Multiple endocrine neoplasia syndromes US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Multiple endocrine neoplasia syndromes. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Multiple endocrine neoplasia syndromes US Medical PG Question 1: A 27-year-old man comes to the physician because of worsening abdominal pain over the last several months. He has also had recent feelings of sadness and a lack of motivation at work, where he is employed as a computer programmer. He denies suicidal thoughts. He has a history of multiple kidney stones. He has a family history of thyroid cancer in his father and uncle, who both underwent thyroidectomy before age 30. His temperature is 37°C (98°F), blood pressure is 138/86 mm Hg, and pulse is 87/min. Physical examination shows diffuse tenderness over the abdomen and obesity but is otherwise unremarkable. Serum studies show:
Na+ 141 mEq/L
K+ 3.6 mEq/L
Glucose 144 mg/dL
Ca2+ 12.1 mg/dL
Albumin 4.1 g/dL
PTH 226 pg/mL (normal range 12–88 pg/mL)
Results of a RET gene test return abnormal. The physician refers him to an endocrine surgeon. Which of the following is the most appropriate next step in diagnosis?
- A. Thyroidectomy
- B. Urine 5-HIAA
- C. Urine metanephrines (Correct Answer)
- D. Midnight salivary cortisol
- E. Serum gastrin
Multiple endocrine neoplasia syndromes Explanation: ***Urine metanephrines***
- The patient's presentation, including **abdominal pain**, **constipation** (implied by pain, mood changes, and high calcium), **hypertension**, **hypercalcemia** with **elevated PTH**, and a family history of **thyroid cancer** with an **abnormal RET gene test**, is highly suggestive of **MEN 2A** (Multiple Endocrine Neoplasia type 2A).
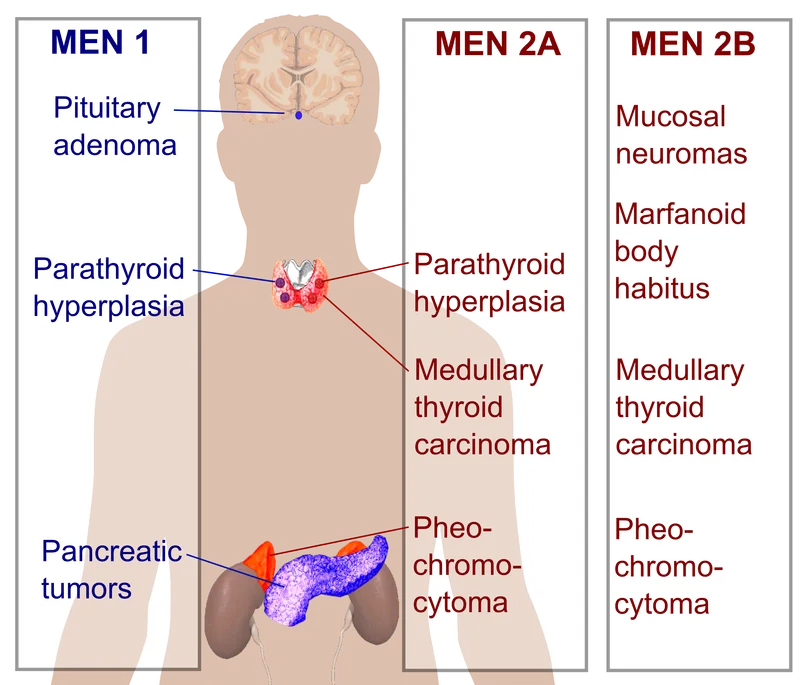
- **MEN 2A** is characterized by **medullary thyroid carcinoma** (MTC), **pheochromocytoma**, and **primary hyperparathyroidism**. Given the strong suspicion of MEN 2A and the presence of hypertension, screening for **pheochromocytoma** with **urine metanephrines** is crucial before any surgical intervention (e.g., thyroidectomy) due to the risk of a hypertensive crisis.
*Thyroidectomy*
- While a **thyroidectomy** is indicated for **medullary thyroid carcinoma** (strongly suggested by the family history of thyroid cancer and abnormal RET gene), it should **not be the immediate next step** before ruling out **pheochromocytoma**.
