Pheochromocytoma resection US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Pheochromocytoma resection. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Pheochromocytoma resection US Medical PG Question 1: A 30-year-old man comes to the physician for follow-up evaluation for hypertension. He reports a 1-month history of episodic throbbing headaches, palpitations, and paroxysmal sweating. Blood pressure is 160/90 mm Hg. He appears pale but physical examination is otherwise unremarkable. Laboratory studies show elevated urine and plasma metanephrines. A CT scan of the abdomen shows a mass in the left adrenal gland. Which of the following is the most appropriate initial pharmacotherapy for this patient?
- A. Propranolol
- B. Phenoxybenzamine (Correct Answer)
- C. Hydrochlorothiazide
- D. Octreotide
- E. Clonidine
Pheochromocytoma resection Explanation: ***Phenoxybenzamine***
- This patient presents with symptoms highly suggestive of a **pheochromocytoma** (episodic throbbing headaches, palpitations, paroxysmal sweating, hypertension), confirmed by **elevated metanephrines** and an **adrenal mass**.
- **Alpha-blockade** with phenoxybenzamine is the initial and crucial step for blood pressure control to prevent a **hypertensive crisis** during surgical tumor removal.
*Propranolol*
- **Beta-blockers** like propranolol should only be administered *after* adequate alpha-blockade has been established.
- Giving a beta-blocker first can lead to **unopposed alpha-adrenergic stimulation**, worsening hypertension and potentially causing a hypertensive crisis.
*Hydrochlorothiazide*
- This is a **thiazide diuretic** used for essential hypertension and is not appropriate for the acute management of a **pheochromocytoma-induced hypertensive crisis**.
- It does not address the underlying catecholamine excess and would be ineffective in preventing a crisis.
*Octreotide*
- **Octreotide** is a somatostatin analog primarily used to treat neuroendocrine tumors like **carcinoid syndrome** or VIPomas.
- It has no role in the management of pheochromocytoma, which arises from chromaffin cells and secretes catecholamines.
*Clonidine*
- **Clonidine** is an **alpha-2 adrenergic agonist** that reduces sympathetic outflow from the central nervous system.
- While it can lower blood pressure, it is not the first-line agent for pheochromocytoma and does not provide the comprehensive, irreversible alpha-blockade needed for surgical preparation.
Pheochromocytoma resection US Medical PG Question 2: A 25-year-old man presents to the emergency department with a severe pulsatile headache for an hour. He says that he is having palpitations as well. He adds that he has had several episodes of headache in the past which resolved without seeking medical attention. He is a non-smoker and does not drink alcohol. He denies use of any illicit drugs. He looks scared and anxious. His temperature is 37°C (98.6°F), respirations are 25/min, pulse is 107/min, and blood pressure is 221/161 mm Hg. An urgent urinalysis reveals elevated plasma metanephrines. What is the next best step in the management of this patient?
- A. Hydralazine
- B. Amlodipine
- C. Phenoxybenzamine followed by propranolol (Correct Answer)
- D. Propranolol followed by phenoxybenzamine
- E. Emergent surgery
Pheochromocytoma resection Explanation: ***Phenoxybenzamine followed by propranolol***
- This patient presents with symptoms highly suggestive of a **pheochromocytoma crisis**, including **severe headache**, **palpitations**, **hypertension**, **tachycardia**, and **anxiety**, along with elevated **plasma metanephrines**. The initial management for a pheochromocytoma crisis is **alpha-blockade** (e.g., with phenoxybenzamine) to control the severe hypertension, followed by **beta-blockade** (e.g., with propranolol) to manage tachycardia and prevent unopposed alpha-agonist effects.
- Giving a beta-blocker before an alpha-blocker can lead to **unopposed alpha-adrenergic stimulation**, which can cause a life-threatening increase in blood pressure due to vasoconstriction.
*Hydralazine*
- While **hydralazine** is a potent direct vasodilator used for hypertensive emergencies, it is generally **not the first-line treatment for pheochromocytoma** crisis.
- It can cause reflex **tachycardia**, which might be detrimental in a patient with excessive catecholamine release.
*Amlodipine*
- **Amlodipine** is a **calcium channel blocker** that can lower blood pressure.
- However, it is **not the preferred initial agent for the acute hypertensive crisis** associated with pheochromocytoma, which requires specific alpha-blockade.
*Propranolol followed by phenoxybenzamine*
- Administering a **beta-blocker** (propranolol) before an **alpha-blocker** (phenoxybenzamine) in a patient with pheochromocytoma is **contraindicated** and potentially dangerous.
