Electrolyte disorders (Na, K, Ca, Mg) US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Electrolyte disorders (Na, K, Ca, Mg). These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Electrolyte disorders (Na, K, Ca, Mg) US Medical PG Question 1: A 52-year-old woman is brought to the emergency department by her husband because of weakness, abdominal pain, and a productive cough for 4 days. She also reports increased urination for the past 2 days. This morning, she had nausea and five episodes of vomiting. She has type 1 diabetes mellitus and hypertension. Current medications include insulin and lisinopril. She admits to have forgotten to take her medication in the last few days. Her temperature is 38.4°C (101.1°F), pulse is 134/min, respirations 31/min, and blood pressure is 95/61 mm Hg. Examination shows dry mucous membranes and decreased skin turgor. Abdominal examination shows diffuse tenderness with no guarding or rebound. Bowel sounds are normal. Laboratory studies show:
Serum
Na+ 139 mEq/L
K+ 5.3 mEq/L
Cl- 106 mEq/L
Glucose 420 mg/dL
Creatinine 1.0 mg/dL
Urine
Blood negative
Glucose 4+
Ketones 3+
Arterial blood gas analysis on room air shows:
pH 7.12
pCO2 17 mm Hg
pO2 86 mm Hg
HCO3- 12 mEq/L
Which of the following is the most likely underlying cause of this patient's increased potassium?
- A. Muscle cell breakdown
- B. Extracellular potassium shift (Correct Answer)
- C. Repeated vomiting
- D. Increased renal potassium absorption
- E. Intracellular potassium shift
Electrolyte disorders (Na, K, Ca, Mg) Explanation: ***Extracellular potassium shift***
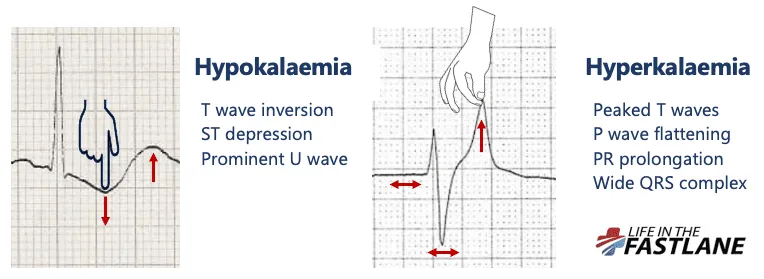
- The patient's **diabetic ketoacidosis (DKA)** leads to severe **acidosis (pH 7.12)**. In acidosis, hydrogen ions shift into cells, causing potassium to shift out of cells into the extracellular fluid to maintain electroneutrality, leading to **hyperkalemia** [2], [3].
- Additionally, the lack of insulin in DKA impairs the **Na+/K+-ATPase pump**, which normally moves potassium into cells, further contributing to extracellular potassium accumulation [2].
*Muscle cell breakdown*
- While significant muscle cell breakdown (e.g., in rhabdomyolysis) can release intracellular potassium into the circulation, there is no evidence of muscle injury in this patient.
- The primary driver of hyperkalemia in this context is metabolic acidosis and insulin deficiency, not muscle breakdown.
*Repeated vomiting*
- Repeated vomiting typically causes **hypokalemia** due to loss of gastric acid and subsequent renal potassium wasting [1].
- This patient's potassium is elevated, and while she did vomit, it is not the cause of hyperkalemia.
*Increased renal potassium absorption*
- Increased renal potassium absorption is not a typical physiological response to DKA and would usually be seen in conditions causing **hypovolemia with increased aldosterone** or certain **renal tubular acidosis** types, which are not the primary issue here.
- In DKA, the body tries to excrete excess potassium through the kidneys, although this can be impaired by reduced renal perfusion due to dehydration [3].
*Intracellular potassium shift*
- An intracellular potassium shift would lead to **hypokalemia**, not the hyperkalemia observed in this patient.
- Conditions like **alkalosis** or **insulin administration** cause potassium to move into cells.