- Performing a thyroidectomy in a patient with an undiagnosed pheochromocytoma can lead to a **life-threatening hypertensive crisis** during surgery.
*Urine 5-HIAA*
- **Urine 5-HIAA** (5-hydroxyindoleacetic acid) is a test for **carcinoid syndrome**, which presents with flushing, diarrhea, and bronchospasm.
- These symptoms are **not consistent** with the patient's presentation, and carcinoid syndrome is **not a component of MEN 2A**.
*Midnight salivary cortisol*
- **Midnight salivary cortisol** is used to screen for **Cushing's syndrome**, which is characterized by symptoms such as central obesity, moon facies, striae, and muscle weakness.
- While the patient is obese, his other symptoms and laboratory findings are **not suggestive of Cushing's syndrome**, and it is not typically associated with MEN 2A.
*Serum gastrin*
- **Serum gastrin** levels are measured to diagnose **Zollinger-Ellison syndrome**, characterized by severe peptic ulcer disease and diarrhea due to a gastrinoma.
- While gastrinomas can occur in **MEN 1**, they are **not a feature of MEN 2A**, and the patient's symptoms are more consistent with other endocrine dysfunctions.
Multiple endocrine neoplasia syndromes US Medical PG Question 2: A 16-year-old boy is brought to the emergency department after losing consciousness. He had no preceding chest pain or palpitations. His father has cataracts and had frontal balding in his twenties but has no history of cardiac disease. His paternal grandfather also had early-onset balding. His pulse is 43/min. Physical examination shows frontal hair loss, temporal muscle wasting, and testicular atrophy. Neurologic examination shows bilateral foot drop and weakness of the intrinsic hand muscles. An ECG shows bradycardia with third-degree atrioventricular block. The severity of this patient's symptoms compared to that of his father is most likely due to which of the following genetic properties?
- A. Penetrance
- B. Codominance
- C. Anticipation (Correct Answer)
- D. Loss of heterozygosity
- E. Pleiotropy
Multiple endocrine neoplasia syndromes Explanation: ***Anticipation***
- **Anticipation** describes a genetic phenomenon where the severity of a genetic disorder increases and/or the age of onset decreases in successive generations. This is typical of disorders caused by **trinucleotide repeat expansions**, such as myotonic dystrophy.
- The patient's severe symptoms (third-degree AV block, foot drop, muscle wasting) occurring at a young age, compared to his father's milder symptoms (cataracts, early balding) without cardiac disease, are a classic presentation of anticipation in **myotonic dystrophy type 1 (DM1)**.
*Penetrance*
- **Penetrance** refers to the proportion of individuals with a particular genotype that express the associated phenotype.
- While it explains whether or not a trait is expressed, it does not explain the increasing severity or earlier onset across generations.
*Codominance*
- **Codominance** occurs when two different alleles for a gene are both expressed, and both phenotypes are observable (e.g., AB blood type).
- This concept does not apply to the increasing severity or earlier onset of symptoms observed in this family.
*Loss of heterozygosity*
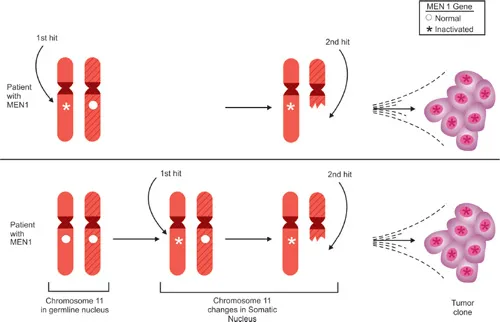
- **Loss of heterozygosity** is a genetic event where an individual inheriting one mutated allele for a tumor suppressor gene loses the normal allele, leading to disease (e.g., retinoblastoma).
- This mechanism primarily relates to tumor formation and is not relevant to the progressive worsening of symptoms across generations in the context of myotonic dystrophy.
*Pleiotropy*
- **Pleiotropy** refers to a single gene affecting multiple phenotypic traits (e.g., the FBN1 gene in Marfan syndrome affecting skeletal, ocular, and cardiovascular systems).
