Postoperative hypocalcemia management US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Postoperative hypocalcemia management. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Postoperative hypocalcemia management US Medical PG Question 1: A 48-year-old woman underwent a thyroidectomy with central neck dissection due to papillary thyroid carcinoma. On day 2 postoperatively, she developed irritability, dysphagia, difficulty breathing, and spasms in different muscle groups in her upper and lower extremities. The vital signs include blood pressure 102/65 mm Hg, heart rate 93/min, respiratory rate 17/min, and temperature 36.1℃ (97.0℉). Physical examination shows several petechiae on her forearms, muscle twitching in her upper and lower extremities, expiratory wheezes on lung auscultation, decreased S1 and S2 and the presence of an S3 on cardiac auscultation, and positive Trousseau and Chvostek signs. Laboratory studies show:
Ca2+ 4.4 mg/dL
Mg2+ 1.7 mEq/L
Na+ 140 mEq/L
K+ 4.3 mEq/L
Cl- 107 mEq/L
HCO3- 25 mEq/L
Administration of which of the following agents could prevent the patient’s condition?
- A. Anticonvulsants prior to and for 1 week after the operation
- B. Vitamin D and ionic calcium prior to and 2 weeks after the operation (Correct Answer)
- C. Potassium supplementation prior to and 2 weeks after the operation
- D. Calcium gluconate intraoperatively
- E. Magnesium sulfate intraoperatively
Postoperative hypocalcemia management Explanation: ***Vitamin D and ionic calcium prior to and 2 weeks after the operation***
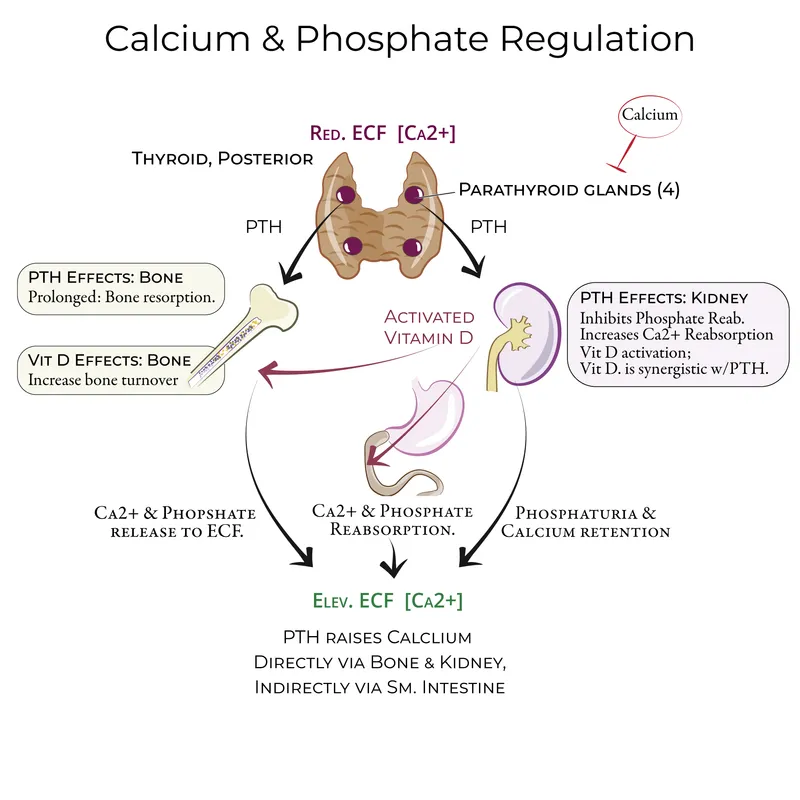
- The patient's symptoms are consistent with **hypocalcemia** (low calcium), a common complication after thyroidectomy due to inadvertent parathyroid gland removal or damage. Prophylactic **calcium and vitamin D supplementation** can prevent severe postoperative hypocalcemia by helping maintain calcium homeostasis.
