Assessment of volume status US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Assessment of volume status. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Assessment of volume status US Medical PG Question 1: A 56-year-old man is brought to the Emergency Department with intense chest pain that radiates to his left arm and jaw. He also complains of feeling lightheaded. Upon arrival, his blood pressure is 104/60 mm Hg, pulse is 102/min, respiratory rate is 25/min, body temperature is 36.5°C (97.7°F), and oxygen saturation is 94% on room air. An electrocardiogram shows an ST-segment elevation in I, aVL, and V5-6. The patient is transferred to the cardiac interventional suite for a percutaneous coronary intervention. The patient is admitted to the hospital after successful revascularization. During his first night on the ICU floor his urinary output is 0.15 mL/kg/h. Urinalysis shows muddy brown casts. Which of the following outcomes specific to the patient’s condition would you expect to find?
- A. Blood urea nitrogen (BUN):Serum creatinine ratio (Cr) < 15:1 (Correct Answer)
- B. Urinary osmolality 900 mOsmol/kg (normal: 500–800 mOsmol/kg)
- C. Urinary osmolality 550 mOsmol/kg (normal: 500–800 mOsmol/kg)
- D. FENa+ < 1%
- E. Blood urea nitrogen (BUN):Serum creatinine ratio (Cr) > 20:1
Assessment of volume status Explanation: ***Blood urea nitrogen (BUN):Serum creatinine ratio (Cr) < 15:1***
- The patient's presentation with **ST-segment elevation myocardial infarction (STEMI)** followed by low urinary output and **muddy brown casts** strongly indicates **acute tubular necrosis (ATN)**, a form of intrinsic renal failure.
- In ATN, **tubular damage** impairs reabsorption of urea more than creatinine, leading to a **BUN:Cr ratio typically less than 15:1**.
*Urinary osmolality 900 mOsmol/kg (normal: 500–800 mOsmol/kg)*
- A urinary osmolality of 900 mOsmol/kg indicates appropriately concentrated urine, which is characteristic of **prerenal azotemia**, not ATN.
- In ATN, the damaged tubules lose their ability to concentrate urine, resulting in **isosthenuric** urine with osmolality typically **< 350 mOsmol/kg** (approaching plasma osmolality).
*Urinary osmolality 550 mOsmol/kg (normal: 500–800 mOsmol/kg)*
- While 550 mOsmol/kg is within the normal range, it is still **too concentrated for ATN**.
- In ATN, damaged tubules cannot effectively concentrate urine, resulting in **urine osmolality < 350 mOsmol/kg** (isosthenuric, similar to plasma osmolality of ~290 mOsmol/kg).
- This value of 550 mOsmol/kg suggests preserved concentrating ability, which would be more consistent with prerenal azotemia or normal renal function.
*FENa+ < 1%*
- A **fractional excretion of sodium (FENa+) less than 1%** indicates good tubular reabsorption of sodium and is characteristic of **prerenal azotemia**, where the kidneys are attempting to conserve volume.
- In ATN, the damaged tubules cannot effectively reabsorb sodium, so the **FENa+ is typically greater than 2%**.
*Blood urea nitrogen (BUN):Serum creatinine ratio (Cr) > 20:1*
- A **BUN:Cr ratio greater than 20:1** is characteristic of **prerenal azotemia**, reflecting decreased renal perfusion causing increased urea reabsorption relative to creatinine.
- In ATN, the **tubular damage** leads to inefficient urea reabsorption, keeping the ratio **below 15:1**.
Assessment of volume status US Medical PG Question 2: A 27-year-old man is brought to the emergency department 30 minutes after being shot in the abdomen during a violent altercation. His temperature is 36.5°C (97.7°F), pulse is 118/min and regular, and blood pressure is 88/65 mm Hg. Examination shows cool extremities. Abdominal examination shows a 2.5-cm entrance wound in the left upper quadrant at the midclavicular line, below the left costal margin. Focused ultrasound shows free fluid in the left upper quadrant. Which of the following sets of hemodynamic changes is most likely in this patient?