- While myotonic dystrophy exhibits pleiotropy (affecting multiple systems), pleiotropy itself does not explain the intergenerational increase in severity or decrease in age of onset, which is specifically attributed to anticipation.
Multiple endocrine neoplasia syndromes US Medical PG Question 3: A 30-year-old man presents to his primary care physician for a routine check-up. During the appointment, he remarks that he has started noticing some thinning and hair loss without other symptoms. The physician reassures him that he is likely experiencing male-pattern baldness and explains that the condition is largely inherited. Specifically he notes that there are multiple genes that are responsible for the condition so it is difficult to predict the timing and development of hair loss. What genetic principle is being illustrated by this scenario?
- A. Uniparental disomy
- B. Polygenic inheritance (Correct Answer)
- C. Pleiotropy
- D. Anticipation
- E. Heteroplasmy
Multiple endocrine neoplasia syndromes Explanation: ***Polygenic inheritance***
- This scenario describes male-pattern baldness as being influenced by **multiple genes**, which is the definition of polygenic inheritance.
- The difficulty in predicting the timing and development of hair loss further supports polygenic inheritance, as the combined effect of several genes and environmental factors can lead to a **continuous variation** in phenotypic expression.
*Uniparental disomy*
- This refers to the inheritance of **two copies of a chromosome** or part of a chromosome from **one parent** and no copies from the other parent.
- It is typically associated with specific genetic disorders like Prader-Willi or Angelman syndromes and does not explain the general inheritance pattern of male-pattern baldness.
*Pleiotropy*
- **Pleiotropy** occurs when a **single gene** affects **multiple seemingly unrelated phenotypic traits**.
- This principle is incorrect because the scenario explicitly states that male-pattern baldness is influenced by "multiple genes," not a single gene affecting multiple traits.
*Anticipation*
- **Anticipation** is a phenomenon where the symptoms of a genetic disorder become more severe or appear earlier with each successive generation.
- This phenomenon is observed in conditions like Huntington's disease or myotonic dystrophy and is not the genetic principle described for male-pattern baldness.
*Heteroplasmy*
- **Heteroplasmy** refers to the presence of **more than one type of mitochondrial DNA** (mtDNA) within a single cell or individual.
- This principle is exclusive to mitochondrial inheritance and is not relevant to the inheritance pattern of male-pattern baldness, which is generally considered to be affected by nuclear genes.
Multiple endocrine neoplasia syndromes US Medical PG Question 4: A 45-year-old woman comes to see you for a second opinion regarding an upcoming surgery for pancreatic insulinoma. While taking a surgical history, she tells you she previously had a pituitary tumor resected. For which additional neoplasms might you consider testing her?
- A. Parathyroid adenoma (Correct Answer)
- B. Medullary thyroid carcinoma
- C. Mucosal neuroma
- D. Multiple myeloma
- E. Pheochromocytoma
Multiple endocrine neoplasia syndromes Explanation: ***Parathyroid adenoma***
- The patient's history of a **pituitary tumor** and a **pancreatic insulinoma** strongly suggests **Multiple Endocrine Neoplasia Type 1 (MEN1)**.
- **Parathyroid adenomas** are the most common manifestation of MEN1, affecting over 90% of patients, and should be screened for.
*Medullary thyroid carcinoma*
- This is a characteristic component of **Multiple Endocrine Neoplasia Type 2 (MEN2)**.
- MEN2 includes medullary thyroid carcinoma, pheochromocytoma, and parathyroid hyperplasia, which is distinct from the patient's presentation.
*Mucosal neuroma*
- **Mucosal neuromas** are associated with **Multiple Endocrine Neoplasia Type 2B (MEN2B)**, a subtype of MEN2.
- MEN2B also typically involves medullary thyroid carcinoma and pheochromocytoma, which do not align with the patient's current tumors.
*Multiple myeloma*
- This is a **hematologic malignancy** involving plasma cells and is not typically associated with the type of endocrine tumors seen in this patient.
- There is no direct link between multiple myeloma and pituitary or pancreatic neuroendocrine tumors.