- This sequence could lead to **unopposed alpha-adrenergic stimulation**, resulting in profound **vasoconstriction** and an extreme, life-threatening increase in blood pressure.
*Emergent surgery*
- While surgical removal of the tumor (adrenalectomy) is the **definitive treatment** for pheochromocytoma, it is **not the immediate next step** in a hypertensive crisis.
- The patient needs **pharmacological stabilization** of blood pressure and heart rate first to reduce surgical risks.
Pheochromocytoma resection US Medical PG Question 3: A 20-year-old man is brought to the emergency room for evaluation of a back injury sustained while at work. A CT scan of the lumbar spine shows an incidental 2-cm mass adjacent to the inferior vena cava. Histologic examination of a biopsy specimen of the mass shows clusters of chromaffin cells. This mass is most likely to secrete which of the following substances?
- A. Aldosterone
- B. Dehydroepiandrosterone
- C. Norepinephrine (Correct Answer)
- D. Cortisol
- E. Estrogen
Pheochromocytoma resection Explanation: **Norepinephrine**
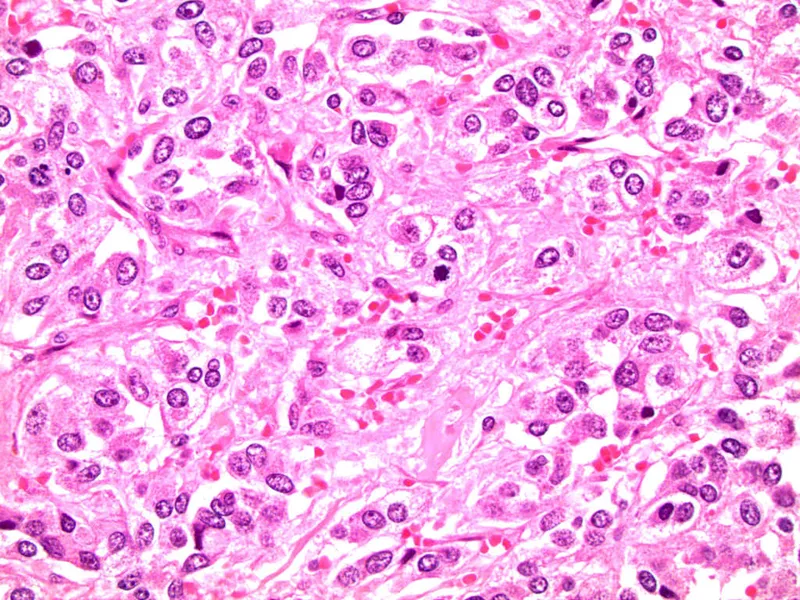
- The description of a mass with **clusters of chromaffin cells** is characteristic of a **pheochromocytoma**, a tumor typically arising from the **adrenal medulla**.
- **Pheochromocytomas** are known to secrete catecholamines, primarily **norepinephrine** and epinephrine.
*Aldosterone*
- **Aldosterone** is secreted by the **zona glomerulosa** of the **adrenal cortex** and is involved in blood pressure regulation.
- Tumors secreting aldosterone are usually **aldosteronomas** (Conn's syndrome) and do not arise from chromaffin cells.
*Dehydroepiandrosterone*
- **Dehydroepiandrosterone (DHEA)** is an **adrenal androgen** secreted by the **zona reticularis** of the adrenal cortex.
- Its secretion is associated with cortical tumors or hyperplasia, not chromaffin cell tumors.
*Cortisol*
- **Cortisol** is a glucocorticoid produced by the **zona fasciculata** of the **adrenal cortex**.
- Elevated cortisol levels are usually due to **Cushing's syndrome**, often caused by adrenal adenomas or hyperplasia, not chromaffin cell tumors.
*Estrogen*
- While small amounts of **estrogen** can be produced by the adrenal glands, the primary sites of estrogen synthesis are the **ovaries** and **placenta**.
- A tumor composed of **chromaffin cells** is not typically associated with significant estrogen secretion.
