Parathyroidectomy procedures US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Parathyroidectomy procedures. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Parathyroidectomy procedures US Medical PG Question 1: A 45-year-old man undergoes a parathyroidectomy given recurrent episodes of dehydration and kidney stones caused by hypercalcemia secondary to an elevated PTH level. He is recovering on the surgical floor on day 3. His temperature is 97.6°F (36.4°C), blood pressure is 122/81 mmHg, pulse is 84/min, respirations are 12/min, and oxygen saturation is 98% on room air. The patient is complaining of perioral numbness currently. What is the most appropriate management of this patient?
- A. Potassium
- B. TSH level
- C. Vitamin D
- D. Observation
- E. Calcium gluconate (Correct Answer)
Parathyroidectomy procedures Explanation: ***Calcium gluconate***
- The patient's presentation of **perioral numbness** following a parathyroidectomy, especially given a history of hypercalcemia, is highly suggestive of **hypocalcemia**.
- **Calcium gluconate** is indicated for acute symptomatic hypocalcemia to rapidly raise serum calcium levels and alleviate symptoms.
*Potassium*
- There is no clinical indication for **potassium** supplementation; the symptom of perioral numbness is not associated with potassium imbalance.
- Parathyroidectomy and hypercalcemia primarily affect calcium and phosphate metabolism, not typically potassium.
*TSH level*
- A **TSH level** is used to assess thyroid function, which is generally not directly affected by parathyroidectomy unless thyroid tissue was incidentally damaged.
- The symptoms presented do not suggest a thyroid dysfunction.
*Vitamin D*
- While **vitamin D** is crucial for calcium absorption and might be used in chronic management of hypocalcemia, it would not provide the immediate relief needed for acute symptomatic hypocalcemia.
- Acute symptoms like perioral numbness require a rapid elevation of serum calcium.
*Observation*
- **Observation** is inappropriate given the patient's symptomatic presentation of **perioral numbness**, which indicates acute and potentially worsening hypocalcemia.
- Untreated symptomatic hypocalcemia can progress to more severe complications such as seizures, arrhythmias, and laryngospasm.
Parathyroidectomy procedures US Medical PG Question 2: A 35-year-old man comes to the physician for evaluation of a neck mass and hoarseness. He has no history of major medical illness. Physical examination shows a 2.5-cm fixed, irregular thyroid nodule. His serum calcitonin concentration is elevated. The nodule is most likely comprised of cells that are embryologically derived from which of the following structures?
- A. Second branchial pouch
- B. Fourth branchial arch
- C. Surface ectoderm
- D. Third branchial pouch
- E. Neural crest cells (Correct Answer)
Parathyroidectomy procedures Explanation: ***Neural crest cells***
- The elevated **serum calcitonin** in the presence of a thyroid nodule is highly suggestive of **medullary thyroid carcinoma (MTC)**.
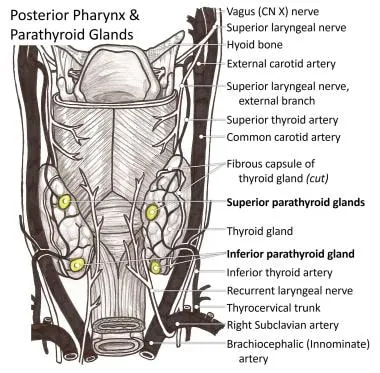
- **MTC** originates from the **parafollicular C cells** of the thyroid, which are embryologically derived from **neural crest cells** that migrate to the **ultimobranchial body** (from the 4th/5th pharyngeal pouch) during development and subsequently integrate into the thyroid gland.
- This is the definitive embryological origin of calcitonin-producing C cells.
*Second branchial pouch*
- The second branchial pouch typically gives rise to the **palatine tonsil crypts** and **tonsillar fossa**.
- It is not associated with the development of the **parafollicular C cells** or thyroid malignancies.
