Minimally invasive endocrine procedures US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Minimally invasive endocrine procedures. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Minimally invasive endocrine procedures US Medical PG Question 1: A patient presents with periods of severe headaches and flushing however every time they have come to the physician they have not experienced any symptoms. The only abnormal finding is a blood pressure of 175 mmHg/100 mmHg. It is determined that the optimal treatment for this patient is surgical. Prior to surgery which of the following noncompetitive inhibitors should be administered?
- A. Phentolamine
- B. Isoproterenol
- C. Atropine
- D. Propranolol
- E. Phenoxybenzamine (Correct Answer)
Minimally invasive endocrine procedures Explanation: ***Phenoxybenzamine***
- This patient likely has a **pheochromocytoma**, which explains the episodic headaches, flushing, and hypertension. **Phenoxybenzamine** is a **non-competitive, irreversible alpha-adrenergic blocker** that is crucial for preoperative preparation to prevent a **hypertensive crisis** during surgery.
- Its **irreversible binding** provides sustained alpha blockade, essential to control blood pressure and avoid catecholamine-induced surges during tumor manipulation.
*Phentolamine*
- **Phentolamine** is a **competitive alpha-adrenergic blocker** used to manage acute hypertensive episodes, but it has a shorter duration of action.
- It is not preferred for sustained preoperative alpha blockade due to its **reversible nature** and potential for drug washout during surgery, which could lead to catecholamine surges.
*Isoproterenol*
- **Isoproterenol** is a **beta-adrenergic agonist** that increases heart rate and contractility, and causes bronchodilation.
- It would be contraindicated in a patient with pheochromocytoma as it could worsen hypertension and cardiac symptoms by stimulating beta receptors that are already overly sensitive to endogenous catecholamines.
*Atropine*
- **Atropine** is a **muscarinic acetylcholine receptor antagonist** that blocks parasympathetic effects, like bradycardia and salivation.
- It has no role in managing hypertension or the catecholamine excess seen in pheochromocytoma.
*Propranolol*
- **Propranolol** is a **non-selective beta-adrenergic blocker** that can be used to control tachycardia and arrhythmias in pheochromocytoma, but only *after* adequate alpha-blockade has been established.
- Using **propranolol alone** or before alpha-blockade can lead to **unopposed alpha-adrenergic stimulation**, resulting in a severe, life-threatening hypertensive crisis.
Minimally invasive endocrine procedures US Medical PG Question 2: A 27-year-old man presents to the emergency department after being stabbed. The patient was robbed at a local pizza parlor and was stabbed over 10 times with a large kitchen knife with an estimated 7 inch blade in the ventral abdomen. His temperature is 97.6°F (36.4°C), blood pressure is 74/54 mmHg, pulse is 180/min, respirations are 19/min, and oxygen saturation is 98% on room air. The patient is intubated and given blood products and vasopressors. Physical exam is notable for multiple stab wounds over the patient's abdomen inferior to the nipple line. Which of the following is the best next step in management?
- A. Exploratory laparotomy (Correct Answer)
- B. Diagnostic peritoneal lavage
- C. CT scan of the abdomen and pelvis
- D. Exploratory laparoscopy
- E. FAST exam
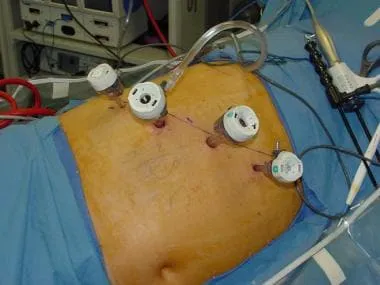
Minimally invasive endocrine procedures Explanation: ***Exploratory laparotomy***
- The patient presents with **multiple stab wounds** to the abdomen and signs of **hemorrhagic shock** (BP 74/54 mmHg, HR 180/min), which are clear indications for immediate surgical intervention.
- An exploratory laparotomy allows for direct visualization and repair of internal injuries, which is critical in this life-threatening situation.
*Diagnostic peritoneal lavage*
- While DPL can detect intra-abdominal bleeding, it is an **invasive procedure** and may delay definitive treatment in a hemodynamically unstable patient with obvious penetrating trauma.
- It is **less specific** than a laparotomy for identifying the exact location and nature of injuries, and it has largely been replaced by imaging studies or direct surgical exploration in unstable patients.
