Body fluid compartments US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Body fluid compartments. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Body fluid compartments US Medical PG Question 1: A 62-year-old man presents to the emergency department with confusion. The patient’s wife states that her husband has become more somnolent over the past several days and now is very confused. The patient has no complaints himself, but is answering questions inappropriately. The patient has a past medical history of diabetes and hypertension. His temperature is 98.3°F (36.8°C), blood pressure is 127/85 mmHg, pulse is 138/min, respirations are 14/min, and oxygen saturation is 99% on room air. Physical exam is notable for a confused man with dry mucous membranes. Initial laboratory studies are ordered as seen below.
Serum:
Na+: 135 mEq/L
Cl-: 100 mEq/L
K+: 3.0 mEq/L
HCO3-: 23 mEq/L
BUN: 30 mg/dL
Glucose: 1,299 mg/dL
Creatinine: 1.5 mg/dL
Ca2+: 10.2 mg/dL
Which of the following is the most appropriate initial treatment for this patient?
- A. Insulin, normal saline, and potassium (Correct Answer)
- B. Normal saline and potassium
- C. Insulin and potassium
- D. Insulin
- E. Insulin and normal saline
Body fluid compartments Explanation: ***Insulin, normal saline, and potassium***
- This patient is presenting with **hyperosmolar hyperglycemic state (HHS)**, characterized by severe hyperglycemia (glucose 1299 mg/dL), dehydration (dry mucous membranes, high BUN and creatinine), and altered mental status. The initial treatment involves intravenous fluids to correct dehydration, insulin to lower blood glucose, and potassium supplementation due to potential shifts as insulin is administered.
- **Normal saline** addresses the severe dehydration, **insulin** corrects hyperglycemia, and **potassium supplementation** prevents hypokalemia, which is common during HHS treatment as glucose and potassium shift intracellularly.
*Normal saline and potassium*
- While **normal saline** and **potassium** are crucial for rehydration and electrolyte balance, omitting **insulin** would fail to address the core problem of severe hyperglycemia in HHS.
- Without insulin, blood glucose levels will remain dangerously high, leading to persistent osmotic diuresis and worsening dehydration.
*Insulin and potassium*
- Administering **insulin** without addressing the profound **dehydration** with intravenous fluids can lead to **hypovolemic shock** as insulin further drives glucose and water into cells.
- Rehydration is the priority in HHS management before or concurrent with insulin administration.
*Insulin*
- Giving only **insulin** would be detrimental, as the patient is severely dehydrated and hypokalemic (K+ 3.0 mEq/L, and will drop further with insulin).
- This approach would exacerbate dehydration and could cause life-threatening arrhythmias due to severe hypokalemia.
*Insulin and normal saline*
- While addressing hyperglycemia and dehydration, omitting **potassium supplementation** is dangerous because insulin drives potassium into cells, potentially causing severe **hypokalemia** and cardiac arrhythmias.
- The patient already has a low-normal potassium level, which will likely drop further with insulin treatment.
Body fluid compartments US Medical PG Question 2: A 28-year-old research assistant is brought to the emergency department for severe chemical burns 30 minutes after accidentally spilling hydrochloric acid on himself. The burns cover both hands and forearms. His temperature is 37°C (98.6°F), pulse is 112/min, respirations are 20/min, and blood pressure is 108/82 mm Hg. Initial stabilization and resuscitation is begun, including respiratory support, fluid resuscitation, and cardiovascular stabilization. The burned skin is irrigated with saline water to remove the chemical agent. Which of the following is the most appropriate method to verify adequate fluid infusion in this patient?
- A. The Parkland formula
- B. Blood pressure
- C. Pulmonary capillary wedge pressure
- D. Heart rate
- E. Urinary output (Correct Answer)
Body fluid compartments Explanation: ***Urinary output***
- Maintaining a specific **urinary output** (e.g., adult with major burns: 0.5-1.0 mL/kg/hr or 30-50 mL/hr) is the most reliable clinical indicator of adequate fluid resuscitation in burn patients.
- This ensures sufficient end-organ perfusion and avoids both under-resuscitation (leading to shock and organ damage) and over-resuscitation (risk of compartment syndrome and pulmonary edema).
