Blood component therapy US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Blood component therapy. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Blood component therapy US Medical PG Question 1: A 36-year-old woman is brought to the emergency department 20 minutes after being involved in a high-speed motor vehicle collision. On arrival, she is unconscious. Her pulse is 140/min, respirations are 12/min and shallow, and blood pressure is 76/55 mm Hg. 0.9% saline infusion is begun. A focused assessment with sonography shows blood in the left upper quadrant of the abdomen. Her hemoglobin concentration is 7.6 g/dL and hematocrit is 22%. The surgeon decided to move the patient to the operating room for an emergent explorative laparotomy. Packed red blood cell transfusion is ordered prior to surgery. However, a friend of the patient asks for the transfusion to be held as the patient is a Jehovah's Witness. The patient has no advance directive and there is no documentation showing her refusal of blood transfusions. The patient's husband and children cannot be contacted. Which of the following is the most appropriate next best step in management?
- A. Administer hydroxyethyl starch
- B. Transfusion of packed red blood cells (Correct Answer)
- C. Consult hospital ethics committee
- D. Administer high-dose iron dextran
Blood component therapy Explanation: ***Transfusion of packed red blood cells***
- This patient is in **hemorrhagic shock** (tachycardia, hypotension, low hemoglobin, and hematocrit with evidence of active bleeding), requiring emergent blood transfusion to prevent irreversible organ damage and death.
- In an **emergency setting** with an **unconscious patient** and **no documented refusal** of blood products, the principle of **presumed consent** for life-saving treatment takes precedence, especially when next of kin cannot be reached.
*Administer hydroxyethyl starch*
- **Colloids** like hydroxyethyl starch can temporarily increase intravascular volume but do not provide oxygen-carrying capacity, which is critically needed for a patient with severe anemia and hemorrhagic shock.
- While useful for volume expansion, it is **not a substitute for blood products** in severe bleeding and can have adverse effects such as kidney injury.
*Consult hospital ethics committee*
- Consulting an ethics committee is appropriate for **complex ethical dilemmas** when there is time for deliberation and the patient's life is not in immediate danger.
- In this acute, life-threatening emergency, **delaying treatment** to consult an ethics committee would jeopardize the patient's life and is not appropriate.
*Administer high-dose iron dextran*
- **Iron dextran** is used to treat iron-deficiency anemia and works by supporting red blood cell production over several days to weeks.
- It is **ineffective in acute hemorrhagic shock** where immediate restoration of oxygen-carrying capacity is required.
Blood component therapy US Medical PG Question 2: A 26-year-old woman is brought to the emergency department after a motor vehicle accident. She was driving on the highway when she was struck by a van. At the hospital she was conscious but was bleeding heavily from an open wound in her left leg. Pulse is 120/min and blood pressure is 96/68 mm Hg. She receives 3 L of intravenous saline and her pulse slowed to 80/min and blood pressure elevated to 116/70 mm Hg. The next morning she is found to have a hemoglobin of 6.2 g/dL. Her team decides to transfuse 1 unit of packed RBCs. Twenty minutes into the transfusion she develops a diffuse urticarial rash, wheezing, fever, and hypotension. The transfusion is immediately stopped and intramuscular epinephrine is administered. Which of the following scenarios is most consistent with this patient's reaction to the blood transfusion?
- A. A patient history of cardiovascular disease
- B. Unsanitary blood product storage practices in the hospital
- C. A patient history of frequent sinopulmonary infections (Correct Answer)
- D. Facial twitching when the patient's cheek is tapped
- E. Prior transfusion reactions caused by the same donor
Blood component therapy Explanation: ***A patient history of frequent sinopulmonary infections***
- The diffuse **urticarial rash, wheezing, fever, and hypotension** after a blood transfusion are classic signs of a **severe allergic reaction (anaphylaxis)**.
- Patients with a history of frequent sinopulmonary infections often have **IgA deficiency**, which can lead to the formation of anti-IgA antibodies. If transfused with blood containing IgA, these antibodies can trigger a severe anaphylactic reaction.
