Endocrine surgery complications US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Endocrine surgery complications. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Endocrine surgery complications US Medical PG Question 1: A 48-year-old woman underwent a thyroidectomy with central neck dissection due to papillary thyroid carcinoma. On day 2 postoperatively, she developed irritability, dysphagia, difficulty breathing, and spasms in different muscle groups in her upper and lower extremities. The vital signs include blood pressure 102/65 mm Hg, heart rate 93/min, respiratory rate 17/min, and temperature 36.1℃ (97.0℉). Physical examination shows several petechiae on her forearms, muscle twitching in her upper and lower extremities, expiratory wheezes on lung auscultation, decreased S1 and S2 and the presence of an S3 on cardiac auscultation, and positive Trousseau and Chvostek signs. Laboratory studies show:
Ca2+ 4.4 mg/dL
Mg2+ 1.7 mEq/L
Na+ 140 mEq/L
K+ 4.3 mEq/L
Cl- 107 mEq/L
HCO3- 25 mEq/L
Administration of which of the following agents could prevent the patient’s condition?
- A. Anticonvulsants prior to and for 1 week after the operation
- B. Vitamin D and ionic calcium prior to and 2 weeks after the operation (Correct Answer)
- C. Potassium supplementation prior to and 2 weeks after the operation
- D. Calcium gluconate intraoperatively
- E. Magnesium sulfate intraoperatively
Endocrine surgery complications Explanation: ***Vitamin D and ionic calcium prior to and 2 weeks after the operation***
- The patient's symptoms are consistent with **hypocalcemia** (low calcium), a common complication after thyroidectomy due to inadvertent parathyroid gland removal or damage. Prophylactic **calcium and vitamin D supplementation** can prevent severe postoperative hypocalcemia by helping maintain calcium homeostasis.
- The patient's calcium level of 4.4 mg/dL (normal range 8.5-10.2 mg/dL) confirms severe hypocalcemia. The presence of **Trousseau and Chvostek signs**, muscle spasms, and dysphagia are classic signs of hypocalcemic tetany.
*Anticonvulsants prior to and for 1 week after the operation*
- This patient's symptoms are not indicative of an underlying seizure disorder, but rather **neuromuscular excitability** due to hypocalcemia. Anticonvulsants would not address the root cause.
- While severe hypocalcemia can rarely lead to seizures, prophylactic anticonvulsant administration is not standard practice for preventing this specific post-thyroidectomy complication.
*Potassium supplementation prior to and 2 weeks after the operation*
- The patient's potassium level is 4.3 mEq/L, which is within the normal range (3.5-5.0 mEq/L). **Hyperkalemia or hypokalemia** is not the primary issue here.
- Potassium supplementation would not address the hypocalcemia causing her symptoms and could potentially lead to **hyperkalemia**, which has its own set of dangers.
*Calcium gluconate intraoperatively*
- **Intraoperative calcium gluconate** is typically used for acute, severe hypocalcemia or cardiac arrest, not as a prophylactic measure. Administering it intraoperatively would not prevent the delayed onset of hypocalcemia seen on day 2.
- The goal is to prevent hypocalcemia by supporting calcium levels proactively, rather than treating an acute drop during surgery, which is rare.
*Magnesium sulfate intraoperatively*
- The patient's magnesium level of 1.7 mEq/L is at the lower limit of normal (1.7-2.2 mEq/L). While **hypomagnesemia** can impair PTH secretion and cause refractory hypocalcemia, magnesium supplementation is not the primary prophylactic strategy for post-thyroidectomy hypocalcemia.
- Intraoperative magnesium sulfate would not address the fundamental issue of parathyroid gland injury or removal causing the hypocalcemia. Calcium and vitamin D remain the cornerstone of prevention.
Endocrine surgery complications US Medical PG Question 2: A 38-year-old woman undergoes hemithyroidectomy for treatment of localized, well-differentiated papillary thyroid carcinoma. The lesion is removed with clear margins. However, during the surgery, a structure lying directly adjacent to the superior thyroid artery at the upper pole of the thyroid lobe is damaged. This patient is most likely to experience which of the following symptoms?