*The Parkland formula*
- The **Parkland formula** is used to *calculate* the initial fluid volume needed, but it does not *verify* the adequacy of the infusion once started.
- This formula provides a starting point for fluid administration, which then needs to be adjusted based on the patient's response.
*Blood pressure*
- **Blood pressure** can be misleading in burn patients; it may remain deceptively normal due to compensatory mechanisms even with significant fluid deficits.
- It is a late indicator of hypovolemic shock, and relying solely on it can lead to under-resuscitation.
*Pulmonary capillary wedge pressure*
- **Pulmonary capillary wedge pressure (PCWP)** requires invasive monitoring via a pulmonary artery catheter, which is rarely indicated for routine fluid management in burn patients due to its invasiveness and associated risks.
- Less invasive and equally effective methods, like urinary output, are preferred for monitoring resuscitation.
*Heart rate*
- **Heart rate** is a sensitive but non-specific indicator of fluid status; it can be elevated due to pain, anxiety, or infection, not solely hypovolemia.
- While a decreasing heart rate can indicate improved fluid status, it is not as reliable or direct an indicator of end-organ perfusion as urinary output.
Body fluid compartments US Medical PG Question 3: A medical student is studying human physiology. She learns that there is a membrane potential across cell membranes in excitable cells. The differential distribution of anions and cations both inside and outside the cells significantly contributes to the genesis of the membrane potential. Which of the following distributions of anions and cations best explains the above phenomenon?
- A. High concentration of K+ outside the cell and low concentration of K+ inside the cell
- B. High concentration of Na+ outside the cell and high concentration of K+ inside the cell (Correct Answer)
- C. High concentration of Ca2+ outside the cell and high concentration of Cl- inside the cell
- D. Low concentration of K+ outside the cell and high concentration of Ca2+ inside the cell
- E. Low concentration of Cl- outside the cell and high concentration of Cl- inside the cell
Body fluid compartments Explanation: ***High concentration of Na+ outside the cell and high concentration of K+ inside the cell***
- This distribution is maintained by the **Na+/K+ ATPase pump**, which actively transports **3 Na+ ions out of the cell** and **2 K+ ions into the cell**, against their concentration gradients.
- This differential concentration of **sodium** and **potassium** ions is critical for establishing the negative **resting membrane potential** as K+ channels allow K+ to leak out, making the inside more negative.
*High concentration of K+ outside the cell and low concentration of K+ inside the cell*
- This statement is incorrect as the normal physiological state is characterized by a **high concentration of K+ inside the cell** and a low concentration outside.
- An increase in extracellular K+ concentration (hyperkalemia) would **depolarize** the cell, affecting excitability.
*High concentration of Ca2+ outside the cell and high concentration of Cl- inside the cell*
- While Ca2+ is indeed in higher concentration outside the cell, Cl- is typically in **higher concentration outside the cell** compared to inside, which contributes to the membrane potential through its electrochemical gradient.
- An elevated intracellular Cl- concentration would make the cell more negative if Cl- channels were open but is not the primary determinant.
*Low concentration of K+ outside the cell and high concentration of Ca2+ inside the cell*
- The first part is correct—low K+ outside is normal—but a **high concentration of Ca2+ inside the cell** is generally an indicator of cellular pathology or specific physiological events like muscle contraction or neurotransmitter release, not a steady-state condition contributing to resting potential.
- Normal intracellular Ca2+ is kept very low due to active pumps.
*Low concentration of Cl- outside the cell and high concentration of Cl- inside the cell*
- This statement is incorrect as **chloride ions** are typically in a **higher concentration outside the cell** than inside.
- The influx of Cl- into the cell, when channels are open, usually hyperpolarizes the membrane, contributing to inhibition, but its gradient is opposite to what is described.
Body fluid compartments US Medical PG Question 4: A scientist is studying the excretion of a novel toxin X by the kidney in order to understand the dynamics of this new substance. He discovers that this new toxin X has a clearance that is half that of inulin in a particular patient. This patient's filtration fraction is 20% and his para-aminohippuric acid (PAH) dynamics are as follows:
Urine volume: 100 mL/min
Urine PAH concentration: 30 mg/mL
Plasma PAH concentration: 5 mg/mL
Given these findings, what is the clearance of the novel toxin X?
