Thyroidectomy indications and techniques US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Thyroidectomy indications and techniques. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Thyroidectomy indications and techniques US Medical PG Question 1: A 48-year-old woman underwent a thyroidectomy with central neck dissection due to papillary thyroid carcinoma. On day 2 postoperatively, she developed irritability, dysphagia, difficulty breathing, and spasms in different muscle groups in her upper and lower extremities. The vital signs include blood pressure 102/65 mm Hg, heart rate 93/min, respiratory rate 17/min, and temperature 36.1℃ (97.0℉). Physical examination shows several petechiae on her forearms, muscle twitching in her upper and lower extremities, expiratory wheezes on lung auscultation, decreased S1 and S2 and the presence of an S3 on cardiac auscultation, and positive Trousseau and Chvostek signs. Laboratory studies show:
Ca2+ 4.4 mg/dL
Mg2+ 1.7 mEq/L
Na+ 140 mEq/L
K+ 4.3 mEq/L
Cl- 107 mEq/L
HCO3- 25 mEq/L
Administration of which of the following agents could prevent the patient’s condition?
- A. Anticonvulsants prior to and for 1 week after the operation
- B. Vitamin D and ionic calcium prior to and 2 weeks after the operation (Correct Answer)
- C. Potassium supplementation prior to and 2 weeks after the operation
- D. Calcium gluconate intraoperatively
- E. Magnesium sulfate intraoperatively
Thyroidectomy indications and techniques Explanation: ***Vitamin D and ionic calcium prior to and 2 weeks after the operation***
- The patient's symptoms are consistent with **hypocalcemia** (low calcium), a common complication after thyroidectomy due to inadvertent parathyroid gland removal or damage. Prophylactic **calcium and vitamin D supplementation** can prevent severe postoperative hypocalcemia by helping maintain calcium homeostasis.
- The patient's calcium level of 4.4 mg/dL (normal range 8.5-10.2 mg/dL) confirms severe hypocalcemia. The presence of **Trousseau and Chvostek signs**, muscle spasms, and dysphagia are classic signs of hypocalcemic tetany.
*Anticonvulsants prior to and for 1 week after the operation*
- This patient's symptoms are not indicative of an underlying seizure disorder, but rather **neuromuscular excitability** due to hypocalcemia. Anticonvulsants would not address the root cause.
- While severe hypocalcemia can rarely lead to seizures, prophylactic anticonvulsant administration is not standard practice for preventing this specific post-thyroidectomy complication.
*Potassium supplementation prior to and 2 weeks after the operation*
- The patient's potassium level is 4.3 mEq/L, which is within the normal range (3.5-5.0 mEq/L). **Hyperkalemia or hypokalemia** is not the primary issue here.
- Potassium supplementation would not address the hypocalcemia causing her symptoms and could potentially lead to **hyperkalemia**, which has its own set of dangers.
*Calcium gluconate intraoperatively*
- **Intraoperative calcium gluconate** is typically used for acute, severe hypocalcemia or cardiac arrest, not as a prophylactic measure. Administering it intraoperatively would not prevent the delayed onset of hypocalcemia seen on day 2.
- The goal is to prevent hypocalcemia by supporting calcium levels proactively, rather than treating an acute drop during surgery, which is rare.
*Magnesium sulfate intraoperatively*
- The patient's magnesium level of 1.7 mEq/L is at the lower limit of normal (1.7-2.2 mEq/L). While **hypomagnesemia** can impair PTH secretion and cause refractory hypocalcemia, magnesium supplementation is not the primary prophylactic strategy for post-thyroidectomy hypocalcemia.
- Intraoperative magnesium sulfate would not address the fundamental issue of parathyroid gland injury or removal causing the hypocalcemia. Calcium and vitamin D remain the cornerstone of prevention.
Thyroidectomy indications and techniques US Medical PG Question 2: A 50-year-old man is brought in by ambulance to the emergency department with difficulty breathing and speaking. His wife reports that he might have swallowed a fishbone. While taking his history the patient develops a paroxysmal cough. Visualization of his oropharynx and larynx shows a fishbone lodged in the right piriform recess. After successfully removing the fishbone the patient feels comfortable, but he is not able to cough like before. Damage to which of the following nerves is responsible for the impaired cough reflex in this patient?