*A patient history of cardiovascular disease*
- While cardiovascular disease can influence how a patient tolerates a transfusion, it does not directly cause the specific constellation of symptoms like **urticaria, wheezing, and fever** that point to an allergic reaction.
- Cardiovascular issues might exacerbate circulatory collapse but wouldn't be the primary cause of an immediate, systemic allergic response.
*Unsanitary blood product storage practices in the hospital*
- Unsanitary storage practices are typically associated with **bacterial contamination** of blood products, leading to a **febrile non-hemolytic transfusion reaction** or **septic shock**, often with severe rigors and high fever.
- This scenario would not commonly present with prominent **urticaria and wheezing** as primary symptoms of an acute reaction.
*Facial twitching when the patient's cheek is tapped*
- Facial twitching when the cheek is tapped is known as **Chvostek's sign**, which is indicative of **hypocalcemia**.
- While rapid transfusion of large volumes of blood can sometimes lead to hypocalcemia due to citrate binding, the primary symptoms described (urticaria, wheezing, fever, hypotension) are not typical of hypocalcemia and point more strongly to an allergic reaction.
*Prior transfusion reactions caused by the same donor*
- While prior reactions to blood from the same donor could occur, it is highly unlikely in this scenario as blood components are typically sourced from various donors.
- The focus is on the patient's intrinsic predisposition (like IgA deficiency) rather than a specific donor incompatibility, especially since this is likely her first transfusion given the trauma.
Blood component therapy US Medical PG Question 3: A 34-year-old primigravida was brought to an obstetric clinic with a chief complaint of painless vaginal bleeding. She was diagnosed with placenta praevia and transfused with 2 units of whole blood. Five hours after the transfusion, she developed a fever and chills. How could the current situation be prevented?
- A. Administering prophylactic epinephrine
- B. ABO grouping and Rh typing before transfusion
- C. Transfusing leukocyte reduced blood products (Correct Answer)
- D. Performing Coombs test before transfusion
- E. Administering prophylactic immunoglobulins
Blood component therapy Explanation: ***Transfusing leukocyte reduced blood products***
- The patient's symptoms of **fever and chills** occurring hours after transfusion are characteristic of a **febrile non-hemolytic transfusion reaction (FNHTR)**.
- FNHTRs are caused by residual **donor leukocytes** in the transfused blood product, which release **cytokines** during storage or react with recipient antibodies, and can be prevented by using **leukoreduced blood products**.
*Administering prophylactic epinephrine*
- **Epinephrine** is used to treat severe **anaphylactic and allergic reactions** but does not prevent the underlying mechanism of FNHTRs.
- Its prophylactic administration is not a standard practice for preventing transfusion reactions like FNHTRs.
*ABO grouping and Rh typing before transfusion*
- **ABO grouping and Rh typing** are crucial for preventing **acute hemolytic transfusion reactions**, which are much more severe and involve erythrocyte incompatibility.
- These tests would not prevent a **febrile non-hemolytic transfusion reaction (FNHTR)** caused by leukocyte components.
*Performing Coombs test before transfusion*
- The **Coombs test (Direct Antiglobulin Test)** detects antibodies attached to red blood cells and is primarily used to diagnose **autoimmune hemolytic anemia** or delayed hemolytic transfusion reactions.
- It does not prevent FNHTRs, which are unrelated to red blood cell incompatibility or antibody-mediated hemolysis.
*Administering prophylactic immunoglobulins*
- **Prophylactic immunoglobulins** are used in specific situations like **immunodeficiency** or **Rh incompatibility (RhoGAM)** to prevent alloimmunization, but not for preventing FNHTRs.
- This intervention would not target the mechanism leading to fever and chills caused by donor leukocyte interactions.