- The patient's calcium level of 4.4 mg/dL (normal range 8.5-10.2 mg/dL) confirms severe hypocalcemia. The presence of **Trousseau and Chvostek signs**, muscle spasms, and dysphagia are classic signs of hypocalcemic tetany.
*Anticonvulsants prior to and for 1 week after the operation*
- This patient's symptoms are not indicative of an underlying seizure disorder, but rather **neuromuscular excitability** due to hypocalcemia. Anticonvulsants would not address the root cause.
- While severe hypocalcemia can rarely lead to seizures, prophylactic anticonvulsant administration is not standard practice for preventing this specific post-thyroidectomy complication.
*Potassium supplementation prior to and 2 weeks after the operation*
- The patient's potassium level is 4.3 mEq/L, which is within the normal range (3.5-5.0 mEq/L). **Hyperkalemia or hypokalemia** is not the primary issue here.
- Potassium supplementation would not address the hypocalcemia causing her symptoms and could potentially lead to **hyperkalemia**, which has its own set of dangers.
*Calcium gluconate intraoperatively*
- **Intraoperative calcium gluconate** is typically used for acute, severe hypocalcemia or cardiac arrest, not as a prophylactic measure. Administering it intraoperatively would not prevent the delayed onset of hypocalcemia seen on day 2.
- The goal is to prevent hypocalcemia by supporting calcium levels proactively, rather than treating an acute drop during surgery, which is rare.
*Magnesium sulfate intraoperatively*
- The patient's magnesium level of 1.7 mEq/L is at the lower limit of normal (1.7-2.2 mEq/L). While **hypomagnesemia** can impair PTH secretion and cause refractory hypocalcemia, magnesium supplementation is not the primary prophylactic strategy for post-thyroidectomy hypocalcemia.
- Intraoperative magnesium sulfate would not address the fundamental issue of parathyroid gland injury or removal causing the hypocalcemia. Calcium and vitamin D remain the cornerstone of prevention.
Postoperative hypocalcemia management US Medical PG Question 2: A 45-year-old woman presents to her primary care provider complaining of daytime drowsiness and fatigue. She reports that she can manage at most a couple of hours of work before needing a nap. She has also noted impaired memory and a 6.8 kg (15 lb) weight gain. She denies shortness of breath, chest pain, lightheadedness, or blood in her stool. At the doctor’s office, the vital signs include: pulse 58/min, blood pressure 104/68 mm Hg, and oxygen saturation 99% on room air. The physical exam is notable only for slightly dry skin. The complete blood count (CBC) is within normal limits. Which of the following is a likely additional finding in this patient?
- A. Tremor
- B. Anxiety
- C. Hypercholesterolemia (Correct Answer)
- D. Lid lag
- E. Palpitations
Postoperative hypocalcemia management Explanation: ***Hypercholesterolemia***
- The patient's symptoms of **fatigue, weight gain, impaired memory, daytime drowsiness, dry skin, and bradycardia** are classic for **hypothyroidism**.
- **Hypothyroidism** leads to a decrease in the breakdown of **lipids**, resulting in elevated **LDL cholesterol and triglycerides**.
*Tremor*
- A **fine tremor** is commonly associated with **hyperthyroidism**, not hypothyroidism, due to sympathetic overactivity.
- It is a sign of an **overactive metabolic state**, which is the opposite of the patient's presentation.
*Anxiety*
- While anxiety can be a symptom of many conditions, it is more typically associated with **hyperthyroidism** due to increased metabolic activity and sympathetic tone.
- Patients with **hypothyroidism** tend to experience **depression, lethargy, and slowed mentation** rather than anxiety.
*Lid lag*
- **Lid lag** (Graefe's sign) is a classic ophthalmic sign of **hyperthyroidism**, often seen in **Graves' ophthalmopathy**.