*Fourth branchial arch*
- The fourth branchial arch gives rise to the **superior laryngeal nerve** and associated laryngeal cartilages.
- While the **ultimobranchial body** (from the 4th/5th pharyngeal pouch) does contribute C cells to the thyroid, these cells themselves are derived from **neural crest cells** that migrate to this structure, not from the pouch itself.
- Therefore, the embryological origin is neural crest, not the branchial arch/pouch.
*Surface ectoderm*
- Surface ectoderm forms structures such as the **epidermis of the skin**, **hair**, **nails**, and **lens of the eye**.
- It does not contribute to the development of the **C cells** or the thyroid gland.
*Third branchial pouch*
- The third branchial pouch gives rise to the **inferior parathyroid glands** and the majority of the **thymus**.
- While it contributes to endocrine tissues, it does not form the **parafollicular C cells** of the thyroid.
Parathyroidectomy procedures US Medical PG Question 3: A 50-year-old man undergoes parathyroidectomy for treatment-resistant hyperparathyroidism. The procedure is complicated by brisk bleeding from the superior thyroid artery near the external branch of the superior laryngeal nerve. To stop the bleeding, the artery is ligated at its origin. Which of the following is most likely the origin of the artery that was injured in this patient?
- A. Thyrocervical trunk
- B. Ascending pharyngeal artery
- C. Internal carotid artery
- D. Subclavian artery
- E. External carotid artery (Correct Answer)
Parathyroidectomy procedures Explanation: ***External carotid artery***
- The **superior thyroid artery** is the first branch to arise from the **external carotid artery** in the neck.
- Ligation of this artery at its origin is a common surgical maneuver to control bleeding during thyroid or parathyroid surgery.
*Thyrocervical trunk*
- The **thyrocervical trunk** is a branch of the **subclavian artery** and gives rise to the inferior thyroid artery, not the superior thyroid artery.
- Injury to the superior thyroid artery would not necessitate ligation of a vessel originating from the thyrocervical trunk.
*Ascending pharyngeal artery*
- The **ascending pharyngeal artery** is a small artery that branches from the **external carotid artery** but supplies the pharynx, not the thyroid gland.
- It is not typically implicated in bleeding during parathyroidectomy or in relation to the superior laryngeal nerve.
*Internal carotid artery*
- The **internal carotid artery** primarily supplies the brain and does not have branches in the neck that supply the thyroid or parathyroid glands.
- It arises from the common carotid artery but does not give off the superior thyroid artery.
*Subclavian artery*
- The **subclavian artery** gives rise to the **thyrocervical trunk**, which then supplies the inferior thyroid artery, but not directly the superior thyroid artery.
- The superior thyroid artery originates higher up from the external carotid artery.
Parathyroidectomy procedures US Medical PG Question 4: A 72-year-old woman with a medical history significant for chronic kidney disease stage 4, hypertension, and type 2 diabetes mellitus, presents to the office for a scheduled visit. During her last visit, the physician started discussing with her the possibility of starting her on dialysis for her chronic kidney disease. The patient has no complaints about her health and enjoys spending time with her family. At presentation, she is afebrile; the blood pressure is 139/89 mm Hg and the heart rate is 80/min. On physical examination, her pulses are bounding, the complexion is pale, she has a grade ⅙ holosystolic murmur, breath sounds remain clear, and 2+ pedal edema to the knee. The measurement of which of the following laboratory values is most appropriate to screen for renal osteodystrophy in this patient?
- A. Erythrocyte sedimentation rate
- B. Serum vitamin B-12 level
- C. Serum C-reactive protein level
- D. Serum thyroid-stimulating hormone level
- E. Serum intact parathyroid hormone level (Correct Answer)
Parathyroidectomy procedures Explanation: ***Serum intact parathyroid hormone level***
- **Renal osteodystrophy**, a common complication of **chronic kidney disease (CKD)** stage 4 and 5, is primarily caused by secondary hyperparathyroidism.
