Recurrent laryngeal nerve protection US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Recurrent laryngeal nerve protection. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
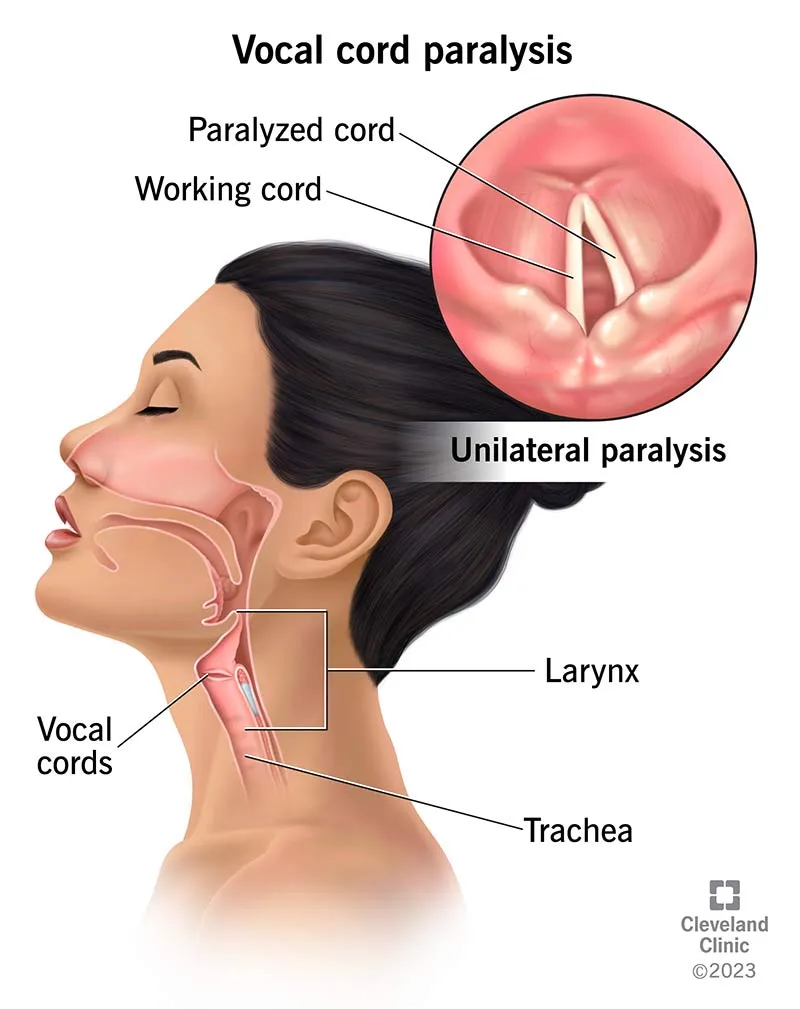
Recurrent laryngeal nerve protection US Medical PG Question 1: A 45-year-old male patient presents with difficulty swallowing and hoarseness that has progressively worsened over the past month. During physical examination, the physician notices that the patient's left vocal cord is paralyzed. The paralysis is most likely due to compression of which of the following nerves?