*Pheochromocytoma*
- **Pheochromocytoma** is a tumor of the adrenal medulla and is a hallmark of **Multiple Endocrine Neoplasia Type 2 (MEN2)**.
- While it is an endocrine tumor, it is not part of the triad seen in MEN1 (pituitary, parathyroid, and pancreatic tumors).
Multiple endocrine neoplasia syndromes US Medical PG Question 5: A 31-year-old man comes to the physician because of worsening abdominal pain, an inability to concentrate at work, and a general lack of motivation over the past several months. He has a history of spontaneous passage of two kidney stones. His father and uncle underwent thyroidectomy before the age of 35 for thyroid cancer. Physical examination shows diffuse tenderness over the abdomen. Serum studies show:
Na+ 142 mEq/L
K+ 3.7 mEq/L
Glucose 131 mg/dL
Ca2+ 12.3 mg/dL
Albumin 4.1 g/dL
Parathyroid hormone 850 pg/mL
Further evaluation is most likely to show elevated levels of which of the following?
- A. Serum aldosterone to renin ratio
- B. Serum prolactin
- C. Urine metanephrines (Correct Answer)
- D. Urine 5-hydroxyindoleacetic acid
- E. Midnight salivary cortisol
Multiple endocrine neoplasia syndromes Explanation: ***Urine metanephrines***
- The patient's presentation with **hypercalcemia** (Ca2+ 12.3 mg/dL) and **elevated PTH** (850 pg/mL) indicates **hyperparathyroidism**.
- The family history of **thyroidectomy for thyroid cancer before age 35** (medullary thyroid cancer) along with hyperparathyroidism points towards **Multiple Endocrine Neoplasia type 2 (MEN2)**. MEN2 syndromes often include **pheochromocytoma**, which is diagnosed by elevated **urine metanephrines**.
*Serum aldosterone to renin ratio*
- This ratio is used to screen for **primary hyperaldosteronism**, which presents with **hypertension and hypokalemia**.
- The patient's blood pressure is not mentioned as elevated, and his **potassium (3.7 mEq/L) is within normal limits**, making primary hyperaldosteronism less likely.
*Serum prolactin*
- Elevated serum prolactin levels indicate **hyperprolactinemia**, which is a feature of **MEN1 (Multiple Endocrine Neoplasia type 1)**.
- While MEN1 also includes hyperparathyroidism, the family history of **early-onset thyroid cancer** (suggesting medullary thyroid cancer, not typically seen in MEN1) points more strongly to MEN2.
*Urine 5-hydroxyindoleacetic acid*
- Elevated levels of **5-HIAA in urine** are indicative of a **carcinoid tumor**, which secretes serotonin.
- Carcinoid tumors are not typically associated with the constellation of symptoms and family history presented, particularly hyperparathyroidism and early-onset medullary thyroid cancer.
*Midnight salivary cortisol*
- This test is used to diagnose **Cushing's syndrome**, which is characterized by elevated cortisol levels and symptoms like central obesity, moon facies, and striae.
- The patient's symptoms are not consistent with Cushing's syndrome, and the laboratory findings (hypercalcemia, elevated PTH) point to a different endocrine disorder.
Multiple endocrine neoplasia syndromes US Medical PG Question 6: A 47-year-old woman complains of weight gain and irregular menses for the past 2 years. She has gained 13 kg (28.6 lb) and feels that most of the weight gain is in her abdomen and face. She has type 2 diabetes and hypertension for 1 year, and they are difficult to control with medications. Vital signs include a temperature of 36.9°C (98.4°F), blood pressure of 160/100 mm Hg, and pulse of 95/min. The patient's late-night salivary cortisol is elevated. Morning plasma ACTH is high. Brain magnetic resonance imaging shows a 2 cm pituitary adenoma. Which of the following is the optimal therapy for this patient?