Pheochromocytoma resection US Medical PG Question 4: A 30-year-old man comes to the physician after receiving a high blood pressure reading of 160/90 mm Hg at an annual employee health check-up. During the past few months, the patient has had occasional headaches and mild abdominal pain, both of which were relieved with ibuprofen. He has also had several episodes of heart palpitations. He has no history of serious illness. His mother and father both have hypertension. He has smoked one pack of cigarettes daily for the past 10 years and drinks one glass of wine daily. He occasionally smokes marijuana. He appears pale. His temperature is 36.8°C (98.2°F), pulse is 103/min, and blood pressure is 164/102 mm Hg. Physical examination shows no abnormalities. Laboratory studies show:
Hemoglobin 15.3 g/dL
Leukocyte count 7,900/mm3
Platelet count 223,000/mm3
Serum
Na+ 138 mEq/L
K+ 4.6 mEq/L
Cl- 103 mEq/L
Urea nitrogen 14 mg/dL
Glucose 90 mg/dL
Creatinine 0.9 mg/dL
Plasma metanephrines 1.2 nmol/L (N < 0.5 nmol/L)
Urine toxicology screening is positive for tetrahydrocannabinol (THC). Renal doppler shows no abnormalities. A CT scan of the abdomen shows a mass in the left adrenal gland. Which of the following is the most appropriate next step in management of this patient?
- A. Resection of adrenal mass
- B. Phenoxybenzamine (Correct Answer)
- C. Propranolol
- D. Metoprolol
- E. MIBG therapy
Pheochromocytoma resection Explanation: ***Phenoxybenzamine***
- The patient's presentation with **hypertension**, **palpitations**, and significantly elevated **plasma metanephrines** (1.2 nmol/L vs. normal < 0.5 nmol/L), along with an **adrenal mass**, strongly suggests a **pheochromocytoma**.
- **Alpha-blockade** with phenoxybenzamine is the crucial first step to control blood pressure and prevent a **hypertensive crisis** during subsequent surgical resection.
*Resection of adrenal mass*
- While surgical resection is the **definitive treatment** for pheochromocytoma, it should **not be performed before adequate alpha-blockade**.
- **Unprepared surgery** can lead to a fatal hypertensive crisis due to uncontrolled catecholamine release during manipulation of the tumor.
*Propranolol*
- Propranolol is a **non-selective beta-blocker** and should **not be initiated before alpha-blockade** in pheochromocytoma.
- Blocking beta-adrenergic receptors can lead to **unopposed alpha-adrenergic vasoconstriction**, potentially worsening hypertension and causing a crisis.
*Metoprolol*
- Metoprolol is a **selective beta-1 blocker** and, like other beta-blockers, should **not be used before alpha-blockade** in pheochromocytoma.
- While it may have fewer peripheral vasoconstrictive effects than non-selective beta-blockers, the risk of unopposed alpha-stimulation remains significant.
*MIBG therapy*
- **Metaiodobenzylguanidine (MIBG) therapy** is a form of **radiotherapy** used for metastatic or inoperable pheochromocytoma/paraganglioma.
- It is **not the initial management** for a resectable adrenal mass in a patient with a newly diagnosed pheochromocytoma.
Pheochromocytoma resection US Medical PG Question 5: A 43-year-old male with a history of thyroid cancer status post total thyroidectomy presents to his primary care physician after repeated bouts of headaches. His headaches are preceded by periods of anxiety, palpitations, and sweating. The patient says he is unable to pinpoint any precipitating factors and instead says the events occur without warning. Of note, the patient's father and uncle also have a history of thyroid cancer. On exam his vitals are: T 36.8 HR 87, BP 135/93, RR 14, and O2 Sat 100% on room air. The patient's TSH is within normal limits, and he reports taking his levothyroxine as prescribed. What is the next best step in diagnosing this patient's chief complaint?
- A. 24-hour urine free cortisol
- B. Plasma aldosterone/renin ratio
- C. Abdominal CT scan with and without IV contrast
- D. Plasma fractionated metanephrines (Correct Answer)
- E. High dose dexamethasone suppression test
Pheochromocytoma resection Explanation: ***Plasma fractionated metanephrines***
- The patient's symptoms of **anxiety, palpitations, sweating, and headaches** occurring in discrete "attacks" are classic for a **pheochromocytoma**, a tumor that secretes catecholamines.
- Given the patient's and his family's history of **thyroid cancer**, specifically likely **medullary thyroid cancer** due to the familial link, there is a high suspicion for **Multiple Endocrine Neoplasia type 2 (MEN2)**, which commonly includes pheochromocytoma. **Plasma fractionated metanephrines** are the most sensitive screening test for pheochromocytoma.
*24-hour urine free cortisol*
- This test is used to detect **Cushing's syndrome**, which involves excessive cortisol production.