- It is caused by increased sympathetic stimulation of the **levator palpebrae superioris muscle**, not a feature of hypothyroidism.
*Palpitations*
- **Palpitations** are a common symptom of **hyperthyroidism** due to increased heart rate and contractility.
- In contrast, **hypothyroidism** is usually associated with **bradycardia** and a *slowed heart rate*, as seen in this patient.
Postoperative hypocalcemia management US Medical PG Question 3: A 1-year-old boy presents to pediatrics clinic for a well-child visit. He has no complaints. He has a cleft palate and an abnormal facial appearance. He has been riddled with recurrent infections and is followed by cardiology for a ventricular septal defect (VSD). Vital signs are stable, and the patient's physical exam is benign. If this patient's medical history is part of a larger syndrome, what might one also discover that is consistent with the manifestations of this syndrome?
- A. Kidney stones
- B. A positive Chvostek's sign (Correct Answer)
- C. B-cell deficiency
- D. Hypoactive deep tendon reflexes
- E. A shortened QT Interval
Postoperative hypocalcemia management Explanation: ***A positive Chvostek's sign***
- The constellation of **cleft palate**, **abnormal facial appearance**, **recurrent infections**, and a **ventricular septal defect (VSD)** strongly suggests **DiGeorge syndrome**.
- In DiGeorge syndrome, hypoparathyroidism leads to **hypocalcemia**, which can manifest as neuromuscular irritability, including a positive **Chvostek's sign** (facial muscle twitching upon tapping the facial nerve).
*Kidney stones*
- **Kidney stones** are typically associated with **hypercalcemia** or other metabolic disorders, not hypocalcemia seen in DiGeorge syndrome.
- While DiGeorge patients can have renal anomalies, **nephrolithiasis** is not a characteristic feature of the syndrome.
*B-cell deficiency*
- DiGeorge syndrome is characterized by **T-cell deficiency** due to thymic hypoplasia or aplasia, not primarily B-cell deficiency.
- While **B cells** may be secondarily affected due to lack of T-cell help, the primary immunodeficiency is related to T-lymphocytes.
*Hypoactive deep tendon reflexes*
- **Hypocalcemia** typically causes **hyperactive deep tendon reflexes** and increased neuromuscular excitability, not hypoactivity.
- **Hypoactive reflexes** might suggest conditions like hypothyroidism or certain neurological disorders.
*A shortened QT Interval*
- **Hypocalcemia** is associated with a **prolonged QT interval** on an electrocardiogram, not a shortened one.
- A **shortened QT interval** can occur in conditions like hypercalcemia or genetic channelopathies.
Postoperative hypocalcemia management US Medical PG Question 4: A 57-year-old man comes to the emergency department for the evaluation of worsening fatigue, urinary frequency, and constipation over the past 5 days. He was recently diagnosed with metastatic bladder cancer and is currently awaiting treatment. He has smoked 1 pack of cigarettes daily for 35 years. Physical examination shows dry mucous membranes and diffuse abdominal tenderness. An ECG shows a shortened QT interval. Which of the following sets of serum findings is most likely in this patient?
$$$ Calcium %%% Phosphorus %%% Parathyroid hormone %%% 1,25-dihydroxyvitamin D $$$
- A. ↑ ↓ ↓ ↓ (Correct Answer)
- B. ↑ ↑ ↓ ↑
- C. ↑ ↑ ↑ ↓
- D. ↑ ↓ ↑ ↑
- E. ↓ ↑ ↑ ↓
Postoperative hypocalcemia management Explanation: ***↑ ↓ ↓ ↓***
- This pattern of **elevated calcium**, **low phosphorus**, **low parathyroid hormone (PTH)**, and **low 1,25-dihydroxyvitamin D** is characteristic of **humoral hypercalcemia of malignancy (HHM)**. Malignant cells, particularly those from bladder cancer, can secrete **parathyroid hormone-related peptide (PTHrP)**, mimicking PTH, leading to increased bone resorption and renal calcium reabsorption, while suppressing endogenous PTH and indirectly leading to low 1,25-dihydroxyvitamin D synthesis.