- A. Unilateral adrenalectomy
- B. Bilateral adrenalectomy
- C. Pituitary radiotherapy
- D. Medical therapy
- E. Transsphenoidal pituitary adenomectomy (Correct Answer)
Multiple endocrine neoplasia syndromes Explanation: ***Transsphenoidal pituitary adenomectomy***
- This patient presents with **Cushing's disease**, characterized by **elevated late-night salivary cortisol** and **high morning plasma ACTH**, coupled with a **pituitary adenoma** on MRI. **Transsphenoidal pituitary adenomectomy** is the first-line and most effective treatment for Cushing's disease, offering the highest chance of remission by directly removing the adenoma.
- Successful surgical removal of the tumor can quickly normalize **ACTH** and **cortisol** levels, leading to significant improvement in symptoms like **weight gain**, **hypertension**, **diabetes**, and **menstrual irregularities**.
*Unilateral adrenalectomy*
- This procedure treats **adrenal adenomas** causing Cushing's syndrome (primary adrenal hypercortisolism), which is characterized by **low or undetectable ACTH levels**. This patient has **high ACTH**, indicating a pituitary source.
- Performing a unilateral adrenalectomy in this case would not address the underlying **pituitary tumor** and would not cure Cushing's disease.
*Bilateral adrenalectomy*
- This is a treatment for severe, refractory Cushing's disease, or as a palliative measure, when **pituitary surgery** has failed or is contraindicated.
- While it effectively removes the source of **cortisol**, it leads to **adrenal insufficiency**, requiring lifelong corticosteroid replacement, and carries the risk of **Nelson's Syndrome** (rapid pituitary tumor growth due to loss of negative feedback).
*Pituitary radiotherapy*
- **Pituitary radiotherapy** is a secondary treatment option, typically used when **transsphenoidal surgery** fails to achieve remission, or if there is residual tumor.
- It has a slower onset of action (months to years) compared to surgery, and the patient's severe symptoms require more immediate control.
*Medical therapy*
- **Medical therapies** (e.g., **ketoconazole**, **mifepristone**, **pasireotide**) are often used as bridging therapy before surgery, when surgery is contraindicated, or for patients with persistent disease after surgery.
- They help control **hypercortisolism** but do not cure the underlying **pituitary adenoma**, making **surgical removal** the preferred definitive treatment.
Multiple endocrine neoplasia syndromes US Medical PG Question 7: A 21-year-old male college student is very anxious about having thyroid cancer as he found a lump in his neck a few days ago. He has also had diarrhea and a feeling of warmth on his face for 3 days now. His father and uncle both have been diagnosed with thyroid cancer. The lump is about 1 cm in diameter and is fixed and nontender on palpation. Physical examination is otherwise unremarkable. Ultrasound shows a non-cystic cold nodule that requires fine needle aspiration for diagnosis. Thyroid functions tests are normal, and his calcitonin level is 346 ug/ml. Which of the following genetic mutations would warrant thyroidectomy in this patient?
- A. A loss of function of PPARɣ
- B. MEN1 gene mutation
- C. Down expression of the Ras protooncogene
- D. RET gene mutation (Correct Answer)
- E. Activating mutation of the BRAF gene
Multiple endocrine neoplasia syndromes Explanation: ***RET gene mutation***
- The patient's symptoms (neck lump, flushing, diarrhea, elevated calcitonin, family history of thyroid cancer) are highly suggestive of **medullary thyroid carcinoma (MTC)**. MTC is strongly associated with **activating germline mutations in the RET proto-oncogene**, which warrant prophylactic thyroidectomy.
- An elevated **calcitonin level** is a key biochemical marker for MTC, and a positive family history, especially with features of MEN 2 syndrome, points towards a germline RET mutation.
*A loss of function of PPARɣ*
- **PPARɣ (Peroxisome Proliferator-Activated Receptor gamma)** loss of function is not directly associated with medullary thyroid carcinoma or the symptoms described.
- Mutations in PPARG are occasionally seen in follicular thyroid carcinoma, but not MTC.
*MEN1 gene mutation*
- **MEN1 gene mutations** are associated with **Multiple Endocrine Neoplasia Type 1 (MEN 1)**, which includes parathyroid hyperplasia, pituitary adenomas, and pancreatic endocrine tumors, but generally **not medullary thyroid carcinoma**.
- While MEN1 can cause endocrine tumors, it does not typically present with the significantly elevated calcitonin or the specific type of thyroid cancer seen in this patient.