- A. Left superior laryngeal nerve
- B. Left vagus nerve
- C. Right recurrent laryngeal nerve
- D. Left recurrent laryngeal nerve (Correct Answer)
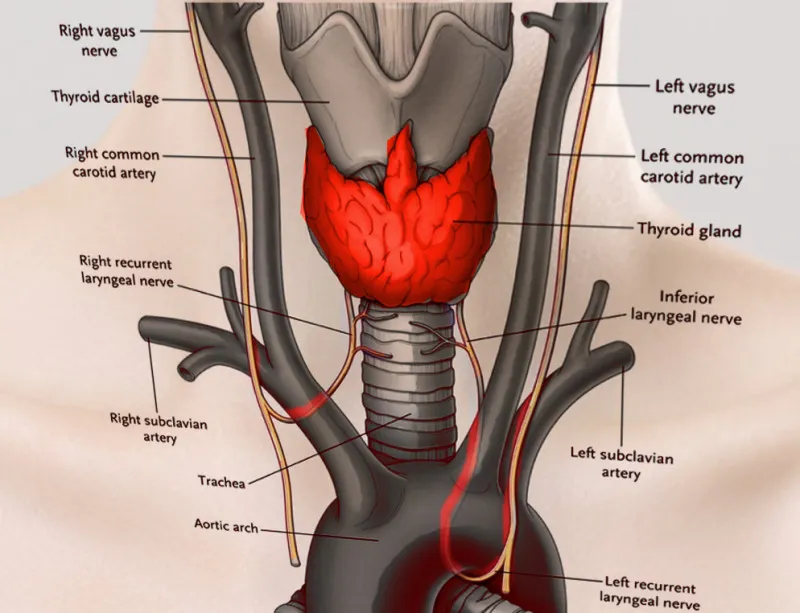
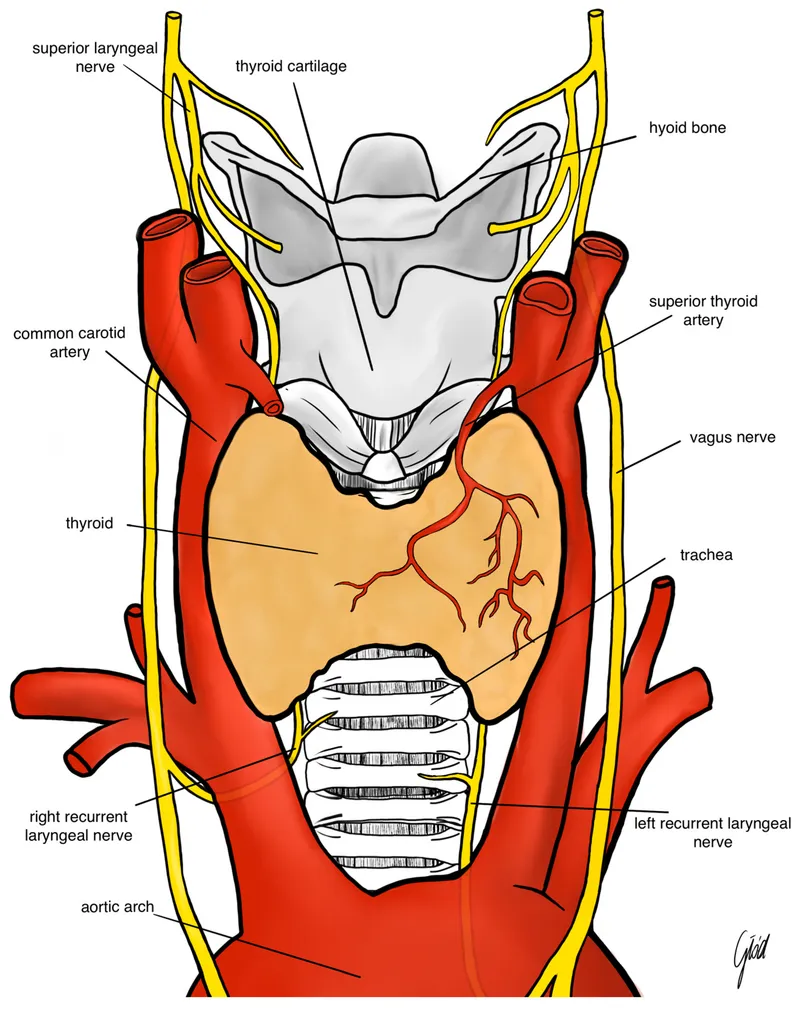
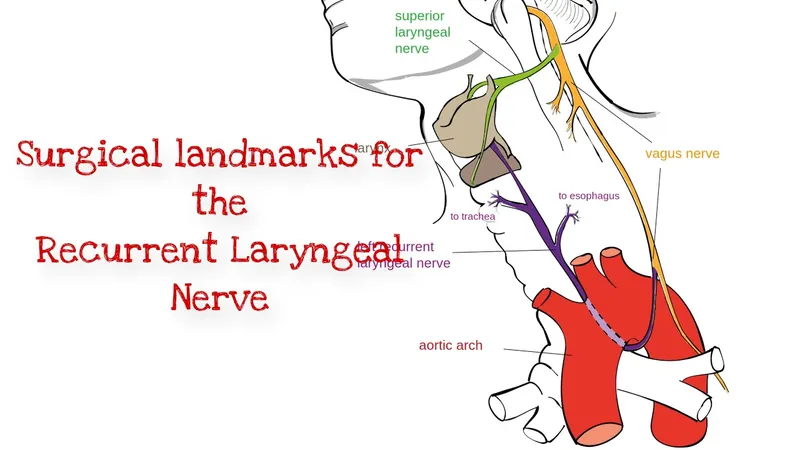
Recurrent laryngeal nerve protection Explanation: ***Left recurrent laryngeal nerve***
- The **left recurrent laryngeal nerve** innervates all intrinsic muscles of the left larynx, except the cricothyroid muscle [1].