- A. Shortness of breath
- B. Weakness of shoulder shrug
- C. Voice pitch limitation (Correct Answer)
- D. Difficulty swallowing
- E. Ineffective cough
Endocrine surgery complications Explanation: ***Voice pitch limitation***
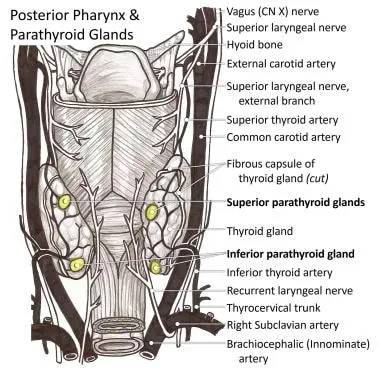
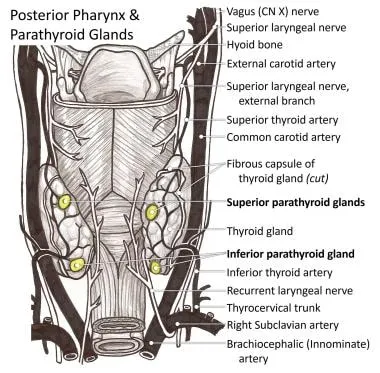
- Damage to the structure directly adjacent to the **superior thyroid artery** at the upper pole of the thyroid likely involves the **external branch of the superior laryngeal nerve (EBSLN)**.
- This nerve innervates the **cricothyroid muscle**, which is responsible for **tensing the vocal cords** and controlling **voice pitch**.
- Injury results in inability to change pitch, voice fatigue during prolonged speaking, and reduced vocal range.
*Shortness of breath*
- While damage to other nerves like the **recurrent laryngeal nerve** could cause vocal cord paralysis and potentially lead to airway compromise, this is less directly associated with the superior thyroid artery.
- Shortness of breath is not the specific consequence of EBSLN injury near the superior thyroid artery.
*Weakness of shoulder shrug*
- Weakness of shoulder shrug is associated with damage to the **spinal accessory nerve (cranial nerve XI)**, which innervates the **trapezius muscle**.
- This nerve is anatomically distinct from structures near the superior thyroid artery at the upper pole of the thyroid.
*Difficulty swallowing*
- Difficulty swallowing (dysphagia) can result from damage to the **vagus nerve (cranial nerve X)** or its pharyngeal branches, but it is not the direct consequence of injury near the superior thyroid artery.
- Damage to the EBSLN primarily affects voice pitch and quality, not swallowing.
*Ineffective cough*
- An ineffective cough results from paralysis of the vocal cords (preventing glottic closure) or weakness of respiratory muscles, typically from **recurrent laryngeal nerve** damage or phrenic nerve injury.
- EBSLN damage primarily affects voice pitch and does not significantly impair cough effectiveness.
Endocrine surgery complications US Medical PG Question 3: A 50-year-old woman comes to the physician because of palpitations and irritability. Over the past 4 months, she has had several episodes of heart racing and skipping beats that lasted between 30 seconds and several hours. She has also been arguing with her husband more, often about the temperature being too warm. The patient has also lost 8.8-kg (19.4-lb) over the past 4 months, despite being less strict with her diet. She has mild asthma treated with inhaled bronchodilators. Her pulse is 102/min and blood pressure is 148/98 mm Hg. On physical examination, the skin is warm and moist. A mass is palpated in the anterior neck area. On laboratory studies, thyroid stimulating hormone is undetectable and there are antibodies against the thyrotropin-receptor. Thyroid scintigraphy shows diffusely increased iodine uptake. Two weeks later, a single oral dose of radioactive iodine is administered. This patient will most likely require which of the following in the long-term?
- A. Propranolol therapy
- B. Near-total thyroidectomy
- C. L-thyroxine therapy (Correct Answer)
- D. Methimazole therapy
- E. Estrogen replacement therapy
Endocrine surgery complications Explanation: * ***L-thyroxine therapy***
* Radioactive iodine ablation for **Graves' disease** often leads to **permanent hypothyroidism**, necessitating **lifelong thyroid hormone replacement** with levothyroxine.
