluid overload that has not responded to maximal diuretic therapy.
- It is not the initial step in managing heart failure with preserved ejection fraction and would only be considered in highly selected cases with **acute kidney injury** or diuretic resistance.
Fluid management in special populations US Medical PG Question 5: An 81-year-old man is admitted to the hospital due to acute decompensated heart failure. He has type 2 diabetes mellitus, hypertension, coronary artery disease, and congestive heart failure. Current medications include lisinopril, metformin, and low-dose aspirin. He has smoked one pack of cigarettes daily for 45 years. His temperature is 37.6°C (99.7°F), pulse is 105/min and regular, respirations are 21/min, and blood pressure is 103/64 mm Hg. Laboratory studies show:
Hemoglobin 13.7 g/dL
Leukocyte count 8200/mm3
Serum
Na+ 128 mEq/L
Cl- 98 mEq/L
K+ 4.9 mEq/L
Urea nitrogen 58 mg/dL
Glucose 200 mg/dL
Creatinine 2.2 mg/dL
Which of the following changes in the medication regimen is most appropriate in this patient at this time?
- A. Begin vancomycin therapy
- B. Discontinue aspirin therapy
- C. Begin nitroprusside therapy
- D. Discontinue metformin therapy (Correct Answer)
- E. Begin hydrochlorothiazide therapy
Fluid management in special populations Explanation: ***Discontinue metformin therapy***
- The patient has **acute decompensated heart failure** with **acute kidney injury** (creatinine 2.2 mg/dL, BUN 58 mg/dL). Metformin is **contraindicated in acute kidney injury** due to the significantly increased risk of **lactic acidosis**.
- With renal failure, metformin excretion is impaired, leading to drug accumulation and dangerous elevations in lactic acid levels. **Immediate discontinuation** is critical to prevent this life-threatening complication.
- Current guidelines recommend avoiding metformin when eGFR <30 mL/min or creatinine >1.5 mg/dL in males.
*Begin vancomycin therapy*
- There is **no indication of bacterial infection** (normal leukocyte count 8200/mm³, only mild temperature elevation to 37.6°C, no localizing signs).
- Initiating broad-spectrum antibiotics like vancomycin without clear evidence of infection contributes to **antibiotic resistance** and potential adverse effects.
*Discontinue aspirin therapy*
- The patient has a history of **coronary artery disease** and **congestive heart failure**, making him high risk for acute coronary events.
- Aspirin provides crucial **antiplatelet therapy** for secondary prevention of cardiovascular events in this patient population and should be continued.
*Begin nitroprusside therapy*
- Nitroprusside is a potent vasodilator used in **hypertensive emergencies** or severe heart failure with elevated blood pressure.
- This patient currently has **hypotension** (BP 103/64 mm Hg), and nitroprusside would further lower blood pressure, potentially causing cardiovascular collapse and end-organ hypoperfusion.
*Begin hydrochlorothiazide therapy*
- While diuretics are used in heart failure, hydrochlorothiazide is a **thiazide diuretic** primarily effective with preserved renal function (eGFR >30 mL/min).
- This patient has **elevated creatinine (2.2 mg/dL)**, indicating acute kidney injury, which would significantly limit the efficacy of hydrochlorothiazide. **Loop diuretics** (furosemide) would be more appropriate if diuresis is needed in the setting of renal impairment.
Fluid management in special populations US Medical PG Question 6: A 69-year-old male presents to the emergency department for slurred speech and an inability to use his right arm which occurred while he was eating dinner. The patient arrived at the emergency department within one hour. A CT scan was performed of the head and did not reveal any signs of hemorrhage. The patient is given thrombolytics and is then managed on the neurology floor. Three days later, the patient is recovering and is stable. He seems depressed but is doing well with his symptoms gradually improving as compared to his initial presentation. The patient complains of neck pain that has worsened slowly over the past few days for which he is being given ibuprofen. Laboratory values are ordered and return as indicated below:
Serum:
Na+: 130 mEq/L
K+: 3.7 mEq/L
Cl-: 100 mEq/L
HCO3-: 24 mEq/L
Urea nitrogen: 7 mg/dL
Glucose: 70 mg/dL
Creatinine: 0.9 mg/dL
Ca2+: 9.7 mg/dL
Urine:
Appearance: dark
Glucose: negative
WBC: 0/hpf
Bacterial: none
Na+: 320 mEq/L/24 hours
His temperature is 99.5°F (37.5°C), pulse is 95/min, blood pressure is 129/70 mmHg, respirations are 10/min, and oxygen saturation is 98% on room air. Which of the following is the best next step in management?