*CT scan of the abdomen and pelvis*
- A CT scan requires a **hemodynamically stable** patient and time for scanning and interpretation, which this patient does not have.
- Delaying definitive treatment for imaging in a patient with severe shock could lead to worse outcomes.
*Exploratory laparoscopy*
- Although less invasive, laparoscopy can be time-consuming and may not be feasible or safe in a patient with **profound hemorrhagic shock** and extensive injuries, especially if major vascular or visceral damage is suspected.
- Conversion to a **laparotomy** is often necessary in cases of significant injury, making immediate open exploration more efficient.
*FAST exam*
- A FAST exam can rapidly detect free fluid in the abdomen, suggesting internal bleeding, but it does **not provide specific information** about the source or extent of the injuries.
- While useful in the initial assessment, a positive FAST exam in a hemodynamically unstable patient with penetrating trauma directly points to the need for immediate surgical intervention, not further diagnostic delay.
Minimally invasive endocrine procedures US Medical PG Question 3: A 34-year-old woman is recovering in the post-operative unit following a laparoscopic procedure for chronic endometriosis. She had initially presented with complaints of painful menstrual cramps that kept her bedridden most of the day. She also mentioned to her gynecologist that she had been diagnosed with endometriosis 4 years ago, and she could not find a medication or alternative therapeutic measure that helped. Her medical history was significant for surgery she had 6 years ago to remove tumors she had above her kidneys, after which she was prescribed hydrocortisone. An hour after the laparoscopic procedure, she calls the nurse because she is having difficulty breathing. The nurse records her vital signs include: blood pressure 85/55 mm Hg, respirations 20/min, and pulse 115/min. The patient suddenly loses consciousness. Intravenous fluids are started immediately. She gains consciousness, but her blood pressure is unchanged. Which of the following is the most likely cause of the hypotension?
- A. Bleeding profusely through the surgical site
- B. Improper supplementation of steroids (Correct Answer)
- C. Infection involving the suture line
- D. High doses of anesthetic drugs
- E. Loss of fluids during the procedure
Minimally invasive endocrine procedures Explanation: ***Improper supplementation of steroids***
- The patient's history of **bilateral adrenalectomy (tumors above kidneys)** for which she was prescribed **hydrocortisone** indicates **adrenal insufficiency**. Stressful events like surgery require an increased dose of steroids, and improper supplementation can lead to an **adrenal crisis**.
- The symptoms of **hypotension, tachycardia, and loss of consciousness** are characteristic of an **adrenal crisis (acute adrenal insufficiency)**, which occurs when the body lacks sufficient cortisol during stress.
*Bleeding profusely through the surgical site*
- While **hemorrhage** can cause hypotension and tachycardia, the patient regained consciousness with IV fluids but her **blood pressure remained unchanged**, which is less typical for isolated blood loss if volume is restored without addressing the underlying cause.
- There is no direct mention of visible bleeding, the prompt only states the patient lost consciousness and her blood pressure is unchanged.
*Infection involving the suture line*
- **Surgical site infections** typically manifest several days post-op, presenting with **fever, erythema, and purulent drainage**, not acute hypotension and loss of consciousness an hour after surgery.
- The immediate post-operative timeline and systemic symptoms are not consistent with a localized wound infection as the primary cause of this acute decline.
*High doses of anesthetic drugs*
- Anesthetic drugs can cause **vasodilation and hypotension**. However, their effects are usually transient and would likely resolve more completely with IV fluids, especially an hour after a laparoscopic procedure.
- If it was due to anesthetic drugs, the patient's blood pressure would likely normalize with fluid administration once the effects of the anesthetic began to wear off, which is not the case here.
*Loss of fluids during the procedure*
- **Fluid loss** during surgery can cause hypotension, but intravenous fluids were administered, and the patient regained consciousness.
- If fluid loss were the sole cause, resolving consciousness and maintaining low blood pressure typically indicates the fluid loss was not completely compensated, but the primary cause for the persistent hypotension is not just volume.