- A. Inferior laryngeal nerve
- B. Internal laryngeal nerve (Correct Answer)
- C. External laryngeal nerve
- D. Superior laryngeal nerve
- E. Recurrent laryngeal nerve
Thyroidectomy indications and techniques Explanation: ***Internal laryngeal nerve***
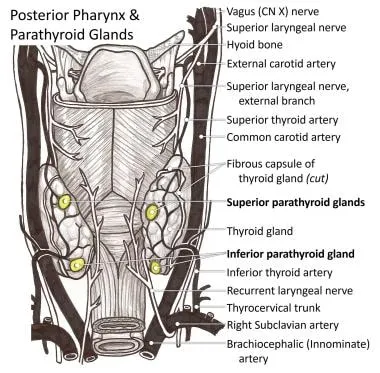
- The internal laryngeal nerve is the **sensory nerve** of the larynx above the vocal cords, including the piriform recess. Damage to this nerve, often due to trauma from a foreign body like a fishbone, impairs the **afferent limb of the cough reflex**.
- A fishbone lodged in the **piriform recess** directly implicates the sensory function of the internal laryngeal nerve, explaining the subsequent loss of the cough reflex even after removal of the foreign body.
*Inferior laryngeal nerve*
- This nerve is primarily **motor** to almost all intrinsic laryngeal muscles and provides **sensory innervation** below the vocal folds. Damage would primarily affect phonation (hoarseness) or breathing due to vocal cord paralysis.
- It would not directly affect the sensory input initiating a cough reflex from the piriform recess, which is above the vocal folds.
*External laryngeal nerve*
- The external laryngeal nerve is a **motor nerve** supplying the **cricothyroid muscle**, which is responsible for tensing the vocal cords and altering voice pitch.
- Damage to this nerve would lead to **hoarseness** and difficulty with high-pitched sounds, not an impaired cough reflex from the piriform recess.
*Superior laryngeal nerve*
- The superior laryngeal nerve divides into the internal and external laryngeal nerves. While it contains sensory fibers that lead to the internal laryngeal nerve, stating damage to the entire superior laryngeal nerve is less specific than identifying the internal laryngeal nerve as the direct cause of the sensory deficit.
- Damage to the superior laryngeal nerve would encompass both sensory and motor deficits (internal and external branches), but the specific symptom of impaired cough reflex primarily points to the internal laryngeal branch.
*Recurrent laryngeal nerve*
- This nerve is another name for the **inferior laryngeal nerve** and is primarily **motor** to the intrinsic laryngeal muscles (except cricothyroid) and provides sensory innervation below the vocal cords.
- Damage to this nerve primarily results in **vocal cord paralysis** and voice changes (hoarseness), not the sensory loss affecting the cough reflex from the piriform recess.
Thyroidectomy indications and techniques US Medical PG Question 3: A 4-year-old-female presents with a flattened, reddish 2 cm lump located at the base of the tongue. The patient's mother reports her having trouble swallowing, often leading to feeding difficulties. The mother also reports lethargy, constipation, dry skin, and hypothermia. Which of the following is the most appropriate management of this patient’s presentation?