* The patient presents with classic **hyperthyroidism** symptoms (palpitations, irritability, weight loss, heat intolerance, warm/moist skin, goiter, undetectable TSH, positive **TSH receptor antibodies**, diffuse uptake on scintigraphy), treated with radioactive iodine.
* *Propranolol therapy*
* Propranolol is a **beta-blocker** used for symptomatic relief of hyperthyroidism, particularly palpitations and tremors.
* It does **not treat the underlying cause** of hyperthyroidism or subsequent hypothyroidism, and therefore is not a long-term solution after successful radioactive iodine therapy.
* *Near-total thyroidectomy*
* A near-total thyroidectomy is a surgical option for hyperthyroidism, especially in cases of very large goiters, contraindications to radioactive iodine, or malignancy.
* While it also often leads to **hypothyroidism** requiring long-term L-thyroxine, it was **not the chosen treatment modality** in this scenario (radioactive iodine was administered).
* *Methimazole therapy*
* Methimazole is an **antithyroid drug** used to decrease thyroid hormone synthesis in hyperthyroidism.
* It is used as a **primary treatment for hyperthyroidism** or as preparation for definitive therapy like radioactive iodine or surgery; it is not a long-term treatment after successful radioactive iodine ablation has induced hypothyroidism.
* *Estrogen replacement therapy*
* Estrogen replacement therapy is used for symptoms of **menopause** or to prevent osteoporosis, but it has no direct role in the management of thyroid disorders.
* The patient's symptoms are clearly indicative of a **thyroid pathology**, not primarily menopausal symptoms.
Endocrine surgery complications US Medical PG Question 4: Immediately after undergoing a right total knee replacement, a 69-year-old woman has severe abdominal pain, non-bloody emesis, and confusion. She has a history of Hashimoto thyroiditis that is well-controlled with levothyroxine and hyperlipidemia that is controlled by diet. She underwent bunion removal surgery from her right foot 10 years ago. Her temperature is 39°C (102.2°F), pulse is 120/min, and blood pressure is 60/30 mm Hg. Abdominal examination shows a diffusely tender abdomen with normal bowel sounds. She is confused and oriented to person but not place or time. Laboratory studies are pending. Which of the following is the most appropriate next step in the management of this patient?
- A. High-dose hydrocortisone
- B. Exploratory laparotomy
- C. CT angiogram of the abdomen
- D. Noncontrast CT of the head
- E. Intravenous isotonic saline infusion (Correct Answer)
Endocrine surgery complications Explanation: ***Intravenous isotonic saline infusion***
- The patient presents with **shock** (BP 60/30 mm Hg, pulse 120/min, confusion), which is immediately life-threatening and requires urgent intervention.
- **IV fluid resuscitation** is the **first priority** in any shock state to restore intravascular volume, improve tissue perfusion, and stabilize hemodynamics.
- While this patient has features concerning for **acute adrenal crisis** (Hashimoto thyroiditis with possible polyglandular autoimmune syndrome, post-surgical stress, fever, hypotension, confusion), **fluid resuscitation must be initiated immediately** before or concurrent with other therapies.
- In practice, **high-dose hydrocortisone should be given simultaneously** with fluids, but restoring circulating volume is the foundational first step.
*High-dose hydrocortisone*
- This patient has **Hashimoto thyroiditis** and presents with shock after major surgery (a known precipitant), raising strong suspicion for **acute adrenal crisis**.
- Patients with autoimmune thyroid disease can have concurrent **autoimmune adrenal insufficiency** (Schmidt syndrome/APS-2).
- **Hydrocortisone is critical** and should be given immediately (typically 100 mg IV), but **not before addressing the shock state** with fluid resuscitation.
- This would be the appropriate **second step** or given concurrently with fluids.
*Exploratory laparotomy*
- While the patient has **severe abdominal pain** and **diffuse tenderness**, the overall presentation (fever, hypotension, post-op state) suggests **medical shock** rather than a surgical emergency.
- **Normal bowel sounds** make mechanical obstruction or perforation less likely.
- Surgery is inappropriate until the patient is hemodynamically stabilized and a surgical cause is confirmed.