Electrolyte disorders (Na, K, Ca, Mg) US Medical PG Question 2: A physician at an internal medicine ward notices that several of his patients have hyponatremia without any associated symptoms. Severe hyponatremia, often defined as < 120 mEq/L, is associated with altered mental status, coma, and seizures, and warrants treatment with hypertonic saline. Because some patients are chronically hyponatremic, with serum levels < 120 mEq/L, but remain asymptomatic, the physician is considering decreasing the cutoff for severe hyponatremia to < 115 mEq/L. Changing the cutoff to < 115 mEq/L would affect the validity of serum sodium in predicting severe hyponatremia requiring hypertonic saline in which of the following ways?
- A. Increased sensitivity and decreased positive predictive value
- B. Increased specificity and decreased positive predictive value
- C. Decreased specificity and increased negative predictive value
- D. Increased specificity and decreased negative predictive value (Correct Answer)
- E. Decreased sensitivity and decreased positive predictive value
Electrolyte disorders (Na, K, Ca, Mg) Explanation: ***Increased specificity and decreased negative predictive value***
- **Increasing the cutoff from <120 to <115 mEq/L makes the diagnostic criteria MORE STRINGENT** (fewer patients classified as "severe").
- **Specificity INCREASES**: With a stricter cutoff, fewer patients without true severe disease (asymptomatic chronic hyponatremia) will be falsely labeled as "severe" and unnecessarily treated with hypertonic saline. Specificity measures the ability to correctly identify patients who do NOT have the target condition (symptomatic severe hyponatremia requiring treatment).
- **Negative Predictive Value (NPV) DECREASES**: Patients with sodium levels between 115-120 mEq/L will now test "negative" for severe hyponatremia (falling above the new threshold), but some of these patients may still develop symptoms requiring treatment. Therefore, a "negative" test result (Na >115) becomes less reliable at ruling out the need for future treatment, decreasing NPV.
- **Note**: Sensitivity will DECREASE (more symptomatic patients with Na 115-120 will be missed), and PPV will INCREASE (those identified as severe are more likely to truly need treatment).
*Increased sensitivity and decreased positive predictive value*
- Moving the cutoff to a more stringent value (<115 mEq/L) would **decrease sensitivity**, not increase it, because patients with sodium 115-120 mEq/L who have symptoms would be missed.
- The positive predictive value would **increase**, not decrease, because patients classified as "severe" under the stricter criteria are more likely to truly require hypertonic saline.
*Increased specificity and decreased positive predictive value*
- **Increased specificity** is correct, as explained above.
- However, **PPV would increase**, not decrease, with a more stringent cutoff. When fewer patients are classified as "severe," those who meet the stricter criteria are more likely to truly have severe disease requiring treatment.
*Decreased specificity and increased negative predictive value*
- Specificity would **increase**, not decrease, with stricter diagnostic criteria (fewer false positives).
- NPV would **decrease**, not increase, because patients just above the new threshold (Na 115-120) who test "negative" may still require treatment.
*Decreased sensitivity and decreased positive predictive value*
- **Decreased sensitivity** is correct—the stricter cutoff will miss symptomatic patients with sodium 115-120 mEq/L.
- However, **PPV would increase**, not decrease. With stricter criteria, patients identified as "severe" are more likely to truly have severe disease requiring hypertonic saline.
Electrolyte disorders (Na, K, Ca, Mg) US Medical PG Question 3: A 45-year-old man undergoes a parathyroidectomy given recurrent episodes of dehydration and kidney stones caused by hypercalcemia secondary to an elevated PTH level. He is recovering on the surgical floor on day 3. His temperature is 97.6°F (36.4°C), blood pressure is 122/81 mmHg, pulse is 84/min, respirations are 12/min, and oxygen saturation is 98% on room air. The patient is complaining of perioral numbness currently. What is the most appropriate management of this patient?
- A. Potassium
- B. TSH level
- C. Vitamin D
- D. Observation
- E. Calcium gluconate (Correct Answer)
Electrolyte disorders (Na, K, Ca, Mg) Explanation: ***Calcium gluconate***
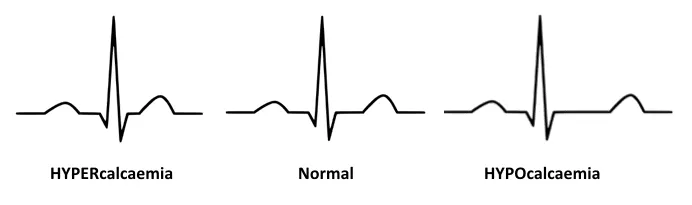
- The patient's presentation of **perioral numbness** following a parathyroidectomy, especially given a history of hypercalcemia, is highly suggestive of **hypocalcemia**.
