Thyroid nodule evaluation US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Thyroid nodule evaluation. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Thyroid nodule evaluation US Medical PG Question 1: A 36-year-old woman comes to the physician for a follow-up visit after she had a PET scan that showed a nodule on the thyroid gland. She has no difficulty or pain while swallowing. She was treated for non-Hodgkin lymphoma at the age of 28 years, which included external beam radiation to the head and neck and 4 cycles of chemotherapy. She appears healthy. Vital signs are within normal limits. Physical examination shows no abnormalities. Serum studies show:
Glucose 82 mg/dL
Creatinine 0.7 mg/dL
Thyroid-stimulating hormone 3 μU/mL
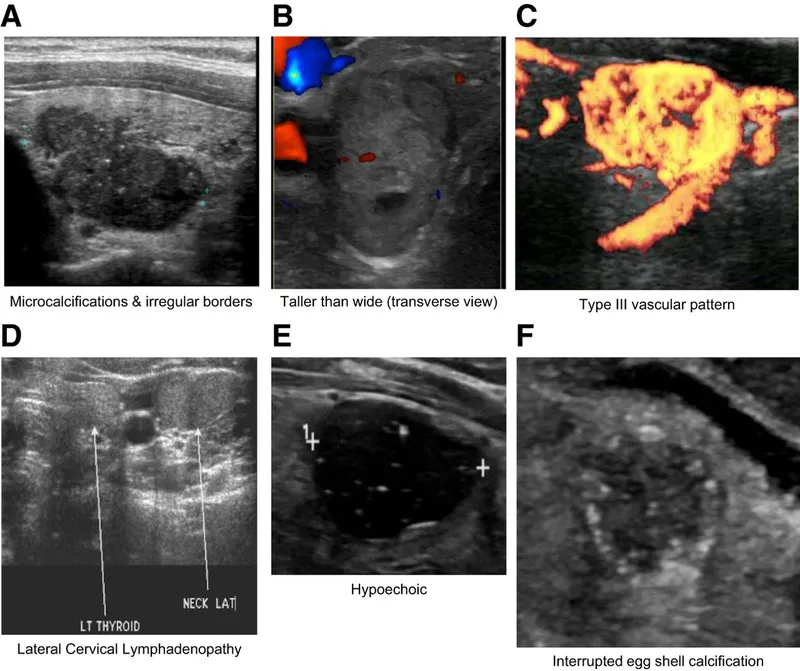
Ultrasound of the neck shows a 1.2-cm (0.5-in) nodule on the left lobe of the thyroid with irregular margins and microcalcifications. A fine-needle aspiration biopsy shows Psammoma bodies and cells with clear, ground-glass, empty nuclei. Which of the following is the most appropriate next step in management?
- A. Thyroid scintigraphy
- B. Observation and follow-up in 3 months
- C. Radioiodine therapy
- D. Total thyroidectomy (Correct Answer)
Thyroid nodule evaluation Explanation: ***Total thyroidectomy***
- The fine-needle aspiration biopsy findings of **Psammoma bodies** and **clear, ground-glass, empty nuclei** are classic for **papillary thyroid carcinoma**, which is the most common type of thyroid cancer.
- Given the patient's history of **neck radiation** for lymphoma (a risk factor for thyroid cancer), the concerning ultrasound features (irregular margins, microcalcifications), and the confirmed diagnosis of papillary thyroid carcinoma, **total thyroidectomy** is the definitive treatment.