Minimally invasive endocrine procedures US Medical PG Question 4: A 45-year-old man undergoes a parathyroidectomy given recurrent episodes of dehydration and kidney stones caused by hypercalcemia secondary to an elevated PTH level. He is recovering on the surgical floor on day 3. His temperature is 97.6°F (36.4°C), blood pressure is 122/81 mmHg, pulse is 84/min, respirations are 12/min, and oxygen saturation is 98% on room air. The patient is complaining of perioral numbness currently. What is the most appropriate management of this patient?
- A. Potassium
- B. TSH level
- C. Vitamin D
- D. Observation
- E. Calcium gluconate (Correct Answer)
Minimally invasive endocrine procedures Explanation: ***Calcium gluconate***
- The patient's presentation of **perioral numbness** following a parathyroidectomy, especially given a history of hypercalcemia, is highly suggestive of **hypocalcemia**.
- **Calcium gluconate** is indicated for acute symptomatic hypocalcemia to rapidly raise serum calcium levels and alleviate symptoms.
*Potassium*
- There is no clinical indication for **potassium** supplementation; the symptom of perioral numbness is not associated with potassium imbalance.
- Parathyroidectomy and hypercalcemia primarily affect calcium and phosphate metabolism, not typically potassium.
*TSH level*
- A **TSH level** is used to assess thyroid function, which is generally not directly affected by parathyroidectomy unless thyroid tissue was incidentally damaged.
- The symptoms presented do not suggest a thyroid dysfunction.
*Vitamin D*
- While **vitamin D** is crucial for calcium absorption and might be used in chronic management of hypocalcemia, it would not provide the immediate relief needed for acute symptomatic hypocalcemia.
- Acute symptoms like perioral numbness require a rapid elevation of serum calcium.
*Observation*
- **Observation** is inappropriate given the patient's symptomatic presentation of **perioral numbness**, which indicates acute and potentially worsening hypocalcemia.
- Untreated symptomatic hypocalcemia can progress to more severe complications such as seizures, arrhythmias, and laryngospasm.
Minimally invasive endocrine procedures US Medical PG Question 5: A 47-year-old woman comes to the physician for a mass in her left breast she noticed 2 days ago during breast self-examination. She has hypothyroidism treated with levothyroxine. There is no family history of breast cancer. Examination shows large, moderately ptotic breasts. The mass in her left breast is small (approximately 1 cm x 0.5 cm), firm, mobile, and painless. It is located 4 cm from her nipple-areolar complex at the 7 o'clock position. There are no changes in the skin or nipple, and there is no palpable axillary adenopathy. No masses are palpable in her right breast. A urine pregnancy test is negative. Mammogram showed a soft tissue mass with poorly defined margins. Core needle biopsy confirms a low-grade infiltrating ductal carcinoma. The pathological specimen is positive for estrogen receptors and negative for progesterone and human epidermal growth factor receptor 2 (HER2) receptors. Staging shows no distant metastatic disease. Which of the following is the most appropriate next step in management?
- A. Lumpectomy with sentinel lymph node biopsy followed by hormone therapy
- B. Nipple-sparing mastectomy with axillary lymph node dissection followed by hormone therapy
- C. Nipple-sparing mastectomy with axillary lymph node dissection, followed by radiation and hormone therapy
- D. Radical mastectomy followed by hormone therapy
- E. Lumpectomy with sentinel lymph node biopsy, followed by radiation and hormone therapy (Correct Answer)
Minimally invasive endocrine procedures Explanation: **Lumpectomy with sentinel lymph node biopsy, followed by radiation and hormone therapy**
- The patient has **early-stage (T1N0M0) estrogen receptor (ER)-positive, HER2-negative invasive ductal carcinoma** suitable for **breast-conserving surgery (lumpectomy)**.
- **Lumpectomy** must be followed by **radiation therapy** to the remaining breast tissue to reduce the risk of local recurrence, and **endocrine therapy** (due to ER positivity) is indicated to reduce systemic recurrence risk.
- **Sentinel lymph node biopsy** is performed to stage the axilla; if positive, an axillary lymph node dissection may be indicated. However, in this case, the mass is small, and there is no palpable axillary adenopathy, making sentinel lymph node biopsy the appropriate initial step.
*Lumpectomy with sentinel lymph node biopsy followed by hormone therapy*
- While **lumpectomy with sentinel lymph node biopsy** and **hormone therapy** are part of the appropriate management, **radiation therapy** to the conserved breast is a critical component that is missing from this option.