- **Calcium gluconate** is indicated for acute symptomatic hypocalcemia to rapidly raise serum calcium levels and alleviate symptoms.
*Potassium*
- There is no clinical indication for **potassium** supplementation; the symptom of perioral numbness is not associated with potassium imbalance.
- Parathyroidectomy and hypercalcemia primarily affect calcium and phosphate metabolism, not typically potassium.
*TSH level*
- A **TSH level** is used to assess thyroid function, which is generally not directly affected by parathyroidectomy unless thyroid tissue was incidentally damaged.
- The symptoms presented do not suggest a thyroid dysfunction.
*Vitamin D*
- While **vitamin D** is crucial for calcium absorption and might be used in chronic management of hypocalcemia, it would not provide the immediate relief needed for acute symptomatic hypocalcemia.
- Acute symptoms like perioral numbness require a rapid elevation of serum calcium.
*Observation*
- **Observation** is inappropriate given the patient's symptomatic presentation of **perioral numbness**, which indicates acute and potentially worsening hypocalcemia.
- Untreated symptomatic hypocalcemia can progress to more severe complications such as seizures, arrhythmias, and laryngospasm.
Electrolyte disorders (Na, K, Ca, Mg) US Medical PG Question 4: A 28-year-old African American woman presents to her primary care physician with two weeks of nausea, abdominal pain, and increased urination. She states she has had kidney stones in the past and is concerned because her current pain is different in character from what she had experienced then. In addition she reports increasing weakness and fatigue over the past several months as well as mild shortness of breath. Chest radiography shows bilateral hilar adenopathy. Which of the following processes is most likely responsible for her current symptoms?
- A. Osteoclast-driven bone resorption
- B. Increased intestinal absorption of calcium (Correct Answer)
- C. Ectopic parathyroid hormone release
- D. Increased production of parathyroid hormone
- E. Increased renal calcium reabsorption
Electrolyte disorders (Na, K, Ca, Mg) Explanation: ***Increased intestinal absorption of calcium***
- The constellation of symptoms including **bilateral hilar adenopathy**, chronic fatigue, weakness, and hypercalcemia symptoms (nausea, abdominal pain, increased urination) in an African American woman is highly suggestive of **sarcoidosis**.
- In sarcoidosis, activated macrophages within granulomas produce **1α-hydroxylase**, which converts **25-hydroxyvitamin D to 1,25-dihydroxyvitamin D (calcitriol)**, leading to increased intestinal absorption of calcium and subsequent hypercalcemia.
*Osteoclast-driven bone resorption*
- While hypercalcemia can result from increased osteoclast activity (e.g., in **malignancy** or **primary hyperparathyroidism**), sarcoidosis-associated hypercalcemia is primarily due to increased gut absorption of calcium.
- The patient's history does not strongly point to significant bone destructive processes that would be the primary cause of her hypercalcemia.
*Ectopic parathyroid hormone release*
- **Ectopic PTH release** is characteristic of certain malignancies, such as squamous cell carcinoma, leading to **hypercalcemia of malignancy**.
- This syndrome is typically associated with very high calcium levels and PTHrP (parathyroid hormone-related peptide) production, not the clinical picture of sarcoidosis.
*Increased production of parathyroid hormone*
- **Increased PTH production** (primary hyperparathyroidism) causes hypercalcemia by increasing bone resorption, renal calcium reabsorption, and renal production of calcitriol.
- Although some symptoms overlap, the presence of **bilateral hilar adenopathy** and the absence of clear evidence for a parathyroid adenoma makes this less likely than sarcoidosis.
*Increased renal calcium reabsorption*
- While increased renal calcium reabsorption contributes to hypercalcemia, in the context of sarcoidosis, it is a secondary effect due to the overall calcium imbalance, not the primary mechanism.
- The principal driver of hypercalcemia in this patient's likely condition is the **overproduction of active vitamin D** leading to increased intestinal absorption.