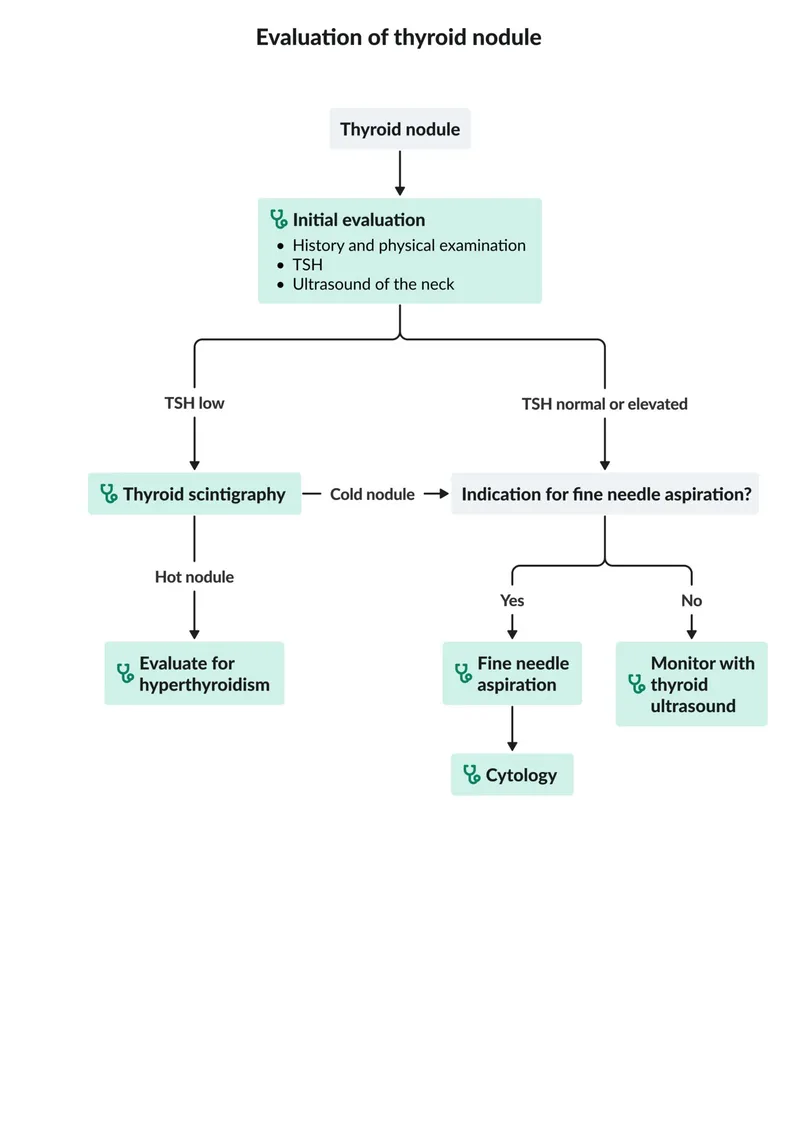
*Thyroid scintigraphy*
- **Thyroid scintigraphy** is primarily used to assess the functional status of thyroid nodules (hot vs. cold) and is helpful if the TSH is suppressed or if the FNA is indeterminate.
- In this case, the **fine-needle aspiration (FNA) biopsy** has already provided a definitive diagnosis of papillary thyroid cancer, making scintigraphy unnecessary for initial management.
*Observation and follow-up in 3 months*
- **Observation** is not appropriate given the definitive diagnosis of **papillary thyroid carcinoma** confirmed by biopsy and the patient's history of neck radiation.
- Papillary thyroid cancer, although often slow-growing, requires active management, especially with adverse features on ultrasound and a clear diagnosis.
*Radioiodine therapy*
- **Radioiodine therapy** is typically used as **adjuvant treatment** *after* thyroidectomy to ablate residual thyroid tissue or treat metastatic disease, particularly in higher-risk cases.
- It is not the primary treatment for localized papillary thyroid carcinoma.
Thyroid nodule evaluation US Medical PG Question 2: A 27-year-old man comes to the physician because of worsening abdominal pain over the last several months. He has also had recent feelings of sadness and a lack of motivation at work, where he is employed as a computer programmer. He denies suicidal thoughts. He has a history of multiple kidney stones. He has a family history of thyroid cancer in his father and uncle, who both underwent thyroidectomy before age 30. His temperature is 37°C (98°F), blood pressure is 138/86 mm Hg, and pulse is 87/min. Physical examination shows diffuse tenderness over the abdomen and obesity but is otherwise unremarkable. Serum studies show:
Na+ 141 mEq/L
K+ 3.6 mEq/L
Glucose 144 mg/dL
Ca2+ 12.1 mg/dL
Albumin 4.1 g/dL
PTH 226 pg/mL (normal range 12–88 pg/mL)
Results of a RET gene test return abnormal. The physician refers him to an endocrine surgeon. Which of the following is the most appropriate next step in diagnosis?