Cardiac output (CO) | Pulmonary capillary wedge pressure (PCWP) | Systemic vascular resistance (SVR) | Central venous pressure (CVP)
- A. ↑ ↓ ↓ ↓
- B. ↓ ↓ ↑ ↑
- C. ↓ ↓ ↓ ↓
- D. ↓ ↓ ↑ ↓ (Correct Answer)
- E. ↓ ↑ ↑ ↑
Assessment of volume status Explanation: ***↓ ↓ ↑ ↓***
- This patient is in **hypovolemic shock** due to hemorrhage, leading to decreased **cardiac output (CO)** and **pulmonary capillary wedge pressure (PCWP)** due to reduced preload.
- The body compensates for hypovolemia by increasing **systemic vascular resistance (SVR)** to maintain perfusion to vital organs, while **central venous pressure (CVP)** decreases due to the depleted blood volume.
*↑ ↓ ↓ ↓*
- An increased **cardiac output** is inconsistent with hypovolemic shock, where the heart's ability to pump blood is compromised by a lack of circulating volume.
- While **PCWP**, **SVR**, and **CVP** decreasing could be seen in some forms of shock, the elevated CO rules out hypovolemic shock.
*↓ ↓ ↑ ↑*
- An elevated **central venous pressure (CVP)** is inconsistent with hypovolemic shock, as CVP reflects right atrial pressure and would be low due to decreased blood volume.
- While other parameters such as **CO** and **PCWP** decreasing and **SVR** increasing can be seen in hypovolemic shock, the increased CVP suggests a different hemodynamic state, like cardiogenic shock.
*↓ ↓ ↓ ↓*
- A decrease in **systemic vascular resistance (SVR)** is characteristic of **distributive shock** (e.g., septic or neurogenic shock), not hypovolemic shock, where compensatory vasoconstriction would lead to increased SVR.
- While **CO**, **PCWP**, and **CVP** would decrease due to overall poor perfusion, the SVR response differentiates it from hypovolemic shock.
*↓ ↑ ↑ ↑*
- An elevated **pulmonary capillary wedge pressure (PCWP)** and **central venous pressure (CVP)** indicate increased fluid volume or cardiac dysfunction, which is contrary to the reduced preload seen in hypovolemic shock.
- While **cardiac output (CO)** may decrease in cardiogenic shock, the other elevated pressures point away from a primary hypovolemic cause.
Assessment of volume status US Medical PG Question 3: On cardiology service rounds, your team sees a patient admitted with an acute congestive heart failure exacerbation. In congestive heart failure, decreased cardiac function leads to decreased renal perfusion, which eventually leads to excess volume retention. To test your knowledge of physiology, your attending asks you which segment of the nephron is responsible for the majority of water absorption. Which of the following is a correct pairing of the segment of the nephron that reabsorbs the majority of all filtered water with the means by which that segment absorbs water?
- A. Distal convoluted tubule via passive diffusion following ion reabsorption
- B. Distal convoluted tubule via aquaporin channels
- C. Thick ascending loop of Henle via passive diffusion following ion reabsorption
- D. Proximal convoluted tubule via passive diffusion following ion reabsorption (Correct Answer)
- E. Collecting duct via aquaporin channels
Assessment of volume status Explanation: ***Proximal convoluted tubule via passive diffusion following ion reabsorption***
- The **proximal convoluted tubule (PCT)** is responsible for reabsorbing approximately **65-70% of filtered water**, making it the primary site of water reabsorption in the nephron.
- This water reabsorption primarily occurs **passively**, following the active reabsorption of solutes (especially **sodium ions**), which creates an osmotic gradient.
*Distal convoluted tubule via passive diffusion following ion reabsorption*
- The **distal convoluted tubule (DCT)** reabsorbs a much smaller percentage of filtered water (around 5-10%) and its water reabsorption is largely **regulated by ADH**, not primarily simple passive diffusion following bulk ion reabsorption.
- While some passive water movement occurs, it is not the main mechanism or location for the majority of water reabsorption.
*Distal convoluted tubule via aquaporin channels*
- While aquaporin channels do play a role in water reabsorption in the DCT, particularly under the influence of **ADH**, the DCT is not the segment responsible for the **majority of all filtered water absorption**.
- The bulk of water reabsorption occurs earlier in the nephron, independently of ADH for the most part.
*Thick ascending loop of Henle via passive diffusion following ion reabsorption*
- The **thick ascending loop of Henle** is primarily involved in reabsorbing ions like Na+, K+, and Cl- but is largely **impermeable to water**.