- Although Cushing's can cause **hypertension**, the paroxysmal symptoms of anxiety, palpitations, and sweating are not typical of Cushing's syndrome.
*Plasma aldosterone/renin ratio*
- This ratio is used to screen for **primary hyperaldosteronism**, a cause of secondary hypertension.
- While the patient has **hypertension (135/93 mm Hg)**, his symptom complex of episodic anxiety, palpitations, and sweating is not characteristic of primary hyperaldosteronism.
*Abdominal CT scan with and without IV contrast*
- An abdominal CT scan can visualize adrenal masses, but it is typically performed *after* biochemical confirmation of a pheochromocytoma to localize the tumor.
- Performing imaging before biochemical testing risks incidentalomas or missing a biochemically active but small tumor, and it is not the most appropriate *next step* in diagnosis given the strong clinical suspicion.
*High dose dexamethasone suppression test*
- This test is specifically used to differentiate between **Cushing's disease** (pituitary ACTH excess) and other causes of Cushing's syndrome.
- The patient's symptoms are not consistent with excessive cortisol production, making this test inappropriate for his chief complaint.
Pheochromocytoma resection US Medical PG Question 6: A 67-year-old woman with tertiary hyperparathyroidism and end-stage renal disease on hemodialysis has persistent hypercalcemia (calcium 12.8 mg/dL) despite maximal medical management with cinacalcet and vitamin D restriction. She has severe pruritus, calciphylaxis, and vascular calcifications. All four parathyroid glands are enlarged on imaging. Evaluate the optimal surgical strategy considering her complex medical status and need for ongoing dialysis access.
- A. Single adenoma resection guided by sestamibi
- B. Subtotal parathyroidectomy (3.5 gland resection)
- C. Total parathyroidectomy without autotransplantation
- D. Total parathyroidectomy with forearm autotransplantation (Correct Answer)
- E. Medical management escalation with denosumab
Pheochromocytoma resection Explanation: ***Total parathyroidectomy with forearm autotransplantation***
- In **tertiary hyperparathyroidism** with four-gland enlargement, this procedure provides definitive treatment while allowing for easier access if **recurrent hyperplasia** occurs.
- Placing the tissue in the **forearm** avoids risky neck re-explorations in the future and is the standard for patients who may remain on long-term dialysis.
*Single adenoma resection guided by sestamibi*
- This approach is inappropriate because **tertiary hyperparathyroidism** involves **multiglandular hyperplasia**, not a single solitary adenoma.
- Imaging with **sestamibi** is less reliable in renal patients, and leaving three hyperplastic glands would lead to surgical failure.
*Subtotal parathyroidectomy (3.5 gland resection)*
- While a valid option for some, it carries a higher risk of **persistent hypercalcemia** or recurrence within the neck remnant compared to total resection.
- In patients with **calciphylaxis** and severe symptoms, many surgeons prefer total resection to ensure immediate clearance of excess **parathyroid hormone**.
*Total parathyroidectomy without autotransplantation*
- This technique leads to permanent **hypoparathyroidism**, which is difficult to manage and can result in **adynamic bone disease**.
- It is generally reserved for patients who are not candidates for future transplantation and have severe, life-threatening **hypercalcemia** where no hormonal replacement is desired.
*Medical management escalation with denosumab*
- The patient has already failed **maximal medical management** including **cinacalcet**, and her severe **calciphylaxis** is a surgical emergency.
- **Denosumab** does not address the underlying autonomous parathyroid hyperplasia and is not a definitive treatment for **tertiary hyperparathyroidism**.
Pheochromocytoma resection US Medical PG Question 7: A 30-year-old man presents with a 6 cm adrenal mass discovered incidentally. Biochemical workup shows elevated 24-hour urine metanephrines and plasma free metanephrines. He also has elevated serum calcium, PTH, and a pancreatic head mass on CT. Genetic testing confirms MEN 2B syndrome. Evaluate the management priorities and sequencing of interventions.
- A. Simultaneous thyroidectomy and bilateral adrenalectomy
- B. Medical management of pheochromocytoma then parathyroidectomy
- C. Immediate thyroidectomy followed by staged procedures
- D. Adrenalectomy first, then thyroidectomy, then other tumors (Correct Answer)
- E. Pancreatic surgery first due to mass effect
Pheochromocytoma resection Explanation: ***Adrenalectomy first, then thyroidectomy, then other tumors***
- Prioritizing **pheochromocytoma** resection is critical to avoid a life-threatening **hypertensive crisis** during subsequent surgeries.