- The patient's symptoms of fatigue, constipation, urinary frequency, and signs like dry mucous membranes and a shortened QT interval on ECG are all consistent with **hypercalcemia**.
*↑ ↑ ↓ ↑*
- This pattern suggests **hypercalcemia** with **elevated phosphorus** and **elevated 1,25-dihydroxyvitamin D**, which is inconsistent with HHM. Elevated phosphorus is more commonly seen in conditions like **renal failure** or **tumor lysis syndrome**, neither of which are indicated here.
- Elevated 1,25-dihydroxyvitamin D is typically seen in **granulomatous diseases** (e.g., sarcoidosis) or **lymphomas** causing hypercalcemia, not bladder carcinoma.
*↑ ↑ ↑ ↓*
- This profile indicates **hypercalcemia**, **elevated phosphorus**, and **elevated PTH**, which is consistent with **primary hyperparathyroidism**. However, primary hyperparathyroidism typically presents with inappropriately elevated PTH for the level of hypercalcemia, and it's less likely to develop acute, severe hypercalcemia with malignancy unless concurrent.
- The patient's presentation with advanced bladder cancer makes HHM a more likely cause of hypercalcemia than primary hyperparathyroidism.
*↑ ↓ ↑ ↑*
- This constellation, with **elevated calcium**, **low phosphorus**, and **elevated PTH**, is classic for **primary hyperparathyroidism**. In this condition, inappropriately high PTH levels cause increased bone resorption, renal calcium reabsorption, and renal phosphate excretion, leading to hypophosphatemia.
- While primary hyperparathyroidism causes hypercalcemia, the clinical context of advanced metastatic bladder cancer makes HHM a much more probable diagnosis in this patient, and PTH would be suppressed in HHM due to PTHrP mimicking its effects.
*↓ ↑ ↑ ↓*
- This pattern describes **hypocalcemia** (low calcium) with **elevated phosphorus** and **elevated PTH**. This is the hallmark of **secondary hyperparathyroidism**, often seen in **chronic kidney disease**, where low calcium and high phosphorus stimulate PTH release.
- The patient in the vignette presents with symptoms of hypercalcemia, not hypocalcemia, making this option inconsistent with the clinical picture.
Postoperative hypocalcemia management US Medical PG Question 5: A 28-year-old woman presents to her primary care physician with recurring muscle cramps that have lasted for the last 2 weeks. She mentions that she commonly has these in her legs and back. She also has a constant tingling sensation around her mouth. On physical examination, her vital signs are stable. The Trousseau sign and Chvostek sign are present with exaggerated deep tendon reflexes. A comprehensive blood test reveals the following:
Na+ 140 mEq/L
K+ 4.5 mEq/L
Chloride 100 mEq/L
Bicarbonate 24 mEq/L
Creatinine 0.9 mg/dL
Ca2+ 7.0 mg/dL
Which of the following electrophysiologic mechanisms best explain this woman’s clinical features?
- A. Decreased firing threshold for action potential (Correct Answer)
- B. Reduction of afterhyperpolarization
- C. Inhibition of sodium current through sodium leak channels (NALCN)
- D. Inhibition of Na+ and Ca2+ currents through cyclic nucleotide-gated (CNG) channels
- E. Stimulation of GABA (γ-aminobutyric acid) receptors
Postoperative hypocalcemia management Explanation: ***Decreased firing threshold for action potential***
- The patient exhibits symptoms of **hypocalcemia** (muscle cramps, perioral tingling, positive Trousseau and Chvostek signs), indicated by her **low serum Ca2+ (7.0 mg/dL)**.
- **Hypocalcemia** leads to increased neuronal excitability by **decreasing the threshold for action potential firing**.