- **Intact parathyroid hormone (iPTH)** is critical in diagnosing and monitoring this condition, as elevated levels indicate impaired mineral and bone metabolism due to failing kidneys.
*Erythrocyte sedimentation rate*
- **Erythrocyte sedimentation rate (ESR)** is a general marker of inflammation and is not specific for renal osteodystrophy.
- While CKD can be associated with inflammation, ESR does not directly assess mineral and bone disorders.
*Serum vitamin B-12 level*
- **Vitamin B-12** deficiency can cause anemia and neurological symptoms, but it is not directly involved in the pathogenesis or diagnosis of renal osteodystrophy.
- This test would be more relevant if the patient presented with symptoms of **pernicious anemia** or neuropathy.
*Serum C-reactive protein level*
- **C-reactive protein (CRP)**, like ESR, is a general **inflammatory marker** and does not provide specific information about bone health or mineral metabolism in CKD.
- High CRP levels might indicate infection or systemic inflammation but are not used to screen for renal osteodystrophy.
*Serum thyroid-stimulating hormone level*
- **Thyroid-stimulating hormone (TSH)** assesses **thyroid function**, which is distinct from renal osteodystrophy.
- Thyroid disorders can impact bone health, but TSH is not the primary screening test for bone disease related to CKD.
Parathyroidectomy procedures US Medical PG Question 5: Three hours after undergoing a total right hip replacement, a 71-year-old woman has tingling around the lips and numbness in her fingertips. Her surgery was complicated by unintentional laceration of the right femoral artery that resulted in profuse bleeding. She appears uncomfortable. Examination shows an adducted thumb, extended fingers, and flexed metacarpophalangeal joints and wrists. Tapping on the cheeks leads to contraction of the facial muscles. Which of the following is the most likely cause of this patient's symptoms?
- A. Acute kidney injury
- B. Parathyroid ischemia
- C. Intravascular hemolysis
- D. Calcium chelation (Correct Answer)
- E. Metabolic acidosis
Parathyroidectomy procedures Explanation: ***Calcium chelation***
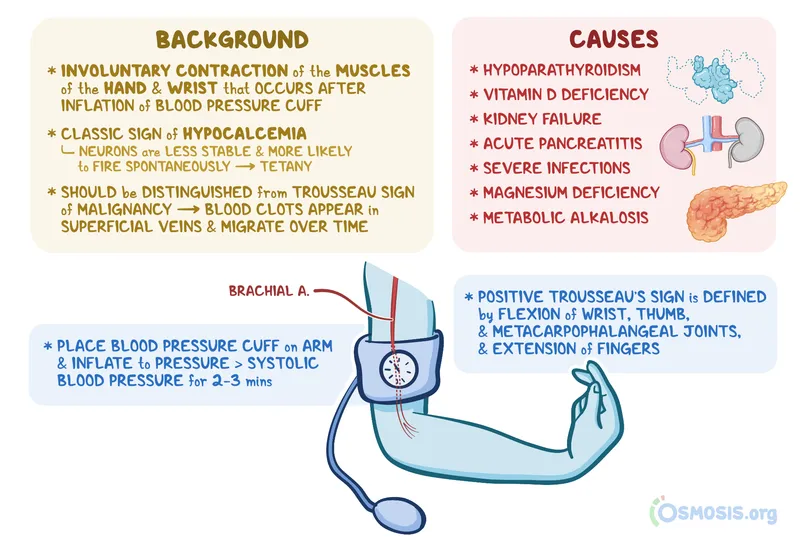
- The patient exhibits symptoms of **hypocalcemia**, including perioral tingling, fingertip numbness, **Trousseau sign** (adducted thumb, extended fingers, flexed metacarpophalangeal joints and wrists), and **Chvostek's sign** (facial muscle contraction upon tapping the cheek).
- Her significant blood loss and subsequent transfusion likely involved large volumes of **citrated blood products** (e.g., packed red blood cells), where citrate acts as an **anticoagulant** by chelating calcium, leading to transient hypocalcemia.