- Omitting **radiation therapy** after lumpectomy for invasive breast cancer significantly increases the risk of local recurrence.
*Nipple-sparing mastectomy with axillary lymph node dissection followed by hormone therapy*
- A **nipple-sparing mastectomy** is a more aggressive surgical approach than typically required for a **small, early-stage tumor** like this, which is amenable to breast-conserving surgery.
- **Axillary lymph node dissection** is usually reserved for cases with clinically positive lymph nodes or a positive sentinel lymph node biopsy, not as an initial step when there is no palpable axillary adenopathy.
*Nipple-sparing mastectomy with axillary lymph node dissection, followed by radiation and hormone therapy*
- This option involves an **unnecessarily extensive surgical procedure (nipple-sparing mastectomy with axillary lymph node dissection)** for a **small (1cm x 0.5cm) early-stage tumor** that can be managed with breast-conserving therapy.
- While radiation and hormone therapy are relevant, the initial surgical choice is too aggressive given the clinical presentation.
*Radical mastectomy followed by hormone therapy*
- **Radical mastectomy** (which includes removal of the breast, underlying chest muscle, and axillary lymph nodes) is rarely performed today due to its significant morbidity and is not indicated for this **early-stage tumor**.
- **Modified radical mastectomy**, which removes the breast and axillary lymph nodes while preserving the chest muscle, is typically only considered if breast-conserving surgery is not feasible or desired, and **hormone therapy** would be indicated, but **radiation** may also be needed depending on other factors.
Minimally invasive endocrine procedures US Medical PG Question 6: A 47-year-old woman presents to the clinic complaining of difficulty swallowing that started 1 month ago. The patient also reports a weight loss of 10 lbs during this time, without a change in her appetite. She denies fatigue, cough, hoarseness, pain, or hemoptysis. The patient has a history of childhood lymphoma, which was treated with radiation. She takes no medications. She has smoked 1 pack of cigarettes per day since she was 25 years old. Her physical exam is notable for a palpable nodule on the right side of the thyroid. An ultrasound is performed, which confirms a 1.2 cm hyperechoic nodule in the right lobe. Thyroid function labs are drawn and shown below:
Serum TSH: 0.2 mU/L
Serum thyroxine (T4): 187 nmol/L
Serum triiodothyronine (T3): 3.3 nmol/L
Which of the following is the next best step in management?
- A. Radioactive iodine
- B. Partial thyroidectomy
- C. Fine needle aspiration (Correct Answer)
- D. Levothyroxine
- E. Thyroid scintigraphy
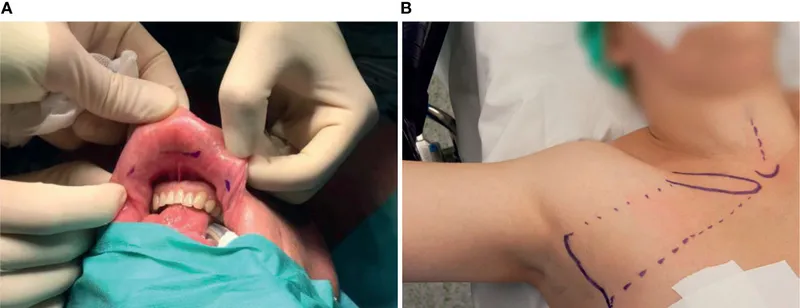
Minimally invasive endocrine procedures Explanation: ***Fine needle aspiration***
- This patient has several risk factors for **thyroid malignancy**, including a history of **radiation exposure** to the neck (for childhood lymphoma) and a palpable thyroid nodule associated with **dysphagia** and unexplained **weight loss**. Fine needle aspiration (FNA) is the best next step to evaluate for malignancy.
- The patient also presents with **hyperthyroidism** (low TSH, elevated T4), but the primary concern given the clinical picture is to rule out thyroid cancer.
- Per American Thyroid Association guidelines, FNA is indicated for any nodule in a patient with a history of head/neck radiation exposure.
*Radioactive iodine*
- Radioactive iodine ablation is used to treat **hyperthyroidism**, especially in cases of **Graves' disease** or toxic nodular goiter. While the patient has hyperthyroidism, the presence of a suspicious nodule warrants investigation for malignancy first.
