Hyperparathyroidism surgical management US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Hyperparathyroidism surgical management. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Hyperparathyroidism surgical management US Medical PG Question 1: A 71-year-old man comes to the emergency department because of a 2-month history of severe muscle cramps and back pain. He says that he is homeless and has not visited a physician in the past 20 years. He is 183 cm (6 ft 0 in) tall and weighs 62 kg (137 lb); BMI is 18.5 kg/m2. His blood pressure is 154/88 mm Hg. Physical examination shows pallor, multiple cutaneous excoriations, and decreased sensation over the lower extremities. Serum studies show:
Calcium 7.2 mg/dL
Phosphorus 5.1 mg/dL
Glucose 221 mg/dL
Creatinine 4.5 mg/dL
An x-ray of the spine shows alternating sclerotic and radiolucent bands in the lumbar and thoracic vertebral bodies. Which of the following is the most likely explanation for these findings?
- A. Primary hypoparathyroidism
- B. Secondary hyperparathyroidism (Correct Answer)
- C. Multiple myeloma
- D. Pseudohypoparathyroidism
- E. Tertiary hyperparathyroidism
Hyperparathyroidism surgical management Explanation: ***Secondary hyperparathyroidism***
- This patient presents with **hypocalcemia** (7.2 mg/dL) and **hyperphosphatemia** (5.1 mg/dL) in the context of **renal insufficiency** (creatinine 4.5 mg/dL), which are hallmarks of chronic kidney disease (CKD).
- **Secondary hyperparathyroidism** is a common complication of CKD, where the parathyroid glands overproduce PTH in response to low serum calcium and impaired phosphate excretion, leading to characteristic bone changes like **osteomalacia** and **osteitis fibrosa**, which can manifest as alternating sclerotic and radiolucent bands on X-ray (rugger-jersey spine).
*Primary hypoparathyroidism*
- This condition is characterized by **low PTH**, leading to both **hypocalcemia** and **hyperphosphatemia**.
- However, it would not typically present with the severe **renal insufficiency** seen in this patient, and the bone changes would differ.
*Multiple myeloma*
- Multiple myeloma is a plasma cell malignancy that often causes **hypercalcemia** due to bone destruction.
- It would not typically present with **hypocalcemia** and hyperphosphatemia, nor would it cause the specific rugger-jersey spine appearance (alternating sclerotic and radiolucent bands).
*Pseudohypoparathyroidism*
- This is a rare genetic disorder where target tissues are resistant to PTH, resulting in **hypocalcemia** and **hyperphosphatemia** despite **high PTH levels**.
- While it shares some lab findings, it is typically diagnosed in childhood and often associated with specific physical features (e.g., short stature, brachydactyly), which are not mentioned.
*Tertiary hyperparathyroidism*
- This condition develops in patients with long-standing **secondary hyperparathyroidism** where the parathyroid glands become autonomous, leading to **hypercalcemia** and **hyperphosphatemia** or normal phosphate levels.
- The patient's **hypocalcemia** makes tertiary hyperparathyroidism unlikely, as it typically involves elevated calcium levels due to uncontrolled PTH secretion.
Hyperparathyroidism surgical management US Medical PG Question 2: A 37-year-old female presents to her primary care physician with constipation and abdominal pain. She notes that the pain has been present for several days and is not related to food. She also reports increased urinary frequency without incontinence, as well as increased thirst. She takes no medications, but notes taking vitamin supplements daily. Her vital signs are: BP 130/72 mmHg, HR 82 bpm, T 97.0 degrees F, and RR 12 bpm. Lab studies reveal: Na 139, K 4.1, Cl 104, HCO3 25, Cr 0.9, and Ca 12.4. Further studies show an increased ionized calcium, decreased PTH, and normal phosphate. What is the most likely cause of this patient's symptoms?