*Acute kidney injury*
- While acute kidney injury can cause electrolyte imbalances, it typically leads to **hyperphosphatemia**, not necessarily acute symptomatic hypocalcemia presenting within hours of surgery in this manner.
- The patient's immediate post-operative presentation points away from kidney injury being the primary cause of these acute neurological symptoms.
*Parathyroid ischemia*
- **Parathyroid ischemia** could cause hypocalcemia due to reduced parathyroid hormone production, but it is typically associated with **neck surgeries** (e.g., thyroidectomy) and not directly with hip replacement or arterial laceration.
- The onset of symptoms within hours of surgery is too rapid for parathyroid ischemia to fully manifest, as the half-life of PTH is short, but the subsequent drop in calcium would take longer to become clinically significant.
*Intravascular hemolysis*
- **Intravascular hemolysis** can occur due to transfusion reactions or other causes, leading to symptoms like fever, chills, and hemoglobinuria.
- It does not directly cause the specific neurological signs of hypocalcemia described (Trousseau's and Chvostek's signs).
*Metabolic acidosis*
- **Metabolic acidosis** can alter calcium binding to albumin, leading to an **increase in ionized calcium** (the physiologically active form), rather than a decrease.
- While acidosis can occur after massive blood loss and shock, it would not explain the classic signs of hypocalcemia.
Parathyroidectomy procedures US Medical PG Question 6: A 28-year-old man comes to the physician for a follow-up examination after a previous visit showed an elevated serum calcium level. He has a history of bipolar disorder. His mother had a parathyroidectomy in her 30s. The patient does not drink alcohol or smoke. Current medications include lithium and a daily multivitamin. His vital signs are within normal limits. Physical examination shows no abnormalities. Laboratory studies show:
Serum
Sodium 146 mEq/L
Potassium 3.7 mEq/L
Calcium 11.2 mg/dL
Magnesium 2.3 mEq/L
PTH 610 pg/mL
Albumin 4.2 g/dL
24-hour urine
Calcium 23 mg
Which of the following is the most likely cause of this patient’s findings?
- A. Lithium toxicity
- B. Parathyroid adenoma
- C. Excess calcium intake
- D. Excess vitamin D intake
- E. Abnormal calcium sensing receptors (Correct Answer)
Parathyroidectomy procedures Explanation: ***Abnormal calcium sensing receptors***
- The patient's **hypocalciuric hypercalcemia** (high serum calcium, low urine calcium) in the presence of an **elevated PTH** suggests a defect in calcium sensing.
- The family history of parathyroidectomy in the mother is consistent with an inherited condition affecting **calcium-sensing receptors (CaSRs)**, such as **familial hypocalciuric hypercalcemia (FHH)**.
*Lithium toxicity*
- **Lithium** can cause hypercalcemia by increasing the set point for calcium at the parathyroid gland, leading to increased PTH secretion.
- However, lithium typically does not lead to **hypocalciuria** to the extent seen in FHH, as it does not directly affect the kidney's CaSR in the same manner.
*Parathyroid adenoma*
- A **parathyroid adenoma** would cause **primary hyperparathyroidism**, characterized by hypercalcemia and elevated PTH.
- However, primary hyperparathyroidism typically presents with **hypercalciuria** due to the PTH-mediated increase in renal calcium reabsorption being overwhelmed by the increased filtered calcium load, unlike the hypocalciuria seen here.
*Excess calcium intake*
- **Excess calcium intake** could lead to hypercalcemia, but this would typically suppress PTH (unless it's a milk-alkali syndrome variant).
- It would also lead to **hypercalciuria** as the kidneys attempt to excrete the excess calcium, which is not observed here with a suppressed 24-hour urine calcium.
*Excess vitamin D intake*
- **Excess vitamin D intake** causes hypercalcemia by increasing intestinal calcium absorption and bone resorption, and would typically lead to **suppressed PTH** levels.