Electrolyte disorders (Na, K, Ca, Mg) US Medical PG Question 5: A 21-year-old woman is admitted to the hospital for severe malnutrition with a BMI of 15 kg/m2. Past medical history is significant for chronic anorexia nervosa. During the course of her stay, she is treated with parenteral fluids and nutrition management. On the 4th day, her status changes. Her blood pressure is 110/75 mm Hg, heart rate is 120/min, respiratory rate is 25/min, and temperature is 37.0°C (98.6°F). On physical exam, her heart is tachycardic with a regular rhythm and her lungs are clear to auscultation bilaterally. She appears confused, disoriented, and agitated. Strength in her lower extremities is 4/5. What is the next step in management?
- A. MRI of the brain
- B. Administer insulin
- C. Measure electrolytes (Correct Answer)
- D. Arrange for outpatient counseling
- E. Doppler ultrasound on lower extremities
Electrolyte disorders (Na, K, Ca, Mg) Explanation: ***Measure electrolytes***
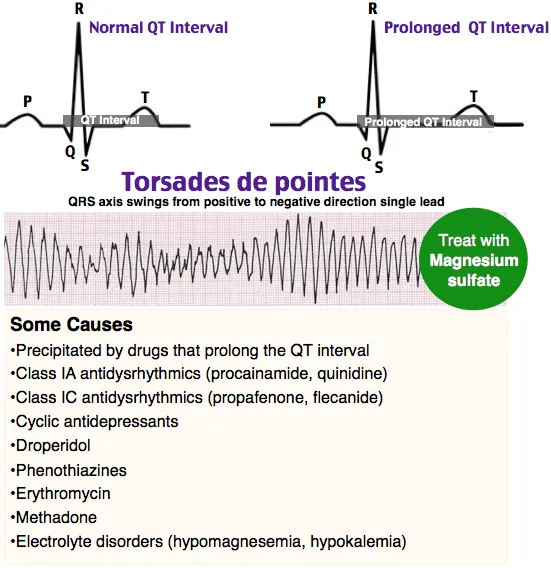
- The patient's presentation with **confusion, disorientation, agitation**, and **lower extremity weakness** after refeeding for severe **malnutrition** is highly suggestive of **refeeding syndrome**. This syndrome is characterized by severe electrolyte shifts, particularly **hypophosphatemia**, **hypokalemia**, and **hypomagnesemia**.
- Measuring electrolytes immediately is crucial to diagnose and then correct these imbalances, which can lead to life-threatening complications like **cardiac arrhythmias**, **respiratory failure**, and **seizures**.
*MRI of the brain*
- While neurological symptoms are present, a brain MRI is not the immediate first step given the context of refeeding in a severely malnourished patient.
- The symptoms are more consistent with **metabolic derangements** associated with **refeeding syndrome** than an acute primary neurological event.
*Administer insulin*
- Administering insulin without knowing the patient's glucose or electrolyte status could be dangerous, especially given the increased risk of **hypokalemia** and **hypophosphatemia** in refeeding syndrome, which insulin can exacerbate.
- Refeeding syndrome typically involves glucose shifts, but **hypoglycemia** is not the primary immediate concern, and hyperinsulinemia in this context can cause cellular uptake of electrolytes leading to further depletion.
*Arrange for outpatient counseling*
- The patient is acutely ill and experiencing a potentially life-threatening complication requiring immediate medical intervention.
- **Outpatient counseling** is not appropriate for an acute hospital admission with severe, rapidly changing symptoms.
*Doppler ultrasound on lower extremities*
- While immobility can increase the risk of deep vein thrombosis (DVT), the patient's symptoms of **confusion, agitation, tachycardia, tachypnea**, and **weakness** are not primary indicators of DVT.
- The clinical picture points strongly towards **metabolic complications** of refeeding.
Electrolyte disorders (Na, K, Ca, Mg) US Medical PG Question 6: A 45-year-old man presents to the physician with limb weakness over the last 24 hours. He is an otherwise healthy man with no significant past medical history. On physical examination, his vital signs are stable. On neurological examination, there is decreased strength in the muscles of all 4 extremities, and the deep tendon reflexes are depressed. A detailed laboratory evaluation shows that he has generalized decreased neuronal excitability due to an electrolyte imbalance. Which of the following electrolyte imbalances is most likely to be present in the man?