- Its impermeability to water is crucial for creating the **osmotic gradient** in the renal medulla, which is necessary for later water reabsorption.
*Collecting duct via aquaporin channels*
- The **collecting duct** is critically important for **regulated water reabsorption** via **aquaporin-2 channels** under the influence of **ADH**, allowing for fine-tuning of urine concentration.
- However, it reabsorbs only a variable portion (typically 5-19%) of the remaining filtered water, not the **majority of all filtered water**.
Assessment of volume status US Medical PG Question 4: A 26-year-old male is brought into the emergency room because he collapsed after working out. The patient is a jockey, and he states that he feels dehydrated and has an upcoming meet for which he needs to lose some weight. On exam, the patient has dry mucosa with cracked lips. His temperature is 98.9 deg F (37.2 deg C), blood pressure is 115/70 mmHg, pulse is 105/min, and respirations are 18/min. The patient's blood pressure upon standing up is 94/65 mmHg. His serum Na+ is 125 mEq/L and K+ is 3.0 mEq/L. His urinalysis reveals Na+ of 35 mEq/L and K+ of 32 mEq/L. The abuse of which of the following is most likely responsible for the patient's presentation?
- A. Metoprolol
- B. Polyethylene glycol
- C. Furosemide (Correct Answer)
- D. Spironolactone
- E. Amiloride
Assessment of volume status Explanation: ***Furosemide***
- The patient's **hyponatremia** (Na+ 125 mEq/L), **hypokalemia** (K+ 3.0 mEq/L), and signs of **dehydration** (dry mucosa, cracked lips, orthostatic hypotension, tachycardia) are consistent with the overuse of a **loop diuretic**.
- **Furosemide** inhibits the Na-K-2Cl cotransporter in the **thick ascending limb of the loop of Henle**, leading to significant excretion of sodium, potassium, and water.
- The **high urinary sodium (35 mEq/L) and potassium (32 mEq/L)** confirm **renal wasting**, which is the hallmark of diuretic abuse (as opposed to GI losses or poor intake, which would show low urinary electrolytes).
*Metoprolol*
- **Metoprolol** is a beta-blocker that primarily reduces heart rate and blood pressure, but it does not cause significant electrolyte disturbances like **hyponatremia** or **hypokalemia**, or profound dehydration.
- While it can lower blood pressure, it would not typically cause the combination of **orthostatic hypotension** and electrolyte abnormalities seen here.
*Polyethylene glycol*
- **Polyethylene glycol** is an osmotic laxative used for constipation or bowel preparation, which can cause fluid and electrolyte imbalances but typically presents with **diarrhea** and more pronounced gastrointestinal symptoms.
- Importantly, GI losses would result in **low urinary electrolytes** (kidney conserving electrolytes), not the high urinary Na+ and K+ seen here.
*Spironolactone*
- **Spironolactone** is a potassium-sparing diuretic, which would typically cause **hyperkalemia** rather than the **hypokalemia** observed in this patient.
- It also does not usually cause severe **hyponatremia** or profound dehydration to the extent seen here.
*Amiloride*
- **Amiloride** is a potassium-sparing diuretic, similar to spironolactone, and would lead to **potassium retention** (hyperkalemia) rather than severe **hypokalemia**.
- It has a mild diuretic effect and would not typically cause the profound **electrolyte imbalances** and dehydration observed.