- Damage or compression of this nerve leads to **left vocal cord paralysis** and associated symptoms like hoarseness and difficulty swallowing (dysphagia).
*Left superior laryngeal nerve*
- The **superior laryngeal nerve** innervates the cricothyroid muscle, which is responsible for tensing the vocal cords.
- Damage to this nerve primarily affects **pitch control** and would not typically cause complete vocal cord paralysis.
*Left vagus nerve*
- The **vagus nerve** gives rise to both the superior and recurrent laryngeal nerves [1].
- While damage to the main vagus nerve would cause vocal cord paralysis, the more specific finding of isolated vocal cord paralysis points to an issue with its branch, the recurrent laryngeal nerve [1].
*Right recurrent laryngeal nerve*
- The **right recurrent laryngeal nerve** controls the intrinsic muscles of the right larynx.
- Damage to this nerve would result in **right vocal cord paralysis**, not left vocal cord paralysis as described in the patient.
Recurrent laryngeal nerve protection US Medical PG Question 2: A 3-year-old girl is brought to the physician by her parents because of a barking cough, a raspy voice, and noisy breathing for the last 3 days. Five days ago, she had a low-grade fever and runny nose. She attends daycare. Her immunizations are up-to-date. Her temperature is 37.8°C (100°F) and respirations are 33/min. Physical examination shows supraclavicular retractions. There is a high-pitched sound present on inspiration. Examination of the throat shows erythema without exudates. Which of the following is the most likely location of the anatomic narrowing causing this patient's symptoms?
- A. Bronchioles
- B. Pharynx
- C. Subglottic larynx (Correct Answer)
- D. Distal trachea
- E. Epiglottis
Recurrent laryngeal nerve protection Explanation: ***Subglottic larynx***
- The patient's symptoms of **barking cough**, **raspy voice**, **stridor** (high-pitched inspiratory sound), and **supraclavicular retractions** are classic for **croup** (laryngotracheobronchitis), which is caused by inflammation and narrowing of the subglottic region of the larynx.
- The preceding low-grade fever and runny nose are typical of a viral upper respiratory infection, which commonly precedes croup.
*Bronchioles*
- Narrowing in the bronchioles typically causes **wheezing** (a high-pitched whistling sound on expiration) and **respiratory distress**, often seen in conditions like **bronchiolitis** or **asthma**.
- A barking cough and raspy voice are not characteristic symptoms of bronchiolar obstruction.
*Pharynx*
- Inflammation and narrowing of the pharynx primarily cause **sore throat**, **difficulty swallowing** (dysphagia), and sometimes **muffled voice**.
- It would not typically lead to a barking cough, stridor, or severe inspiratory distress.
*Distal trachea*
- While tracheal narrowing can cause stridor, the classic **barking cough** and **hoarseness** (raspy voice) are more specifically localized to the laryngeal area.
- Obstruction in the distal trachea would be less likely to affect voice quality as significantly as subglottic narrowing.
*Epiglottis*
- **Epiglottitis** presents as a rapidly progressive, life-threatening condition with **high fever**, **dysphagia**, **drooling**, and a **muffled "hot potato" voice**.
- The patient would typically appear toxic and prefer to sit in the **tripod position**, which is not described in this case, and her symptoms are less acute.
Recurrent laryngeal nerve protection US Medical PG Question 3: A 10-month-old boy is brought to the clinic with a history of recurrent episodes of stridor and wheezing. His mother reports that his wheezing is exacerbated by crying, feeding, and flexion of the neck, and is relieved by extension of the neck. Occasionally he vomits after feeding. What is the most likely diagnosis?