- Administering radioactive iodine without first ruling out malignancy in a suspicious nodule could delay definitive treatment for cancer or complicate its management.
*Partial thyroidectomy*
- **Partial thyroidectomy** would be considered if the FNA results indicate malignancy or a highly suspicious follicular neoplasm.
- Performing surgery without a prior FNA would be premature, as many thyroid nodules are benign and do not require surgical intervention unless causing compressive symptoms or confirmed malignancy.
*Levothyroxine*
- **Levothyroxine** is used to treat **hypothyroidism** or to suppress TSH in cases of benign thyroid nodules or after thyroid cancer surgery.
- This patient is **hyperthyroid**, making exogenous levothyroxine inappropriate.
*Thyroid scintigraphy*
- **Thyroid scintigraphy** (radioactive iodine uptake scan) is useful in characterizing thyroid nodules as "hot" (functioning) or "cold" (non-functioning) in the context of hyperthyroidism.
- "Hot" nodules are rarely malignant, while "cold" nodules have a higher (though still relatively low) risk of malignancy. However, given the patient's strong risk factors for thyroid cancer and compressive symptoms, an FNA is more direct and informative for assessing malignancy than scintigraphy at this stage.
Minimally invasive endocrine procedures US Medical PG Question 7: A 50-year-old man undergoes parathyroidectomy for treatment-resistant hyperparathyroidism. The procedure is complicated by brisk bleeding from the superior thyroid artery near the external branch of the superior laryngeal nerve. To stop the bleeding, the artery is ligated at its origin. Which of the following is most likely the origin of the artery that was injured in this patient?
- A. Thyrocervical trunk
- B. Ascending pharyngeal artery
- C. Internal carotid artery
- D. Subclavian artery
- E. External carotid artery (Correct Answer)
Minimally invasive endocrine procedures Explanation: ***External carotid artery***
- The **superior thyroid artery** is the first branch to arise from the **external carotid artery** in the neck.
- Ligation of this artery at its origin is a common surgical maneuver to control bleeding during thyroid or parathyroid surgery.
*Thyrocervical trunk*
- The **thyrocervical trunk** is a branch of the **subclavian artery** and gives rise to the inferior thyroid artery, not the superior thyroid artery.
- Injury to the superior thyroid artery would not necessitate ligation of a vessel originating from the thyrocervical trunk.
*Ascending pharyngeal artery*
- The **ascending pharyngeal artery** is a small artery that branches from the **external carotid artery** but supplies the pharynx, not the thyroid gland.
- It is not typically implicated in bleeding during parathyroidectomy or in relation to the superior laryngeal nerve.
*Internal carotid artery*
- The **internal carotid artery** primarily supplies the brain and does not have branches in the neck that supply the thyroid or parathyroid glands.
- It arises from the common carotid artery but does not give off the superior thyroid artery.
*Subclavian artery*
- The **subclavian artery** gives rise to the **thyrocervical trunk**, which then supplies the inferior thyroid artery, but not directly the superior thyroid artery.
- The superior thyroid artery originates higher up from the external carotid artery.
Minimally invasive endocrine procedures US Medical PG Question 8: A 30-year-old woman is brought to the urgent care clinic by her husband. She complains of numbness around her lips and a tingling sensation in her hands and feet. She underwent near-total thyroidectomy for an enlarged thyroid gland a month ago. Vital signs include: blood pressure is 130/70 mm Hg, pulse is 72/min, respiratory rate is 16/min, and temperature is 37.0°C (98.6°F). A surgical incision scar is present in the anterior aspect of the neck. The attending physician inflates the blood pressure cuff above 150 mm Hg and observes the patient a couple of minutes while measuring her blood pressure. The patient develops sudden stiffness and tingling in her hand. Blood test results are as follows:
Hemoglobin (Hb%) 10.2 g/dL
White blood cell count 7000/mm3
Platelet count 160,000/mm3
Calcium, serum (Ca2+) 6.0 mg/dL
Albumin 4 g/dL
Alanine aminotransferase (ALT), serum 15 U/L
Aspartate aminotransferase (AST), serum 8 U/L
Serum creatinine 0.5 mg/dL
Urea 27 mg/dL
Sodium 137 mEq/L
Potassium 4.5 mEq/L
Magnesium 2.5 mEq/L
Urinalysis shows no white or red blood cells and leukocyte esterase is negative. Which of the following is the next best step in the management of this patient?