*CT angiogram of the abdomen*
- This could evaluate for **mesenteric ischemia**, but the patient is **too unstable** for imaging.
- The clinical picture better fits **adrenal crisis** or **septic shock** rather than vascular catastrophe.
- **Delaying resuscitation** for imaging in a patient with severe hypotension would be harmful.
*Noncontrast CT of the head*
- The patient's **confusion** is most likely due to **hypoperfusion** and **shock** rather than a primary intracranial process.
- **Altered mental status** is a common manifestation of shock and adrenal crisis.
- Cerebral perfusion depends on adequate systemic blood pressure, making **circulatory stabilization the priority**.
Endocrine surgery complications US Medical PG Question 5: An obese 52-year-old man is brought to the emergency department because of increasing shortness of breath for the past 8 hours. Two months ago, he noticed a mass on the right side of his neck and was diagnosed with laryngeal cancer. He has smoked two packs of cigarettes daily for 27 years. He drinks two pints of rum daily. He appears ill. He is oriented to person, place, and time. His temperature is 37°C (98.6°F), pulse is 111/min, respirations are 34/min, and blood pressure is 140/90 mm Hg. Pulse oximetry on room air shows an oxygen saturation of 89%. Examination shows a 9-cm, tender, firm subglottic mass on the right side of the neck. Cervical lymphadenopathy is present. His breathing is labored and he has audible inspiratory stridor but is able to answer questions. The lungs are clear to auscultation. Arterial blood gas analysis on room air shows:
pH 7.36
PCO2 45 mm Hg
PO2 74 mm Hg
HCO3- 25 mEq/L
He has no advanced directive. Which of the following is the most appropriate next step in management?
- A. Comfort care measures
- B. Cricothyroidotomy (Correct Answer)
- C. Tracheostomy
- D. Intramuscular epinephrine
- E. Tracheal stenting
Endocrine surgery complications Explanation: ***Correct: Cricothyroidotomy***
- This patient has **impending complete airway obstruction** evidenced by inspiratory stridor, severe tachypnea (34/min), hypoxia (O2 sat 89%), and a large obstructing laryngeal mass
- **Cricothyroidotomy** is the emergent surgical airway procedure of choice when there is **imminent or actual complete upper airway obstruction** and endotracheal intubation cannot be safely performed
- The subglottic mass makes endotracheal intubation **extremely dangerous** - instrumentation could precipitate complete obstruction and inability to ventilate
- Cricothyroidotomy provides **immediate airway access** (can be performed in 30-60 seconds) below the level of obstruction, making it life-saving in this emergency
- In the "cannot intubate, cannot ventilate" scenario, cricothyroidotomy is the definitive emergency intervention per ATLS and airway management guidelines
*Incorrect: Tracheostomy*
- While tracheostomy provides definitive airway management, it is a **controlled, elective procedure** typically performed in the OR that takes 20-30 minutes
- This patient requires **immediate airway access** - waiting for OR setup and performing tracheostomy risks complete airway collapse and death
- Tracheostomy may be performed later as a planned procedure once the airway is secured with cricothyroidotomy
- The presence of stridor indicates **critical airway narrowing** requiring emergency intervention, not elective surgery
*Incorrect: Comfort care measures*
- The patient is **alert and oriented** without an advanced directive indicating wishes for comfort care only
- This is an **acute, reversible condition** with appropriate emergency airway intervention
- Presumed consent applies in life-threatening emergencies when the patient cannot formally consent but intervention would be life-saving
- Comfort care would be inappropriate without documented patient wishes or irreversible terminal condition
*Incorrect: Intramuscular epinephrine*
- Epinephrine is indicated for **anaphylaxis** or angioedema causing airway edema from allergic/inflammatory mechanisms
- This patient has **mechanical obstruction** from a solid tumor mass, which will not respond to epinephrine
- Epinephrine causes vasoconstriction and reduces mucosal edema but cannot reduce tumor mass
- Would delay definitive airway management and not address the underlying problem
*Incorrect: Tracheal stenting*
- Tracheal stenting requires **bronchoscopy** in a controlled setting and is used for palliation of tracheal narrowing
- Cannot be performed emergently in an unstable patient with impending airway obstruction
- The obstruction is at the **laryngeal/subglottic level**, not typically amenable to emergency stenting
- Requires time for procedure setup and sedation, which this patient cannot afford given the critical airway emergency
Endocrine surgery complications US Medical PG Question 6: A 67-year-old woman with tertiary hyperparathyroidism and end-stage renal disease on hemodialysis has persistent hypercalcemia (calcium 12.8 mg/dL) despite maximal medical management with cinacalcet and vitamin D restriction. She has severe pruritus, calciphylaxis, and vascular calcifications. All four parathyroid glands are enlarged on imaging. Evaluate the optimal surgical strategy considering her complex medical status and need for ongoing dialysis access.