- A. Demeclocycline
- B. Fluid restriction (Correct Answer)
- C. Oral salt tablets
- D. Continue conservative management
- E. Conivaptan
Fluid management in special populations Explanation: ***Fluid restriction***
- The patient presents with **hyponatremia** (Na+ 130 mEq/L) and elevated urine sodium (320 mEq/L/24 hours) in the setting of recent stroke and possible SIADH (**Syndrome of Inappropriate Antidiuretic Hormone secretion**).
- **Fluid restriction** is the initial and most crucial step in managing euvolemic hyponatremia due to SIADH, reducing water intake to allow the kidney to excrete excess water and correct serum sodium.
*Demeclocycline*
- **Demeclocycline** is a tetracycline derivative that inhibits the action of ADH on renal tubules, used in chronic or refractory cases of SIADH.
- It is *not* the first-line treatment for acute, moderate hyponatremia, especially when fluid restriction has not yet been attempted.
*Oral salt tablets*
- **Oral salt tablets** would increase the solute load but would also draw water, potentially worsening hyponatremia if unrestricted fluid intake persists in SIADH.
- This intervention is generally not appropriate for **euvolemic hyponatremia** where the primary issue is excess free water.
*Continue conservative management*
- With a sodium level of 130 mEq/L, this is considered **mild to moderate hyponatremia** and requires active intervention to prevent potential neurological complications.
- Simply continuing conservative management without addressing the underlying **hyponatremia** or its cause would be inadequate and potentially harmful.
*Conivaptan*
- **Conivaptan** is an ADH receptor antagonist that can be used for persistent or significant hyponatremia in SIADH.
- It is typically reserved for more severe or refractory cases of hyponatremia and is usually administered intravenously, making it less suitable as a first-line outpatient management strategy.
Fluid management in special populations US Medical PG Question 7: A 35-year-old woman is brought to the emergency department 45 minutes after being rescued from a house fire. On arrival, she appears confused and has shortness of breath. The patient is 165 cm (5 ft 5 in) tall and weighs 55 kg (121 lb); BMI is 20 kg/m2. Her pulse is 125/min, respirations are 29/min, and blood pressure is 105/65 mm Hg. Pulse oximetry on room air shows an oxygen saturation of 97%. Examination shows second and third-degree