- Adequate medical preparation with **alpha-blockade** followed by beta-blockade is mandatory before any surgical intervention in these patients.
*Simultaneous thyroidectomy and bilateral adrenalectomy*
- Simultaneous procedures significantly increase **perioperative risk** and operative time without ensuring hemodynamic stability during the thyroid portion.
- Managing the **catecholamine surge** from a pheochromocytoma is safer when performed as a separate, initial stage.
*Medical management of pheochromocytoma then parathyroidectomy*
- While **alpha-blockade** is necessary, the question asks for the sequence of surgical interventions, where adrenalectomy must precede other operations.
- This patient presents with features suggestive of **MEN 2B**, which classically does not include hyperparathyroidism, unlike **MEN 1** or **MEN 2A**.
*Immediate thyroidectomy followed by staged procedures*
- Performing a **thyroidectomy** first is contraindicated because the stress of surgery and anesthesia can trigger a **pheochromocytoma crisis**.
- Even if medullary thyroid carcinoma is aggressive, the risk of immediate **intraoperative death** from pheochromocytoma takes precedence.
*Pancreatic surgery first due to mass effect*
- Although a **pancreatic head mass** is present (suggestive of MEN 1 overlap or separate pathology), it is not the immediate life-threatening priority.
- Operating on the pancreas before controlling and removing the **pheochromocytoma** exposes the patient to severe hemodynamic instability.
Pheochromocytoma resection US Medical PG Question 8: A 38-year-old woman with primary hyperparathyroidism (calcium 11.8 mg/dL, PTH 185 pg/mL) has negative sestamibi scan and ultrasound. She desires surgical cure and has no medical contraindications. She has a Z-score of -2.8 on DEXA scan and a history of recurrent kidney stones. Evaluate the surgical approach and expected outcomes.
- A. Defer surgery until localization studies are positive
- B. Bilateral neck exploration with identification of all four glands (Correct Answer)
- C. Minimally invasive parathyroidectomy of the largest gland
- D. Medical management with cinacalcet and bisphosphonates
- E. Intraoperative PTH-guided focused exploration
Pheochromocytoma resection Explanation: ***Bilateral neck exploration with identification of all four glands***
- When **preoperative localization** studies (Sestamibi and Ultrasound) are negative, a **bilateral neck exploration** is the gold standard to identify the source of primary hyperparathyroidism.
- This patient has clear indications for surgery including **nephrolithiasis**, a **Z-score of -2.8** (osteoporosis), and symptomatic hypercalcemia, making surgical intervention necessary despite negative imaging.
*Defer surgery until localization studies are positive*
- **Negative imaging** does not rule out primary hyperparathyroidism or contraindicate surgery when biochemical evidence is clear.
- Deferring treatment would risk further **bone loss** and recurrent **kidney stones** in a patient who already meets surgical criteria.
*Minimally invasive parathyroidectomy of the largest gland*
- **Minimally invasive parathyroidectomy (MIP)** requires precise preoperative localization to guide the surgeon to a specific quadrant.
- Attempting MIP without localization increases the risk of **surgical failure** and missing ectopic or multiglandular disease.
*Medical management with cinacalcet and bisphosphonates*
- **Medical management** is generally reserved for patients who are not surgical candidates or those who refuse surgery.
- While cinacalcet lowers **PTH** and calcium, it does not provide a **permanent cure** for the underlying adenoma or hyperplasia and is not the first-line choice for a young, fit patient.
*Intraoperative PTH-guided focused exploration*
- **Focused exploration** relies on knowing which side to explore first; without imaging, there is no target for a "focused" approach.
- While **intraoperative PTH** (ioPTH) monitoring is a useful adjunct to confirm cure, it does not replace the need for a comprehensive **bilateral search** when imaging is nonlocalizing.
Pheochromocytoma resection US Medical PG Question 9: A 55-year-old woman presents with a 4 cm thyroid nodule. FNA shows Hurthle cell neoplasm (follicular variant). Preoperative ultrasound shows no lymphadenopathy. She undergoes thyroid lobectomy, and final pathology reveals a 3.8 cm Hurthle cell carcinoma with capsular invasion but no vascular invasion. Analyze the pathology findings and determine the next step in management.