- A. Vitamin overdose (Correct Answer)
- B. Vitamin deficiency
- C. Inherited disorder
- D. Plasma cell neoplasm
- E. Primary endocrine dysfunction
Hyperparathyroidism surgical management Explanation: ***Vitamin overdose***
- The patient's symptoms of **constipation**, **abdominal pain**, **increased urinary frequency**, and **thirst** are classic signs of **hypercalcemia**.
- The lab findings of **hypercalcemia (Ca 12.4)**, **increased ionized calcium**, **decreased PTH**, and increased phosphate, coupled with a history of daily vitamin supplements, strongly suggest **Vitamin D toxicity** from overdose, which leads to increased calcium absorption and bone resorption.
*Vitamin deficiency*
- Vitamin deficiencies typically do not cause **hypercalcemia**; in fact, severe **Vitamin D deficiency** can lead to **hypocalcemia** and **secondary hyperparathyroidism**.
- Symptoms associated with common vitamin deficiencies (e.g., scurvy, rickets) are not consistent with this patient's presentation.
*Inherited disorder*
- While some **inherited disorders** (e.g., **Familial Hypocalciuric Hypercalcemia**) can cause hypercalcemia, the distinguishing feature is typically a **normal or mildly elevated PTH** and **low urinary calcium excretion**, which is not entirely aligned with the presented PTH and phosphate levels and the acute onset suggested by symptoms.
- The patient's history of **vitamin supplement** use provides a more direct and likely explanation for acute hypercalcemia.
*Plasma cell neoplasm*
- **Plasma cell neoplasms** like **multiple myeloma** can cause **hypercalcemia** due to increased bone resorption from osteoclast-activating factors.
- However, hypercalcemia from these conditions is often accompanied by other signs of malignancy such as **renal failure**, **anemia**, or **bone lesions**, which are not reported in this case, and the **decreased PTH** points away from malignancy-associated humorally mediated hypercalcemia.
*Primary endocrine dysfunction*
- **Primary hyperparathyroidism** is a common cause of **hypercalcemia**, but it is characterized by **elevated or inappropriately normal PTH levels** in the presence of hypercalcemia, which contradicts the **decreased PTH** found in this patient.
- Other endocrine causes of hypercalcemia, such as **thyrotoxicosis** or **adrenal insufficiency**, present with distinct clinical features not described here.
Hyperparathyroidism surgical management US Medical PG Question 3: A 45-year-old man undergoes a parathyroidectomy given recurrent episodes of dehydration and kidney stones caused by hypercalcemia secondary to an elevated PTH level. He is recovering on the surgical floor on day 3. His temperature is 97.6°F (36.4°C), blood pressure is 122/81 mmHg, pulse is 84/min, respirations are 12/min, and oxygen saturation is 98% on room air. The patient is complaining of perioral numbness currently. What is the most appropriate management of this patient?
- A. Potassium
- B. TSH level
- C. Vitamin D
- D. Observation
- E. Calcium gluconate (Correct Answer)
Hyperparathyroidism surgical management Explanation: ***Calcium gluconate***
- The patient's presentation of **perioral numbness** following a parathyroidectomy, especially given a history of hypercalcemia, is highly suggestive of **hypocalcemia**.
- **Calcium gluconate** is indicated for acute symptomatic hypocalcemia to rapidly raise serum calcium levels and alleviate symptoms.
*Potassium*
- There is no clinical indication for **potassium** supplementation; the symptom of perioral numbness is not associated with potassium imbalance.
- Parathyroidectomy and hypercalcemia primarily affect calcium and phosphate metabolism, not typically potassium.
*TSH level*
- A **TSH level** is used to assess thyroid function, which is generally not directly affected by parathyroidectomy unless thyroid tissue was incidentally damaged.
- The symptoms presented do not suggest a thyroid dysfunction.
*Vitamin D*
- While **vitamin D** is crucial for calcium absorption and might be used in chronic management of hypocalcemia, it would not provide the immediate relief needed for acute symptomatic hypocalcemia.
- Acute symptoms like perioral numbness require a rapid elevation of serum calcium.