- A. Week-long course of penicillin
- B. No treatment is necessary, counsel mother on alternative feeding techniques
- C. Thyroid hormone replacement therapy with levothyroxine (Correct Answer)
- D. Combination therapy of methimazole and Beta-blockers
- E. Radioactive iodine ablation
Thyroidectomy indications and techniques Explanation: ***Thyroid hormone replacement therapy with levothyroxine***
- The patient's symptoms of **lethargy, constipation, dry skin, and hypothermia** are classic signs of **hypothyroidism**
- The **flattened, reddish 2 cm lump at the base of the tongue** causing **dysphagia** is highly suggestive of a **lingual thyroid**, a developmental anomaly where thyroid tissue fails to descend from the base of the tongue during embryonic development
- In **90% of lingual thyroid cases**, this ectopic tissue represents the **only functioning thyroid tissue** in the body, leading to hypothyroidism
- **Levothyroxine replacement** is the first-line management, addressing the hypothyroidism and often reducing the size of the lingual thyroid mass, improving swallowing difficulties
- Surgical excision is reserved for cases where medical management fails or severe airway/swallowing obstruction persists
*Week-long course of penicillin*
- Penicillin is an **antibiotic** used to treat **bacterial infections**
- The patient's symptoms indicate an **endocrine disorder** (hypothyroidism) and **developmental anomaly** (lingual thyroid), not an infectious process
- No signs of infection such as fever, leukocytosis, or acute inflammation are present
*No treatment is necessary, counsel mother on alternative feeding techniques*
- Given the **significant systemic symptoms** of hypothyroidism (lethargy, constipation, dry skin, hypothermia) and feeding difficulties, **treatment is clearly necessary**
- **Untreated congenital hypothyroidism** in a child leads to severe developmental delays, intellectual disability, and growth retardation (cretinism)
- While feeding techniques may help with dysphagia, they do not address the underlying hypothyroidism requiring urgent treatment
*Combination therapy of methimazole and Beta-blockers*
- **Methimazole** (antithyroid medication) and **beta-blockers** are used to treat **hyperthyroidism** (overactive thyroid)
- The patient's symptoms (lethargy, constipation, hypothermia, dry skin) are characteristic of **hypothyroidism** (underactive thyroid), making antithyroid therapy completely inappropriate
- This would further suppress thyroid function and worsen the patient's condition
*Radioactive iodine ablation*
- **Radioactive iodine (I-131) ablation** is used to treat **hyperthyroidism** (Graves' disease, toxic nodules) or **thyroid cancer**
- It is a **destructive treatment** that eliminates thyroid tissue
- In this patient with a **lingual thyroid likely representing the only functioning thyroid tissue**, ablation would cause **complete thyroid failure** and severe, permanent hypothyroidism
- Radioactive iodine is also **contraindicated in children** except for specific cases of thyroid cancer
Thyroidectomy indications and techniques US Medical PG Question 4: A 29-year-old woman presents to a physician for evaluation of palpitations, increased sweating, and unintentional weight loss despite a good appetite. She also reports difficulty swallowing and voice changes. All of the symptoms have developed over the past 6 months. The patient has no concurrent illnesses and takes no medications. The vital signs include the following: blood pressure 125/80 mm Hg, heart rate 106/min, respiratory rate 15/min, and temperature 37.0℃ (98.6℉). The physical examination was significant for increased perspiration, fine digital tremors, and a small mass on the posterior aspect of the tongue, which moves with movements of the tongue. There is no neck swelling. The thyroid profile is as follows:
Triiodothyronine (T3) 191 ng/dL (2.93 nmol/L)
Thyroxine (T4), total 22 µg/dL (283.1 nmol/L)
Thyroid-stimulating hormone (TSH) 0.2 µU/mL (0.2 mU/L)
A radioiodine thyroid scan reveals hyper-functional thyroid tissue at the base of the patient’s tongue. Which of the following statements is correct?
- A. This patient is at increased risk of thyroid carcinoma development.
- B. There is a male predilection for this condition.
- C. This condition results from a failure of caudal migration of thyroid tissue. (Correct Answer)
- D. Most often in such a condition, there is an additional thyroid tissue elsewhere in the neck.
- E. Ectopic thyroid tissue is most commonly found in the mediastinum.
Thyroidectomy indications and techniques Explanation: ***This condition results from a failure of caudal migration of thyroid tissue.***
- This patient's symptoms (palpitations, sweating, weight loss with good appetite, dysphagia, voice changes, and a mass at the base of the tongue, along with **hyperthyroidism** on labs) are highly suggestive of a **lingual thyroid**.
- **Lingual thyroid** occurs when the thyroid gland fails to descend from its embryological origin at the **foramen cecum** at the base of the tongue to its normal position in the neck during embryological development.