- A. 1,500 mL/min
- B. 600 mL/min
- C. 300 mL/min
- D. 60 mL/min (Correct Answer)
- E. 120 mL/min
Body fluid compartments Explanation: ***60 ml/min***
- First, calculate the **renal plasma flow (RPF)** using PAH clearance: RPF = (Urine PAH conc. × Urine vol.) / Plasma PAH conc. = (30 mg/mL × 100 mL/min) / 5 mg/mL = 600 mL/min.
- Next, calculate the **glomerular filtration rate (GFR)**, which is the clearance of inulin. GFR = RPF × Filtration Fraction = 600 mL/min × 0.20 = 120 mL/min. Toxin X clearance is half of inulin clearance, so 120 mL/min / 2 = **60 mL/min**.
*1,500 ml/min*
- This value is likely obtained if an incorrect formula or conversion was made, possibly by misinterpreting the units or the relationship between GFR, RPF, and filtration fraction.
- It significantly overestimates the clearance for a substance that is cleared at half the rate of inulin.
*600 ml/min*
- This value represents the **renal plasma flow (RPF)**, calculated using the PAH clearance data.
- It does not account for the filtration fraction or the fact that toxin X clearance is half of inulin clearance (GFR).
*300 ml/min*
- This value would be obtained if the renal plasma flow (RPF) was incorrectly halved, or if an intermediate calculation was misinterpreted as the final answer.
- It does not align with the given filtration fraction and the relationship between toxin X and inulin clearance.
*120 ml/min*
- This value represents the **glomerular filtration rate (GFR)**, which is equal to the clearance of inulin (RPF × Filtration Fraction = 600 mL/min × 0.20 = 120 mL/min).
- The question states that the clearance of toxin X is **half** that of inulin, so this is an intermediate step, not the final answer.
Body fluid compartments US Medical PG Question 5: An experiment to determine the effects of gravity on blood pressure is conducted on 3 individuals of equal height and blood pressure oriented in different positions in space. Participant A is strapped in a supine position on a bed turned upside down in a vertical orientation with his head towards the floor and his feet towards the ceiling. Participant B is strapped in a supine position on a bed turned downwards in a vertical orientation with his head towards the ceiling and his feet just about touching the floor. Participant C is strapped in a supine position on a bed in a horizontal orientation. Blood pressure readings are then taken at the level of the head, heart, and feet from all 3 participants. Which of these positions will have the lowest recorded blood pressure reading?
- A. Participant B: at the level of the feet
- B. Participant A: at the level of the head
- C. Participant C: at the level of the heart
- D. Participant A: at the level of the feet (Correct Answer)
- E. Participant C: at the level of the feet
Body fluid compartments Explanation: ***Participant A: at the level of the feet***
- In Participant A, the feet are positioned **highest vertically** relative to the heart and are also above the head due to the upside-down vertical orientation. Due to gravity, blood pressure decreases with increasing height above the heart.
- This position would result in the lowest hydrostatic pressure at the feet, leading to the **lowest recorded blood pressure reading**.
*Participant B: at the level of the feet*
- In Participant B, the feet are positioned **below the heart** (towards the floor) in a vertical orientation.
- This position would experience some of the **highest hydrostatic pressure** due to gravity, leading to a high blood pressure reading, not the lowest.
*Participant A: at the level of the head*
- In Participant A, the head is positioned **below the heart** (towards the floor) in an upside-down vertical orientation.
- This position would experience increased hydrostatic pressure, hence a **higher blood pressure** compared to the feet.
*Participant C: at the level of the heart*
- Participant C is in a horizontal position, meaning all body parts are at roughly the same hydrostatic level relative to the heart.
- Blood pressure readings would be **similar across all points** (head, heart, feet) and would reflect the systemic arterial pressure without significant hydrostatic effects, thus not the lowest compared to other extreme positions.
*Participant C: at the level of the feet*
- In Participant C (horizontal), the feet are at approximately the **same hydrostatic level** as the heart.