*Down expression of the Ras protooncogene*
- **RAS gene mutations** (like HRAS, KRAS, NRAS) are commonly found in **follicular and papillary thyroid carcinomas**, but not in medullary thyroid carcinoma.
- "Down expression" or reduced expression of a proto-oncogene would typically reduce its oncogenic potential, which is less likely to cause a rapidly growing, aggressively presenting tumor like MTC.
*Activating mutation of the BRAF gene*
- **BRAF V600E mutation** is the most common genetic alteration in **papillary thyroid carcinoma (PTC)**. BRAF is a serine/threonine kinase involved in the MAPK signaling pathway.
- While PTC is a common thyroid cancer, the patient's presentation with flushing, diarrhea, and high calcitonin is classic for **medullary thyroid carcinoma**, not papillary thyroid carcinoma.
Multiple endocrine neoplasia syndromes US Medical PG Question 8: A 67-year-old woman with tertiary hyperparathyroidism and end-stage renal disease on hemodialysis has persistent hypercalcemia (calcium 12.8 mg/dL) despite maximal medical management with cinacalcet and vitamin D restriction. She has severe pruritus, calciphylaxis, and vascular calcifications. All four parathyroid glands are enlarged on imaging. Evaluate the optimal surgical strategy considering her complex medical status and need for ongoing dialysis access.
- A. Single adenoma resection guided by sestamibi
- B. Subtotal parathyroidectomy (3.5 gland resection)
- C. Total parathyroidectomy without autotransplantation
- D. Total parathyroidectomy with forearm autotransplantation (Correct Answer)
- E. Medical management escalation with denosumab
Multiple endocrine neoplasia syndromes Explanation: ***Total parathyroidectomy with forearm autotransplantation***
- In **tertiary hyperparathyroidism** with four-gland enlargement, this procedure provides definitive treatment while allowing for easier access if **recurrent hyperplasia** occurs.
- Placing the tissue in the **forearm** avoids risky neck re-explorations in the future and is the standard for patients who may remain on long-term dialysis.
*Single adenoma resection guided by sestamibi*
- This approach is inappropriate because **tertiary hyperparathyroidism** involves **multiglandular hyperplasia**, not a single solitary adenoma.
- Imaging with **sestamibi** is less reliable in renal patients, and leaving three hyperplastic glands would lead to surgical failure.
*Subtotal parathyroidectomy (3.5 gland resection)*
- While a valid option for some, it carries a higher risk of **persistent hypercalcemia** or recurrence within the neck remnant compared to total resection.
- In patients with **calciphylaxis** and severe symptoms, many surgeons prefer total resection to ensure immediate clearance of excess **parathyroid hormone**.
*Total parathyroidectomy without autotransplantation*
- This technique leads to permanent **hypoparathyroidism**, which is difficult to manage and can result in **adynamic bone disease**.
- It is generally reserved for patients who are not candidates for future transplantation and have severe, life-threatening **hypercalcemia** where no hormonal replacement is desired.
*Medical management escalation with denosumab*
- The patient has already failed **maximal medical management** including **cinacalcet**, and her severe **calciphylaxis** is a surgical emergency.
- **Denosumab** does not address the underlying autonomous parathyroid hyperplasia and is not a definitive treatment for **tertiary hyperparathyroidism**.
Multiple endocrine neoplasia syndromes US Medical PG Question 9: A 30-year-old man presents with a 6 cm adrenal mass discovered incidentally. Biochemical workup shows elevated 24-hour urine metanephrines and plasma free metanephrines. He also has elevated serum calcium, PTH, and a pancreatic head mass on CT. Genetic testing confirms MEN 2B syndrome. Evaluate the management priorities and sequencing of interventions.
- A. Simultaneous thyroidectomy and bilateral adrenalectomy
- B. Medical management of pheochromocytoma then parathyroidectomy
- C. Immediate thyroidectomy followed by staged procedures
- D. Adrenalectomy first, then thyroidectomy, then other tumors (Correct Answer)
- E. Pancreatic surgery first due to mass effect
Multiple endocrine neoplasia syndromes Explanation: ***Adrenalectomy first, then thyroidectomy, then other tumors***
- Prioritizing **pheochromocytoma** resection is critical to avoid a life-threatening **hypertensive crisis** during subsequent surgeries.