- It would also typically result in **hypercalciuria** due to the increased filtered calcium load, contrasting with the low urine calcium in this patient.
Parathyroidectomy procedures US Medical PG Question 7: A 75-year-old man is referred for thyroidectomy for treatment of thyroid nodules. A portion of the thyroid gland is resected, and the neck is closed with sutures. After awakening from anesthesia, the patient complains of ‘hoarseness’. His vital signs are normal and his incisional pain is minimal. The surgeon realizes he most likely damaged the recurrent laryngeal nerve. Which of the following should the surgeon tell the patient?
- A. "A mistake occurred during the operation, but there was no harm to you."
- B. "We made a mistake during the operation that may have harmed you." (Correct Answer)
- C. "The case took longer than we thought it would, but everything went well."
- D. "A mistake occurred because this hospital has poor operating room protocols."
- E. "The operation was successful and no complications occurred."
Parathyroidectomy procedures Explanation: ***\"We made a mistake during the operation that may have harmed you.\"***
- This statement accurately reflects the situation, acknowledging both the **mistake** and the potential **harm** to the patient (hoarseness due to recurrent laryngeal nerve damage).
- Open communication and honesty about medical errors are essential for maintaining **trust** and fulfilling ethical obligations to the patient.
*\"A mistake occurred during the operation, but there was no harm to you.\"*
- This statement is inaccurate because the patient is experiencing **hoarseness**, which is a sign of harm (recurrent laryngeal nerve damage).
- Dismissing the patient's symptom as "no harm" is **dishonest** and undermines trust.
*\"The case took longer than we thought it would, but everything went well.\"*
- This statement is misleading as it downplays a significant complication (recurrent laryngeal nerve damage) by implying that "everything went well" despite the patient's hoarseness.
- It avoids addressing the specific concern and does not acknowledge any **error** or **harm**.
*\"A mistake occurred because this hospital has poor operating room protocols.\"*
- While a mistake may have occurred, blaming the hospital's protocols is an attempt to deflect personal responsibility and can be seen as unprofessional.
- This statement introduces a potentially contentious issue that should be addressed internally rather than with the patient when disclosing the error.
*\"The operation was successful and no complications occurred.\"*
- This statement is explicitly false, as **hoarseness** due to recurrent laryngeal nerve damage is a direct and recognized **complication** of thyroidectomy.
- Making such a claim is unethical and violates the principle of **informed consent** and truthful disclosure.
Parathyroidectomy procedures US Medical PG Question 8: An obese 52-year-old man is brought to the emergency department because of increasing shortness of breath for the past 8 hours. Two months ago, he noticed a mass on the right side of his neck and was diagnosed with laryngeal cancer. He has smoked two packs of cigarettes daily for 27 years. He drinks two pints of rum daily. He appears ill. He is oriented to person, place, and time. His temperature is 37°C (98.6°F), pulse is 111/min, respirations are 34/min, and blood pressure is 140/90 mm Hg. Pulse oximetry on room air shows an oxygen saturation of 89%. Examination shows a 9-cm, tender, firm subglottic mass on the right side of the neck. Cervical lymphadenopathy is present. His breathing is labored and he has audible inspiratory stridor but is able to answer questions. The lungs are clear to auscultation. Arterial blood gas analysis on room air shows:
pH 7.36
PCO2 45 mm Hg
PO2 74 mm Hg
HCO3- 25 mEq/L
He has no advanced directive. Which of the following is the most appropriate next step in management?