- A. Laryngomalacia
- B. Congenital subglottic stenosis
- C. Gastroesophageal reflux disease
- D. Double aortic arch (Correct Answer)
- E. Recurrent viral wheeze
Recurrent laryngeal nerve protection Explanation: ***Double aortic arch***
- A **double aortic arch** forms a complete vascular ring around the trachea and esophagus, causing symptoms that worsen with feeding and neck flexion due to increased pressure on these structures.
- The characteristic relief with neck extension and symptoms like stridor, wheezing, and vomiting after feeding are classic signs of airway and esophageal compression by a **vascular ring**.
*Laryngomalacia*
- This condition involves the **collapse of supraglottic structures** during inspiration, typically causing inspiratory stridor, which is often louder when supine or agitated.
- While symptoms can worsen with feeding and crying, the hallmark relief with neck extension and vomiting after feeding due to esophageal compression are not typical features.
*Congenital subglottic stenosis*
- This involves a **narrowing of the airway** below the vocal cords, leading to inspiratory and expiratory stridor, and often biphasic stridor.
- The symptoms are usually persistent and are not characteristically relieved by neck extension or exacerbated by feeding and crying in such a distinct manner.
*Gastroesophageal reflux disease*
- While GERD can cause recurrent vomiting, cough, and even wheezing due to aspiration, it typically does not present with stridor.
- The clear correlation of worsening with neck flexion and relief with neck extension strongly points away from isolated GERD as the primary cause.
*Recurrent viral wheeze*
- This common condition in infants involves episodes of wheezing that are often triggered by **viral respiratory infections**.
- It usually lacks the specific exacerbating and relieving factors related to neck position and feeding, such as relief with neck extension and concurrent vomiting after feeding.
Recurrent laryngeal nerve protection US Medical PG Question 4: During a thyroidectomy, a surgeon must carefully identify and preserve the parathyroid glands. These glands are most commonly located posterior to which part of the thyroid gland?
- A. Superior poles
- B. Inferior poles (Correct Answer)
- C. Pyramidal lobe
- D. Middle third
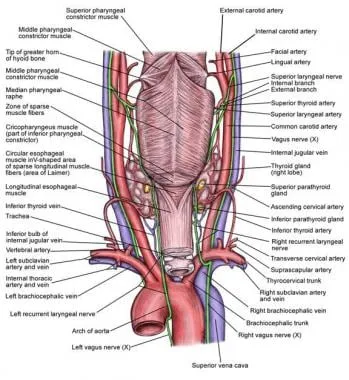
Recurrent laryngeal nerve protection Explanation: Detailed anatomical knowledge is crucial during thyroidectomy to ensure preservation of vital structures [1].
***Inferior poles***
- The **inferior parathyroid glands** (parathyroid IV) are most commonly located posterior to the **inferior poles** of the thyroid gland [1].
- While they are more variable in position than superior glands and can descend into the thymus or mediastinum, the **most common location** is still posterior to the inferior poles [1].
- During thyroidectomy, these glands are frequently encountered in the inferior pole region and must be carefully preserved [1].
*Superior poles*
- The **superior parathyroid glands** (parathyroid III) are typically found at the **middle-to-upper third** of the thyroid, near the cricothyroid junction, rather than directly at the superior poles.
- While their position is more constant than inferior glands, they are not specifically located at the superior poles themselves.
*Pyramidal lobe*
- The **pyramidal lobe** is an embryological remnant extending superiorly from the thyroid isthmus.
- It is not associated with parathyroid gland location, as parathyroids are distinct endocrine structures located on the posterior thyroid surface.
*Middle third*
- The **superior parathyroid glands** are often found near the middle third of the thyroid posteriorly.
- However, when considering all four parathyroid glands (both superior and inferior pairs), the **inferior glands** at the inferior poles represent the most common overall location pattern.
Recurrent laryngeal nerve protection US Medical PG Question 5: A 27-year-old man comes to the physician because of a 1-day history of right-sided facial weakness and sound intolerance. Three days ago, he hit the right side of his head in a motor vehicle collision. He neither lost consciousness nor sought medical attention. Physical examination shows drooping of the mouth on the right side. Sensation over the face is not impaired. Impedance audiometry shows an absence of the acoustic reflex in the right ear. Which of the following muscles is most likely paralyzed in this patient?