- A. Single adenoma resection guided by sestamibi
- B. Subtotal parathyroidectomy (3.5 gland resection)
- C. Total parathyroidectomy without autotransplantation
- D. Total parathyroidectomy with forearm autotransplantation (Correct Answer)
- E. Medical management escalation with denosumab
Endocrine surgery complications Explanation: ***Total parathyroidectomy with forearm autotransplantation***
- In **tertiary hyperparathyroidism** with four-gland enlargement, this procedure provides definitive treatment while allowing for easier access if **recurrent hyperplasia** occurs.
- Placing the tissue in the **forearm** avoids risky neck re-explorations in the future and is the standard for patients who may remain on long-term dialysis.
*Single adenoma resection guided by sestamibi*
- This approach is inappropriate because **tertiary hyperparathyroidism** involves **multiglandular hyperplasia**, not a single solitary adenoma.
- Imaging with **sestamibi** is less reliable in renal patients, and leaving three hyperplastic glands would lead to surgical failure.
*Subtotal parathyroidectomy (3.5 gland resection)*
- While a valid option for some, it carries a higher risk of **persistent hypercalcemia** or recurrence within the neck remnant compared to total resection.
- In patients with **calciphylaxis** and severe symptoms, many surgeons prefer total resection to ensure immediate clearance of excess **parathyroid hormone**.
*Total parathyroidectomy without autotransplantation*
- This technique leads to permanent **hypoparathyroidism**, which is difficult to manage and can result in **adynamic bone disease**.
- It is generally reserved for patients who are not candidates for future transplantation and have severe, life-threatening **hypercalcemia** where no hormonal replacement is desired.
*Medical management escalation with denosumab*
- The patient has already failed **maximal medical management** including **cinacalcet**, and her severe **calciphylaxis** is a surgical emergency.
- **Denosumab** does not address the underlying autonomous parathyroid hyperplasia and is not a definitive treatment for **tertiary hyperparathyroidism**.
Endocrine surgery complications US Medical PG Question 7: A 30-year-old man presents with a 6 cm adrenal mass discovered incidentally. Biochemical workup shows elevated 24-hour urine metanephrines and plasma free metanephrines. He also has elevated serum calcium, PTH, and a pancreatic head mass on CT. Genetic testing confirms MEN 2B syndrome. Evaluate the management priorities and sequencing of interventions.
- A. Simultaneous thyroidectomy and bilateral adrenalectomy
- B. Medical management of pheochromocytoma then parathyroidectomy
- C. Immediate thyroidectomy followed by staged procedures
- D. Adrenalectomy first, then thyroidectomy, then other tumors (Correct Answer)
- E. Pancreatic surgery first due to mass effect
Endocrine surgery complications Explanation: ***Adrenalectomy first, then thyroidectomy, then other tumors***
- Prioritizing **pheochromocytoma** resection is critical to avoid a life-threatening **hypertensive crisis** during subsequent surgeries.
- Adequate medical preparation with **alpha-blockade** followed by beta-blockade is mandatory before any surgical intervention in these patients.
*Simultaneous thyroidectomy and bilateral adrenalectomy*
- Simultaneous procedures significantly increase **perioperative risk** and operative time without ensuring hemodynamic stability during the thyroid portion.
- Managing the **catecholamine surge** from a pheochromocytoma is safer when performed as a separate, initial stage.