*Observation*
- **Observation** is inappropriate given the patient's symptomatic presentation of **perioral numbness**, which indicates acute and potentially worsening hypocalcemia.
- Untreated symptomatic hypocalcemia can progress to more severe complications such as seizures, arrhythmias, and laryngospasm.
Hyperparathyroidism surgical management US Medical PG Question 4: A 57-year-old man is brought to the emergency department 2 hours after the onset of severe nausea and vomiting. He also has cramping abdominal pain and feels fatigued. Two months ago, he injured his lumbar spine in a car accident and lost complete motor and sensory function below the level of injury. He has been bedridden ever since and is cared for at home. He has type 2 diabetes mellitus and renal insufficiency. Examination shows dry mucosal membranes and sensory impairment with flaccid paralysis in both lower limbs that is consistent with prior examinations. Laboratory studies show:
Serum
Calcium 12.8 mg/dL
Parathyroid hormone, N-terminal 180 pg/mL
Thyroid-stimulating hormone 2.5 μU/mL
Thyroxine 8 μg/dL
Calcitriol Decreased
Creatinine 2.6 mg/dL
Urine
Calcium 550 mg/24 h
In addition to administration of intravenous 0.9% saline and calcitonin, which of the following is the most appropriate next step in management?
- A. Thiazide diuretics
- B. Reduced calcium intake
- C. Bisphosphonates (Correct Answer)
- D. Hemodialysis
- E. Glucocorticoids
Hyperparathyroidism surgical management Explanation: ***Bisphosphonates***
- This patient presents with **severe hypercalcemia** (12.8 mg/dL) with symptoms of nausea, vomiting, and abdominal pain. Given his prolonged immobilization due to a spinal cord injury, **immobilization-induced hypercalcemia** is highly likely.
- After initial rehydration with 0.9% saline and calcitonin to rapidly lower calcium, **bisphosphonates** (e.g., zoledronic acid) are the most appropriate next step to inhibit osteoclast activity and **reduce bone resorption**, which is the primary driver of hypercalcemia in immobilized patients.
*Thiazide diuretics*
- Thiazide diuretics **increase calcium reabsorption** in the renal tubules, which would worsen hypercalcemia.
- These are typically used to treat hypercalciuria (and prevent kidney stones) in normocalcemic patients, not hypercalcemia.
*Reduced calcium intake*
- While reducing dietary calcium is a general recommendation for hypercalcemia, it is **insufficient** as the primary treatment for acute, severe hypercalcemia driven by **increased bone resorption**.
- The main problem here is bone breakdown, not excessive intake.
*Hemodialysis*
- Hemodialysis is reserved for **severe, refractory hypercalcemia** that does not respond to intravenous fluids, calcitonin, and bisphosphonates, especially in patients with severe renal failure.
- While this patient has renal insufficiency (Cr 2.6 mg/dL), other less invasive and highly effective treatments should be tried first.
*Glucocorticoids*
- Glucocorticoids are effective in treating hypercalcemia associated with certain conditions like **granulomatous diseases** (e.g., sarcoidosis) or **hematologic malignancies** (e.g., multiple myeloma).
- They work by reducing intestinal calcium absorption and decreasing production of calcitriol. They are **not indicated** for immobilization-induced hypercalcemia.
Hyperparathyroidism surgical management US Medical PG Question 5: A 25-year-old woman comes to the physician for a pre-employment examination. Her current medications include an oral contraceptive and a daily multivitamin. Physical examination is unremarkable. Serum studies show calcium of 11.8 mg/dL, phosphorus of 2.3 mg/dL, and parathyroid hormone level of 615 pg/mL. A 24-hour urine collection shows a low urinary calcium level. Which of the following is the most likely underlying cause of this patient’s laboratory findings?