*This patient is at increased risk of thyroid carcinoma development.*
- While thyroid carcinoma can occur in lingual thyroids, the risk is generally **low**, ranging from 1-3%. The primary concern is often the obstructive symptoms and hyperthyroidism.
- The most significant association with increased risk of thyroid carcinoma is usually with **radiation exposure** or certain genetic syndromes, which are not mentioned here.
*There is a male predilection for this condition.*
- **Lingual thyroid** is more common in **females**, with a female-to-male ratio of approximately 4:1 to 7:1.
- This condition is also more often diagnosed during periods of **increased physiological demand for thyroid hormones**, such as puberty, pregnancy, or menopause.
*Most often in such a condition, there is an additional thyroid tissue elsewhere in the neck.*
- In over 70% of cases, the lingual thyroid is the **ONLY functioning thyroid tissue** present in the patient.
- This is why surgical removal of a lingual thyroid requires careful consideration of potential **post-operative hypothyroidism** and lifelong hormone replacement.
*Ectopic thyroid tissue is most commonly found in the mediastinum.*
- The **base of the tongue (lingual thyroid)** is the **most common site** of ectopic thyroid tissue, accounting for approximately 90% of cases.
- Other less common locations for ectopic thyroid include sublingual, subhyoid, mediastinal, and very rarely intracardiac or intrasplenic areas.
Thyroidectomy indications and techniques US Medical PG Question 5: A six year-old female presents for evaluation of dry skin, fatigue, sensitivity to cold and constipation. The patient’s mother recalls that the patient had surgery to remove a “benign mass” at the base of her tongue 3 months ago because of trouble swallowing. What was the likely cause of the surgically removed mass?
- A. Failed caudal migration of the thyroid gland (Correct Answer)
- B. Iodine deficiency
- C. Failed fusion of the palatine shelves with the nasal septum
- D. Radiation exposure
- E. Maternal Diabetes Mellitus
Thyroidectomy indications and techniques Explanation: ***Failed caudal migration of the thyroid gland***
- The symptoms of **dry skin, fatigue, cold sensitivity, and constipation** are classic signs of **hypothyroidism**.
- A mass at the **base of the tongue** that is later removed and leads to hypothyroidism strongly suggests a **lingual thyroid**, which results from the thyroid gland's **failure to descend** from its embryonic origin at the foramen cecum.
*Iodine deficiency*
- While iodine deficiency can cause **hypothyroidism** and **goiter**, it typically does not present as a **discrete mass** at the base of the tongue requiring surgical removal.
- It would usually result in a more generalized **enlargement of the thyroid gland**, often in the neck.
*Failed fusion of the palatine shelves with the nasal septum*
- This developmental anomaly leads to a **cleft palate**, affecting the **roof of the mouth**.
- It has no direct association with thyroid function or masses at the base of the tongue.
*Radiation exposure*
- Radiation exposure can increase the risk of thyroid cancer or hypothyroidism later in life, but it typically doesn't cause a congenital benign mass at the base of the tongue that presents in early childhood.
- Furthermore, the specific presentation points to a developmental anomaly rather than an acquired condition.
*Maternal Diabetes Mellitus*
- Maternal diabetes can lead to various congenital anomalies in the fetus, such as **macrosomia, caudal regression syndrome, or cardiac defects**.
- However, it is not a recognized cause of a lingual thyroid or a failure of thyroid migration.
Thyroidectomy indications and techniques US Medical PG Question 6: A previously healthy 39-year-old woman comes to the physician because of a slowly enlarging, painless neck mass that she first noticed 3 months ago. During this period, she has also experienced intermittent palpitations, hair loss, and a weight loss of 4.5 kg (10 lb). There is no personal or family history of serious illness. She appears anxious and fidgety. Her temperature is 37.1°C (98.8°F), pulse is 101/min and irregular, respirations are 16/min, and blood pressure is 140/90 mm Hg. Physical examination shows a firm, nontender left anterior cervical nodule that moves with swallowing. Laboratory studies show:
TSH 0.4 μU/mL
T4 13.2 μg/dL
T3 196 ng/dL
Ultrasonography confirms the presence of a 3-cm solid left thyroid nodule. A thyroid 123I radionuclide scintigraphy scan shows increased uptake in a nodule in the left lobe of the thyroid gland with suppression of the remainder of the thyroid tissue. Which of the following is the most likely underlying mechanism of this patient's condition?