- **Mechanism**: Extracellular calcium ions normally bind to negatively charged groups on voltage-gated sodium channels, stabilizing them in the closed state and increasing the threshold for opening.
- With **low calcium**, this stabilization is reduced, allowing sodium channels to open more easily at less negative membrane potentials, effectively **lowering the firing threshold**.
- This results in spontaneous depolarizations and the neuromuscular hyperexcitability seen clinically as tetany, muscle cramps, and hyperreflexia.
*Stimulation of GABA (γ-aminobutyric acid) receptors*
- **GABA receptor stimulation** leads to **inhibition of neuronal activity** by increasing chloride influx, hyperpolarizing the cell, and reducing excitability.
- This would **decrease muscle cramps and excitability**, opposite to the patient's symptoms.
*Reduction of afterhyperpolarization*
- While hypocalcemia does affect membrane excitability, the **primary mechanism** is the decreased threshold for sodium channel activation, not afterhyperpolarization changes.
- Reduction of afterhyperpolarization would affect repetitive firing patterns but does not explain the initial hyperexcitability at the sodium channel level.
*Inhibition of sodium current through sodium leak channels (NALCN)*
- **NALCN channels** contribute to resting membrane potential; their inhibition would lead to **hyperpolarization** and reduced excitability.
- This is opposite to the **hypocalcemic hyperexcitability** observed in this patient.
*Inhibition of Na+ and Ca2+ currents through cyclic nucleotide-gated (CNG) channels*
- **CNG channels** are primarily involved in sensory signal transduction (vision, olfaction).
- Their inhibition would cause specific sensory deficits, not the generalized neuromuscular hyperexcitability seen in **hypocalcemia**.
Postoperative hypocalcemia management US Medical PG Question 6: An 80-year-old male with known metastatic prostate cancer presents to your office with vague complaints of "achy bones." Strangely, he refers to you using the name of another physician. On physical exam, he is afebrile, but mildly tachycardic at 100 beats/min. Mucous membranes are dry. Cardiac exam shows regular rhythm and no murmurs. The patient has diffuse, nonfocal abdominal pain. He cannot articulate the correct date. You check the patient's serum calcium level, which is found to be 15.3 mg/dL. What is the best next step in management?
- A. Calcitonin
- B. Intravenous normal saline (Correct Answer)
- C. Furosemide
- D. Pamidronate
- E. Hemodialysis
Postoperative hypocalcemia management Explanation: ***Intravenous normal saline***
- The patient exhibits classic symptoms of **hypercalcemia** (vague bone aches, confusion, dry mucous membranes, tachycardia, diffuse nonfocal abdominal pain) in the context of metastatic prostate cancer and a severely elevated serum calcium level of 15.3 mg/dL.
- **Volume expansion with intravenous normal saline** is the initial and most crucial step in managing severe hypercalcemia, as it helps to restore hydration and promote renal calcium excretion.
*Calcitonin*
- **Calcitonin** can rapidly lower serum calcium by inhibiting osteoclastic bone resorption and increasing renal calcium excretion, but its effect is typically transient and less potent than initial hydration.
- It is often used as an adjunct to saline and bisphosphonates, especially in cases where a rapid but temporary decrease in calcium is needed.
*Furosemide*
- **Furosemide** (a loop diuretic) should only be considered *after* adequate volume repletion has been achieved, as it can worsen dehydration and electrolyte abnormalities if given prematurely.
- It works by inhibiting calcium reabsorption in the loop of Henle, but **dehydration must be corrected first** to ensure effective GFR and avoid electrolyte imbalance.
*Pamidronate*
- **Pamidronate** (a bisphosphonate) is a potent inhibitor of osteoclast-mediated bone resorption and is effective in long-term management of hypercalcemia of malignancy.
- However, its onset of action is slow (2-4 days) and therefore it is not the best *initial step* for acutely symptomatic and severely hypercalcemic patients.