*Medical management of pheochromocytoma then parathyroidectomy*
- While **alpha-blockade** is necessary, the question asks for the sequence of surgical interventions, where adrenalectomy must precede other operations.
- This patient presents with features suggestive of **MEN 2B**, which classically does not include hyperparathyroidism, unlike **MEN 1** or **MEN 2A**.
*Immediate thyroidectomy followed by staged procedures*
- Performing a **thyroidectomy** first is contraindicated because the stress of surgery and anesthesia can trigger a **pheochromocytoma crisis**.
- Even if medullary thyroid carcinoma is aggressive, the risk of immediate **intraoperative death** from pheochromocytoma takes precedence.
*Pancreatic surgery first due to mass effect*
- Although a **pancreatic head mass** is present (suggestive of MEN 1 overlap or separate pathology), it is not the immediate life-threatening priority.
- Operating on the pancreas before controlling and removing the **pheochromocytoma** exposes the patient to severe hemodynamic instability.
Endocrine surgery complications US Medical PG Question 8: A 38-year-old woman with primary hyperparathyroidism (calcium 11.8 mg/dL, PTH 185 pg/mL) has negative sestamibi scan and ultrasound. She desires surgical cure and has no medical contraindications. She has a Z-score of -2.8 on DEXA scan and a history of recurrent kidney stones. Evaluate the surgical approach and expected outcomes.
- A. Defer surgery until localization studies are positive
- B. Bilateral neck exploration with identification of all four glands (Correct Answer)
- C. Minimally invasive parathyroidectomy of the largest gland
- D. Medical management with cinacalcet and bisphosphonates
- E. Intraoperative PTH-guided focused exploration
Endocrine surgery complications Explanation: ***Bilateral neck exploration with identification of all four glands***
- When **preoperative localization** studies (Sestamibi and Ultrasound) are negative, a **bilateral neck exploration** is the gold standard to identify the source of primary hyperparathyroidism.
- This patient has clear indications for surgery including **nephrolithiasis**, a **Z-score of -2.8** (osteoporosis), and symptomatic hypercalcemia, making surgical intervention necessary despite negative imaging.
*Defer surgery until localization studies are positive*
- **Negative imaging** does not rule out primary hyperparathyroidism or contraindicate surgery when biochemical evidence is clear.
- Deferring treatment would risk further **bone loss** and recurrent **kidney stones** in a patient who already meets surgical criteria.
*Minimally invasive parathyroidectomy of the largest gland*
- **Minimally invasive parathyroidectomy (MIP)** requires precise preoperative localization to guide the surgeon to a specific quadrant.
- Attempting MIP without localization increases the risk of **surgical failure** and missing ectopic or multiglandular disease.
*Medical management with cinacalcet and bisphosphonates*
- **Medical management** is generally reserved for patients who are not surgical candidates or those who refuse surgery.
- While cinacalcet lowers **PTH** and calcium, it does not provide a **permanent cure** for the underlying adenoma or hyperplasia and is not the first-line choice for a young, fit patient.
*Intraoperative PTH-guided focused exploration*
- **Focused exploration** relies on knowing which side to explore first; without imaging, there is no target for a "focused" approach.
- While **intraoperative PTH** (ioPTH) monitoring is a useful adjunct to confirm cure, it does not replace the need for a comprehensive **bilateral search** when imaging is nonlocalizing.
Endocrine surgery complications US Medical PG Question 9: A 55-year-old woman presents with a 4 cm thyroid nodule. FNA shows Hurthle cell neoplasm (follicular variant). Preoperative ultrasound shows no lymphadenopathy. She undergoes thyroid lobectomy, and final pathology reveals a 3.8 cm Hurthle cell carcinoma with capsular invasion but no vascular invasion. Analyze the pathology findings and determine the next step in management.
- A. Completion thyroidectomy within 2 weeks (Correct Answer)
- B. Radioactive iodine ablation without further surgery
- C. Observation with ultrasound surveillance every 6 months
- D. External beam radiation therapy
- E. Prophylactic modified radical neck dissection
Endocrine surgery complications Explanation: ***Completion thyroidectomy within 2 weeks***
- For **Hurthle cell carcinoma** (HCC), a completion thyroidectomy is indicated when a malignancy is confirmed post-lobectomy, especially given HCC's aggressive nature and size approaching **4 cm**.