- A. Extrarenal calcitriol production
- B. Impaired phosphate excretion
- C. Hyperplasia of parathyroid chief cells
- D. IL-1-induced osteoclast activation
- E. Defect in calcium-sensing receptors (Correct Answer)
Hyperparathyroidism surgical management Explanation: ***Defect in calcium-sensing receptors***
- The constellation of **hypercalcemia**, **low urinary calcium**, **elevated PTH**, and **hypophosphatemia** is highly suggestive of **Familial Hypocalciuric Hypercalcemia (FHH)**, which is caused by an inactivating defect in calcium-sensing receptors (CaSR) in the parathyroid glands and renal tubules.
- In FHH, the parathyroid glands misinterpret the elevated serum calcium as normal or low, leading to **inappropriately high PTH secretion**, while the kidneys excessively reabsorb calcium due to defective CaSRs, resulting in low urinary calcium excretion.
*Extrarenal calcitriol production*
- This would cause **hypercalcemia** and **hyperphosphatemia** due to increased intestinal absorption of both calcium and phosphate.
- **PTH levels** would typically be suppressed, not elevated, in response to hypercalcemia.
*Impaired phosphate excretion*
- This would lead to **hyperphosphatemia**, not the **hypophosphatemia** observed in the patient.
- While hyperphosphatemia can indirectly affect calcium, it does not directly explain the high PTH in the presence of hypercalcemia and low urinary calcium.
*Hyperplasia of parathyroid chief cells*
- Parathyroid chief cell hyperplasia leads to **primary hyperparathyroidism**, characterized by **hypercalcemia**, **elevated PTH**, and typically **hypercalciuria** (high urinary calcium) due to PTH's actions on the kidney, unlike the low urinary calcium seen in this patient.
- While PTH is elevated and calcium is high, the distinguishing feature here is the **low urinary calcium**, which rules out typical primary hyperparathyroidism.
*IL-1-induced osteoclast activation*
- This mechanism is seen in the **humoral hypercalcemia of malignancy (HHM)**, often due to parathyroid hormone-related protein (PTHrP) secretion or cytokine release by tumors.
- In HHM, **PTH levels** would be suppressed, and **phosphate would be normal or low**, but the hallmark is the absence of elevated PTH and often very high calcium, which doesn't match this patient's profile.
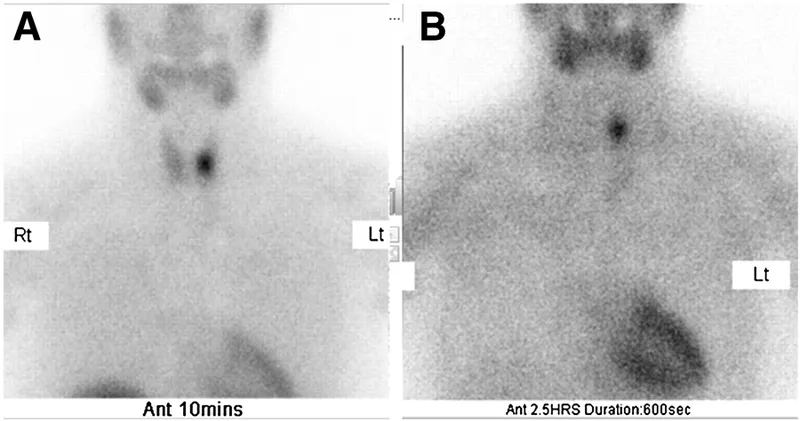
Hyperparathyroidism surgical management US Medical PG Question 6: A 64-year-old woman presents to an endocrinologist after her second time having a kidney stone in the last year. The patient reports no other symptoms except overall fatigue. On evaluation, the patient’s temperature is 98.4°F (36.9°C), blood pressure is 120/76 mmHg, pulse is 72/min, and respirations are 12/min. The patient has no neck masses and no tenderness to palpation in the abdomen. On laboratory workup, the endocrinologist finds that the patient has elevated parathyroid hormone levels and serum calcium. For surgical planning, the patient undergoes a sestamibi scan, which localizes disease to an area near the superior aspect of the thyroid in the right neck. Which of the following is the embryologic origin of this tissue?