- A. Thyroidectomy
- B. Urine 5-HIAA
- C. Urine metanephrines (Correct Answer)
- D. Midnight salivary cortisol
- E. Serum gastrin
Thyroid nodule evaluation Explanation: ***Urine metanephrines***
- The patient's presentation, including **abdominal pain**, **constipation** (implied by pain, mood changes, and high calcium), **hypertension**, **hypercalcemia** with **elevated PTH**, and a family history of **thyroid cancer** with an **abnormal RET gene test**, is highly suggestive of **MEN 2A** (Multiple Endocrine Neoplasia type 2A).
- **MEN 2A** is characterized by **medullary thyroid carcinoma** (MTC), **pheochromocytoma**, and **primary hyperparathyroidism**. Given the strong suspicion of MEN 2A and the presence of hypertension, screening for **pheochromocytoma** with **urine metanephrines** is crucial before any surgical intervention (e.g., thyroidectomy) due to the risk of a hypertensive crisis.
*Thyroidectomy*
- While a **thyroidectomy** is indicated for **medullary thyroid carcinoma** (strongly suggested by the family history of thyroid cancer and abnormal RET gene), it should **not be the immediate next step** before ruling out **pheochromocytoma**.
- Performing a thyroidectomy in a patient with an undiagnosed pheochromocytoma can lead to a **life-threatening hypertensive crisis** during surgery.
*Urine 5-HIAA*
- **Urine 5-HIAA** (5-hydroxyindoleacetic acid) is a test for **carcinoid syndrome**, which presents with flushing, diarrhea, and bronchospasm.
- These symptoms are **not consistent** with the patient's presentation, and carcinoid syndrome is **not a component of MEN 2A**.
*Midnight salivary cortisol*
- **Midnight salivary cortisol** is used to screen for **Cushing's syndrome**, which is characterized by symptoms such as central obesity, moon facies, striae, and muscle weakness.
- While the patient is obese, his other symptoms and laboratory findings are **not suggestive of Cushing's syndrome**, and it is not typically associated with MEN 2A.
*Serum gastrin*
- **Serum gastrin** levels are measured to diagnose **Zollinger-Ellison syndrome**, characterized by severe peptic ulcer disease and diarrhea due to a gastrinoma.
- While gastrinomas can occur in **MEN 1**, they are **not a feature of MEN 2A**, and the patient's symptoms are more consistent with other endocrine dysfunctions.
Thyroid nodule evaluation US Medical PG Question 3: A 65-year-old man with a 40-pack-year smoking history presents with hemoptysis and a persistent cough. Chest CT shows a 3.5 cm centrally located mass in the right main bronchus. Positron emission tomography confirms a malignant nodule. Bronchoscopy with transbronchial biopsy is performed and a specimen sample of the nodule is sent for frozen section analysis. The tissue sample is most likely to show which of the following tumor types?
- A. Carcinoid tumor
- B. Metastasis of colorectal cancer
- C. Small cell lung carcinoma
- D. Large cell carcinoma
- E. Squamous cell carcinoma (Correct Answer)
Thyroid nodule evaluation Explanation: ***Squamous cell carcinoma***
- This is the most likely diagnosis given the **central location** in the main bronchus, **heavy smoking history**, and presentation with **hemoptysis**.
- **Squamous cell carcinoma** accounts for 25-30% of lung cancers and characteristically arises in **central/proximal airways**, making it readily accessible by **bronchoscopy**.
- Histologically, it shows **keratin pearls** and **intercellular bridges** on biopsy.
- The **central endobronchial location** and ability to obtain tissue via transbronchial biopsy strongly favor squamous cell over peripheral tumors.
*Carcinoid tumor*
- **Carcinoid tumors** are **neuroendocrine tumors** that can present as central endobronchial masses and cause hemoptysis.
- However, they are typically **slow-growing** with more indolent presentation, and PET scans show **variable uptake** (often less intense than aggressive carcinomas).
- They represent only **1-2% of lung tumors** and occur more commonly in **younger, non-smoking patients**.
*Metastasis of colorectal cancer*
- While lung is a common site for **colorectal metastases**, these typically present as **multiple peripheral nodules** rather than a solitary central endobronchial mass.
- The clinical presentation strongly suggests **primary lung cancer** rather than metastatic disease.
- Without history of colorectal cancer, this is unlikely.
*Small cell lung carcinoma*
- **Small cell lung carcinoma** (SCLC) represents 15% of lung cancers and typically presents as a **large central mass** with early mediastinal involvement.
- However, SCLC is usually **too extensive at presentation** for transbronchial biopsy alone and often requires mediastinoscopy or CT-guided biopsy.