Blood component therapy US Medical PG Question 4: A 55-year-old man with known coronary artery disease presents to the ED with epigastric pain, worsening fatigue, and melena. He takes aspirin and rosuvastatin, but took ibuprofen over the past two weeks for lower back pain. He denies nausea, vomiting, hematemesis, chest pain, fever, and weight loss. Sitting blood pressure is 100/70 mmHg and pulse is 90/min, but standing blood pressure is 85/60 mmHg and pulse is 110/min. Airway is patent. His hands feel cold and clammy. Abdominal exam confirms epigastric pain, but no rebound tenderness or guarding. Despite 2 liters of lactated Ringer's, the blood pressure and pulse have not changed. What hemoglobin (Hb) threshold should be considered if packed red blood cell (pRBC) transfusion is ordered in this patient?
- A. < 10
- B. threshold does not matter
- C. < 9
- D. < 7
- E. < 8 (Correct Answer)
Blood component therapy Explanation: ***< 8***
- This patient presents with signs of **hemodynamic instability** (orthostasis, cold extremities, persistent hypotension despite fluid resuscitation) and active upper gastrointestinal bleeding (melena, epigastric pain, recent NSAID use).
- In patients with **hemodynamic instability** due to acute blood loss, the transfusion threshold is generally higher, at **Hb < 8 g/dL**, to ensure adequate oxygen delivery, especially in the setting of coronary artery disease.
*< 10*
- A transfusion threshold of **Hb < 10 g/dL** is typically reserved for patients with more severe conditions like **unstable angina**, active myocardial ischemia, or when severe symptoms of anemia persist despite an Hb > 8 g/dL.
- While this patient has coronary artery disease, his immediate need for transfusion is driven by acute blood loss and instability, not solely anemic angina.
*threshold does not matter*
- This statement is incorrect as transfusion decisions are based on specific **hemoglobin thresholds** and clinical context to optimize patient outcomes and avoid unnecessary transfusions.
- Ignoring thresholds could lead to either undertransfusion (risking organ damage) or overtransfusion (risking complications like TACO or TRALI).
*< 9*
- An Hb threshold of **< 9 g/dL** might be considered in some scenarios of acute bleeding, but with clear signs of **hemodynamic instability** and severe symptoms, an Hb of 8 g/dL or less is a more commonly accepted trigger.
- The combination of ongoing bleeding, significant orthostasis, and cold extremities points to a more urgent need for correction.
*< 7*
- A transfusion threshold of **Hb < 7 g/dL** is generally applied to hemodynamically stable patients without significant comorbidities, as demonstrated in the TRICC trial.
- This patient is **hemodynamically unstable** and has significant comorbidity (coronary artery disease), warranting a higher transfusion threshold.
Blood component therapy US Medical PG Question 5: A 65-year-old man presents to the emergency department by ambulance following a motor vehicle accident. He was a restrained passenger. At the hospital, he is bleeding heavily from a large wound in his left leg. A review of medical records reveals a history of atrial fibrillation for which he takes warfarin. His international normalized ratio (INR) 2 days ago was 2.6. On physical exam he is cool and clammy. The vital signs include: heart rate 130/min and blood pressure 96/54 mm Hg. Aggressive resuscitation with intravenous normal saline is begun. Which of the following is the next best step to correct this patient's underlying coagulopathy?