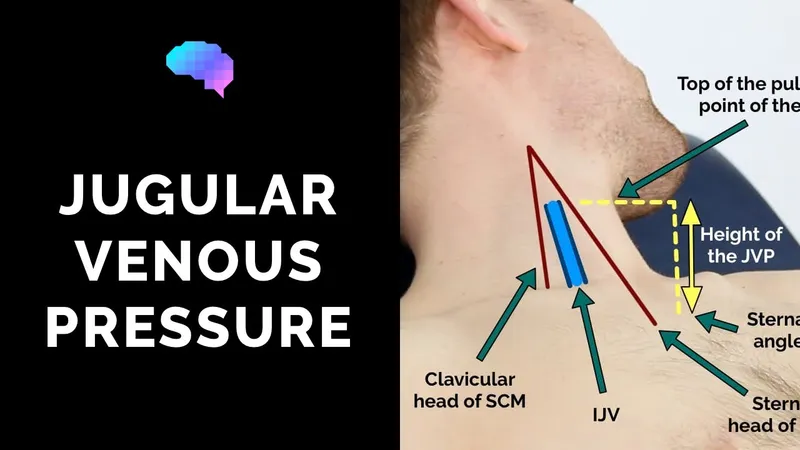
Assessment of volume status US Medical PG Question 5: A 46-year-old male was found unconscious in the field and brought to the emergency department by EMS. The patient was intubated in transit and given a 2 liter bolus of normal saline. On arrival, the patient's blood pressure is 80/60 mmHg and temperature is 37.5°C. Jugular veins are flat and capillary refill time is 4 seconds.
Vascular parameters are measured and are as follows:
Cardiac index - Low
Pulmonary capillary wedge pressure (PCWP) - Low
Systemic vascular resistance - High
Which of the following is the most likely diagnosis?
- A. Septic shock
- B. Anaphylactic shock
- C. Cardiogenic shock
- D. Hypovolemic shock (Correct Answer)
- E. Neurogenic shock
Assessment of volume status Explanation: ***Hypovolemic shock***
- The patient presents with **hypotension**, **flat jugular veins**, **prolonged capillary refill**, and a **low cardiac index** and **low pulmonary capillary wedge pressure (PCWP)**, all indicative of inadequate intravascular volume.
- The **high systemic vascular resistance** is a compensatory mechanism to maintain blood pressure in the setting of decreased circulating volume.
*Septic shock*
- Septic shock typically presents with **vasodilation**, leading to a **low systemic vascular resistance**, which contradicts the findings in this patient.
- While patients can be hypotensive, the vascular parameters, especially SVR, do not align with septic shock.
*Anaphylactic shock*
- This type of shock is characterized by widespread **vasodilation** and increased capillary permeability, leading to a **low systemic vascular resistance** and often significant **edema** or **urticaria**, none of which are suggested here.
- While it can cause hypotension and low PCWP due to fluid shifts, the high SVR makes it less likely.
*Cardiogenic shock*
- Cardiogenic shock is characterized by **pump failure**, leading to a **low cardiac index** but a **high PCWP** due to fluid backup in the pulmonary circulation.
- This directly contrasts the patient's low PCWP.
*Neurogenic shock*
- Neurogenic shock involves a loss of **sympathetic tone**, resulting in widespread **vasodilation** and a **low systemic vascular resistance**, often accompanied by **bradycardia**.
- The high SVR in this patient rules out neurogenic shock.
Assessment of volume status US Medical PG Question 6: A 78-year-old male with history of coronary artery disease, status post coronary stent placement currently on aspirin and clopidogrel was found down in his bathroom by his wife. His GCS score was 3 and an accurate physical exam is limited. A stat non-contrast CT scan of his brain demonstrated a large right parietal intracranial hemorrhage with surrounding edema. He was promptly transferred to the intensive care unit (ICU) for monitoring. Over the next day, his mental status continues to worsen but repeat CT scan shows no new bleeding. In addition, the patient’s urinary output has been >200 cc/hr over the last several hours and increasing. His temperature is 99.0 deg F (37.2 deg C), blood pressure is 125/72 mmHg, pulse is 87/min, and respirations are 13/min. Which of the following values would most likely correspond to the patient’s urine specific gravity, urine osmolality, plasma osmolality, and serum sodium?
- A. Low, High, High, High
- B. Low, Low, High, High (Correct Answer)
- C. High, High, Low, Low
- D. Low, Low, High, Low
- E. High, Low, Low, High
Assessment of volume status Explanation: ***Low, Low, High, High***
- This patient's presentation, particularly the **large intracranial hemorrhage**, worsening mental status despite no new bleeding, and especially the **high urinary output (>200 cc/hr)**, is classic for **diabetes insipidus (DI)**, often neurogenic DI, due to damage to the posterior pituitary or hypothalamus.
- In DI, there is a deficiency of **ADH (vasopressin)**, leading to the kidneys' inability to reabsorb water. This results in the excretion of large volumes of **dilute urine** (low urine specific gravity, low urine osmolality) and concentration of the plasma (high plasma osmolality and hypernatremia, which means high serum sodium).