- Histology shows **small cells with scant cytoplasm**, **salt-and-pepper chromatin**, and **oat-cell morphology**.
- While possible, the single accessible endobronchial mass is more characteristic of squamous cell.
*Large cell carcinoma*
- **Large cell carcinoma** is a **diagnosis of exclusion** made when tumors lack features of adenocarcinoma, squamous cell, or small cell differentiation.
- It typically presents as **large peripheral masses** rather than central endobronchial lesions.
- It represents only **10% of lung cancers** and is less common than squamous cell carcinoma in this clinical scenario.
Thyroid nodule evaluation US Medical PG Question 4: A 47-year-old woman presents to the clinic complaining of difficulty swallowing that started 1 month ago. The patient also reports a weight loss of 10 lbs during this time, without a change in her appetite. She denies fatigue, cough, hoarseness, pain, or hemoptysis. The patient has a history of childhood lymphoma, which was treated with radiation. She takes no medications. She has smoked 1 pack of cigarettes per day since she was 25 years old. Her physical exam is notable for a palpable nodule on the right side of the thyroid. An ultrasound is performed, which confirms a 1.2 cm hyperechoic nodule in the right lobe. Thyroid function labs are drawn and shown below:
Serum TSH: 0.2 mU/L
Serum thyroxine (T4): 187 nmol/L
Serum triiodothyronine (T3): 3.3 nmol/L
Which of the following is the next best step in management?
- A. Radioactive iodine
- B. Partial thyroidectomy
- C. Fine needle aspiration (Correct Answer)
- D. Levothyroxine
- E. Thyroid scintigraphy
Thyroid nodule evaluation Explanation: ***Fine needle aspiration***
- This patient has several risk factors for **thyroid malignancy**, including a history of **radiation exposure** to the neck (for childhood lymphoma) and a palpable thyroid nodule associated with **dysphagia** and unexplained **weight loss**. Fine needle aspiration (FNA) is the best next step to evaluate for malignancy.
- The patient also presents with **hyperthyroidism** (low TSH, elevated T4), but the primary concern given the clinical picture is to rule out thyroid cancer.
- Per American Thyroid Association guidelines, FNA is indicated for any nodule in a patient with a history of head/neck radiation exposure.
*Radioactive iodine*
- Radioactive iodine ablation is used to treat **hyperthyroidism**, especially in cases of **Graves' disease** or toxic nodular goiter. While the patient has hyperthyroidism, the presence of a suspicious nodule warrants investigation for malignancy first.
- Administering radioactive iodine without first ruling out malignancy in a suspicious nodule could delay definitive treatment for cancer or complicate its management.
*Partial thyroidectomy*
- **Partial thyroidectomy** would be considered if the FNA results indicate malignancy or a highly suspicious follicular neoplasm.
- Performing surgery without a prior FNA would be premature, as many thyroid nodules are benign and do not require surgical intervention unless causing compressive symptoms or confirmed malignancy.
*Levothyroxine*
- **Levothyroxine** is used to treat **hypothyroidism** or to suppress TSH in cases of benign thyroid nodules or after thyroid cancer surgery.
- This patient is **hyperthyroid**, making exogenous levothyroxine inappropriate.
*Thyroid scintigraphy*
- **Thyroid scintigraphy** (radioactive iodine uptake scan) is useful in characterizing thyroid nodules as "hot" (functioning) or "cold" (non-functioning) in the context of hyperthyroidism.
- "Hot" nodules are rarely malignant, while "cold" nodules have a higher (though still relatively low) risk of malignancy. However, given the patient's strong risk factors for thyroid cancer and compressive symptoms, an FNA is more direct and informative for assessing malignancy than scintigraphy at this stage.
Thyroid nodule evaluation US Medical PG Question 5: A 75-year-old woman comes to the physician because of a 3-month history of involuntary weight loss and a painless lump on her neck. Physical examination shows a firm, irregular swelling on the right side of the neck. Ultrasonography of the thyroid gland shows a 2-cm nodule with irregular margins and microcalcifications in the right thyroid lobe. A biopsy of the thyroid nodule is performed. Which of the following changes would be most consistent with anaplasia?