- Total thyroidectomy is necessary to facilitate future surveillance using **serum thyroglobulin** levels and to prepare for potential **radioactive iodine (RAI)** therapy if needed.
*Radioactive iodine ablation without further surgery*
- **Radioactive iodine (RAI)** therapy cannot be effectively performed if a remnant thyroid lobe is still present, as the normal tissue will sequester the iodine.
- **Hurthle cells** are historically less iodine-avid than other follicular cells, making surgical clearance of all thyroid tissue even more critical before considering RAI.
*Observation with ultrasound surveillance every 6 months*
- **Observation** is generally reserved for low-risk papillary microcarcinomas or minimally invasive follicular carcinomas <1-2 cm without high-risk features.
- The presence of **capsular invasion** and the histological subtype of **Hurthle cell carcinoma** in a 3.8 cm lesion represent a higher risk that mandates definitive surgical management.
*External beam radiation therapy*
- **External beam radiation** is not a primary treatment for localized Hurthle cell carcinoma and is typically reserved for **palliative care** or unresectable local recurrence.
- It does not replace the standard of care for surgical management of a resectable **thyroid malignancy**.
*Prophylactic modified radical neck dissection*
- **Prophylactic neck dissection** is not recommended for Hurthle cell carcinoma because it primarily spreads **hematogenously** rather than through lymphatic channels.
- Surgical management of the neck is only indicated if there is clinical or radiological evidence of **cervical lymphadenopathy**, which was absent in this patient.
Endocrine surgery complications US Medical PG Question 10: A 42-year-old woman with a family history of pheochromocytoma undergoes resection of a 5 cm right adrenal mass. Preoperatively, she was adequately alpha-blocked with phenoxybenzamine. During tumor manipulation, her blood pressure rises to 220/130 mmHg despite anesthesia deepening. Immediately after tumor removal, her blood pressure drops to 70/40 mmHg. Analyze the hemodynamic changes and determine management priorities.
- A. Immediate aggressive fluid resuscitation and vasopressors
- B. Continue phenoxybenzamine and observe
- C. Administer phentolamine for hypertensive crisis
- D. Emergency re-exploration for bleeding
- E. Decrease anesthesia depth and give beta-blockers
Endocrine surgery complications Explanation: ***Immediate aggressive fluid resuscitation and vasopressors***
- Sudden **hypotension** after tumor removal occurs because the body is no longer receiving the massive surge of **catecholamines** while existing **alpha-blockade** (phenoxybenzamine) persists.
- Management requires **large-volume intravenous fluids** to address pre-existing **volume depletion** and vasopressors to maintain mean arterial pressure until the vascular tone is restored.
*Continue phenoxybenzamine and observe*
- Phenoxybenzamine is a **non-competitive alpha-antagonist** used preoperatively to control hypertension; it has a long half-life and cannot be reversed quickly.
- Continuing observation without intervention in a patient with a blood pressure of **70/40 mmHg** would lead to organ malperfusion and **cardiovascular collapse**.
*Administer phentolamine for hypertensive crisis*
- Phentolamine is appropriate for managing the **intraoperative hypertensive surge** caused by tumor manipulation, but it is contraindicated once the patient is hypotensive.
- Giving a vasodilator during the post-resection **hypotensive phase** would exacerbate the low blood pressure and worsen the clinical state.
*Emergency re-exploration for bleeding*
- Although postoperative hemorrhage is a concern, the timing of this collapse matches the **physiologic withdrawal** of catecholamines precisely upon ligation of the adrenal vein.
- Hemodynamic instability should first be treated with **fluid boluses** and pressors; surgical re-exploration is reserved for confirmed cases of **hemoperitoneum**.
*Decrease anesthesia depth and give beta-blockers*
- Decreasing anesthesia depth may help slightly with blood pressure but is insufficient to counteract the loss of **endogenous vasopressors**.
- Giving **beta-blockers** in the setting of hypotension is dangerous as it reduces **cardiac output** and compensatory tachycardia, further decreasing blood pressure.
More Endocrine surgery complications US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.