- A. Anterior belly of the digastric
- B. Stylopharyngeus
- C. Cricothyroid
- D. Tensor tympani
- E. Stylohyoid (Correct Answer)
Recurrent laryngeal nerve protection Explanation: ***Stylohyoid***
- The patient presents with **facial nerve (CN VII) injury** following head trauma, evidenced by **facial weakness** and **hyperacusis** (sound intolerance).
- The **absent acoustic reflex** indicates paralysis of the **stapedius muscle** (the primary muscle responsible for the acoustic reflex and sound dampening).
- Among the options provided, **stylohyoid** is the only muscle innervated by the **facial nerve (CN VII)**, making it the correct answer in this context.
- The stylohyoid is innervated by the **nerve to stylohyoid**, a branch of CN VII.
*Anterior belly of the digastric*
- The **anterior belly of the digastric** is innervated by the **mylohyoid nerve**, a branch of the **trigeminal nerve (CN V3)**.
- This would not be affected in facial nerve injury.
*Stylopharyngeus*
- The **stylopharyngeus muscle** is innervated by the **glossopharyngeal nerve (CN IX)**.
- Damage would cause **dysphagia** and **loss of taste** on the posterior third of the tongue, not facial weakness or hyperacusis.
*Cricothyroid*
- The **cricothyroid muscle** is innervated by the **external branch of the superior laryngeal nerve** (from **vagus nerve, CN X**).
- Its paralysis causes **voice changes** and difficulty with high-pitched phonation, not facial nerve symptoms.
*Tensor tympani*
- The **tensor tympani muscle** is innervated by the **nerve to tensor tympani**, a branch of the **trigeminal nerve (V3)**.
- Although it dampens sound, it would not be affected in facial nerve injury; the **stapedius muscle** (CN VII) is responsible for the acoustic reflex and hyperacusis when paralyzed.
Recurrent laryngeal nerve protection US Medical PG Question 6: A 54-year-old man comes to the physician because of dysphagia and hoarseness of voice for the past 3 months. Initially, he had difficulty swallowing solid food but now has difficulty swallowing porridge and liquids as well. He has recently been choking on his oral secretions. During this period, he has had an 8.2-kg (18-lb) weight loss. He has noticed increasing weakness of both arms over the past year. He appears ill. His temperature is 36.8°C (98.2°F), pulse is 74/min, respirations are 14/min, and blood pressure is 114/74 mmHg. Examination shows tongue atrophy and pooled oral secretions. There is diffuse muscle atrophy with occasional twitching. He is unable to lift his arms above the chest level. Deep tendon reflexes are 3+ in all extremities. Sensation to pinprick, light touch, and vibration is intact. Laboratory studies show:
Hemoglobin 16.1 g/dL
Leukocyte count 10,900/mm3
Erythrocyte sedimentation rate 20 mm/h
Serum
Na+ 133 mEq/L
K+ 4.2 mEq/L
Cl- 101 mEq/L
Urea nitrogen 12 mg/dL
Creatinine 1.1 mg/dL
Creatine kinase 320 U/L
Albumin 4.3 mg/dL
Lactate dehydrogenase 307 U/L
An esophagogastroduodenoscopy shows no abnormalities. Which of the following is the most likely cause of this patient's symptoms?
- A. Autoimmune destruction of acetylcholine receptors
- B. Dilation of the central spinal canal
- C. Multiple cerebral infarctions
- D. Destruction of upper and lower motor neurons (Correct Answer)
- E. Demyelination of peripheral nerves
Recurrent laryngeal nerve protection Explanation: ***Destruction of upper and lower motor neurons***
- The constellation of **dysphagia**, **hoarseness**, **tongue atrophy**, **generalized muscle atrophy with twitching (fasciculations)**, and **hyperreflexia (3+ deep tendon reflexes)** points strongly to **amyotrophic lateral sclerosis (ALS)**, which involves both upper and lower motor neuron degeneration.
- The progressive weakness, weight loss, and choking on secretions are consistent with bulbar and limb involvement in ALS, a neurodegenerative disorder.
*Autoimmune destruction of acetylcholine receptors*
- This describes **myasthenia gravis**, which typically presents with **fluctuating weakness** that worsens with activity and improves with rest.