- A. Negative staining of tumor cells for thyroglobulin (Correct Answer)
- B. Disorganized proliferation of mature thyroid cells
- C. Increased expression of thyroid transcription factor-1
- D. Replacement of thyroid cells by normal squamous epithelium
- E. Reduced number of functional thyroid cells
Thyroid nodule evaluation Explanation: ***Negative staining of tumor cells for thyroglobulin***
- Anaplastic thyroid carcinoma is characterized by extreme **dedifferentiation**, losing most of the features of normal thyroid cells, including the ability to produce **thyroglobulin**.
- Therefore, **negative or weak staining for thyroglobulin** (a marker of thyroid differentiation) in a highly malignant thyroid tumor is consistent with anaplasia.
*Disorganized proliferation of mature thyroid cells*
- This description is more consistent with a **benign tumor** or hyperplastic nodule where cells retain their mature characteristics but grow abnormally.
- In contrast, anaplastic carcinomas involve highly **undifferentiated cells** that bear little resemblance to mature thyroid cells.
*Increased expression of thyroid transcription factor-1*
- **Thyroid transcription factor-1 (TTF-1)** is a nuclear protein expressed in various thyroid neoplasms, including well-differentiated carcinomas.
- While TTF-1 expression can occur in anaplastic carcinoma, it is usually **lost or significantly reduced** due to dedifferentiation, making increased expression inconsistent with anaplasia.
*Replacement of thyroid cells by normal squamous epithelium*
- This describes **squamous metaplasia**, a common finding in chronic inflammation or conditions like Hashimoto's thyroiditis, but it isn't anaplasia.
- Anaplastic carcinoma involves **malignant transformation** of thyroid cells into highly pleomorphic, undifferentiated cells, not replacement by normal non-thyroid cells.
*Reduced number of functional thyroid cells*
- While anaplastic carcinomas replace normal thyroid tissue, leading to a reduced number of functional cells, this is a **consequence** of the disease, not a defining characteristic of anaplasia itself.
- Anaplasia refers to the **histological appearance** of highly undifferentiated, malignant cells, rather than simply a reduction in functional cell count.
Thyroid nodule evaluation US Medical PG Question 6: A 45-year-old man comes to the physician for the evaluation of difficulty swallowing that has worsened over the past year. He also reports some hoarseness and generalized bone, muscle, and joint pain. During the past six months, he has had progressive constipation and two episodes of kidney stones. He also reports recurrent episodes of throbbing headaches, diaphoresis, and palpitations. He does not smoke or drink alcohol. He takes no medications. His vital signs are within normal limits. Physical examination and an ECG show no abnormalities. Laboratory studies show calcium concentration of 12 mg/dL, phosphorus concentration of 2 mg/dL, alkaline phosphatase concentration of 100 U/L, and calcitonin concentration of 11 pg/mL (N < 8.8). Ultrasonography of the neck shows hypoechoic thyroid lesions with irregular margins and microcalcifications. Which of the following is the most likely underlying cause of this patient's condition?
- A. Altered RET proto-oncogene expression (Correct Answer)
- B. Deleted VHL gene
- C. Disrupted menin protein function
- D. Exposure to ionizing radiation
- E. Mutated NF1 gene
Thyroid nodule evaluation Explanation: ***Altered RET proto-oncogene expression***
- This patient's symptoms are highly suggestive of **multiple endocrine neoplasia type 2A (MEN2A)**, which is caused by gain-of-function mutations in the **RET proto-oncogene**.
- **MEN2A** typically presents with **medullary thyroid carcinoma** (hypoechoic thyroid lesions, elevated calcitonin), **pheochromocytoma** (throbbing headaches, diaphoresis, palpitations), and **primary hyperparathyroidism** (hypercalcemia, hypophosphatemia, bone/muscle/joint pain, kidney stones).
*Deleted VHL gene*
- A deleted **VHL gene** is associated with **Von Hippel-Lindau disease**, characterized by **retinal and cerebellar hemangioblastomas**, **renal cell carcinoma**, and **pheochromocytoma**.
- While pheochromocytoma is present, the thyroid and parathyroid findings are not consistent with VHL disease.
*Disrupted menin protein function*
- Disrupted **menin protein function** is characteristic of **multiple endocrine neoplasia type 1 (MEN1)**, which includes **pituitary tumors**, **parathyroid adenomas** (leading to hyperparathyroidism), and **pancreatic endocrine tumors**.