- A. Gain-of-function mutations of the TSH receptor (Correct Answer)
- B. Thyroglobulin antibody production
- C. Activation of oncogenes promoting cell division
- D. Persistent TSH stimulation and heterogeneous thyroid tissue hyperplasia
- E. Thyroid peroxidase autoantibody-mediated destruction of thyroid tissue
Thyroidectomy indications and techniques Explanation: ***Gain-of-function mutations of the TSH receptor***
- The patient's symptoms (palpitations, weight loss, anxiety, irregular pulse) and lab results (low TSH, high T3/T4) indicate **hyperthyroidism**. The **hot nodule** on scintigraphy with suppressed surrounding tissue points to a **toxic adenoma**.
- **Gain-of-function mutations** in the TSH receptor gene (e.g., *TSHR* gene) cause constitutive activation of the receptor, leading to autonomous thyroid hormone production independent of TSH.
*Thyroglobulin antibody production*
- **Antithyroglobulin antibodies** are typically associated with autoimmune thyroid diseases like **Hashimoto's thyroiditis** (hypothyroidism) or occasionally Graves' disease (hyperthyroidism), but the specific presentation here points to a functional nodule.
- While they can be present in Graves' disease, the scintigraphy showing a **single hot nodule** with suppressed surrounding tissue is not characteristic of Graves' disease, which typically shows diffuse uptake.
*Activation of oncogenes promoting cell division*
- While thyroid nodules can be malignant and involve **oncogene activation** (e.g., *BRAF, RET/PTC*), this mechanism primarily relates to uncontrolled cell growth and **cancer**, not necessarily hyperfunction and excessive hormone production (toxic nodule).
- Malignant nodules are typically "cold" on scintigraphy, meaning they do not take up iodine, unlike the **"hot" nodule** described in this patient.
*Persistent TSH stimulation and heterogeneous thyroid tissue hyperplasia*
- This description is characteristic of a **multinodular goiter** or **diffuse hyperplasia**, often seen in conditions of **chronic TSH stimulation** (e.g., iodine deficiency leading to hypothyroidism and compensatory TSH rise).
- The patient has **suppressed TSH** and a **single hyperfunctioning nodule**, not diffuse hyperplasia or chronic TSH stimulation.
*Thyroid peroxidase autoantibody-mediated destruction of thyroid tissue*
- **Thyroid peroxidase (TPO) antibodies** are involved in **Hashimoto's thyroiditis**, an autoimmune condition leading to gradual **destruction of thyroid tissue** and **hypothyroidism**.
- This patient presents with **hyperthyroidism** and a hyperfunctioning nodule, which is the opposite of the clinical picture seen with TPO antibody-mediated destruction.
Thyroidectomy indications and techniques US Medical PG Question 7: A 75-year-old man is referred for thyroidectomy for treatment of thyroid nodules. A portion of the thyroid gland is resected, and the neck is closed with sutures. After awakening from anesthesia, the patient complains of ‘hoarseness’. His vital signs are normal and his incisional pain is minimal. The surgeon realizes he most likely damaged the recurrent laryngeal nerve. Which of the following should the surgeon tell the patient?
- A. "A mistake occurred during the operation, but there was no harm to you."
- B. "We made a mistake during the operation that may have harmed you." (Correct Answer)
- C. "The case took longer than we thought it would, but everything went well."
- D. "A mistake occurred because this hospital has poor operating room protocols."
- E. "The operation was successful and no complications occurred."
Thyroidectomy indications and techniques Explanation: ***\"We made a mistake during the operation that may have harmed you.\"***
- This statement accurately reflects the situation, acknowledging both the **mistake** and the potential **harm** to the patient (hoarseness due to recurrent laryngeal nerve damage).