- A. 24-hour urinary calcium
- B. Serum vitamin D level
- C. CT scan abdomen with pancreatic protocol
- D. Thyroid function tests
- E. Serum parathyroid hormone (PTH) level (Correct Answer)
Minimally invasive endocrine procedures Explanation: ***Serum parathyroid hormone (PTH) level***
- The patient presents with **symptoms of hypocalcemia** (perioral numbness, tingling in hands and feet, positive Trousseau's sign, and serum calcium of 6.0 mg/dL) following a **near-total thyroidectomy**.
- Measuring **PTH levels** is crucial to determine if the hypocalcemia is due to **parathyroid gland damage** (low PTH) or another cause (high PTH).
*24-hour urinary calcium*
- This test is primarily used in the workup of **hypercalcemia** or **kidney stone disease** to assess calcium excretion.
- It is **not the initial diagnostic step** for symptomatic hypocalcemia post-thyroidectomy.
*Serum vitamin D level*
- While **vitamin D deficiency** can contribute to hypocalcemia, the acute onset of symptoms following thyroid surgery strongly points to parathyroid involvement.
- Addressing the **immediate calcium deficit** and evaluating PTH are higher priorities than measuring vitamin D levels at this stage.
*CT scan abdomen with pancreatic protocol*
- A CT scan of the abdomen with pancreatic protocol is used to evaluate **pancreatic pathology**, such as pancreatitis or tumors.
- This investigation is **irrelevant** to the patient's symptoms and recent thyroid surgery.
*Thyroid function tests*
- While important for managing patients post-thyroidectomy, routine thyroid function tests (TSH, T3, T4) are primarily to assess for **hypothyroidism** or **hyperthyroidism**.
- They do **not directly explain acute hypocalcemic symptoms** or guide immediate management of low calcium.
Minimally invasive endocrine procedures US Medical PG Question 9: A 30-year-old man comes to the physician after receiving a high blood pressure reading of 160/90 mm Hg at an annual employee health check-up. During the past few months, the patient has had occasional headaches and mild abdominal pain, both of which were relieved with ibuprofen. He has also had several episodes of heart palpitations. He has no history of serious illness. His mother and father both have hypertension. He has smoked one pack of cigarettes daily for the past 10 years and drinks one glass of wine daily. He occasionally smokes marijuana. He appears pale. His temperature is 36.8°C (98.2°F), pulse is 103/min, and blood pressure is 164/102 mm Hg. Physical examination shows no abnormalities. Laboratory studies show:
Hemoglobin 15.3 g/dL
Leukocyte count 7,900/mm3
Platelet count 223,000/mm3
Serum
Na+ 138 mEq/L
K+ 4.6 mEq/L
Cl- 103 mEq/L
Urea nitrogen 14 mg/dL
Glucose 90 mg/dL
Creatinine 0.9 mg/dL
Plasma metanephrines 1.2 nmol/L (N < 0.5 nmol/L)
Urine toxicology screening is positive for tetrahydrocannabinol (THC). Renal doppler shows no abnormalities. A CT scan of the abdomen shows a mass in the left adrenal gland. Which of the following is the most appropriate next step in management of this patient?
- A. Resection of adrenal mass
- B. Phenoxybenzamine (Correct Answer)
- C. Propranolol
- D. Metoprolol
- E. MIBG therapy
Minimally invasive endocrine procedures Explanation: ***Phenoxybenzamine***
- The patient's presentation with **hypertension**, **palpitations**, and significantly elevated **plasma metanephrines** (1.2 nmol/L vs. normal < 0.5 nmol/L), along with an **adrenal mass**, strongly suggests a **pheochromocytoma**.
- **Alpha-blockade** with phenoxybenzamine is the crucial first step to control blood pressure and prevent a **hypertensive crisis** during subsequent surgical resection.
*Resection of adrenal mass*
- While surgical resection is the **definitive treatment** for pheochromocytoma, it should **not be performed before adequate alpha-blockade**.
- **Unprepared surgery** can lead to a fatal hypertensive crisis due to uncontrolled catecholamine release during manipulation of the tumor.