*Hemodialysis*
- **Hemodialysis** is reserved for severe, refractory hypercalcemia, particularly in patients with **renal failure** who cannot handle large fluid loads or excrete calcium effectively.
- While effective, it is an invasive procedure and not typically the first-line treatment for hypercalcemia of malignancy in a patient with presumably intact renal function capable of responding to hydration.
Postoperative hypocalcemia management US Medical PG Question 7: A 30-year-old woman is brought to the urgent care clinic by her husband. She complains of numbness around her lips and a tingling sensation in her hands and feet. She underwent near-total thyroidectomy for an enlarged thyroid gland a month ago. Vital signs include: blood pressure is 130/70 mm Hg, pulse is 72/min, respiratory rate is 16/min, and temperature is 37.0°C (98.6°F). A surgical incision scar is present in the anterior aspect of the neck. The attending physician inflates the blood pressure cuff above 150 mm Hg and observes the patient a couple of minutes while measuring her blood pressure. The patient develops sudden stiffness and tingling in her hand. Blood test results are as follows:
Hemoglobin (Hb%) 10.2 g/dL
White blood cell count 7000/mm3
Platelet count 160,000/mm3
Calcium, serum (Ca2+) 6.0 mg/dL
Albumin 4 g/dL
Alanine aminotransferase (ALT), serum 15 U/L
Aspartate aminotransferase (AST), serum 8 U/L
Serum creatinine 0.5 mg/dL
Urea 27 mg/dL
Sodium 137 mEq/L
Potassium 4.5 mEq/L
Magnesium 2.5 mEq/L
Urinalysis shows no white or red blood cells and leukocyte esterase is negative. Which of the following is the next best step in the management of this patient?
- A. 24-hour urinary calcium
- B. Serum vitamin D level
- C. CT scan abdomen with pancreatic protocol
- D. Thyroid function tests
- E. Serum parathyroid hormone (PTH) level (Correct Answer)
Postoperative hypocalcemia management Explanation: ***Serum parathyroid hormone (PTH) level***
- The patient presents with **symptoms of hypocalcemia** (perioral numbness, tingling in hands and feet, positive Trousseau's sign, and serum calcium of 6.0 mg/dL) following a **near-total thyroidectomy**.
- Measuring **PTH levels** is crucial to determine if the hypocalcemia is due to **parathyroid gland damage** (low PTH) or another cause (high PTH).
*24-hour urinary calcium*
- This test is primarily used in the workup of **hypercalcemia** or **kidney stone disease** to assess calcium excretion.
- It is **not the initial diagnostic step** for symptomatic hypocalcemia post-thyroidectomy.
*Serum vitamin D level*
- While **vitamin D deficiency** can contribute to hypocalcemia, the acute onset of symptoms following thyroid surgery strongly points to parathyroid involvement.
- Addressing the **immediate calcium deficit** and evaluating PTH are higher priorities than measuring vitamin D levels at this stage.
*CT scan abdomen with pancreatic protocol*
- A CT scan of the abdomen with pancreatic protocol is used to evaluate **pancreatic pathology**, such as pancreatitis or tumors.
- This investigation is **irrelevant** to the patient's symptoms and recent thyroid surgery.
*Thyroid function tests*
- While important for managing patients post-thyroidectomy, routine thyroid function tests (TSH, T3, T4) are primarily to assess for **hypothyroidism** or **hyperthyroidism**.
- They do **not directly explain acute hypocalcemic symptoms** or guide immediate management of low calcium.
Postoperative hypocalcemia management US Medical PG Question 8: A 27-year-old man is brought to the emergency department after a motor vehicle accident. He was the unrestrained driver in a head on collision. The patient is responding incoherently and is complaining of being in pain. He has several large lacerations and has been impaled with a piece of metal. IV access is unable to be obtained and a FAST exam is performed. His temperature is 98.2°F (36.8°C), blood pressure is 90/48 mmHg, pulse is 150/min, respirations are 13/min, and oxygen saturation is 98% on room air. Which of the following is the best next step in management?