burns over the anterior surfaces of the chest and abdomen, and the anterior surface of the upper extremities. There is black debris in the mouth and nose. There are coarse breath sounds over the lung bases. Cardiac examination shows no murmurs, rubs, or gallop. Femoral and pedal pulses are palpable bilaterally. Which of the following is the most appropriate fluid regimen for this patient according to the Parkland formula?
- A. Administer 4 liters of intravenous colloids over the next 8 hours
- B. Administer 5 liters of intravenous colloids over the next 6 hours
- C. Administer 5 liters of intravenous crystalloids over the next 6 hours
- D. Administer 8 liters of intravenous colloids over the next 12 hours
- E. Administer 6 liters of intravenous crystalloids over the next 24 hours (Correct Answer)
Fluid management in special populations Explanation: ***Administer 6 liters of intravenous crystalloids over the next 24 hours***
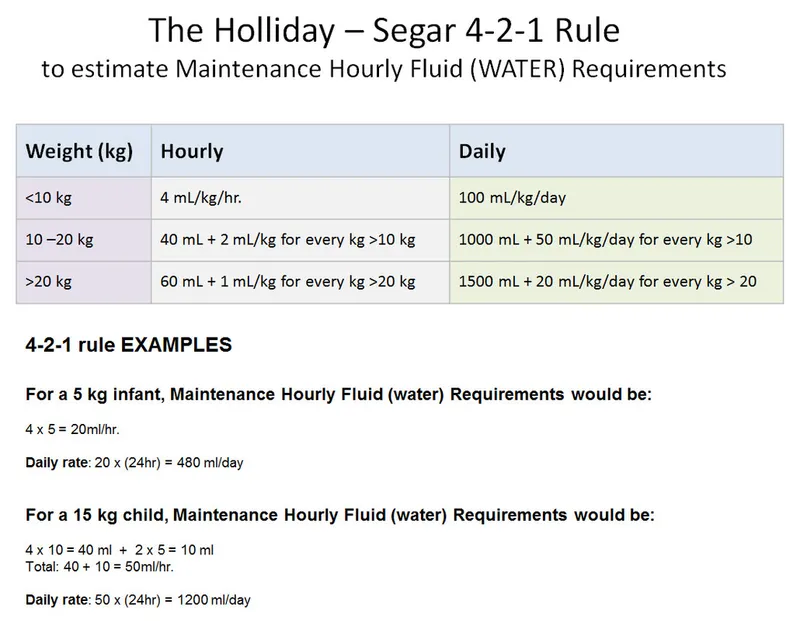
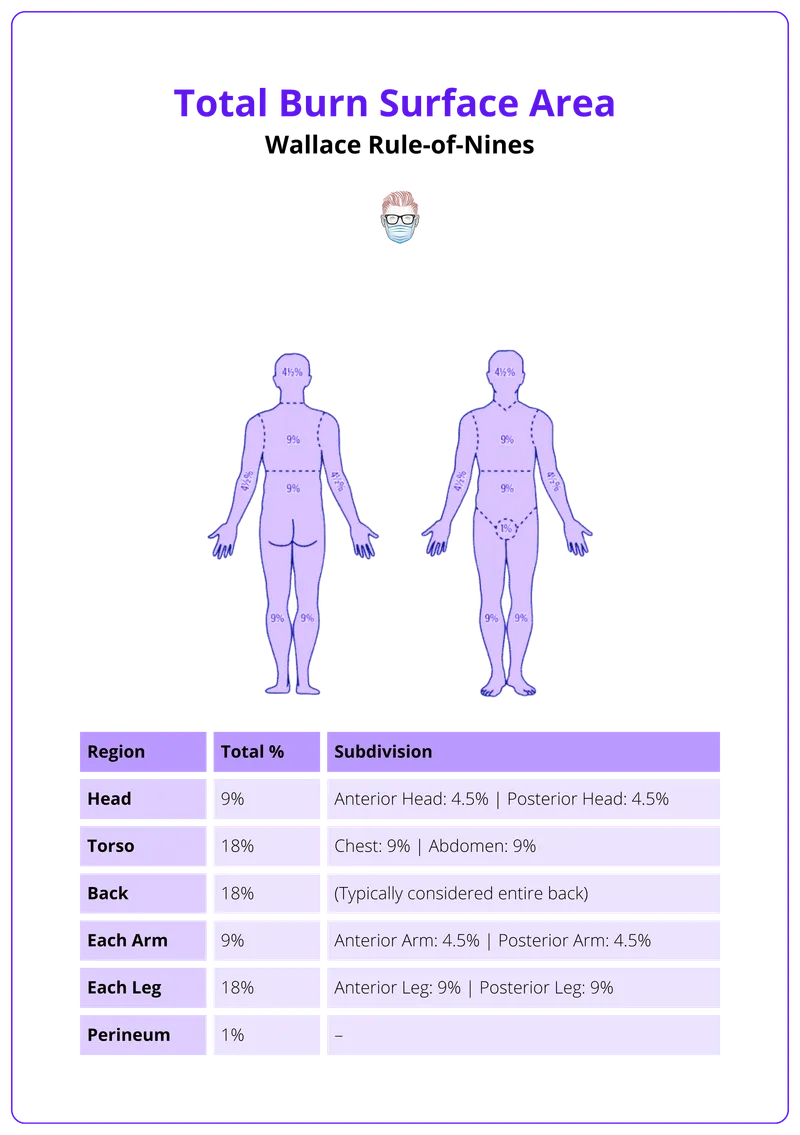
- The **Parkland formula** is 4 mL × weight (kg) × %TBSA burn. The patient's weight is 55 kg. The burns cover the anterior chest (9%), anterior abdomen (9%), and anterior surfaces of both upper extremities (4.5% + 4.5% = 9%), totaling **27% TBSA**.
- Calculation: 4 mL × 55 kg × 27% = **5,940 mL ≈ 6 liters**. Half is given in the first 8 hours (approximately 3 L), and the remaining half over the next 16 hours (approximately 3 L). Total fluid in 24 hours is approximately **6 liters of crystalloids**.
*Administer 4 liters of intravenous colloids over the next 8 hours*
- The Parkland formula primarily uses **crystalloids** (lactated Ringer's solution) for initial fluid resuscitation in burn patients, not colloids.
- Administering only 4 liters would be insufficient given the patient's 27% TBSA burn, and colloids are not first-line.
*Administer 5 liters of intravenous colloids over the next 6 hours*
- **Colloids** are not the first-line fluid for initial burn resuscitation under the Parkland formula; crystalloids are used.
- The timing of 6 hours does not align with the Parkland formula's 24-hour resuscitation period (half in first 8 hours, half in next 16 hours).
*Administer 5 liters of intravenous crystalloids over the next 6 hours*
- While **crystalloids** are appropriate, 5 liters over 6 hours represents an inappropriately rapid infusion rate that does not follow the Parkland formula timing.