*Propranolol*
- Propranolol is a **non-selective beta-blocker** and should **not be initiated before alpha-blockade** in pheochromocytoma.
- Blocking beta-adrenergic receptors can lead to **unopposed alpha-adrenergic vasoconstriction**, potentially worsening hypertension and causing a crisis.
*Metoprolol*
- Metoprolol is a **selective beta-1 blocker** and, like other beta-blockers, should **not be used before alpha-blockade** in pheochromocytoma.
- While it may have fewer peripheral vasoconstrictive effects than non-selective beta-blockers, the risk of unopposed alpha-stimulation remains significant.
*MIBG therapy*
- **Metaiodobenzylguanidine (MIBG) therapy** is a form of **radiotherapy** used for metastatic or inoperable pheochromocytoma/paraganglioma.
- It is **not the initial management** for a resectable adrenal mass in a patient with a newly diagnosed pheochromocytoma.
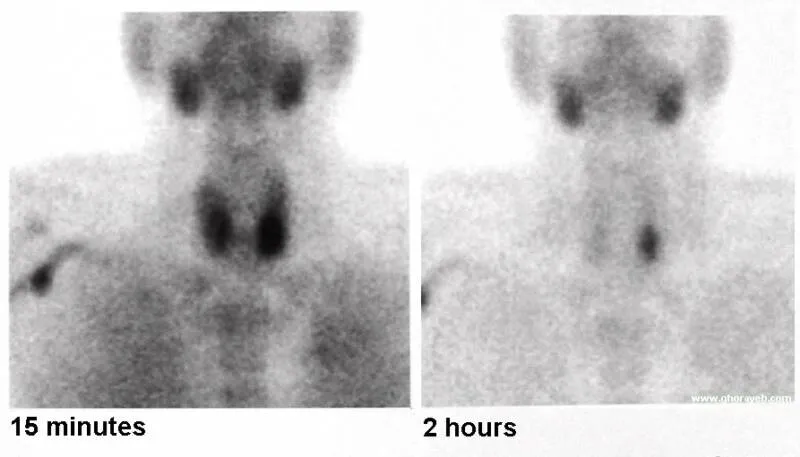
Minimally invasive endocrine procedures US Medical PG Question 10: A 64-year-old woman presents to an endocrinologist after her second time having a kidney stone in the last year. The patient reports no other symptoms except overall fatigue. On evaluation, the patient’s temperature is 98.4°F (36.9°C), blood pressure is 120/76 mmHg, pulse is 72/min, and respirations are 12/min. The patient has no neck masses and no tenderness to palpation in the abdomen. On laboratory workup, the endocrinologist finds that the patient has elevated parathyroid hormone levels and serum calcium. For surgical planning, the patient undergoes a sestamibi scan, which localizes disease to an area near the superior aspect of the thyroid in the right neck. Which of the following is the embryologic origin of this tissue?
- A. Fourth branchial arch
- B. Fourth branchial pouch (Correct Answer)
- C. Third branchial arch
- D. Dorsal wings of the third branchial pouch
- E. Ventral wings of the third branchial pouch
Minimally invasive endocrine procedures Explanation: ***Fourth branchial pouch***
- The superior parathyroid glands, generally located near the superior aspect of the thyroid, develop from the **fourth branchial pouch (dorsal wing)**.
- The **ultimobranchial body (C-cells)** also originates from the fourth branchial pouch.
*Fourth branchial arch*
- The fourth branchial arch forms structures like the **cricothyroid muscle**, pharyngeal constrictors, and laryngeal cartilages.
- It does not give rise to the parathyroid glands.
*Third branchial arch*
- The third branchial arch forms structures including the **stylopharyngeus muscle**, greater horn of the hyoid, and parts of the pharynx.
- It does not contribute to the formation of the parathyroid glands.
*Dorsal wings of the third branchial pouch*
- The **dorsal wings of the third branchial pouch** give rise to the inferior parathyroid glands.
- In this case, the diseased tissue was localized to the superior aspect nearest the superior parathyroid glands, not the inferior glands.
*Ventral wings of the third branchial pouch*
- The **ventral wings of the third branchial pouch** give rise to the thymus.
- This structure is not involved in parathyroid gland development.
More Minimally invasive endocrine procedures US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.