- The reading at the feet in this position would be close to the **baseline arterial pressure**, not the lowest, as there's minimal hydrostatic gradient.
Body fluid compartments US Medical PG Question 6: A 43-year-old woman is found in the hospital to have a plasma sodium concentration of 126 mg/dL. She was hospitalized after she expressed suicidal ideations and was started on a medication for major depressive disorder. Her past medical history is significant for diabetes for which she is currently taking metformin. Her blood pressure while in the hospital has been around 130/85 mmHg and she is not taking any other medications. Laboratory studies show a serum osmolality of 265 mOsm/kg. Which of the following best describes the cell bodies of the cells that are behaving abnormally in this patient?
- A. Basophils in the anterior pituitary
- B. Chromophobes in the anterior pituitary
- C. Acidophils in the anterior pituitary
- D. Located in the hypothalamus (Correct Answer)
- E. Located in the posterior pituitary
Body fluid compartments Explanation: ***Located in the hypothalamus***
- The patient's **hyponatremia** (126 mg/dL) with a **low serum osmolality** (265 mOsm/kg) in the presence of depression and medication suggests **Syndrome of Inappropriate Antidiuretic Hormone (SIADH)**.
- **ADH (vasopressin)** is synthesized in the magnocellular neurosecretory cells of the **hypothalamus** (specifically the supraoptic and paraventricular nuclei) and then transported to the posterior pituitary for release. Since the patient's condition is due to inappropriate ADH secretion, the abnormality originates in the hypothalamus where these cells are located.
*Basophils in the anterior pituitary*
- **Basophils** in the anterior pituitary produce hormones like **TSH, FSH, and LH**, which are not directly involved in the regulation of water balance and sodium levels in the context of SIADH.
- An abnormality in these cells would lead to endocrine dysfunction related to thyroid or gonadal axes, not hyponatremia.
*Chromophobes in the anterior pituitary*
- **Chromophobes** are cells in the anterior pituitary that are typically undifferentiated or degranulated, often representing cells that have released their stored hormones.
- They are not primarily responsible for the production or release of hormones involved in water balance, so an abnormality here is unlikely to cause SIADH.
*Acidophils in the anterior pituitary*
- **Acidophils** in the anterior pituitary produce **growth hormone (GH)** and **prolactin**.
- Abnormalities in these cells would lead to conditions like acromegaly or hyperprolactinemia, neither of which explains the patient's hyponatremia and low serum osmolality.
*Located in the posterior pituitary*
- While the **posterior pituitary** stores and releases **ADH**, it does not synthesize it; the cell bodies responsible for ADH production are in the hypothalamus.
- Therefore, the primary abnormal cells in SIADH are the ones synthesizing ADH in the hypothalamus, not merely storing it in the posterior pituitary.
Body fluid compartments US Medical PG Question 7: An 8-year-old boy is shifted to a post-surgical floor following neck surgery. The surgeon has restricted his oral intake for the next 24 hours. He does not have diarrhea, vomiting, or dehydration. His calculated fluid requirement is 1500 mL/day. However, he receives 2000 mL of intravenous isotonic fluids over 24 hours. Which of the following physiological parameters in the boy’s circulatory system is most likely to be increased?