- A. Acute hypochloremia
- B. Acute hypernatremia
- C. Acute hyperkalemia
- D. Acute hypercalcemia (Correct Answer)
- E. Acute hypomagnesemia
Electrolyte disorders (Na, K, Ca, Mg) Explanation: ***Acute hypercalcemia***
- **Hypercalcemia** causes decreased neuronal excitability by stabilizing nerve cell membranes, leading to **muscle weakness** and depressed deep tendon reflexes.
- The generalized weakness and hyporeflexia described are classic neurological manifestations of elevated calcium levels.
*Acute hypochloremia*
- **Hypochloremia** is often associated with gastrointestinal losses and can lead to **metabolic alkalosis** and muscle cramps but not generalized muscle weakness with depressed reflexes.
- Its direct effect on neuronal excitability to cause such profound weakness is not typical.
*Acute hypernatremia*
- **Hypernatremia** primarily causes neurological symptoms due to **cellular dehydration** and cerebral edema, leading to altered mental status, seizures, or coma.
- It does not typically present with generalized muscle weakness and depressed deep tendon reflexes due to decreased neuronal excitability in the manner described.
*Acute hyperkalemia*
- **Hyperkalemia** can cause muscle weakness and paralysis, but it often progresses to **cardiac arrhythmias** and is typically associated with **increased neuronal excitability** initially, before paralyzing effects.
- While it can lead to weakness, the generalized decreased excitability described is more characteristic of calcium imbalance.
*Acute hypomagnesemia*
- **Hypomagnesemia** typically increases neuronal excitability, leading to symptoms like **muscle cramps**, tremors, hyperreflexia, and even seizures.
- It does not cause generalized muscle weakness with depressed deep tendon reflexes as a primary manifestation of decreased neuronal excitability.
Electrolyte disorders (Na, K, Ca, Mg) US Medical PG Question 7: A 67-year-old man with a history of chronic alcoholism presents to the emergency department after a suicide attempt. The patient was found in his apartment by his grandson with wrist lacerations. He was rushed to the emergency department and was resuscitated en route. The patient has a past medical history of ischemic heart disease and depression. His pulse is barely palpable and he is not responding to questions coherently. His temperature is 98.2°F (36.8°C), blood pressure is 107/48 mmHg, pulse is 160/min, respirations are 14/min, and oxygen saturation is 99% on room air. After fluid resuscitation and wound care, his blood pressure improves to 127/55 mmHg. On physical exam, the patient complains of numbness surrounding his mouth and pain in the location of the lacerations of his wrists. Which of the following best describes the laboratory findings in this patient?
- A. Hyperkalemia
- B. Increased free iron
- C. No lab abnormalities
- D. Hypomagnesemia (Correct Answer)
- E. Hypocalcemia
Electrolyte disorders (Na, K, Ca, Mg) Explanation: ***Hypomagnesemia***
- **Chronic alcoholism** is a significant risk factor for hypomagnesemia due to decreased dietary intake, increased renal excretion, and gastrointestinal losses.
- Clinical signs such as **numbness around the mouth** (circumoral paresthesia), **tachycardia**, and **agitation/confusion** can be manifestations of severe hypomagnesemia, which can also predispose to arrhythmias.
*Hyperkalemia*
- While electrolyte imbalances are common in alcoholism, **hyperkalemia** is less typical in this acute presentation unless associated with other complications like **renal failure** or certain medications.
- The patient's symptoms (numbness, tachycardia) are not classic for hyperkalemia; hyperkalemia often presents with **muscle weakness** or **cardiac arrhythmias** (peaked T waves, widened QRS).
*Increased free iron*
- **Increased free iron** is typically associated with conditions like **hemochromatosis** or acute iron poisoning, neither of which is suggested by the patient's history or symptoms.
- Chronic alcoholism can lead to iron overload in some cases, but this is usually chronic and does not manifest acutely with these neurological or cardiac symptoms.
*No lab abnormalities*
- Given the patient's history of **chronic alcoholism**, presentation with **tachycardia**, altered mental status, and circumoral paresthesia, it is highly unlikely that there would be no laboratory abnormalities.