- A. Reattempt intravenous access
- B. Obtain intraosseous access (Correct Answer)
- C. Place a central line
- D. Administer oral fluids
- E. Exploratory laparotomy
Postoperative hypocalcemia management Explanation: ***Obtain intraosseous access***
- The patient is in **hypotensive shock** (BP 90/48 mmHg, HR 150/min) after a severe trauma, and **IV access cannot be obtained**. **Intraosseous (IO) access** provides a rapid and reliable route for fluid and medication administration in emergent situations when peripheral IV access is difficult or impossible.
- While central line placement is also a viable option, **IO access is generally faster and easier to establish** in an emergency setting by a wide range of providers, making it the **best initial step** when peripheral IV fails.
*Reattempt intravenous access*
- Although obtaining IV access is critical, the question states that it "is unable to be obtained," implying initial attempts have failed or are proving too difficult/time-consuming given the patient's critical state.
- Persisting with repeated attempts risks significant delay in resuscitation, which is detrimental for a patient in shock.
*Place a central line*
- A central line provides reliable access for fluid and medication, but its placement is generally **more time-consuming** and technically challenging than IO access, especially in an agitated, unstable patient in a chaotic emergency setting.
- The immediate priority is rapid access for fluids to address the patient's shock, for which IO is superior in terms of speed of establishment.
*Administer oral fluids*
- The patient is **unstable**, **incoherently responding**, and likely has significant internal injuries given the mechanism of injury (head-on collision, impalement).
- Oral fluids would be **ineffective** and potentially dangerous (risk of aspiration) in this critical, hemodynamically unstable patient who requires immediate intravenous fluid resuscitation.
*Exploratory laparotomy*
- While the patient likely has significant internal injuries requiring surgical intervention (impalement, hypovolemic shock), an **exploratory laparotomy** is a definitive treatment step, not the *best next step in management* for immediate resuscitation.
- **Hemodynamic stabilization** with fluid resuscitation must occur *before* or *simultaneously with* definitive surgical intervention to improve survival chances.
Postoperative hypocalcemia management US Medical PG Question 9: A 27-year-old man is brought to the emergency department by ambulance following a motor vehicle accident 1 hour prior. He appears agitated. His blood pressure is 85/60 mm Hg, the pulse is 110/min, and the respiratory rate is 19/min. Physical examination shows bruising of the left flank and fracture of the left lower thoracic bones. Strict bed rest and monitoring with intravenous fluids is initiated. Urinalysis shows numerous RBCs. A contrast-enhanced CT scan shows normal enhancement of the right kidney. The left renal artery is only visible in the proximal section with a small amount of extravasated blood around the left kidney. The left kidney shows no enhancement. Imaging of the spleen shows no abnormalities. Which of the following is the most appropriate next step in management?
- A. Immediate surgical exploration (Correct Answer)
- B. Observation with delayed repair
- C. Conservative management
- D. Renal artery embolization
- E. Renal artery embolization with delayed nephrectomy
Postoperative hypocalcemia management Explanation: ***Immediate surgical exploration***
- The patient presents with signs of **hemodynamic instability** (BP 85/60, pulse 110/min, agitation) and imaging findings consistent with **left renal artery avulsion** and devascularization (no enhancement of the left kidney, visible only proximally, extravasated blood). These findings necessitate immediate surgical intervention to control hemorrhage and assess kidney viability.
- The goal is to revascularize the kidney if possible, perform a nephrectomy if the kidney is unsalvageable, and manage hemorrhage to stabilize the patient.
*Observation with delayed repair*
- This approach is typically reserved for **hemodynamically stable** patients with renal injuries, especially lower-grade injuries that do not involve complete vessel avulsion or ongoing significant hemorrhage.
- Delaying intervention in a hemodynamically unstable patient with a presumed renal artery avulsion can lead to further decompensation, irreversible kidney damage, and increased mortality.