- Open communication and honesty about medical errors are essential for maintaining **trust** and fulfilling ethical obligations to the patient.
*\"A mistake occurred during the operation, but there was no harm to you.\"*
- This statement is inaccurate because the patient is experiencing **hoarseness**, which is a sign of harm (recurrent laryngeal nerve damage).
- Dismissing the patient's symptom as "no harm" is **dishonest** and undermines trust.
*\"The case took longer than we thought it would, but everything went well.\"*
- This statement is misleading as it downplays a significant complication (recurrent laryngeal nerve damage) by implying that "everything went well" despite the patient's hoarseness.
- It avoids addressing the specific concern and does not acknowledge any **error** or **harm**.
*\"A mistake occurred because this hospital has poor operating room protocols.\"*
- While a mistake may have occurred, blaming the hospital's protocols is an attempt to deflect personal responsibility and can be seen as unprofessional.
- This statement introduces a potentially contentious issue that should be addressed internally rather than with the patient when disclosing the error.
*\"The operation was successful and no complications occurred.\"*
- This statement is explicitly false, as **hoarseness** due to recurrent laryngeal nerve damage is a direct and recognized **complication** of thyroidectomy.
- Making such a claim is unethical and violates the principle of **informed consent** and truthful disclosure.
Thyroidectomy indications and techniques US Medical PG Question 8: An obese 52-year-old man is brought to the emergency department because of increasing shortness of breath for the past 8 hours. Two months ago, he noticed a mass on the right side of his neck and was diagnosed with laryngeal cancer. He has smoked two packs of cigarettes daily for 27 years. He drinks two pints of rum daily. He appears ill. He is oriented to person, place, and time. His temperature is 37°C (98.6°F), pulse is 111/min, respirations are 34/min, and blood pressure is 140/90 mm Hg. Pulse oximetry on room air shows an oxygen saturation of 89%. Examination shows a 9-cm, tender, firm subglottic mass on the right side of the neck. Cervical lymphadenopathy is present. His breathing is labored and he has audible inspiratory stridor but is able to answer questions. The lungs are clear to auscultation. Arterial blood gas analysis on room air shows:
pH 7.36
PCO2 45 mm Hg
PO2 74 mm Hg
HCO3- 25 mEq/L
He has no advanced directive. Which of the following is the most appropriate next step in management?
- A. Comfort care measures
- B. Cricothyroidotomy (Correct Answer)
- C. Tracheostomy
- D. Intramuscular epinephrine
- E. Tracheal stenting
Thyroidectomy indications and techniques Explanation: ***Correct: Cricothyroidotomy***
- This patient has **impending complete airway obstruction** evidenced by inspiratory stridor, severe tachypnea (34/min), hypoxia (O2 sat 89%), and a large obstructing laryngeal mass
- **Cricothyroidotomy** is the emergent surgical airway procedure of choice when there is **imminent or actual complete upper airway obstruction** and endotracheal intubation cannot be safely performed
- The subglottic mass makes endotracheal intubation **extremely dangerous** - instrumentation could precipitate complete obstruction and inability to ventilate
- Cricothyroidotomy provides **immediate airway access** (can be performed in 30-60 seconds) below the level of obstruction, making it life-saving in this emergency
- In the "cannot intubate, cannot ventilate" scenario, cricothyroidotomy is the definitive emergency intervention per ATLS and airway management guidelines
*Incorrect: Tracheostomy*
- While tracheostomy provides definitive airway management, it is a **controlled, elective procedure** typically performed in the OR that takes 20-30 minutes
- This patient requires **immediate airway access** - waiting for OR setup and performing tracheostomy risks complete airway collapse and death
- Tracheostomy may be performed later as a planned procedure once the airway is secured with cricothyroidotomy
- The presence of stridor indicates **critical airway narrowing** requiring emergency intervention, not elective surgery
*Incorrect: Comfort care measures*
- The patient is **alert and oriented** without an advanced directive indicating wishes for comfort care only