- A. Give platelets
- B. Give intravenous vitamin K
- C. Give fresh frozen plasma (FFP) (Correct Answer)
- D. Give cryoprecipitate
- E. Give packed red blood cells
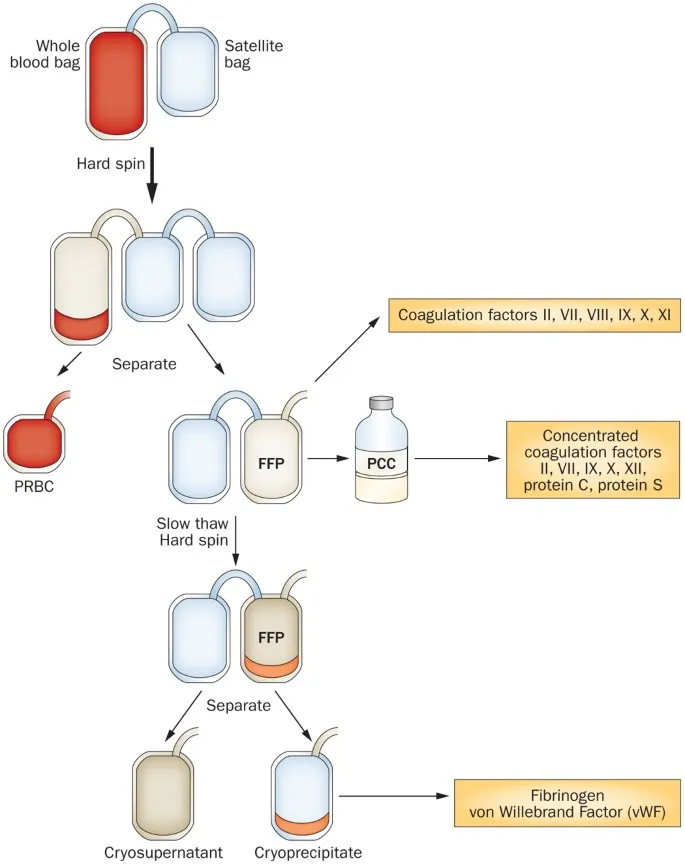
Blood component therapy Explanation: ***Give fresh frozen plasma (FFP)***
- This patient is in **hemorrhagic shock** due to severe bleeding while on **warfarin**, evidenced by tachycardia (HR 130), hypotension (BP 96/54), and cool/clammy skin with an INR of 2.6.
- **Fresh frozen plasma (FFP)** contains all vitamin K-dependent clotting factors (II, VII, IX, X) and is the best option **among those listed** to immediately reverse warfarin's effects in this life-threatening hemorrhage.
- FFP provides rapid reversal within minutes to hours, though it requires large volumes (10-15 mL/kg) and carries risk of transfusion-associated circulatory overload (TACO).
- **Note:** In modern practice, **4-factor prothrombin complex concentrate (PCC)** is preferred over FFP for warfarin reversal (faster, smaller volume, fewer complications), but it is not listed among the options here.
*Give intravenous vitamin K*
- **Vitamin K** reverses warfarin by enabling synthesis of vitamin K-dependent clotting factors (II, VII, IX, X).
- However, it takes **6-24 hours** to produce clinical effect, making it unsuitable as monotherapy for **life-threatening acute bleeding**.
- Vitamin K should be given as **adjunct therapy** alongside FFP, but cannot be the sole intervention in hemorrhagic shock.
*Give platelets*
- **Platelets** are indicated for **thrombocytopenia** (typically <50,000 in active bleeding) or **platelet dysfunction**.
- Warfarin affects **clotting factors**, not platelet count or function, so platelets will not reverse the coagulopathy.
- No indication of thrombocytopenia is mentioned in this case.
*Give cryoprecipitate*
- **Cryoprecipitate** contains **fibrinogen, Factor VIII, Factor XIII, von Willebrand factor, and fibronectin**.
- It does **not contain** the vitamin K-dependent factors (II, VII, IX, X) depleted by warfarin.
- Cryoprecipitate is used for **hypofibrinogenemia** (fibrinogen <100 mg/dL) in massive transfusion or DIC, not for warfarin reversal.
*Give packed red blood cells*
- **Packed red blood cells (PRBCs)** replace blood volume and improve oxygen-carrying capacity in hemorrhagic shock.
- While PRBCs are critical for managing hypovolemia, they **do not contain clotting factors** and will not correct the **warfarin-induced coagulopathy**.
- PRBCs should be transfused in this patient, but they must be combined with FFP to address the underlying bleeding disorder.
Blood component therapy US Medical PG Question 6: A 23-year-old male presents to the emergency room following a gunshot wound to the leg. On arrival his temperature is 99°F (37.2°C), blood pressure is 90/60 mmHg, pulse is 112/min, respirations are 21/min, and pulse oximetry is 99% on room air. Two large bore IVs are placed and he receives crystalloid fluid replacement followed by 2 units of crossmatched packed red blood cells. Immediately following transfusion, his temperature is 102.2°F (39°C), blood pressure is 93/64 mmHg, pulse is 112/min, respirations are 21/min, and pulse oximetry is 99% on room air. There is oozing from his IV sites. You check the records and realize there was a clerical error with the blood bank. What is the mechanism for his current condition?