- A. Fourth branchial arch
- B. Fourth branchial pouch (Correct Answer)
- C. Third branchial arch
- D. Dorsal wings of the third branchial pouch
- E. Ventral wings of the third branchial pouch
Hyperparathyroidism surgical management Explanation: ***Fourth branchial pouch***
- The superior parathyroid glands, generally located near the superior aspect of the thyroid, develop from the **fourth branchial pouch (dorsal wing)**.
- The **ultimobranchial body (C-cells)** also originates from the fourth branchial pouch.
*Fourth branchial arch*
- The fourth branchial arch forms structures like the **cricothyroid muscle**, pharyngeal constrictors, and laryngeal cartilages.
- It does not give rise to the parathyroid glands.
*Third branchial arch*
- The third branchial arch forms structures including the **stylopharyngeus muscle**, greater horn of the hyoid, and parts of the pharynx.
- It does not contribute to the formation of the parathyroid glands.
*Dorsal wings of the third branchial pouch*
- The **dorsal wings of the third branchial pouch** give rise to the inferior parathyroid glands.
- In this case, the diseased tissue was localized to the superior aspect nearest the superior parathyroid glands, not the inferior glands.
*Ventral wings of the third branchial pouch*
- The **ventral wings of the third branchial pouch** give rise to the thymus.
- This structure is not involved in parathyroid gland development.
Hyperparathyroidism surgical management US Medical PG Question 7: A 28-year-old man comes to the physician for a follow-up examination after a previous visit showed an elevated serum calcium level. He has a history of bipolar disorder. His mother had a parathyroidectomy in her 30s. The patient does not drink alcohol or smoke. Current medications include lithium and a daily multivitamin. His vital signs are within normal limits. Physical examination shows no abnormalities. Laboratory studies show:
Serum
Sodium 146 mEq/L
Potassium 3.7 mEq/L
Calcium 11.2 mg/dL
Magnesium 2.3 mEq/L
PTH 610 pg/mL
Albumin 4.2 g/dL
24-hour urine
Calcium 23 mg
Which of the following is the most likely cause of this patient’s findings?
- A. Lithium toxicity
- B. Parathyroid adenoma
- C. Excess calcium intake
- D. Excess vitamin D intake
- E. Abnormal calcium sensing receptors (Correct Answer)
Hyperparathyroidism surgical management Explanation: ***Abnormal calcium sensing receptors***
- The patient's **hypocalciuric hypercalcemia** (high serum calcium, low urine calcium) in the presence of an **elevated PTH** suggests a defect in calcium sensing.
- The family history of parathyroidectomy in the mother is consistent with an inherited condition affecting **calcium-sensing receptors (CaSRs)**, such as **familial hypocalciuric hypercalcemia (FHH)**.
*Lithium toxicity*
- **Lithium** can cause hypercalcemia by increasing the set point for calcium at the parathyroid gland, leading to increased PTH secretion.
- However, lithium typically does not lead to **hypocalciuria** to the extent seen in FHH, as it does not directly affect the kidney's CaSR in the same manner.
*Parathyroid adenoma*
- A **parathyroid adenoma** would cause **primary hyperparathyroidism**, characterized by hypercalcemia and elevated PTH.
- However, primary hyperparathyroidism typically presents with **hypercalciuria** due to the PTH-mediated increase in renal calcium reabsorption being overwhelmed by the increased filtered calcium load, unlike the hypocalciuria seen here.
*Excess calcium intake*
- **Excess calcium intake** could lead to hypercalcemia, but this would typically suppress PTH (unless it's a milk-alkali syndrome variant).
- It would also lead to **hypercalciuria** as the kidneys attempt to excrete the excess calcium, which is not observed here with a suppressed 24-hour urine calcium.
*Excess vitamin D intake*
- **Excess vitamin D intake** causes hypercalcemia by increasing intestinal calcium absorption and bone resorption, and would typically lead to **suppressed PTH** levels.
- It would also typically result in **hypercalciuria** due to the increased filtered calcium load, contrasting with the low urine calcium in this patient.