- The first 8 hours should receive approximately 3 liters, not 5 liters over 6 hours, which could lead to complications such as **pulmonary edema or compartment syndrome**.
*Administer 8 liters of intravenous colloids over the next 12 hours*
- This option incorrectly specifies **colloids** instead of crystalloids as the primary fluid for burn resuscitation according to the Parkland formula.
- The volume of 8 liters exceeds the calculated requirement of 6 liters for this patient's 27% TBSA burn.
Fluid management in special populations US Medical PG Question 8: A 65-year-old woman is brought to the emergency department by her husband who found her lying unconscious at home. He says that the patient has been complaining of progressively worsening weakness and confusion for the past week. Her past medical history is significant for hypertension, systemic lupus erythematosus, and trigeminal neuralgia. Her medications include metoprolol, valsartan, prednisone, and carbamazepine. On admission, blood pressure is 130/70 mm Hg, pulse rate is 100 /min, respiratory rate is 17/min, and temperature is 36.5°C (97.7ºF). She regained consciousness while on the way to the hospital but is still drowsy and disoriented. Physical examination is normal. Finger-stick glucose level is 110 mg/dl. Other laboratory studies show:
Na+ 120 mEq/L (136—145 mEq/L)
K+ 3.5 mEq/L (3.5—5.0 mEq/L)
CI- 107 mEq/L (95—105 mEq/L)
Creatinine 0.8 mg/dL (0.6—1.2 mg/dL)
Serum osmolality 250 mOsm/kg (275—295 mOsm/kg)
Urine Na+ 70 mEq/L
Urine osmolality 350 mOsm/kg
She is admitted to the hospital for further management. Which of the following is the next best step in the management of this patient's condition?
- A. Rapid resuscitation with hypertonic saline (Correct Answer)
- B. Fluid restriction
- C. Tolvaptan
- D. Lithium
- E. Desmopressin
Fluid management in special populations Explanation: **Rapid resuscitation with hypertonic saline**
- The patient presents with **severe hyponatremia** (120 mEq/L) and neurological symptoms (drowsiness, disorientation, history of unconsciousness), indicating a need for **urgent correction** to prevent cerebral edema.
- **Hypertonic saline** (e.g., 3%) is indicated for severe symptomatic hyponatremia to rapidly increase serum sodium levels and reduce brain swelling.
*Fluid restriction*
- **Fluid restriction** is a conservative measure appropriate for **mild to moderate asymptomatic hyponatremia** or as an adjunct in SIADH management once severe symptoms are controlled.
- It would be too slow to address the patient's acute neurological symptoms and severe hyponatremia, potentially delaying critical treatment.
*Tolvaptan*
- **Tolvaptan** is a **vasopressin receptor antagonist** used in the treatment of **euvolemic or hypervolemic hyponatremia**, often in the context of SIADH.
- Its use is generally reserved for patients who have not responded to fluid restriction and is **contraindicated** in patients with severe symptoms or to rapidly correct severe hyponatremia due to the risk of overly rapid correction and osmotic demyelination syndrome.
*Lithium*
- **Lithium** is primarily used as a **mood stabilizer** in psychiatric conditions, particularly bipolar disorder.
- It can cause **nephrogenic diabetes insipidus** as a side effect and is not a treatment for hyponatremia.
*Desmopressin*
- **Desmopressin** is a synthetic analog of **antidiuretic hormone (ADH)** and is used to treat **diabetes insipidus** or nocturnal enuresis.
- Administering desmopressin would **worsen hyponatremia** by promoting water reabsorption, making it an inappropriate choice for this patient.
Fluid management in special populations US Medical PG Question 9: A 25-year-old woman presents to the physician with a complaint of several episodes of headaches in the past 4 weeks that are affecting her school performance. These episodes are getting progressively worse, and over-the-counter medications do not seem to help. She also mentions having to raise her head each time to look at the board while taking notes; she cannot simply glance up with just her eyes. She has no significant past medical or family history and was otherwise well prior to this visit. Physical examination shows an upward gaze palsy and convergence-retraction nystagmus. What structure is most likely to be affected in this patient?
- A. Aqueduct of Sylvius
- B. Inferior colliculi
- C. 3rd ventricle
- D. Tegmentum
- E. Corpora quadrigemina (Correct Answer)
Fluid management in special populations Explanation: ***Corpora quadrigemina***
- The patient presents with classic **Parinaud syndrome** (dorsal midbrain syndrome), characterized by **upward gaze palsy** and **convergence-retraction nystagmus**.