- A. Comfort care measures
- B. Cricothyroidotomy (Correct Answer)
- C. Tracheostomy
- D. Intramuscular epinephrine
- E. Tracheal stenting
Parathyroidectomy procedures Explanation: ***Correct: Cricothyroidotomy***
- This patient has **impending complete airway obstruction** evidenced by inspiratory stridor, severe tachypnea (34/min), hypoxia (O2 sat 89%), and a large obstructing laryngeal mass
- **Cricothyroidotomy** is the emergent surgical airway procedure of choice when there is **imminent or actual complete upper airway obstruction** and endotracheal intubation cannot be safely performed
- The subglottic mass makes endotracheal intubation **extremely dangerous** - instrumentation could precipitate complete obstruction and inability to ventilate
- Cricothyroidotomy provides **immediate airway access** (can be performed in 30-60 seconds) below the level of obstruction, making it life-saving in this emergency
- In the "cannot intubate, cannot ventilate" scenario, cricothyroidotomy is the definitive emergency intervention per ATLS and airway management guidelines
*Incorrect: Tracheostomy*
- While tracheostomy provides definitive airway management, it is a **controlled, elective procedure** typically performed in the OR that takes 20-30 minutes
- This patient requires **immediate airway access** - waiting for OR setup and performing tracheostomy risks complete airway collapse and death
- Tracheostomy may be performed later as a planned procedure once the airway is secured with cricothyroidotomy
- The presence of stridor indicates **critical airway narrowing** requiring emergency intervention, not elective surgery
*Incorrect: Comfort care measures*
- The patient is **alert and oriented** without an advanced directive indicating wishes for comfort care only
- This is an **acute, reversible condition** with appropriate emergency airway intervention
- Presumed consent applies in life-threatening emergencies when the patient cannot formally consent but intervention would be life-saving
- Comfort care would be inappropriate without documented patient wishes or irreversible terminal condition
*Incorrect: Intramuscular epinephrine*
- Epinephrine is indicated for **anaphylaxis** or angioedema causing airway edema from allergic/inflammatory mechanisms
- This patient has **mechanical obstruction** from a solid tumor mass, which will not respond to epinephrine
- Epinephrine causes vasoconstriction and reduces mucosal edema but cannot reduce tumor mass
- Would delay definitive airway management and not address the underlying problem
*Incorrect: Tracheal stenting*
- Tracheal stenting requires **bronchoscopy** in a controlled setting and is used for palliation of tracheal narrowing
- Cannot be performed emergently in an unstable patient with impending airway obstruction
- The obstruction is at the **laryngeal/subglottic level**, not typically amenable to emergency stenting
- Requires time for procedure setup and sedation, which this patient cannot afford given the critical airway emergency
Parathyroidectomy procedures US Medical PG Question 9: A 79-year-old man is admitted to the intensive care unit for hospital acquired pneumonia, a COPD flare, and acute heart failure requiring intubation and mechanical ventilation. On his first night in the intensive care unit, his temperature is 99.7°F (37.6°C), blood pressure is 107/58 mm Hg, and pulse is 150/min which is a sudden change from his previous vitals. Physical exam is notable for jugular venous distension and a rapid heart rate. The ventilator is checked and is functioning normally. Which of the following is the best next step in management for the most likely diagnosis?
- A. Tube thoracostomy
- B. FAST exam
- C. Needle thoracostomy (Correct Answer)
- D. Chest radiograph
- E. Thoracotomy
Parathyroidectomy procedures Explanation: ***Needle thoracostomy***
- The patient's sudden deterioration with **tachycardia**, **hypotension**, and **jugular venous distension** (JVD) in the setting of positive pressure ventilation strongly suggests a **tension pneumothorax**.
- **Needle decompression** is the immediate life-saving intervention for suspected tension pneumothorax, as delaying treatment for diagnostic imaging could be fatal.
*Tube thoracostomy*
- While a **tube thoracostomy** (chest tube insertion) is the definitive treatment for pneumothorax, it requires more time and resources than needle decompression.
- In a true emergency with signs of tension, needle decompression should be performed first to stabilize the patient, followed by a chest tube.
*FAST exam*
- A **Focused Assessment with Sonography for Trauma (FAST) exam** is primarily used to detect free fluid (usually blood) in the abdomen or pericardium in trauma patients.