- This is an **acute, reversible condition** with appropriate emergency airway intervention
- Presumed consent applies in life-threatening emergencies when the patient cannot formally consent but intervention would be life-saving
- Comfort care would be inappropriate without documented patient wishes or irreversible terminal condition
*Incorrect: Intramuscular epinephrine*
- Epinephrine is indicated for **anaphylaxis** or angioedema causing airway edema from allergic/inflammatory mechanisms
- This patient has **mechanical obstruction** from a solid tumor mass, which will not respond to epinephrine
- Epinephrine causes vasoconstriction and reduces mucosal edema but cannot reduce tumor mass
- Would delay definitive airway management and not address the underlying problem
*Incorrect: Tracheal stenting*
- Tracheal stenting requires **bronchoscopy** in a controlled setting and is used for palliation of tracheal narrowing
- Cannot be performed emergently in an unstable patient with impending airway obstruction
- The obstruction is at the **laryngeal/subglottic level**, not typically amenable to emergency stenting
- Requires time for procedure setup and sedation, which this patient cannot afford given the critical airway emergency
Thyroidectomy indications and techniques US Medical PG Question 9: A 68-year-old man is brought to the emergency department because of fever, progressive weakness, and cough for the past five days. He experienced a similar episode 2 months ago, for which he was hospitalized for 10 days while visiting his son in Russia. He states that he has never fully recovered from that episode. He felt much better after being treated with antibiotics, but he still coughs often during meals. He sometimes also coughs up undigested food after eating. For the last 5 days, his coughing has become more frequent and productive of yellowish-green sputum. He takes hydrochlorothiazide for hypertension and pantoprazole for the retrosternal discomfort that he often experiences while eating. He has smoked half a pack of cigarettes daily for the last 30 years and drinks one shot of vodka every day. The patient appears thin. His temperature is 40.1°C (104.2°F), pulse is 118/min, respirations are 22/min, and blood pressure is 125/90 mm Hg. Auscultation of the lungs shows right basal crackles. There is dullness on percussion at the right lung base. The remainder of the physical examination shows no abnormalities. Laboratory studies show:
Hemoglobin 15.4 g/dL
Leukocyte count 17,000/mm3
Platelet count 350,000/mm3
Na+ 139 mEq/L
K+
4.6 mEq/L
Cl- 102 mEq/L
HCO3- 25 mEq/L
Urea Nitrogen 16 mg/dL
Creatinine 1.3 mg/dL
An x-ray of the chest shows a right lower lobe infiltrate. Which of the following is the most likely explanation for this patient's symptoms?
- A. Weak tone of the lower esophageal sphincter
- B. Unrestricted growth of pneumocytes with invasion of the surrounding tissue
- C. Uncoordinated contractions of the esophagus
- D. Formation of a tissue cavity containing necrotic debris
- E. Outpouching of the hypopharynx (Correct Answer)
Thyroidectomy indications and techniques Explanation: ***Outpouching of the hypopharynx***
- The patient's history of coughing up undigested food and coughing during meals suggests **dysphagia** and potential **aspiration**, which can be caused by a **Zenker's diverticulum** (an outpouching of the hypopharynx).
- This condition creates a pouch that can trap food, leading to regurgitation and repeated aspiration pneumonia, as evidenced by his recurrent pneumonia and current symptoms.
- Zenker's diverticulum is the **underlying explanation** that accounts for *all* of this patient's symptoms: the regurgitation of undigested food, dysphagia, and recurrent aspiration pneumonia.
*Weak tone of the lower esophageal sphincter*
- A weak lower esophageal sphincter (LES) primarily causes **gastroesophageal reflux disease (GERD)**, often associated with heartburn and regurgitation of stomach contents, not undigested food.
- While GERD can cause aspiration, the coughing up of *undigested food* is more indicative of a proximal esophageal issue or pharyngeal problem.
*Unrestricted growth of pneumocytes with invasion of the surrounding tissue*
- This describes **lung cancer**, which can present with cough, weight loss, and recurrent pneumonia due to bronchial obstruction.