- Adequate medical preparation with **alpha-blockade** followed by beta-blockade is mandatory before any surgical intervention in these patients.
*Simultaneous thyroidectomy and bilateral adrenalectomy*
- Simultaneous procedures significantly increase **perioperative risk** and operative time without ensuring hemodynamic stability during the thyroid portion.
- Managing the **catecholamine surge** from a pheochromocytoma is safer when performed as a separate, initial stage.
*Medical management of pheochromocytoma then parathyroidectomy*
- While **alpha-blockade** is necessary, the question asks for the sequence of surgical interventions, where adrenalectomy must precede other operations.
- This patient presents with features suggestive of **MEN 2B**, which classically does not include hyperparathyroidism, unlike **MEN 1** or **MEN 2A**.
*Immediate thyroidectomy followed by staged procedures*
- Performing a **thyroidectomy** first is contraindicated because the stress of surgery and anesthesia can trigger a **pheochromocytoma crisis**.
- Even if medullary thyroid carcinoma is aggressive, the risk of immediate **intraoperative death** from pheochromocytoma takes precedence.
*Pancreatic surgery first due to mass effect*
- Although a **pancreatic head mass** is present (suggestive of MEN 1 overlap or separate pathology), it is not the immediate life-threatening priority.
- Operating on the pancreas before controlling and removing the **pheochromocytoma** exposes the patient to severe hemodynamic instability.
Multiple endocrine neoplasia syndromes US Medical PG Question 10: A 38-year-old woman with primary hyperparathyroidism (calcium 11.8 mg/dL, PTH 185 pg/mL) has negative sestamibi scan and ultrasound. She desires surgical cure and has no medical contraindications. She has a Z-score of -2.8 on DEXA scan and a history of recurrent kidney stones. Evaluate the surgical approach and expected outcomes.
- A. Defer surgery until localization studies are positive
- B. Bilateral neck exploration with identification of all four glands (Correct Answer)
- C. Minimally invasive parathyroidectomy of the largest gland
- D. Medical management with cinacalcet and bisphosphonates
- E. Intraoperative PTH-guided focused exploration
Multiple endocrine neoplasia syndromes Explanation: ***Bilateral neck exploration with identification of all four glands***
- When **preoperative localization** studies (Sestamibi and Ultrasound) are negative, a **bilateral neck exploration** is the gold standard to identify the source of primary hyperparathyroidism.
- This patient has clear indications for surgery including **nephrolithiasis**, a **Z-score of -2.8** (osteoporosis), and symptomatic hypercalcemia, making surgical intervention necessary despite negative imaging.
*Defer surgery until localization studies are positive*
- **Negative imaging** does not rule out primary hyperparathyroidism or contraindicate surgery when biochemical evidence is clear.
- Deferring treatment would risk further **bone loss** and recurrent **kidney stones** in a patient who already meets surgical criteria.
*Minimally invasive parathyroidectomy of the largest gland*
- **Minimally invasive parathyroidectomy (MIP)** requires precise preoperative localization to guide the surgeon to a specific quadrant.
- Attempting MIP without localization increases the risk of **surgical failure** and missing ectopic or multiglandular disease.
*Medical management with cinacalcet and bisphosphonates*
- **Medical management** is generally reserved for patients who are not surgical candidates or those who refuse surgery.
- While cinacalcet lowers **PTH** and calcium, it does not provide a **permanent cure** for the underlying adenoma or hyperplasia and is not the first-line choice for a young, fit patient.
*Intraoperative PTH-guided focused exploration*
- **Focused exploration** relies on knowing which side to explore first; without imaging, there is no target for a "focused" approach.
- While **intraoperative PTH** (ioPTH) monitoring is a useful adjunct to confirm cure, it does not replace the need for a comprehensive **bilateral search** when imaging is nonlocalizing.
More Multiple endocrine neoplasia syndromes US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.