- A. IgE mediated reaction
- B. Deposition of immune complexes
- C. Production of leukotrienes
- D. Preformed antibodies (Correct Answer)
- E. T lymphocyte reaction
Blood component therapy Explanation: ***Preformed antibodies***
- The patient's symptoms, including **fever**, persistent **hypotension**, and **oozing from IV sites** (which suggests **DIC**), immediately following a transfusion due to a clerical error, are classic signs of an **acute hemolytic transfusion reaction (AHTR)**.
- AHTRs are caused by the recipient's **preformed antibodies** (e.g., anti-A, anti-B) reacting with donor red blood cell antigens, leading to rapid **intravascular hemolysis**, cytokine release, and activation of the coagulation cascade.
*IgE mediated reaction*
- An **IgE-mediated reaction** (Type I hypersensitivity) typically presents with symptoms like **hives, angioedema, bronchospasm, or anaphylaxis**.
- While transfusion reactions can involve allergic components, the clinical picture of severe hemolysis and DIC points away from a primary IgE-mediated anaphylactic response.
*Deposition of immune complexes*
- **Immune complex deposition** (Type III hypersensitivity) is characteristic of conditions like **serum sickness** or **lupus**.
- These reactions usually manifest hours to days after exposure and typically involve features like **arthritis** or **glomerulonephritis**, which are not seen in this acute scenario.
*Production of leukotrienes*
- **Leukotrienes** are mediators of inflammation and bronchoconstriction, prominently involved in **asthma** and some allergic reactions.
- While they may play a secondary role in the inflammatory response, they are not the primary mechanism initiating an **acute hemolytic transfusion reaction**.
*T lymphocyte reaction*
- **T lymphocyte reactions** are central to **delayed-type hypersensitivity** (Type IV) and **graft-versus-host disease (GVHD)**.
- These reactions have a delayed onset (**days to weeks**) and primarily involve cellular immunity, which does not explain the immediate and severe hemolytic reaction observed.
Blood component therapy US Medical PG Question 7: Which of the following is true regarding nicotine substitution therapy?
- A. Preferably given by gastrointestinal route.
- B. Varenicline comes with a black box warning of cardiovascular death
- C. There should be a 15-minute gap between nicotine gum and coffee/soda/acidic food as they decrease its absorption (Correct Answer)
- D. Nicotine chewing gum is better for constant use as it gives 25% higher blood level than lozenges
Blood component therapy Explanation: ***There should be a 15-minute gap between nicotine gum and coffee/soda/acidic food as they decrease its absorption***
- **Acidic beverages** like coffee, soda, and fruit juices can alter the pH of the mouth and stomach, which significantly **reduces the absorption of nicotine** from gum.
- This recommendation ensures optimal **nicotine delivery** and effectiveness of the therapy in reducing withdrawal symptoms.
*Preferably given by gastrointestinal route*
- Nicotine has poor bioavailability when taken orally due to **extensive first-pass metabolism** in the liver.
- Nicotine substitution therapies are therefore preferentially administered via **transdermal**, **buccal** (gum, lozenges), or **nasal routes** to bypass first-pass metabolism and achieve therapeutic blood levels more effectively.
*Varenicline comes with a black box warning of cardiovascular death*
- Varenicline (Chantix) previously had a black box warning for **neuropsychiatric side effects**, including suicidal ideation and depression, which has since been removed due to further studies.
- It does not carry a black box warning specifically for **cardiovascular death**, though cardiovascular events have been a subject of study, particularly in patients with pre-existing cardiovascular conditions.
*Nicotine chewing gum is better for constant use as it gives 25% higher blood level than lozenges*
- While both nicotine gum and lozenges are effective, the **blood levels achieved are comparable**, and the choice often depends on patient preference and proper technique.
- Nicotine gum is best used with a **"chew and park" technique** to allow buccal absorption, and constant chewing can lead to excessive swallowing of nicotine, causing gastrointestinal upset.