- However, the symptom of coughing up *undigested food* is not typical of primary lung malignancy, and the history strongly points to a swallowing disorder.
*Uncoordinated contractions of the esophagus*
- This refers to esophageal motility disorders like **achalasia** or **diffuse esophageal spasm**, which can cause dysphagia and regurgitation.
- While these can lead to aspiration, the specific complaint of coughing up *undigested food* *after eating* is more characteristic of a pharyngeal pouch (Zenker's diverticulum) rather than general esophageal dysmotility.
*Formation of a tissue cavity containing necrotic debris*
- This describes a **lung abscess**, which is a possible *complication* of aspiration pneumonia, accounting for the fever, productive cough, and infiltrate.
- However, the question asks for the **most likely explanation** for this patient's symptoms—a lung abscess is a *sequela* of aspiration, not the *underlying cause* of the repeated aspiration events.
- It does not explain the pathognomonic finding of coughing up undigested food after eating, which points to Zenker's diverticulum as the root cause.
Thyroidectomy indications and techniques US Medical PG Question 10: A 62-year-old man comes to the physician for a follow-up examination after having been diagnosed with stage II adenocarcinoma of the left lower lung lobe without evidence of distant metastases 1 week ago following an evaluation for a chronic cough. He has hypertension and type 2 diabetes mellitus. He has smoked one pack of cigarettes daily for the past 40 years. His current medications include metformin, sitagliptin, and enalapril. He is 177 cm (5 ft 10 in) tall and weighs 65 kg (143 lb); BMI is 20.7 kg/m2. He appears lethargic. Vital signs are within normal limits. Pulse oximetry shows an oxygen saturation of 98%. Examination shows inspiratory wheezing at the left lung base. The remainder of the examination shows no abnormalities. A complete blood count and serum concentrations of electrolytes, creatinine, glucose, and liver enzymes are within the reference range. Spirometry shows an FEV1 of 1.6 L. The diffusing lung capacity for carbon monoxide (DLCO) is 66% of predicted. Which of the following is the most appropriate next step in the management of this patient?
- A. Schedule lobectomy (Correct Answer)
- B. Administer cisplatin and vinorelbine
- C. Schedule a wedge resection
- D. Administer cisplatin and etoposide
- E. Radiation therapy
Thyroidectomy indications and techniques Explanation: ***Schedule lobectomy***
- The patient has **stage II non-small cell lung cancer (adenocarcinoma)** without distant metastases, making surgical resection with **lobectomy** the treatment of choice for curative intent.
- While pulmonary function is somewhat impaired (FEV1 and DLCO), his overall status, age, and normal labs suggest he can likely tolerate the procedure.
*Administer cisplatin and vinorelbine*
- This combination is a common regimen for **adjuvant chemotherapy** following surgical resection in certain stages of NSCLC, or for advanced unresectable disease.
- It is not the primary treatment for a resectable stage II cancer; **surgery is preferred for cure**.
*Schedule a wedge resection*
- A **wedge resection** (sublobar resection) is typically reserved for patients with very small, peripheral tumors or those with severe comorbidities that preclude lobectomy due to poor pulmonary function.
- Given the patient's stage II disease and potentially curative intent, a **lobectomy is generally preferred** for better oncologic outcomes.
*Administer cisplatin and etoposide*
- This chemotherapy regimen is more commonly used for **small cell lung cancer (SCLC)** or for some advanced NSCLC cases, not typically for resectable stage II adenocarcinoma as a primary treatment.
- Even if used in NSCLC, it would usually be in the context of advanced disease or as part of a neoadjuvant/adjuvant approach with surgery, not as a standalone initial treatment for resectable disease.
*Radiation therapy*
- **Radiation therapy** is often used for inoperable tumors, for patients who refuse surgery, or as an adjuvant treatment.
- For a resectable stage II NSCLC, **surgery offers the best chance for cure**, making radiation therapy alone less appropriate as the first-line definitive treatment strategy.
More Thyroidectomy indications and techniques US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.