- Although primary hyperparathyroidism is present, the thyroid carcinoma is medullary (not follicular/papillary) and the specific symptoms point more toward MEN2A.
*Exposure to ionizing radiation*
- Exposure to **ionizing radiation** is a risk factor for **papillary and follicular thyroid carcinomas**, but not typically **medullary thyroid carcinoma**.
- It also does not explain the concurrent **pheochromocytoma** and **hyperparathyroidism**.
*Mutated NF1 gene*
- A mutated **NF1 gene** is responsible for **neurofibromatosis type 1**, which manifests with **café-au-lait spots**, **neurofibromas**, **optic gliomas**, and sometimes **pheochromocytoma**.
- There are no cutaneous or neurological findings of neurofibromatosis in this patient, and the prominent medullary thyroid carcinoma and hyperparathyroidism are not features of NF1.
Thyroid nodule evaluation US Medical PG Question 7: A 27-year-old woman comes to the physician for a routine health maintenance examination. She feels well. She had a chlamydia infection at the age of 22 years that was treated. Her only medication is an oral contraceptive. She has smoked one pack of cigarettes daily for 6 years. She has recently been sexually active with 3 male partners and uses condoms inconsistently. Her last Pap test was 4 years ago and results were normal. Physical examination shows no abnormalities. A Pap test shows atypical squamous cells of undetermined significance. Which of the following is the most appropriate next step in management?
- A. Repeat cytology in 6 months
- B. Perform laser ablation
- C. Perform loop electrosurgical excision procedure
- D. Perform HPV testing (Correct Answer)
- E. Perform cervical biopsy
Thyroid nodule evaluation Explanation: ***Perform HPV testing***
- For women aged 25-29 with **Atypical Squamous Cells of Undetermined Significance (ASC-US)**, **HPV co-testing** is the preferred next step to risk-stratify for high-grade lesions.
- If **HPV is positive**, the patient should proceed to **colposcopy**; if HPV is negative, she can return to routine screening.
*Repeat cytology in 6 months*
- This approach is typically recommended for adolescents (age <21) with ASC-US or for women aged 21-24 where HPV testing is often not performed due to the high rate of transient HPV infections.
- For women aged ≥25 years with ASC-US, **reflex HPV testing** or **HPV co-testing** (if not done with the initial Pap) is generally preferred over repeat cytology alone.
*Perform laser ablation*
- **Laser ablation** is a treatment for **high-grade cervical intraepithelial neoplasia (CIN2/3)** identified after colposcopy and biopsy, not for initial ASC-US findings.
- Initiating a destructive procedure without further diagnostic evaluation would be premature and over-treatment for ASC-US.
*Perform loop electrosurgical excision procedure*
- **LEEP (loop electrosurgical excision procedure)** is a **diagnostic and therapeutic procedure** typically reserved for confirmed **high-grade CIN (CIN2 or CIN3)** or adenocarcinoma in situ.
- It is an invasive procedure and not appropriate as the initial management step for an ASC-US Pap result.
*Perform cervical biopsy*
- A **cervical biopsy** is performed during a **colposcopy** if abnormal areas are identified, usually following a positive HPV test or higher-grade abnormal cytology (e.g., LSIL, HSIL).
- ASC-US alone does not automatically warrant an immediate colposcopy and biopsy without prior **HPV risk stratification**.
Thyroid nodule evaluation US Medical PG Question 8: A 62-year-old man comes to the physician for a follow-up examination after having been diagnosed with stage II adenocarcinoma of the left lower lung lobe without evidence of distant metastases 1 week ago following an evaluation for a chronic cough. He has hypertension and type 2 diabetes mellitus. He has smoked one pack of cigarettes daily for the past 40 years. His current medications include metformin, sitagliptin, and enalapril. He is 177 cm (5 ft 10 in) tall and weighs 65 kg (143 lb); BMI is 20.7 kg/m2. He appears lethargic. Vital signs are within normal limits. Pulse oximetry shows an oxygen saturation of 98%. Examination shows inspiratory wheezing at the left lung base. The remainder of the examination shows no abnormalities. A complete blood count and serum concentrations of electrolytes, creatinine, glucose, and liver enzymes are within the reference range. Spirometry shows an FEV1 of 1.6 L. The diffusing lung capacity for carbon monoxide (DLCO) is 66% of predicted. Which of the following is the most appropriate next step in the management of this patient?