- A. Interstitial oncotic pressure
- B. Interstitial hydrostatic pressure
- C. Capillary wall permeability
- D. Capillary oncotic pressure
- E. Capillary hydrostatic pressure (Correct Answer)
Body fluid compartments Explanation: ***Capillary hydrostatic pressure***
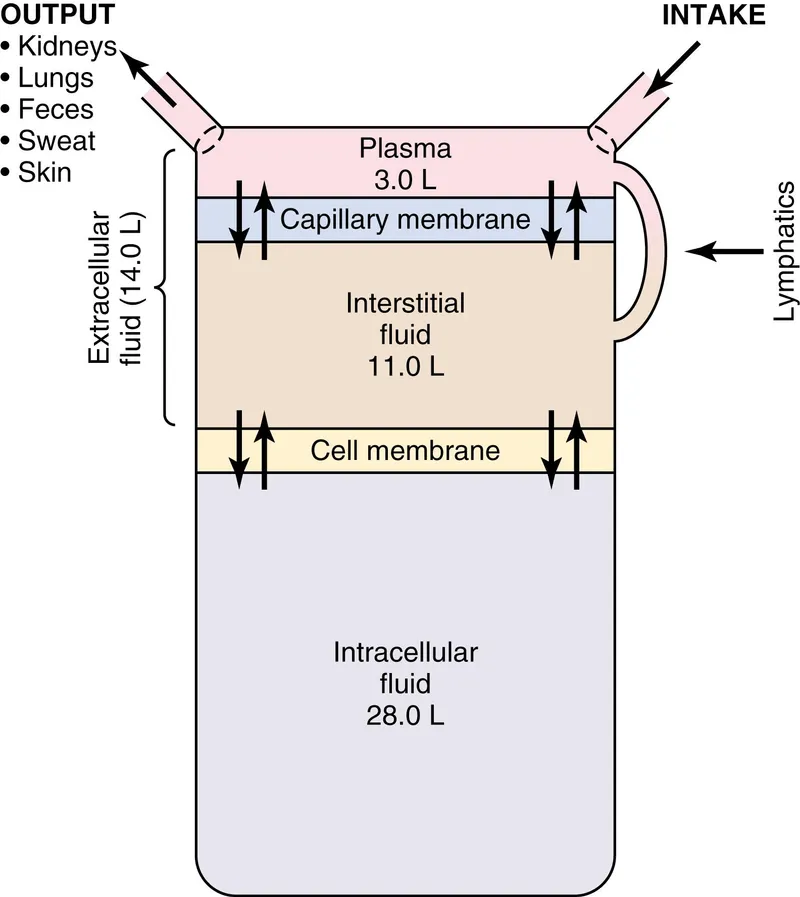
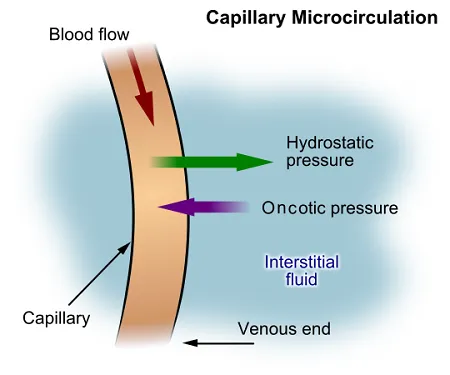
- Giving 2000 mL of intravenous isotonic fluids when the calculated requirement is 1500 mL/day leads to a **positive fluid balance** and **fluid overload**.
- This excess fluid directly increases the **intravascular volume**, thereby raising the **capillary hydrostatic pressure**, which pushes fluid out of the capillaries.
*Interstitial oncotic pressure*
- This pressure is primarily determined by the **protein concentration** in the interstitial fluid.
- While fluid overload can dilute interstitial proteins, it generally does not directly increase interstitial oncotic pressure; rather, it might decrease it due to fluid movement.
*Interstitial hydrostatic pressure*
- As fluid moves out of the capillaries due to increased capillary hydrostatic pressure, the **interstitial hydrostatic pressure** will also increase.
- However, the primary driving force for this change, and thus the most direct consequence of fluid overload, is the increase in capillary hydrostatic pressure.
*Capillary wall permeability*
- This parameter refers to the ease with which substances, including fluid and proteins, can cross the capillary wall.
- Fluid overload does not typically affect **capillary wall permeability** unless there is an underlying condition causing inflammation or damage to the capillary endothelium.
*Capillary oncotic pressure*
- This pressure is mainly determined by the **protein concentration** within the capillaries.
- In a state of fluid overload with isotonic fluids, the plasma proteins are diluted, leading to a **decrease** in capillary oncotic pressure, not an increase.