- While it can cause dysphagia and bulbar symptoms, **muscle atrophy** and **hyperreflexia** are not characteristic features of myasthenia gravis, and **fasciculations** are absent.
*Dilation of the central spinal canal*
- This refers to **syringomyelia**, a condition where a **syrinx (fluid-filled cyst)** forms within the spinal cord, often leading to **cape-like loss of pain and temperature sensation**, weakness, and atrophy.
- This patient's symptoms of widespread muscle atrophy, fasciculations, bulbar dysfunction, and hyperreflexia are not typical of syringomyelia.
*Multiple cerebral infarctions*
- Multiple cerebral infarctions can lead to various neurological deficits depending on their location, but they typically present with acute or subacute onset of focal neurological signs.
- The **progressive nature** of the patient's symptoms, combined with the specific signs of both upper and lower motor neuron involvement (fasciculations, hyperreflexia), is not characteristic of multiple cerebral infarcts.
*Demyelination of peripheral nerves*
- This describes conditions like **Guillain-Barré syndrome** or **chronic inflammatory demyelinating polyneuropathy (CIDP)**, which predominantly affect **peripheral nerves**.
- While demyelination can cause weakness, it typically leads to **hyporeflexia or areflexia**, and does not explain the presence of **fasciculations** or the signs of **upper motor neuron involvement** (e.g., hyperreflexia) seen in this patient.
Recurrent laryngeal nerve protection US Medical PG Question 7: A 63-year-old man comes to the physician because of a 1-month history of difficulty swallowing, low-grade fever, and weight loss. He has smoked one pack of cigarettes daily for 30 years. An esophagogastroduodenoscopy shows an esophageal mass just distal to the upper esophageal sphincter. Histological examination confirms the diagnosis of locally invasive squamous cell carcinoma. A surgical resection is planned. Which of the following structures is at greatest risk for injury during this procedure?
- A. Bronchial branch of thoracic aorta
- B. Left gastric artery
- C. Left inferior phrenic artery
- D. Esophageal branch of thoracic aorta
- E. Inferior thyroid artery (Correct Answer)
Recurrent laryngeal nerve protection Explanation: **Inferior thyroid artery**
- The esophageal mass is located just distal to the **upper esophageal sphincter**, which is in the neck, close to the **thyroid gland**.
- During surgery for an esophageal tumor in this region, the **inferior thyroid artery**, which supplies the thyroid and adjacent structures, is at the greatest risk of injury due to its proximity.
*Bronchial branch of thoracic aorta*
- The **bronchial branches** of the thoracic aorta primarily supply the bronchi and lungs.
- These vessels are located deeper in the thorax, away from the **upper esophageal sphincter** and the initial surgical field for an upper esophageal tumor.
*Left gastric artery*
- The **left gastric artery** supplies the stomach and is a branch of the celiac trunk.
- This artery is located in the **abdomen**, far from the surgical site involving an esophageal mass near the upper esophageal sphincter.
*Left inferior phrenic artery*
- The **left inferior phrenic artery** primarily supplies the diaphragm.
- This vessel originates from the aorta in the **abdominal region**, which is distant from the upper esophageal sphincter.
*Esophageal branch of thoracic aorta*
- **Esophageal branches** directly supply the esophagus; however, the question refers to the **thoracic aorta branches**.
- Tumors near the **upper esophageal sphincter** are usually accessed via a cervical incision, making thoracic branches less likely to be injured compared to arteries located in the neck.
Recurrent laryngeal nerve protection US Medical PG Question 8: A 75-year-old man is referred for thyroidectomy for treatment of thyroid nodules. A portion of the thyroid gland is resected, and the neck is closed with sutures. After awakening from anesthesia, the patient complains of ‘hoarseness’. His vital signs are normal and his incisional pain is minimal. The surgeon realizes he most likely damaged the recurrent laryngeal nerve. Which of the following should the surgeon tell the patient?
- A. "A mistake occurred during the operation, but there was no harm to you."
- B. "We made a mistake during the operation that may have harmed you." (Correct Answer)
- C. "The case took longer than we thought it would, but everything went well."
- D. "A mistake occurred because this hospital has poor operating room protocols."