- A. Schedule lobectomy (Correct Answer)
- B. Administer cisplatin and vinorelbine
- C. Schedule a wedge resection
- D. Administer cisplatin and etoposide
- E. Radiation therapy
Thyroid nodule evaluation Explanation: ***Schedule lobectomy***
- The patient has **stage II non-small cell lung cancer (adenocarcinoma)** without distant metastases, making surgical resection with **lobectomy** the treatment of choice for curative intent.
- While pulmonary function is somewhat impaired (FEV1 and DLCO), his overall status, age, and normal labs suggest he can likely tolerate the procedure.
*Administer cisplatin and vinorelbine*
- This combination is a common regimen for **adjuvant chemotherapy** following surgical resection in certain stages of NSCLC, or for advanced unresectable disease.
- It is not the primary treatment for a resectable stage II cancer; **surgery is preferred for cure**.
*Schedule a wedge resection*
- A **wedge resection** (sublobar resection) is typically reserved for patients with very small, peripheral tumors or those with severe comorbidities that preclude lobectomy due to poor pulmonary function.
- Given the patient's stage II disease and potentially curative intent, a **lobectomy is generally preferred** for better oncologic outcomes.
*Administer cisplatin and etoposide*
- This chemotherapy regimen is more commonly used for **small cell lung cancer (SCLC)** or for some advanced NSCLC cases, not typically for resectable stage II adenocarcinoma as a primary treatment.
- Even if used in NSCLC, it would usually be in the context of advanced disease or as part of a neoadjuvant/adjuvant approach with surgery, not as a standalone initial treatment for resectable disease.
*Radiation therapy*
- **Radiation therapy** is often used for inoperable tumors, for patients who refuse surgery, or as an adjuvant treatment.
- For a resectable stage II NSCLC, **surgery offers the best chance for cure**, making radiation therapy alone less appropriate as the first-line definitive treatment strategy.
Thyroid nodule evaluation US Medical PG Question 9: A 68-year-old man is brought to the emergency department because of fever, progressive weakness, and cough for the past five days. He experienced a similar episode 2 months ago, for which he was hospitalized for 10 days while visiting his son in Russia. He states that he has never fully recovered from that episode. He felt much better after being treated with antibiotics, but he still coughs often during meals. He sometimes also coughs up undigested food after eating. For the last 5 days, his coughing has become more frequent and productive of yellowish-green sputum. He takes hydrochlorothiazide for hypertension and pantoprazole for the retrosternal discomfort that he often experiences while eating. He has smoked half a pack of cigarettes daily for the last 30 years and drinks one shot of vodka every day. The patient appears thin. His temperature is 40.1°C (104.2°F), pulse is 118/min, respirations are 22/min, and blood pressure is 125/90 mm Hg. Auscultation of the lungs shows right basal crackles. There is dullness on percussion at the right lung base. The remainder of the physical examination shows no abnormalities. Laboratory studies show:
Hemoglobin 15.4 g/dL
Leukocyte count 17,000/mm3
Platelet count 350,000/mm3
Na+ 139 mEq/L
K+
4.6 mEq/L
Cl- 102 mEq/L
HCO3- 25 mEq/L
Urea Nitrogen 16 mg/dL
Creatinine 1.3 mg/dL
An x-ray of the chest shows a right lower lobe infiltrate. Which of the following is the most likely explanation for this patient's symptoms?
- A. Weak tone of the lower esophageal sphincter
- B. Unrestricted growth of pneumocytes with invasion of the surrounding tissue
- C. Uncoordinated contractions of the esophagus
- D. Formation of a tissue cavity containing necrotic debris
- E. Outpouching of the hypopharynx (Correct Answer)
Thyroid nodule evaluation Explanation: ***Outpouching of the hypopharynx***
- The patient's history of coughing up undigested food and coughing during meals suggests **dysphagia** and potential **aspiration**, which can be caused by a **Zenker's diverticulum** (an outpouching of the hypopharynx).
- This condition creates a pouch that can trap food, leading to regurgitation and repeated aspiration pneumonia, as evidenced by his recurrent pneumonia and current symptoms.
- Zenker's diverticulum is the **underlying explanation** that accounts for *all* of this patient's symptoms: the regurgitation of undigested food, dysphagia, and recurrent aspiration pneumonia.