Blood component therapy US Medical PG Question 8: An 18-year-old man presents to a rural emergency department after being stabbed multiple times. The patient's past medical history is notable for obesity, diabetes, chronic upper respiratory infections, a 10 pack-year smoking history, and heart failure. He is protecting his airway and he is oxygenating and ventilating well. His temperature is 97.6°F (36.4°C), blood pressure is 74/34 mmHg, pulse is 180/min, respirations are 24/min, and oxygen saturation is 98% on room air. The patient is started on whole blood and the surgeon on call is contacted to take the patient to the operating room. During the secondary survey, the patient complains of shortness of breath. His blood pressure is 54/14 mmHg, pulse is 200/min, respirations are 24/min, and oxygen saturation is 90% on room air. Physical exam is notable for bilateral wheezing on lung exam. The patient goes into cardiac arrest and after 30 minutes, attempts at resuscitation are terminated. Which of the following is associated with this patient's decompensation during resuscitation?
- A. COPD
- B. Congenital long QT syndrome
- C. Heart failure
- D. IgA deficiency
- E. Persistent intraabdominal bleeding (Correct Answer)
Blood component therapy Explanation: ***Persistent intraabdominal bleeding***
- The patient's initial presentation with **uncontrolled hemorrhage due to multiple stab wounds** is the most likely cause of his subsequent decompensation and cardiac arrest. Despite transfusion, persistent bleeding would lead to ongoing **hypovolemic shock**, explaining the worsening hypotension and tachycardia.
- The patient's complaint of shortness of breath and wheezing could be a **reaction to hypovolemic shock** or a **transient pulmonary response** related to the ongoing volume loss and metabolic state, rather than a primary respiratory obstructive process.
*COPD*
- While the patient has a smoking history, his age (18 years old) makes significant **COPD** unlikely to be established enough to cause such a rapid and severe decompensation.
- The **wheezing** could be a non-specific response to shock or hypoperfusion, not necessarily indicative of COPD exacerbation in this acute setting.
*Congenital long QT syndrome*
- This condition is a **cardiac electrical disorder** predisposing to arrhythmias, but it is not directly linked to the traumatic injury or the progressive hypovolemic shock in this clinical scenario.
- There is no specific information in the vignette to suggest an **arrhythmia originating from a prolonged QT interval** as the primary cause of his cardiac arrest.
*Heart failure*
- Although the patient has a history of heart failure, his primary and overwhelming problem is **acute hemorrhagic shock** from the stab wounds. The dramatic drop in blood pressure and rise in heart rate point to volume loss, not primarily cardiogenic shock exacerbation.
- While heart failure can complicate resuscitation, it is not the **direct cause of decompensation** in the face of active, life-threatening hemorrhage.
*IgA deficiency*
- **IgA deficiency** is an immunodeficiency associated with recurrent infections, but it has no direct pathophysiological link to acute traumatic hemorrhage or the rapid cardiovascular collapse experienced by this patient.
- It would not explain the sudden severe signs of **hypovolemic shock** or cardiac arrest in this context.
Blood component therapy US Medical PG Question 9: A 35-year-old man arrives at the emergency department within minutes after a head-on motor vehicle accident. He suffered from blunt abdominal trauma, several lacerations to his face as well as lacerations to his upper and lower extremities. The patient is afebrile, blood pressure is 45/25 mmHg and pulse is 160/minute. A CBC is obtained and is most likely to demonstrate which of the following?
- A. Hb 17 g/dL, Hct 20%
- B. Hb 15 g/dL, Hct 45% (Correct Answer)
- C. Hb 5 g/dL, Hct 30%
- D. Hb 20 g/dL, Hct 60%
- E. Hb 5 g/dL, Hct 20%
Blood component therapy Explanation: ***Hb 15 g/dL, Hct 45%***
- This option represents **normal hemoglobin and hematocrit values**, which are expected in the **initial minutes following acute hemorrhage**.
- In acute blood loss, **whole blood is lost** (both RBCs and plasma together), so the **concentration of RBCs remains unchanged** initially.
- **Hemodilution has not yet occurred**, as there hasn't been enough time for fluid shifts from the extravascular to the intravascular space to dilute the blood.