Hyperparathyroidism surgical management US Medical PG Question 8: A 75-year-old man is referred for thyroidectomy for treatment of thyroid nodules. A portion of the thyroid gland is resected, and the neck is closed with sutures. After awakening from anesthesia, the patient complains of ‘hoarseness’. His vital signs are normal and his incisional pain is minimal. The surgeon realizes he most likely damaged the recurrent laryngeal nerve. Which of the following should the surgeon tell the patient?
- A. "A mistake occurred during the operation, but there was no harm to you."
- B. "We made a mistake during the operation that may have harmed you." (Correct Answer)
- C. "The case took longer than we thought it would, but everything went well."
- D. "A mistake occurred because this hospital has poor operating room protocols."
- E. "The operation was successful and no complications occurred."
Hyperparathyroidism surgical management Explanation: ***\"We made a mistake during the operation that may have harmed you.\"***
- This statement accurately reflects the situation, acknowledging both the **mistake** and the potential **harm** to the patient (hoarseness due to recurrent laryngeal nerve damage).
- Open communication and honesty about medical errors are essential for maintaining **trust** and fulfilling ethical obligations to the patient.
*\"A mistake occurred during the operation, but there was no harm to you.\"*
- This statement is inaccurate because the patient is experiencing **hoarseness**, which is a sign of harm (recurrent laryngeal nerve damage).
- Dismissing the patient's symptom as "no harm" is **dishonest** and undermines trust.
*\"The case took longer than we thought it would, but everything went well.\"*
- This statement is misleading as it downplays a significant complication (recurrent laryngeal nerve damage) by implying that "everything went well" despite the patient's hoarseness.
- It avoids addressing the specific concern and does not acknowledge any **error** or **harm**.
*\"A mistake occurred because this hospital has poor operating room protocols.\"*
- While a mistake may have occurred, blaming the hospital's protocols is an attempt to deflect personal responsibility and can be seen as unprofessional.
- This statement introduces a potentially contentious issue that should be addressed internally rather than with the patient when disclosing the error.
*\"The operation was successful and no complications occurred.\"*
- This statement is explicitly false, as **hoarseness** due to recurrent laryngeal nerve damage is a direct and recognized **complication** of thyroidectomy.
- Making such a claim is unethical and violates the principle of **informed consent** and truthful disclosure.
Hyperparathyroidism surgical management US Medical PG Question 9: A 39-year-old woman presents to the emergency department with right upper quadrant abdominal discomfort for the past couple of hours. She says that the pain is dull in nature and denies any radiation. She admits to having similar episodes of pain in the past which subsided on its own. Her temperature is 37°C (99.6°F), respirations are 16/min, pulse is 78/min, and blood pressure is 122/98 mm Hg. Physical examination is normal except for diffuse tenderness of her abdomen. She undergoes a limited abdominal ultrasound which reveals a 1.4 cm gallbladder polyp. What is the next best step in the management of this patient?
- A. Barium swallow study
- B. Magnetic resonance cholangiopancreatography (MRCP)
- C. Endoscopic retrograde cholangiopancreatography (ERCP)
- D. No further treatment required
- E. Cholecystectomy (Correct Answer)
Hyperparathyroidism surgical management Explanation: ***Cholecystectomy***
- This patient has a **gallbladder polyp** measuring **1.4 cm**, which is above the threshold for concern (typically >1 cm), indicating a higher risk of **malignancy**.
- Given her recurrent **right upper quadrant pain**, even if dull and self-resolving, surgical removal (cholecystectomy) is the recommended management to prevent complications and rule out cancer.
*Barium swallow study*
- A **barium swallow study** is used to evaluate the **esophagus** and **upper gastrointestinal tract** for conditions like dysphagia, reflux, or strictures.
- It is not indicated for the evaluation or management of gallbladder polyps or right upper quadrant pain of biliary origin.
*Magnetic resonance cholangiopancreatography (MRCP)*
- **MRCP** is a non-invasive imaging technique primarily used to visualize the **biliary and pancreatic ducts** for conditions like gallstones, strictures, or tumors.