*Low, High, High, High*
- This pattern would indicate concentrated urine alongside concentrated plasma and high sodium, which contradicts the presence of **polyuria** and the underlying pathology of **diabetes insipidus (DI)**.
- High urine osmolality and specific gravity would suggest intact ADH function and water reabsorption in the kidneys, which is not what occurs in DI.
*High, High, Low, Low*
- This profile describes a state of **concentrated urine** but **dilute plasma** and **hyponatremia**, which is characteristic of the **Syndrome of Inappropriate Antidiuretic Hormone (SIADH)**.
- SIADH is the opposite of diabetes insipidus, involving excessive ADH leading to water retention, not excessive water excretion.
*Low, Low, High, Low*
- While **low urine specific gravity** and **low urine osmolality** are consistent with diabetes insipidus, a **low serum sodium** (hyponatremia) is not.
- In diabetes insipidus, the loss of free water typically leads to **hypernatremia** as the body becomes dehydrated.
*High, Low, Low, High*
- This combination is inconsistent with any common clinical scenario. A **high urine specific gravity** with a **low urine osmolality** is contradictory, as specific gravity is a measure of urine concentration, which correlates with osmolality.
- Furthermore, a **low plasma osmolality** with a **high serum sodium** is physiologically improbable.
Assessment of volume status US Medical PG Question 7: A 48-year-old female presents to the emergency room with mental status changes.
Laboratory analysis of the patient's serum shows:
Na 122 mEq/L
K 3.9 mEq/L
HCO3 24 mEq/L
BUN 21 mg/dL
Cr 0.9 mg/dL
Ca 8.5 mg/dL
Glu 105 mg/dL
Urinalysis shows:
Osmolality 334 mOsm/kg
Na 45 mEq/L
Glu 0 mg/dL
Which of the following is the most likely diagnosis?
- A. Diabetes insipidus
- B. Aspirin overdose
- C. Primary polydipsia
- D. Diarrhea
- E. Lung cancer (Correct Answer)
Assessment of volume status Explanation: ***Lung cancer***
- The patient presents with **hyponatremia** (Na 122 mEq/L) and **mental status changes**, along with a **euvolemic state** (normal BUN, creatinine, and potassium), which are characteristic of **Syndrome of Inappropriate Antidiuretic Hormone (SIADH)**.
- **Small cell lung cancer** is a common cause of **ectopic ADH production**, leading to SIADH.
*Diabetes insipidus*
- Characterized by **hypernatremia** and the excretion of **large volumes of dilute urine** (low urine osmolality), which contradicts the patient's hyponatremia and relatively concentrated urine (334 mOsm/kg).
- This condition involves insufficient ADH or renal unresponsiveness to ADH, leading to free water loss, not retention.
*Aspirin overdose*
- Typically causes an **acid-base disturbance**, often a mixed respiratory alkalosis and metabolic acidosis, and may lead to **tinnitus** and **hyperthermia**.
- While it can affect mental status, it does not directly explain the specific pattern of **hyponatremia** and urine osmolality observed.
*Primary polydipsia*
- Usually results in **hyponatremia** due to excessive water intake, but the urine would be **maximally dilute** (urine osmolality < 100 mOsm/kg) as the kidneys try to excrete the excess water.
- The patient's urine osmolality of 334 mOsm/kg indicates that the kidneys are still able to concentrate urine somewhat, making primary polydipsia less likely.
*Diarrhea*
- Causes **volume depletion** and can lead to various electrolyte abnormalities, but typically results in **hypernatremia** or isotonic hyponatremia with signs of dehydration.
- The patient's lab values do not show signs of dehydration or a primary gastrointestinal disturbance.
Assessment of volume status US Medical PG Question 8: A 32-year-old man is brought to the Emergency Department after 3 consecutive days of diarrhea, fatigue and weakness. His stool has been soft and mucoid, with no blood stains. The patient just came back from a volunteer mission in Guatemala, where he remained asymptomatic. His personal medical history is unremarkable. Today his blood pressure is 98/60 mm Hg, pulse is 110/min, respiratory rate is 19/min, and his body temperature is 36.7°C (98.1°F). On physical exam, he has sunken eyes, dry mucosa, mild diffuse abdominal tenderness, and hyperactive bowel sounds. Initial laboratory tests are shown below:
Serum creatinine (SCr) 1.8 mg/dL
Blood urea nitrogen (BUN) 50 mg/dL
Serum sodium 132 mEq/L
Serum potassium 3.5 mEq/L
Serum chloride 102 mEq/L
Which of the following phenomena would you expect in this patient?