- Alcoholism frequently leads to significant **electrolyte disturbances** and nutritional deficiencies, making "no lab abnormalities" an improbable finding.
*Hypocalcemia*
- While **hypocalcemia** can cause circumoral paresthesia, it is often secondary to **hypomagnesemia** in alcoholic patients.
- **Hypocalcemia** also typically presents with stronger signs of neuromuscular irritability like **tetany**, **Chvostek's sign**, or **Trousseau's sign**, which are not explicitly mentioned.
Electrolyte disorders (Na, K, Ca, Mg) US Medical PG Question 8: A 65-year-old woman is brought to the emergency department by her husband who found her lying unconscious at home. He says that the patient has been complaining of progressively worsening weakness and confusion for the past week. Her past medical history is significant for hypertension, systemic lupus erythematosus, and trigeminal neuralgia. Her medications include metoprolol, valsartan, prednisone, and carbamazepine. On admission, blood pressure is 130/70 mm Hg, pulse rate is 100 /min, respiratory rate is 17/min, and temperature is 36.5°C (97.7ºF). She regained consciousness while on the way to the hospital but is still drowsy and disoriented. Physical examination is normal. Finger-stick glucose level is 110 mg/dl. Other laboratory studies show:
Na+ 120 mEq/L (136—145 mEq/L)
K+ 3.5 mEq/L (3.5—5.0 mEq/L)
CI- 107 mEq/L (95—105 mEq/L)
Creatinine 0.8 mg/dL (0.6—1.2 mg/dL)
Serum osmolality 250 mOsm/kg (275—295 mOsm/kg)
Urine Na+ 70 mEq/L
Urine osmolality 350 mOsm/kg
She is admitted to the hospital for further management. Which of the following is the next best step in the management of this patient's condition?
- A. Rapid resuscitation with hypertonic saline (Correct Answer)
- B. Fluid restriction
- C. Tolvaptan
- D. Lithium
- E. Desmopressin
Electrolyte disorders (Na, K, Ca, Mg) Explanation: **Rapid resuscitation with hypertonic saline**
- The patient presents with **severe hyponatremia** (120 mEq/L) and neurological symptoms (drowsiness, disorientation, history of unconsciousness), indicating a need for **urgent correction** to prevent cerebral edema.
- **Hypertonic saline** (e.g., 3%) is indicated for severe symptomatic hyponatremia to rapidly increase serum sodium levels and reduce brain swelling.
*Fluid restriction*
- **Fluid restriction** is a conservative measure appropriate for **mild to moderate asymptomatic hyponatremia** or as an adjunct in SIADH management once severe symptoms are controlled.
- It would be too slow to address the patient's acute neurological symptoms and severe hyponatremia, potentially delaying critical treatment.
*Tolvaptan*
- **Tolvaptan** is a **vasopressin receptor antagonist** used in the treatment of **euvolemic or hypervolemic hyponatremia**, often in the context of SIADH.
- Its use is generally reserved for patients who have not responded to fluid restriction and is **contraindicated** in patients with severe symptoms or to rapidly correct severe hyponatremia due to the risk of overly rapid correction and osmotic demyelination syndrome.
*Lithium*
- **Lithium** is primarily used as a **mood stabilizer** in psychiatric conditions, particularly bipolar disorder.
- It can cause **nephrogenic diabetes insipidus** as a side effect and is not a treatment for hyponatremia.
*Desmopressin*
- **Desmopressin** is a synthetic analog of **antidiuretic hormone (ADH)** and is used to treat **diabetes insipidus** or nocturnal enuresis.
- Administering desmopressin would **worsen hyponatremia** by promoting water reabsorption, making it an inappropriate choice for this patient.
Electrolyte disorders (Na, K, Ca, Mg) US Medical PG Question 9: A 25-year-old woman is brought to the emergency department 12 hours after ingesting 30 tablets of an unknown drug in a suicide attempt. The tablets belonged to her father, who has a chronic heart condition. She has had nausea and vomiting. She also reports blurring and yellowing of her vision. Her temperature is 36.7°C (98°F), pulse is 51/min, and blood pressure is 108/71 mm Hg. Abdominal examination shows diffuse tenderness with no guarding or rebound. Bowel sounds are normal. An ECG shows prolonged PR-intervals and flattened T-waves. Further evaluation is most likely to show which of the following electrolyte abnormalities?