- A. Completion thyroidectomy within 2 weeks (Correct Answer)
- B. Radioactive iodine ablation without further surgery
- C. Observation with ultrasound surveillance every 6 months
- D. External beam radiation therapy
- E. Prophylactic modified radical neck dissection
Pheochromocytoma resection Explanation: ***Completion thyroidectomy within 2 weeks***
- For **Hurthle cell carcinoma** (HCC), a completion thyroidectomy is indicated when a malignancy is confirmed post-lobectomy, especially given HCC's aggressive nature and size approaching **4 cm**.
- Total thyroidectomy is necessary to facilitate future surveillance using **serum thyroglobulin** levels and to prepare for potential **radioactive iodine (RAI)** therapy if needed.
*Radioactive iodine ablation without further surgery*
- **Radioactive iodine (RAI)** therapy cannot be effectively performed if a remnant thyroid lobe is still present, as the normal tissue will sequester the iodine.
- **Hurthle cells** are historically less iodine-avid than other follicular cells, making surgical clearance of all thyroid tissue even more critical before considering RAI.
*Observation with ultrasound surveillance every 6 months*
- **Observation** is generally reserved for low-risk papillary microcarcinomas or minimally invasive follicular carcinomas <1-2 cm without high-risk features.
- The presence of **capsular invasion** and the histological subtype of **Hurthle cell carcinoma** in a 3.8 cm lesion represent a higher risk that mandates definitive surgical management.
*External beam radiation therapy*
- **External beam radiation** is not a primary treatment for localized Hurthle cell carcinoma and is typically reserved for **palliative care** or unresectable local recurrence.
- It does not replace the standard of care for surgical management of a resectable **thyroid malignancy**.
*Prophylactic modified radical neck dissection*
- **Prophylactic neck dissection** is not recommended for Hurthle cell carcinoma because it primarily spreads **hematogenously** rather than through lymphatic channels.
- Surgical management of the neck is only indicated if there is clinical or radiological evidence of **cervical lymphadenopathy**, which was absent in this patient.
Pheochromocytoma resection US Medical PG Question 10: A 42-year-old woman with a family history of pheochromocytoma undergoes resection of a 5 cm right adrenal mass. Preoperatively, she was adequately alpha-blocked with phenoxybenzamine. During tumor manipulation, her blood pressure rises to 220/130 mmHg despite anesthesia deepening. Immediately after tumor removal, her blood pressure drops to 70/40 mmHg. Analyze the hemodynamic changes and determine management priorities.
- A. Immediate aggressive fluid resuscitation and vasopressors
- B. Continue phenoxybenzamine and observe
- C. Administer phentolamine for hypertensive crisis
- D. Emergency re-exploration for bleeding
- E. Decrease anesthesia depth and give beta-blockers
Pheochromocytoma resection Explanation: ***Immediate aggressive fluid resuscitation and vasopressors***
- Sudden **hypotension** after tumor removal occurs because the body is no longer receiving the massive surge of **catecholamines** while existing **alpha-blockade** (phenoxybenzamine) persists.
- Management requires **large-volume intravenous fluids** to address pre-existing **volume depletion** and vasopressors to maintain mean arterial pressure until the vascular tone is restored.
*Continue phenoxybenzamine and observe*
- Phenoxybenzamine is a **non-competitive alpha-antagonist** used preoperatively to control hypertension; it has a long half-life and cannot be reversed quickly.
- Continuing observation without intervention in a patient with a blood pressure of **70/40 mmHg** would lead to organ malperfusion and **cardiovascular collapse**.
*Administer phentolamine for hypertensive crisis*
- Phentolamine is appropriate for managing the **intraoperative hypertensive surge** caused by tumor manipulation, but it is contraindicated once the patient is hypotensive.
- Giving a vasodilator during the post-resection **hypotensive phase** would exacerbate the low blood pressure and worsen the clinical state.
*Emergency re-exploration for bleeding*
- Although postoperative hemorrhage is a concern, the timing of this collapse matches the **physiologic withdrawal** of catecholamines precisely upon ligation of the adrenal vein.
- Hemodynamic instability should first be treated with **fluid boluses** and pressors; surgical re-exploration is reserved for confirmed cases of **hemoperitoneum**.
*Decrease anesthesia depth and give beta-blockers*
- Decreasing anesthesia depth may help slightly with blood pressure but is insufficient to counteract the loss of **endogenous vasopressors**.
- Giving **beta-blockers** in the setting of hypotension is dangerous as it reduces **cardiac output** and compensatory tachycardia, further decreasing blood pressure.
More Pheochromocytoma resection US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.