- A. Low urine osmolality, high FeNa+, high urine Na+
- B. High urine osmolality, high fractional excretion of sodium (FeNa+), high urine Na+
- C. Low urine osmolality, high FeNa+, low urine Na+
- D. High urine osmolality, low FeNa+, low urine Na+ (Correct Answer)
- E. Low urine osmolality, low FeNa+, high urine Na+
Assessment of volume status Explanation: ***High urine osmolality, low FeNa+, low urine Na+***
- The patient exhibits signs of **dehydration** (hypotension, tachycardia, sunken eyes, dry mucosa) and **acute kidney injury (AKI)** with elevated BUN and creatinine, particularly a **BUN/creatinine ratio of 27.8** (50/1.8). These findings point to **prerenal AKI** due to hypovolemia from diarrhea.
- In prerenal AKI, the kidneys attempt to conserve water and sodium to restore intravascular volume. This leads to **increased ADH** secretion and **aldosterone**, resulting in **high urine osmolality** (concentrated urine), **low fractional excretion of sodium (FeNa+)** (<1%), and **low urine sodium concentration** (<20 mEq/L).
*Low urine osmolality, high FeNa+, high urine Na+*
- This pattern is typical of **acute tubular necrosis (ATN)**, an intrinsic cause of AKI, where tubular damage impairs the kidney's ability to concentrate urine and reabsorb sodium.
- The context of dehydration and prerenal state makes ATN less likely as the initial primary pathology compared to the body's compensatory mechanisms during hypovolemia.
*High urine osmolality, high fractional excretion of sodium (FeNa+), high urine Na+*
- This combination is generally contradictory. High urine osmolality suggests water conservation, while high FeNa+ and urine Na+ indicate sodium wasting, which would typically be seen in diuretic use or specific renal tubular disorders, not uncompensated hypovolemia.
- In prerenal AKI, the body actively reabsorbs sodium to expand volume, leading to low rather than high FeNa+ and urine Na+.
*Low urine osmolality, high FeNa+, low urine Na+*
- This combination is inconsistent. High FeNa+ and low urine Na+ do not usually occur together in a state of hypovolemia. If FeNa+ is high, it implies significant sodium excretion, which would typically be accompanied by higher urine Na+.
- Low urine osmolality also suggests impaired concentrating ability, which is not characteristic of the compensatory mechanisms in prerenal AKI.
*Low urine osmolality, low FeNa+, high urine Na+*
- This combination is also contradictory. Low urine osmolality with low FeNa+ and high urine Na+ does not align with typical kidney responses to dehydration or specific AKI etiologies.
- Low FeNa+ and high urine Na+ are conflicting, as low FeNa+ implies sodium conservation, while high urine Na+ indicates sodium excretion.
Assessment of volume status US Medical PG Question 9: A critical care fellow is interested in whether the auscultatory finding of pulmonary rales can accurately predict hypervolemic state. He conducts a study in 100 patients with volume overloaded state confirmed by a Swan Ganz catheter in his hospital's cardiac critical care unit. He also recruits 100 patients with euvolemic state confirmed by Swan Ganz catheter. He subsequently examines all patients in the unit for rales and finds that 80 patients in the hypervolemic group have rales in comparison to 50 patients in the euvolemic group. Which of the following is the positive predictive value of rales for the presence of hypervolemia?
- A. 50/100
- B. 80/100
- C. 50/70
- D. 80/130 (Correct Answer)
- E. 100/200
Assessment of volume status Explanation: ***80/130***
- The **positive predictive value (PPV)** is the probability that a patient who tests positive for a disease (rales) actually has the disease (hypervolemia). It is calculated as **True Positives / (True Positives + False Positives)**.
- In this study, 80 hypervolemic patients had rales (True Positives), and 50 euvolemic patients had rales (False Positives). Therefore, PPV = 80 / (80 + 50) = 80/130.