- These specific oculomotor signs result from direct damage to the **superior colliculi** and **pretectal area**, which are anatomical components of the **corpora quadrigemina** in the tectal region of the midbrain.
- The superior colliculi control vertical gaze, and the pretectal area coordinates pupillary reflexes and convergence movements. Compression or infiltration of this region (commonly by pineal tumors) produces the characteristic eye movement abnormalities.
- Progressive headaches indicate increased intracranial pressure, often from associated **aqueduct obstruction** causing hydrocephalus, which in turn compresses the tectal structures.
*Aqueduct of Sylvius*
- While obstruction of the aqueduct of Sylvius commonly **causes** Parinaud syndrome by leading to hydrocephalus and mass effect, the aqueduct itself is a CSF pathway and does not directly produce the eye movement abnormalities.
- The question asks which structure is "**affected**" - the affected structure producing these specific symptoms is the tectal region (corpora quadrigemina), not the obstructed aqueduct.
- This is an important distinction: the aqueduct is obstructed, but the corpora quadrigemina is compressed/affected.
*Inferior colliculi*
- The inferior colliculi are part of the corpora quadrigemina but serve the **auditory pathway**, not visual or oculomotor functions.
- Isolated lesions here would cause hearing deficits, not upward gaze palsy or convergence-retraction nystagmus.
*3rd ventricle*
- Lesions obstructing the third ventricle can cause hydrocephalus and headaches but do not directly affect the midbrain tectum unless they extend posteriorly.
- Third ventricular masses more commonly produce **endocrine disturbances** (hypothalamic-pituitary axis dysfunction) rather than the specific dorsal midbrain syndrome seen here.
*Tegmentum*
- The tegmentum is the ventral portion of the midbrain containing the **red nucleus**, **substantia nigra**, and **cranial nerve nuclei (III, IV)**.
- Tegmental lesions produce different oculomotor deficits (e.g., internuclear ophthalmoplegia, third nerve palsy) and movement disorders, not the dorsal midbrain syndrome pattern of Parinaud.
Fluid management in special populations US Medical PG Question 10: A 62-year-old man presents with multiple episodes of hemoptysis for a week. It is associated with generalized weakness, decreased appetite, and a 5.4 kg (12 lb) weight loss in 2 months. He has a smoking history of a pack a day for the last 47 years. Physical examination reveals pallor, while the rest of the results are within normal limits. Laboratory studies reveal decreased hemoglobin and a serum sodium value of 130 mEq/L. Chest X-ray shows a 3 cm rounded opaque shadow. Which of the following conditions is the patient most likely suffering from?
- A. Small cell carcinoma of the lung (Correct Answer)
- B. Squamous cell carcinoma of the lung
- C. Tuberculoma
- D. Lung abscess
- E. Adenocarcinoma of the lung
Fluid management in special populations Explanation: **Small cell carcinoma of the lung**
- The patient's presentation with **hemoptysis**, significant **weight loss**, and a long **smoking history** is highly suggestive of lung cancer.
- **Hyponatremia** (130 mEq/L) in this context often indicates **syndrome of inappropriate antidiuretic hormone secretion (SIADH)**, which is a common paraneoplastic syndrome associated with **small cell lung carcinoma**.
*Squamous cell carcinoma of the lung*
- While squamous cell carcinoma is strongly associated with smoking and can cause hemoptysis, it is less commonly linked to **SIADH and hyponatremia** compared to small cell carcinoma.
- This type of cancer is typically **centrally located** and can lead to **hypercalcemia** due to parathyroid hormone-related peptide (PTHrP) production, which is not seen here.
*Tuberculoma*
- A **tuberculoma** is a localized granuloma that can appear as a rounded opacity on X-ray, but it is less likely to cause significant **systemic symptoms** like profound weight loss and unexplained hyponatremia.
- **Hemoptysis** can occur with tuberculosis, but the overall clinical picture, especially the paraneoplastic features, points away from it.
*Lung abscess*
- A **lung abscess** typically presents with symptoms of infection such as **fever, purulent sputum**, and often a history of aspiration or pneumonia, which are absent here.
- The chest X-ray usually shows a **cavitated lesion with an air-fluid level**, and hyponatremia due to SIADH is not a common association.
*Adenocarcinoma of the lung*
- Although **adenocarcinoma** can cause hemoptysis and weight loss, it is typically more common in **non-smokers** or former smokers and often presents as a peripheral lesion.
- While it can be associated with paraneoplastic syndromes, **SIADH** and subsequent hyponatremia are much less frequent with adenocarcinoma compared to small cell lung carcinoma.
More Fluid management in special populations US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.