- A. Increased serum K+ (Correct Answer)
- B. Decreased serum K+
- C. Decreased serum Na+
- D. Increased serum Na+
- E. Increased serum Ca2+
Electrolyte disorders (Na, K, Ca, Mg) Explanation: ***Increased serum K+***
- The patient presents with classic symptoms of **digoxin toxicity**, including **nausea, vomiting, blurry and yellow vision, bradycardia**, and ECG changes like **prolonged PR interval** and **flattened T-waves**.
- **Digoxin inhibits the Na+/K+-ATPase pump**, leading to an increase in extracellular potassium as potassium cannot enter the cells.
*Decreased serum K+*
- While hypokalemia can exacerbate digoxin toxicity by increasing digoxin binding to the Na+/K+-ATPase, digoxin overdose itself typically causes **hyperkalemia** due to its direct effect on the pump.
- ECG changes like **flattened T-waves** can be seen in hypokalemia, but the overall clinical picture, especially the history of overdose and bradycardia, points more strongly to digoxin toxicity with hyperkalemia.
*Decreased serum Na+*
- **Hyponatremia** is not a characteristic feature of acute digoxin overdose.
- Digoxin primarily affects potassium and calcium channels, with less direct impact on sodium levels, unless related to fluid status changes which are not indicated here.
*Increased serum Na+*
- **Hypernatremia** is not typically associated with digoxin toxicity.
- Digoxin's mechanism of action does not directly lead to increased serum sodium; rather, it primarily inhibits the Na+/K+-ATPase.
*Increased serum Ca2+*
- Digoxin **increases intracellular calcium** by inhibiting the Na+/K+-ATPase, which indirectly leads to increased Na+/Ca2+ exchanger activity.
- However, this primarily affects intracellular levels and **does not typically result in increased serum calcium**.
Electrolyte disorders (Na, K, Ca, Mg) US Medical PG Question 10: A 54-year-old woman presents to her primary care physician complaining of watery diarrhea for the last 3 weeks. She reports now having over 10 bowel movements per day. She denies abdominal pain or rash. A basic metabolic profile is notable for the following: Na: 127 mEq/L; K 2.1 mEq/L; Glucose 98 mg/dL. Following additional work-up, octreotide was started with significant improvement in symptoms and laboratory values. Which of the following is the most likely diagnosis?
- A. Glucagonoma
- B. Gastrinoma
- C. Somatostatinoma
- D. VIPoma (Correct Answer)
- E. Insulinoma
Electrolyte disorders (Na, K, Ca, Mg) Explanation: ***VIPoma***
- The patient's presentation of **prolonged watery diarrhea** (over 10 bowel movements per day for 3 weeks) coupled with **hypokalemia** (K 2.1 mEq/L) and **hyponatremia** (Na 127 mEq/L) strongly points to a VIPoma.
- Absence of abdominal pain and rash, along with improvement following **octreotide** (a somatostatin analog that inhibits VIP release), further supports this diagnosis.
*Glucagonoma*
- Characterized by **necrolytic migratory erythema** (a prominent skin rash) and often **diabetes mellitus**, neither of which are described in this patient.
- While it can cause diarrhea, it typically presents with the characteristic rash.
*Gastrinoma*
- This typically presents with **Zollinger-Ellison syndrome**, which involves **severe, refractory peptic ulcers**, rather than primarily profuse watery diarrhea.
- It also usually causes **elevated gastrin levels** and accompanying severe abdominal pain.
*Somatostatinoma*
- Often presents with a classic triad of **diabetes mellitus**, **cholelithiasis**, and **steatorrhea**, which are not reported in this case.
- Diarrhea is usually due to malabsorption rather than secretory, watery diarrhea.
*Insulinoma*
- The primary symptom of an insulinoma is **hypoglycemia**, often presenting with neuroglycopenic symptoms (e.g., confusion, dizziness) due to excessive insulin secretion.
- The patient's glucose level is normal (98 mg/dL), and her symptoms are unrelated to hypoglycemia.
More Electrolyte disorders (Na, K, Ca, Mg) US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.