Body fluid compartments US Medical PG Question 8: A 35-year-old man is brought to the emergency department from a kitchen fire. The patient was cooking when boiling oil splashed on his exposed skin. His temperature is 99.7°F (37.6°C), blood pressure is 127/82 mmHg, pulse is 120/min, respirations are 12/min, and oxygen saturation is 98% on room air. He has dry, nontender, and circumferential burns over his arms bilaterally, burns over the anterior portion of his chest and abdomen, and tender spot burns with blisters on his shins. A 1L bolus of normal saline is administered and the patient is given morphine and his pulse is subsequently 80/min. A Foley catheter is placed which drains 10 mL of urine. What is the best next step in management?
- A. Additional fluids and escharotomy (Correct Answer)
- B. Escharotomy
- C. Continuous observation
- D. Moist dressings and discharge
- E. Additional fluids and admission to the ICU
Body fluid compartments Explanation: ***Additional fluids and escharotomy***
- The patient has **circumferential full-thickness burns** on both arms (dry, nontender), which require **escharotomy** to prevent compartment syndrome and vascular compromise to the limbs.
- The **oliguria** (10 mL urine output) despite a 1L fluid bolus indicates **inadequate fluid resuscitation** from burn shock. With approximately 40% TBSA burns, the patient requires aggressive fluid resuscitation per the Parkland formula (4 mL/kg/% TBSA), which would be approximately 11 liters in the first 24 hours. Adequate resuscitation targets urine output of 0.5-1 mL/kg/hr (35-70 mL/hr for this patient).
- Both interventions are immediately necessary: fluids for burn shock and escharotomy for circumferential burns.
*Escharotomy*
- While **escharotomy** is essential for the circumferential full-thickness burns to prevent compartment syndrome, it alone will not address the **severe fluid deficit** causing oliguria and hypoperfusion.
- The low urine output reflects systemic hypovolemia from burn shock, not just local compartment issues, requiring aggressive fluid resuscitation.
*Continuous observation*
- **Continuous observation** is inappropriate given the patient's critical findings: circumferential full-thickness burns requiring urgent escharotomy and oliguria indicating inadequate resuscitation.
- Delaying escharotomy can lead to irreversible ischemic damage to the limbs, and inadequate fluid resuscitation can progress to multiorgan failure.
*Moist dressings and discharge*
- This option is completely inappropriate for a patient with **extensive deep burns** (approximately 40% TBSA) including full-thickness injuries requiring hospitalization and specialized burn care.
- Discharge would lead to severe complications including infection, inadequate fluid resuscitation, compartment syndrome, and potential limb loss.
*Additional fluids and admission to the ICU*
- While ICU admission and additional fluids are necessary components of care, this option is **incomplete** because it omits **escharotomy**, which is urgently needed for the circumferential full-thickness burns.
- Escharotomy is a time-sensitive procedure that must be performed promptly to prevent ischemic injury to the limbs from vascular compromise.
Body fluid compartments US Medical PG Question 9: A 62-year-old man presents with multiple episodes of hemoptysis for a week. It is associated with generalized weakness, decreased appetite, and a 5.4 kg (12 lb) weight loss in 2 months. He has a smoking history of a pack a day for the last 47 years. Physical examination reveals pallor, while the rest of the results are within normal limits. Laboratory studies reveal decreased hemoglobin and a serum sodium value of 130 mEq/L. Chest X-ray shows a 3 cm rounded opaque shadow. Which of the following conditions is the patient most likely suffering from?
- A. Small cell carcinoma of the lung (Correct Answer)
- B. Squamous cell carcinoma of the lung
- C. Tuberculoma
- D. Lung abscess
- E. Adenocarcinoma of the lung
Body fluid compartments Explanation: **Small cell carcinoma of the lung**
- The patient's presentation with **hemoptysis**, significant **weight loss**, and a long **smoking history** is highly suggestive of lung cancer.
- **Hyponatremia** (130 mEq/L) in this context often indicates **syndrome of inappropriate antidiuretic hormone secretion (SIADH)**, which is a common paraneoplastic syndrome associated with **small cell lung carcinoma**.
*Squamous cell carcinoma of the lung*
- While squamous cell carcinoma is strongly associated with smoking and can cause hemoptysis, it is less commonly linked to **SIADH and hyponatremia** compared to small cell carcinoma.
- This type of cancer is typically **centrally located** and can lead to **hypercalcemia** due to parathyroid hormone-related peptide (PTHrP) production, which is not seen here.