*50/100*
- This fraction represents the **false positive rate** for rales in this study (50 euvolemic patients with rales out of 100 euvolemic patients).
- It does not account for the true positives or the overall positive test results, making it an incorrect calculation for PPV.
*80/100*
- This fraction represents the **sensitivity** of rales for hypervolemia (80 hypervolemic patients with rales out of 100 hypervolemic patients).
- Sensitivity measures the proportion of actual positives that are correctly identified, not the positive predictive value.
*50/70*
- This fraction represents the **negative predictive value (NPV)**, which is the probability that a patient without rales (negative test) truly does not have hypervolemia.
- NPV = True Negatives / (True Negatives + False Negatives) = 50 / (50 + 20) = 50/70, where 50 euvolemic patients lack rales and 20 hypervolemic patients lack rales.
- While this is a valid epidemiological measure, the question specifically asks for PPV, not NPV.
*100/200*
- This represents the **overall prevalence of hypervolemia** in the entire study population (100 hypervolemic patients out of 200 total patients).
- It does not consider the presence or absence of rales and is unrelated to the positive predictive value of rales.
Assessment of volume status US Medical PG Question 10: An 18-year-old man presents to a rural emergency department after being stabbed multiple times. The patient's past medical history is notable for obesity, diabetes, chronic upper respiratory infections, a 10 pack-year smoking history, and heart failure. He is protecting his airway and he is oxygenating and ventilating well. His temperature is 97.6°F (36.4°C), blood pressure is 74/34 mmHg, pulse is 180/min, respirations are 24/min, and oxygen saturation is 98% on room air. The patient is started on whole blood and the surgeon on call is contacted to take the patient to the operating room. During the secondary survey, the patient complains of shortness of breath. His blood pressure is 54/14 mmHg, pulse is 200/min, respirations are 24/min, and oxygen saturation is 90% on room air. Physical exam is notable for bilateral wheezing on lung exam. The patient goes into cardiac arrest and after 30 minutes, attempts at resuscitation are terminated. Which of the following is associated with this patient's decompensation during resuscitation?
- A. COPD
- B. Congenital long QT syndrome
- C. Heart failure
- D. IgA deficiency
- E. Persistent intraabdominal bleeding (Correct Answer)
Assessment of volume status Explanation: ***Persistent intraabdominal bleeding***
- The patient's initial presentation with **uncontrolled hemorrhage due to multiple stab wounds** is the most likely cause of his subsequent decompensation and cardiac arrest. Despite transfusion, persistent bleeding would lead to ongoing **hypovolemic shock**, explaining the worsening hypotension and tachycardia.
- The patient's complaint of shortness of breath and wheezing could be a **reaction to hypovolemic shock** or a **transient pulmonary response** related to the ongoing volume loss and metabolic state, rather than a primary respiratory obstructive process.
*COPD*
- While the patient has a smoking history, his age (18 years old) makes significant **COPD** unlikely to be established enough to cause such a rapid and severe decompensation.
- The **wheezing** could be a non-specific response to shock or hypoperfusion, not necessarily indicative of COPD exacerbation in this acute setting.
*Congenital long QT syndrome*
- This condition is a **cardiac electrical disorder** predisposing to arrhythmias, but it is not directly linked to the traumatic injury or the progressive hypovolemic shock in this clinical scenario.
- There is no specific information in the vignette to suggest an **arrhythmia originating from a prolonged QT interval** as the primary cause of his cardiac arrest.
*Heart failure*
- Although the patient has a history of heart failure, his primary and overwhelming problem is **acute hemorrhagic shock** from the stab wounds. The dramatic drop in blood pressure and rise in heart rate point to volume loss, not primarily cardiogenic shock exacerbation.
- While heart failure can complicate resuscitation, it is not the **direct cause of decompensation** in the face of active, life-threatening hemorrhage.
*IgA deficiency*
- **IgA deficiency** is an immunodeficiency associated with recurrent infections, but it has no direct pathophysiological link to acute traumatic hemorrhage or the rapid cardiovascular collapse experienced by this patient.
- It would not explain the sudden severe signs of **hypovolemic shock** or cardiac arrest in this context.
More Assessment of volume status US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.