- While it can provide more detail on biliary anatomy, it is not the primary intervention for a large gallbladder polyp with symptomatic presentation; surgery is more definitive given the size.
*Endoscopic retrograde cholangiopancreatography (ERCP)*
- **ERCP** is an invasive endoscopic procedure used to diagnose and treat conditions of the **biliary and pancreatic ducts**, often involving stone removal or stent placement.
- It carries risks and is typically reserved for therapeutic interventions or when MRCP is inconclusive, and not for the initial management of a symptomatic gallbladder polyp.
*No further treatment required*
- A **gallbladder polyp over 1 cm** carries a significant risk of **malignant transformation** and requires intervention.
- This patient also has recurrent symptoms, which further supports the need for treatment rather than watchful waiting, to alleviate symptoms and address the polyp.
Hyperparathyroidism surgical management US Medical PG Question 10: A 30-year-old woman, gravida 1, para 0, at 30 weeks' gestation is brought to the emergency department because of progressive upper abdominal pain for the past hour. The patient vomited once on her way to the hospital. She said she initially had dull, generalized stomach pain about 6 hours prior, but now the pain is located in the upper abdomen and is more severe. There is no personal or family history of any serious illnesses. She is sexually active with her husband. She does not smoke or drink alcohol. Medications include folic acid and a multivitamin. Her temperature is 38.5°C (101.3°F), pulse is 100/min, and blood pressure is 130/80 mm Hg. Physical examination shows right upper quadrant tenderness. The remainder of the examination shows no abnormalities. Laboratory studies show a leukocyte count of 12,000/mm3. Urinalysis shows mild pyuria. Which of the following is the most appropriate definitive treatment in the management of this patient?
- A. Laparoscopic removal of ovarian cysts
- B. Cefoxitin and azithromycin
- C. Appendectomy
- D. Cholecystectomy (Correct Answer)
- E. Intramuscular ceftriaxone followed by cephalexin
Hyperparathyroidism surgical management Explanation: ***Cholecystectomy***
- The patient's presentation (fever, RUQ pain, leukocytosis, vomiting) is classic for **acute cholecystitis** in pregnancy, which requires **cholecystectomy** as the definitive treatment.
- **Laparoscopic cholecystectomy** is safe during pregnancy and is the **preferred definitive treatment** for acute cholecystitis, ideally performed in the second trimester but can be done in the third trimester when indicated.
- While conservative management with antibiotics and supportive care can be attempted initially, cholecystectomy remains the definitive treatment and is increasingly performed during pregnancy to avoid recurrent symptoms and complications.
- The mild pyuria is likely secondary to adjacent inflammation rather than a primary UTI.
*Laparoscopic removal of ovarian cysts*
- Ovarian cysts typically present with **pelvic or lower abdominal pain**, not RUQ tenderness.
- The clinical picture with fever, leukocytosis, and RUQ pain strongly suggests biliary pathology, not ovarian pathology.
*Cefoxitin and azithromycin*
- This regimen is used for **pelvic inflammatory disease (PID)**, which presents with lower abdominal/pelvic pain, cervical motion tenderness, and vaginal discharge.
- The patient's RUQ localization and fever pattern do not support PID as the primary diagnosis.
*Intramuscular ceftriaxone followed by cephalexin*
- This regimen treats **gonorrhea/chlamydia** or uncomplicated UTIs.
- While mild pyuria is present, the dominant clinical features (fever, RUQ pain, leukocytosis) point to cholecystitis, not a primary genitourinary infection.
- Antibiotics alone would not provide definitive treatment for acute cholecystitis.
*Appendectomy*
- **Appendicitis** in pregnancy typically causes **RLQ pain** (though it can migrate superiorly in the third trimester due to uterine displacement).
- The distinct **RUQ localization** with the classic triad of fever, RUQ pain, and leukocytosis makes cholecystitis far more likely than appendicitis.
More Hyperparathyroidism surgical management US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.