*Conservative management*
- **Conservative management** is appropriate for hemodynamically stable patients with minor renal injuries, such as contusions or small lacerations, or for very selected cases of more severe injuries that have spontaneously tamponaded and are not causing significant clinical compromise.
- The patient's **hemodynamic instability** and direct evidence of renal artery injury preclude conservative management in this case.
*Renal artery embolization*
- **Renal artery embolization** is a highly effective, minimally invasive technique for controlling bleeding from renal injuries. However, it is primarily indicated for **hemodynamically stable patients** with contained hemorrhage or specific pseudoaneurysms/AV fistulas.
- In a hemodynamically unstable patient with a complete renal artery avulsion and non-perfused kidney, embolization is unlikely to revascularize the kidney and may even hinder subsequent surgical repair if revascularization is deemed possible. Furthermore, it might not be sufficient to control diffuse or extensive bleeding associated with avulsion.
*Renal artery embolization with delayed nephrectomy*
- While embolization can precede nephrectomy in certain scenarios for better hemorrhage control, it is not the primary immediate step in a **hemodynamically unstable** patient with renal artery avulsion and a non-enhancing kidney.
- The primary concern is the patient's instability, which requires immediate surgical control, and delaying nephrectomy after embolization often isn't feasible if the kidney is completely devascularized and the patient is unstable. The decision for nephrectomy typically occurs during the initial surgical exploration.
Postoperative hypocalcemia management US Medical PG Question 10: A 67-year-old woman with tertiary hyperparathyroidism and end-stage renal disease on hemodialysis has persistent hypercalcemia (calcium 12.8 mg/dL) despite maximal medical management with cinacalcet and vitamin D restriction. She has severe pruritus, calciphylaxis, and vascular calcifications. All four parathyroid glands are enlarged on imaging. Evaluate the optimal surgical strategy considering her complex medical status and need for ongoing dialysis access.
- A. Single adenoma resection guided by sestamibi
- B. Subtotal parathyroidectomy (3.5 gland resection)
- C. Total parathyroidectomy without autotransplantation
- D. Total parathyroidectomy with forearm autotransplantation (Correct Answer)
- E. Medical management escalation with denosumab
Postoperative hypocalcemia management Explanation: ***Total parathyroidectomy with forearm autotransplantation***
- In **tertiary hyperparathyroidism** with four-gland enlargement, this procedure provides definitive treatment while allowing for easier access if **recurrent hyperplasia** occurs.
- Placing the tissue in the **forearm** avoids risky neck re-explorations in the future and is the standard for patients who may remain on long-term dialysis.
*Single adenoma resection guided by sestamibi*
- This approach is inappropriate because **tertiary hyperparathyroidism** involves **multiglandular hyperplasia**, not a single solitary adenoma.
- Imaging with **sestamibi** is less reliable in renal patients, and leaving three hyperplastic glands would lead to surgical failure.
*Subtotal parathyroidectomy (3.5 gland resection)*
- While a valid option for some, it carries a higher risk of **persistent hypercalcemia** or recurrence within the neck remnant compared to total resection.
- In patients with **calciphylaxis** and severe symptoms, many surgeons prefer total resection to ensure immediate clearance of excess **parathyroid hormone**.
*Total parathyroidectomy without autotransplantation*
- This technique leads to permanent **hypoparathyroidism**, which is difficult to manage and can result in **adynamic bone disease**.
- It is generally reserved for patients who are not candidates for future transplantation and have severe, life-threatening **hypercalcemia** where no hormonal replacement is desired.
*Medical management escalation with denosumab*
- The patient has already failed **maximal medical management** including **cinacalcet**, and her severe **calciphylaxis** is a surgical emergency.
- **Denosumab** does not address the underlying autonomous parathyroid hyperplasia and is not a definitive treatment for **tertiary hyperparathyroidism**.
More Postoperative hypocalcemia management US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.