*Weak tone of the lower esophageal sphincter*
- A weak lower esophageal sphincter (LES) primarily causes **gastroesophageal reflux disease (GERD)**, often associated with heartburn and regurgitation of stomach contents, not undigested food.
- While GERD can cause aspiration, the coughing up of *undigested food* is more indicative of a proximal esophageal issue or pharyngeal problem.
*Unrestricted growth of pneumocytes with invasion of the surrounding tissue*
- This describes **lung cancer**, which can present with cough, weight loss, and recurrent pneumonia due to bronchial obstruction.
- However, the symptom of coughing up *undigested food* is not typical of primary lung malignancy, and the history strongly points to a swallowing disorder.
*Uncoordinated contractions of the esophagus*
- This refers to esophageal motility disorders like **achalasia** or **diffuse esophageal spasm**, which can cause dysphagia and regurgitation.
- While these can lead to aspiration, the specific complaint of coughing up *undigested food* *after eating* is more characteristic of a pharyngeal pouch (Zenker's diverticulum) rather than general esophageal dysmotility.
*Formation of a tissue cavity containing necrotic debris*
- This describes a **lung abscess**, which is a possible *complication* of aspiration pneumonia, accounting for the fever, productive cough, and infiltrate.
- However, the question asks for the **most likely explanation** for this patient's symptoms—a lung abscess is a *sequela* of aspiration, not the *underlying cause* of the repeated aspiration events.
- It does not explain the pathognomonic finding of coughing up undigested food after eating, which points to Zenker's diverticulum as the root cause.
Thyroid nodule evaluation US Medical PG Question 10: A 68-year-old man comes to the physician because of a 6-month history of difficulty swallowing pieces of meat and choking frequently during meal times. He also sometimes regurgitates foul-smelling, undigested food particles. Examination shows a 3 x 3 cm soft cystic, immobile mass in the upper third of the left side of his neck anterior to the left sternocleidomastoid muscle that becomes prominent when he coughs. A barium swallow shows an accumulation of contrast on the lateral aspect of the neck at the C5 level. Which of the following is the most likely underlying cause for this patient's condition?
- A. Remnant of the embryological omphalomesenteric duct
- B. Inadequate relaxation of lower esophageal sphincter
- C. Remnant of the thyroglossal duct
- D. Increased intrapharyngeal pressure (Correct Answer)
- E. Remnant of the second branchial cleft
Thyroid nodule evaluation Explanation: ***Increased intrapharyngeal pressure***
- The symptoms of **dysphagia**, **regurgitation of undigested food**, and a **neck mass prominent with coughing** are classic for a **Zenker's diverticulum**, which results from increased intrapharyngeal pressure causing herniation of mucosa through Killian's triangle.
- The barium swallow showing **contrast accumulation** and the location of the mass further support this diagnosis, as Zenker's diverticula are pseudo-diverticula caused by pulsion from high pressure during swallowing.
*Remnant of the embryological omphalomesenteric duct*
- An **omphalomesenteric duct remnant** typically presents as a **Meckel's diverticulum** in the small intestine or an umbilical fistula, not as a neck mass with swallowing difficulties.
- This embryological anomaly is related to the midgut development and has no connection to pharyngeal issues.
*Inadequate relaxation of lower esophageal sphincter*
- **Inadequate relaxation of the lower esophageal sphincter** (LES) is characteristic of **achalasia**, which causes dysphagia and regurgitation, but typically of *fermented* rather than *undigested* food, and does not present with a palpable neck mass as described.
- Achalasia involves the distal esophagus and does not lead to a pharyngeal outpouching.
*Remnant of the thyroglossal duct*
- A **thyroglossal duct cyst** is a midline neck mass that moves with swallowing and tongue protrusion, which is not consistent with the lateral, pulsion-type mass that becomes prominent with coughing.
- While it can be found in the upper third of the neck, its embryological origin and presentation differ significantly from a Zenker's diverticulum.
*Remnant of the second branchial cleft*
- A **second branchial cleft cyst** is typically a lateral neck mass, often located anterior to the sternocleidomastoid muscle, but it is congenital and does not typically present with progressive dysphagia and regurgitation of undigested food in adulthood, nor does it typically become prominent with coughing due to increased intrapharyngeal pressure.
- These cysts are usually asymptomatic unless infected and are not directly related to swallowing mechanics.
More Thyroid nodule evaluation US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.