- While it can sometimes identify pneumothorax, it is not the fastest or most direct intervention for a suspected tension pneumothorax causing hemodynamic instability.
*Chest radiograph*
- A **chest radiograph (CXR)** is the standard diagnostic tool for pneumothorax, but obtaining and interpreting it would delay urgent intervention in a hemodynamically unstable patient with suspected tension pneumothorax.
- The diagnosis of tension pneumothorax is primarily clinical; treatment should not wait for imaging.
*Thoracotomy*
- A **thoracotomy** is a major surgical procedure involving opening the chest, typically reserved for severe trauma, massive hemorrhage, or complex thoracic issues.
- It is an overly aggressive and inappropriate initial intervention for a suspected tension pneumothorax.
Parathyroidectomy procedures US Medical PG Question 10: A 27-year-old man presents to the emergency department with severe dyspnea and sharp chest pain that suddenly started an hour ago after he finished exercising. He has a history of asthma as a child, and he achieves good control of his acute attacks with Ventolin. On examination, his right lung field is hyperresonant along with diminished lung sounds. Chest wall motion during respiration is asymmetrical. His blood pressure is 105/67 mm Hg, respirations are 22/min, pulse is 78/min, and temperature is 36.7°C (98.0°F). The patient is supported with oxygen, given corticosteroids, and has had analgesic medications via a nebulizer. Considering the likely condition affecting this patient, what is the best step in management?
- A. CT scan
- B. ABG
- C. Chest X-rays (Correct Answer)
- D. Tube insertion
- E. Sonogram
Parathyroidectomy procedures Explanation: ***Chest X-rays***
- The patient's presentation with **sudden onset dyspnea** and **sharp chest pain** post-exercise, along with **hyperresonance** and **diminished lung sounds** in the right lung field, is highly suggestive of a **spontaneous pneumothorax**.
- However, the patient is **hemodynamically stable** (BP 105/67, HR 78/min) with no signs of tension physiology (no severe hypotension, marked tachycardia, or cardiovascular collapse).
- In a stable patient with suspected pneumothorax, **chest X-ray is the appropriate first step** to confirm the diagnosis, determine the size of the pneumothorax, and guide subsequent management (observation for small pneumothorax <20%, aspiration, or tube thoracostomy for larger pneumothoraces).
- Immediate intervention without imaging is reserved for unstable patients with tension pneumothorax.
*Tube insertion*
- Chest tube insertion is the definitive treatment for large pneumothoraces (>20%) or hemodynamically unstable patients with tension pneumothorax.
- In this **stable patient**, proceeding directly to tube insertion without imaging confirmation would be premature and not following standard of care.
- The diagnosis should be confirmed and the size estimated via chest X-ray before determining if tube thoracostomy is necessary.
*CT scan*
- CT scan is not indicated as the initial diagnostic test for suspected pneumothorax.
- It provides more detail than needed for this clinical scenario and causes unnecessary delay and radiation exposure when chest X-ray is sufficient.
- CT may be useful for detecting small pneumothoraces not visible on X-ray or evaluating underlying lung disease, but is not the first-line test.
*ABG*
- An Arterial Blood Gas (ABG) might show hypoxia and respiratory alkalosis, providing information about gas exchange.
- However, ABG does not confirm the diagnosis of pneumothorax or guide immediate management decisions.
- It is an adjunctive test that does not take priority over diagnostic imaging in this scenario.
*Sonogram*
- Lung ultrasound can rapidly detect pneumothorax by showing absent lung sliding and is increasingly used in emergency settings, particularly for bedside evaluation.
- While potentially useful, **chest X-ray remains the standard initial imaging modality** for suspected pneumothorax in most emergency departments, as it provides clear documentation of pneumothorax size and is more universally available and interpreted.
- Ultrasound may be preferred in specific situations (unstable patients, point-of-care evaluation), but chest X-ray is the conventional first-line imaging test.
More Parathyroidectomy procedures US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.