*Tuberculoma*
- A **tuberculoma** is a localized granuloma that can appear as a rounded opacity on X-ray, but it is less likely to cause significant **systemic symptoms** like profound weight loss and unexplained hyponatremia.
- **Hemoptysis** can occur with tuberculosis, but the overall clinical picture, especially the paraneoplastic features, points away from it.
*Lung abscess*
- A **lung abscess** typically presents with symptoms of infection such as **fever, purulent sputum**, and often a history of aspiration or pneumonia, which are absent here.
- The chest X-ray usually shows a **cavitated lesion with an air-fluid level**, and hyponatremia due to SIADH is not a common association.
*Adenocarcinoma of the lung*
- Although **adenocarcinoma** can cause hemoptysis and weight loss, it is typically more common in **non-smokers** or former smokers and often presents as a peripheral lesion.
- While it can be associated with paraneoplastic syndromes, **SIADH** and subsequent hyponatremia are much less frequent with adenocarcinoma compared to small cell lung carcinoma.
Body fluid compartments US Medical PG Question 10: A 24-day-old neonate is brought to the emergency department by his parents with high-grade fever, inability to feed, and lethargy. Since his birth, he was active and energetic, feeding every 2-3 hours and making 6-8 wet diapers every day until 2 days ago when he vomited twice, developed diarrhea, and slowly became lethargic. The boy was born at 39 weeks gestation via spontaneous vaginal delivery. He is up to date on all vaccines and is meeting all developmental milestones. He has not been in contact with any sick people lately. Today, his temperature is 39.4°C (102.9°F). He looks floppy and is unresponsive and difficult to rouse. Physical exam reveals a bulging anterior fontanelle. He is admitted to the NICU with the suspicion of neonatal meningitis, cerebrospinal fluid analysis is ordered, and empiric antibiotics are started. Which of the following structures will be punctured during the lumbar puncture procedure?
- A. Nucleus pulposus
- B. Denticulate ligament
- C. Anterior Longitudinal Ligament
- D. Dura layer (Correct Answer)
- E. Pia layer
Body fluid compartments Explanation: ***Dura layer***
- During a **lumbar puncture**, the needle is inserted into the **subarachnoid space** to collect cerebrospinal fluid (CSF). To reach this space, the needle must pass through several layers, including the **dura mater** (and the closely adherent arachnoid mater).
- The dura mater is the **outermost meningeal layer** and must be punctured to access the CSF that surrounds the nerve roots in the cauda equina.
- The needle typically passes through: skin → subcutaneous tissue → supraspinous ligament → interspinous ligament → ligamentum flavum → epidural space → **dura mater** → subarachnoid space.
*Nucleus pulposus*
- The **nucleus pulposus** is the central, gelatinous core of the **intervertebral disc**, which is located anterior to the spinal canal.
- Puncturing the nucleus pulposus would indicate a needle inserted too far anteriorly, potentially damaging the disc and not accessing the CSF.
*Denticulate ligament*
- The **denticulate ligaments** are extensions of the pia mater that anchor the spinal cord to the dura mater.
- These ligaments are located at the level of the spinal cord (which ends at L1-L2), well above the typical lumbar puncture site (L3-L4 or L4-L5). They are not encountered during a properly performed lumbar puncture.
*Anterior Longitudinal Ligament*
- The **anterior longitudinal ligament** is a strong fibrous band that runs along the anterior surfaces of the vertebral bodies.
- This ligament is far anterior to the spinal canal and the target location for a lumbar puncture; puncturing it would mean the needle passed entirely through the vertebral column.
*Pia layer*
- The **pia mater** is the innermost meningeal layer, which is intimately adhered to the surface of the spinal cord and individual nerve roots.
- Lumbar puncture is performed **below the level of the spinal cord** (which terminates at L1-L2 as the conus medullaris) in the region of the **cauda equina**, where only nerve roots are present floating freely in CSF.
- The pia mater covers individual nerve roots but is not a continuous layer at the LP site. The needle enters the subarachnoid space between nerve roots without puncturing the pia mater or the nerve roots themselves.
More Body fluid compartments US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.