- E. "The operation was successful and no complications occurred."
Recurrent laryngeal nerve protection Explanation: ***\"We made a mistake during the operation that may have harmed you.\"***
- This statement accurately reflects the situation, acknowledging both the **mistake** and the potential **harm** to the patient (hoarseness due to recurrent laryngeal nerve damage).
- Open communication and honesty about medical errors are essential for maintaining **trust** and fulfilling ethical obligations to the patient.
*\"A mistake occurred during the operation, but there was no harm to you.\"*
- This statement is inaccurate because the patient is experiencing **hoarseness**, which is a sign of harm (recurrent laryngeal nerve damage).
- Dismissing the patient's symptom as "no harm" is **dishonest** and undermines trust.
*\"The case took longer than we thought it would, but everything went well.\"*
- This statement is misleading as it downplays a significant complication (recurrent laryngeal nerve damage) by implying that "everything went well" despite the patient's hoarseness.
- It avoids addressing the specific concern and does not acknowledge any **error** or **harm**.
*\"A mistake occurred because this hospital has poor operating room protocols.\"*
- While a mistake may have occurred, blaming the hospital's protocols is an attempt to deflect personal responsibility and can be seen as unprofessional.
- This statement introduces a potentially contentious issue that should be addressed internally rather than with the patient when disclosing the error.
*\"The operation was successful and no complications occurred.\"*
- This statement is explicitly false, as **hoarseness** due to recurrent laryngeal nerve damage is a direct and recognized **complication** of thyroidectomy.
- Making such a claim is unethical and violates the principle of **informed consent** and truthful disclosure.
Recurrent laryngeal nerve protection US Medical PG Question 9: An obese 52-year-old man is brought to the emergency department because of increasing shortness of breath for the past 8 hours. Two months ago, he noticed a mass on the right side of his neck and was diagnosed with laryngeal cancer. He has smoked two packs of cigarettes daily for 27 years. He drinks two pints of rum daily. He appears ill. He is oriented to person, place, and time. His temperature is 37°C (98.6°F), pulse is 111/min, respirations are 34/min, and blood pressure is 140/90 mm Hg. Pulse oximetry on room air shows an oxygen saturation of 89%. Examination shows a 9-cm, tender, firm subglottic mass on the right side of the neck. Cervical lymphadenopathy is present. His breathing is labored and he has audible inspiratory stridor but is able to answer questions. The lungs are clear to auscultation. Arterial blood gas analysis on room air shows:
pH 7.36
PCO2 45 mm Hg
PO2 74 mm Hg
HCO3- 25 mEq/L
He has no advanced directive. Which of the following is the most appropriate next step in management?
- A. Comfort care measures
- B. Cricothyroidotomy (Correct Answer)
- C. Tracheostomy
- D. Intramuscular epinephrine
- E. Tracheal stenting
Recurrent laryngeal nerve protection Explanation: ***Correct: Cricothyroidotomy***
- This patient has **impending complete airway obstruction** evidenced by inspiratory stridor, severe tachypnea (34/min), hypoxia (O2 sat 89%), and a large obstructing laryngeal mass
- **Cricothyroidotomy** is the emergent surgical airway procedure of choice when there is **imminent or actual complete upper airway obstruction** and endotracheal intubation cannot be safely performed
- The subglottic mass makes endotracheal intubation **extremely dangerous** - instrumentation could precipitate complete obstruction and inability to ventilate
- Cricothyroidotomy provides **immediate airway access** (can be performed in 30-60 seconds) below the level of obstruction, making it life-saving in this emergency
- In the "cannot intubate, cannot ventilate" scenario, cricothyroidotomy is the definitive emergency intervention per ATLS and airway management guidelines
*Incorrect: Tracheostomy*
- While tracheostomy provides definitive airway management, it is a **controlled, elective procedure** typically performed in the OR that takes 20-30 minutes
- This patient requires **immediate airway access** - waiting for OR setup and performing tracheostomy risks complete airway collapse and death
- Tracheostomy may be performed later as a planned procedure once the airway is secured with cricothyroidotomy
- The presence of stridor indicates **critical airway narrowing** requiring emergency intervention, not elective surgery
*Incorrect: Comfort care measures*