- This is a **critical teaching point**: early CBC values can be **falsely reassuring** and don't reflect the severity of hemorrhagic shock.
*Hb 17 g/dL, Hct 20%*
- This option shows a **medically implausible combination** - the normal Hb:Hct ratio is approximately **1:3**, so an Hb of 17 g/dL should correspond to an Hct of approximately 51%, not 20%.
- This combination cannot occur physiologically and does not represent any stage of acute blood loss.
*Hb 5 g/dL, Hct 30%*
- This shows an **incorrect Hb:Hct ratio** (6:1 instead of the expected 3:1) - if Hb is 5 g/dL, the Hct should be approximately 15%, not 30%.
- While severe anemia can occur with massive blood loss, this would only be apparent **hours after injury** once hemodilution from fluid shifts occurs, not within minutes.
- The implausible ratio makes this medically incorrect.
*Hb 20 g/dL, Hct 60%*
- These values represent **polycythemia** (abnormally high red blood cell counts), which is the opposite of what would be expected after acute traumatic blood loss.
- The Hb:Hct ratio is appropriate (1:3), but the elevated values suggest chronic hypoxemia, dehydration, or myeloproliferative disorders - not acute hemorrhage.
*Hb 5 g/dL, Hct 20%*
- This shows an **incorrect Hb:Hct ratio** (4:1 instead of the expected 3:1) - if Hb is 5 g/dL, the Hct should be approximately 15%, not 20%.
- Even if we accept these as severe anemia values, they would only be seen **several hours after injury** when sufficient time has passed for fluid shifts and hemodilution to occur, not within minutes of the trauma.
Blood component therapy US Medical PG Question 10: A 58-year-old cirrhotic man with ascites undergoes large volume paracentesis (6 liters removed). Four hours later, he becomes hypotensive (BP 80/50 mmHg) and tachycardic (HR 115/min). Labs show: Cr 2.1 mg/dL (baseline 1.0), Na+ 128 mEq/L, Hct 38%. What is the most appropriate immediate management?
- A. 5% albumin 6-8 grams per liter of ascites removed (Correct Answer)
- B. Normal saline bolus 2 liters
- C. Octreotide and midodrine for hepatorenal syndrome
- D. Vasopressors to maintain blood pressure
- E. Re-infusion of filtered ascitic fluid
Blood component therapy Explanation: ***5% albumin 6-8 grams per liter of ascites removed***
- This patient is experiencing **post-paracentesis circulatory dysfunction (PPCD)**, characterized by hypotension and **acute kidney injury** (doubled creatinine) following a large volume paracentesis (>5L).
- Administration of **intravenous albumin** is the gold standard treatement to expand the **effective arterial blood volume** and prevent further deterioration into hepatorenal syndrome.
*Normal saline bolus 2 liters*
- In cirrhotic patients, **crystalloids** are less effective as they rapidly redistribute into the **interstitial space** (third-spacing) and can worsen ascites/edema.
- Saline does not provide the **oncotic pressure** required to counteract the splanchnic vasodilation typical of PPCD.
*Octreotide and midodrine for hepatorenal syndrome*
- While these agents are used for **Hepatorenal Syndrome (HRS)**, the immediate priority in post-procedure hypotension is **volume expansion** to correct the circulatory dysfunction.
- These medications are typically reserved for patients who do not respond to **volume expansion with albumin** or meet specific criteria for type 1 HRS.
*Vasopressors to maintain blood pressure*
- Vasopressors like **norepinephrine** are generally considered after fluid resuscitation with **albumin** has failed to restore hemodynamic stability.
- Using pressors alone ignores the underlying **intravascular volume deficit** caused by the fluid shift after paracentesis.
*Re-infusion of filtered ascitic fluid*
- This is not a standard or recommended clinical practice due to risks of **infection**, **coagulopathy**, and lack of evidence for efficacy.
- The specific requirement in this pathology is **concentrated albumin** to maintain oncotic pressure, which ascitic fluid does not provide efficiently.
More Blood component therapy US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.