- The patient is **alert and oriented** without an advanced directive indicating wishes for comfort care only
- This is an **acute, reversible condition** with appropriate emergency airway intervention
- Presumed consent applies in life-threatening emergencies when the patient cannot formally consent but intervention would be life-saving
- Comfort care would be inappropriate without documented patient wishes or irreversible terminal condition
*Incorrect: Intramuscular epinephrine*
- Epinephrine is indicated for **anaphylaxis** or angioedema causing airway edema from allergic/inflammatory mechanisms
- This patient has **mechanical obstruction** from a solid tumor mass, which will not respond to epinephrine
- Epinephrine causes vasoconstriction and reduces mucosal edema but cannot reduce tumor mass
- Would delay definitive airway management and not address the underlying problem
*Incorrect: Tracheal stenting*
- Tracheal stenting requires **bronchoscopy** in a controlled setting and is used for palliation of tracheal narrowing
- Cannot be performed emergently in an unstable patient with impending airway obstruction
- The obstruction is at the **laryngeal/subglottic level**, not typically amenable to emergency stenting
- Requires time for procedure setup and sedation, which this patient cannot afford given the critical airway emergency
Recurrent laryngeal nerve protection US Medical PG Question 10: A 58-year-old man with type 2 diabetes mellitus comes to the emergency department because of a 2-day history of dysphagia and swelling in the neck and lower jaw. He has had tooth pain on the left side over the past week, which has made it difficult for him to sleep. Four weeks ago, he had a 3-day episode of flu-like symptoms, including sore throat, that resolved without treatment. He has a history of hypertension. Current medications include metformin and lisinopril. He appears distressed. He is 180 cm (5 ft 11 in) tall and weighs 100 kg (220 lbs); his BMI is 31.6 kg/m2. His temperature is 38.4°C (101.1°F), pulse is 90/min, and blood pressure is 110/80 mm Hg. Oral cavity examination shows a decayed lower left third molar with drainage of pus. There is submandibular and anterior neck tenderness and swelling. His leukocyte count is 15,600/mm3, platelet count is 300,000/mm3, and fingerstick blood glucose concentration is 250 mg/dL. Which of the following is the most likely diagnosis?
- A. Angioedema
- B. Peritonsillar abscess
- C. Lymphadenitis
- D. Sublingual hematoma
- E. Ludwig angina (Correct Answer)
Recurrent laryngeal nerve protection Explanation: ***Ludwig angina***
- This patient presents with **rapidly progressive submandibular and anterior neck swelling**, dysphagia, fever, and a history of a recent dental infection (decayed molar with pus drainage). These are classic signs of **Ludwig angina**, a severe cellulitis of the floor of the mouth.
- The patient's **poorly controlled diabetes** and **obesity** are risk factors for severe infections, and the elevated leukocyte count further supports an active bacterial infection.
*Angioedema*
- **Angioedema** typically presents with rapid swelling of the face, lips, tongue, or larynx, but it is usually **non-pitting** and **painless**, without systemic signs of infection (fever, pus, elevated leukocytes).
- While lisinopril can cause angioedema, the presence of **fever, pus drainage from a tooth, and tenderness** makes an infectious etiology more likely than an allergic or bradykinin-mediated angioedema.
*Peritonsillar abscess*
- A **peritonsillar abscess** is characterized by severe **sore throat**, **trismus**, **"hot potato" voice**, and a **uvular deviation**, which are not reported in this patient.
- While it can cause dysphagia and fever, the primary swelling in this case is submandibular and anterior neck, not peritonsillar.
*Lymphadenitis*
- **Cervical lymphadenitis** involves painful, enlarged **lymph nodes**, often in response to an infection. While the patient has an infection, lymphadenitis would present as discrete node enlargement rather than diffuse, board-like swelling of the floor of the mouth and submandibular space.
- The extensive swelling, dysphagia, and involvement of fascial planes are more consistent with a spreading cellulitis like Ludwig angina.
*Sublingual hematoma*
- A **sublingual hematoma** would typically result from **trauma** or a **coagulopathy**, neither of which is indicated in this patient's history.
- It would also not explain the fever, pus drainage, and elevated leukocyte count indicative of an active infection.
More Recurrent laryngeal nerve protection US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.