Valve replacement and repair procedures US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Valve replacement and repair procedures. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
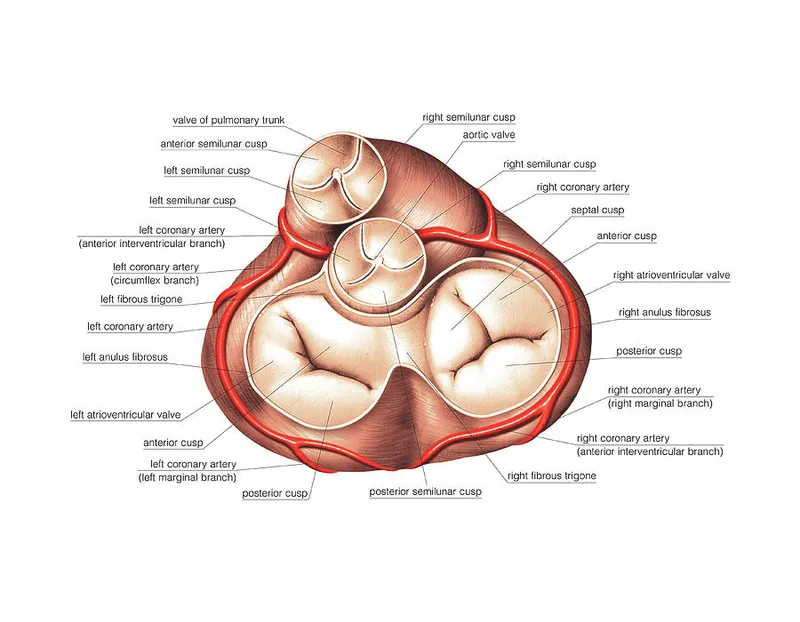
Valve replacement and repair procedures US Medical PG Question 1: A 58-year-old female presents to her primary care physician with complaints of chest pain and palpitations. A thorough past medical history reveals a diagnosis of rheumatic fever during childhood. Echocardiography is conducted and shows enlargement of the left atrium and narrowing of the mitral valve opening. Which of the following should the physician expect to hear on cardiac auscultation?
- A. Continuous, machine-like murmur
- B. Holosystolic murmur that radiates to the axilla
- C. Opening snap following S2 (Correct Answer)
- D. High-pitched, blowing decrescendo murmur in early diastole
- E. Mid-systolic click
Valve replacement and repair procedures Explanation: ***Opening snap following S2***
- The patient's history of **rheumatic fever** and echocardiographic findings of **left atrial enlargement** and **mitral valve narrowing** (mitral stenosis) are classic for this condition.
- An **opening snap** is a high-pitched, sharp sound that occurs shortly after **S2** (the second heart sound) and is pathognomonic for **mitral stenosis**, caused by the sudden tensing of the stenotic mitral valve leaflets as they open during diastole.
- The **S2-OS interval** indicates severity: a shorter interval suggests more severe stenosis.
*Continuous, machine-like murmur*
- This type of murmur is characteristic of a **patent ductus arteriosus (PDA)**, which is a congenital heart defect.
- The patient's symptoms and echocardiographic findings are not consistent with PDA.
*Holosystolic murmur that radiates to the axilla*
- This murmur describes **mitral regurgitation**, which is a leaky mitral valve. While rheumatic fever can cause mitral regurgitation, the echocardiogram shows **narrowing** of the mitral valve, not leakage.
- The radiation to the axilla is classical for the regurgitant jet flowing into the left atrium during systole.
*High-pitched, blowing decrescendo murmur in early diastole*
- This murmur is typical for **aortic regurgitation**, indicating a leaky aortic valve.
- The patient's presentation and echocardiogram findings specifically point to **mitral valve involvement** rather than aortic valve issues.
*Mid-systolic click*
- A **mid-systolic click** is characteristic of **mitral valve prolapse**, often followed by a late systolic murmur.
- The echocardiogram findings of **mitral valve narrowing** are not consistent with mitral valve prolapse.
Valve replacement and repair procedures US Medical PG Question 2: Cardiac muscle serves many necessary functions, leading to a specific structure that serves these functions. The structure highlighted is an important histology component of cardiac muscle. What would be the outcome if this structure diffusely failed to function?
- A. Failure of potassium channels to appropriately open to repolarize the cell
- B. Failure of propagation of the action potential from the conduction system (Correct Answer)
- C. Ineffective excitation-contraction coupling due to insufficient calcium ions
- D. Inappropriate formation of cardiac valve leaflets
- E. Outflow tract obstruction
Valve replacement and repair procedures Explanation: ***Failure of propagation of the action potential from the conduction system***
- The highlighted structure, the **intercalated disc**, contains **gap junctions** which are crucial for the rapid, synchronized spread of **action potentials** between cardiac muscle cells.
- A diffuse failure of these structures would prevent the coordinated electrical activation of the myocardium, leading to a failure of impulse propagation and **compromised cardiac contraction**.
*Failure of potassium channels to appropriately open to repolarize the cell*
- This scenario describes a problem with **ion channel function** within individual cardiomyocytes, affecting their repolarization phase.
- While critical for a single cell's electrical activity, it does not directly relate to the primary function of **intercalated discs** in *propagating* action potentials across multiple cells.
*Ineffective excitation-contraction coupling due to insufficient calcium ions*
- This outcome would result from issues with **calcium handling** mechanisms, such as problems with the **sarcoplasmic reticulum** or **calcium channels**, which are internal to the cardiomyocyte.
- It is distinct from the role of **intercalated discs** in facilitating intercellular communication and electrical spread.
*Inappropriate formation of cardiac valve leaflets*
- The formation of cardiac valve leaflets is an intricate process during **embryological development** involving specific signaling pathways and cell migration.
- This structural defect is not directly related to the function of **intercalated discs** in mature cardiac muscle, which are involved in electrical and mechanical coupling.
*Outflow tract obstruction*
- **Outflow tract obstruction** is a congenital or acquired structural defect affecting the major arteries leaving the heart (e.g., aortic or pulmonary stenosis).
- This is a macroscopic structural anomaly that is not caused by a primary failure of **intercalated disc** function.
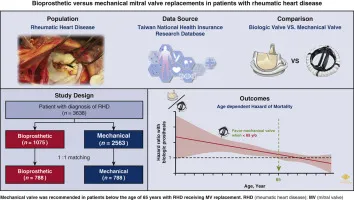
Valve replacement and repair procedures US Medical PG Question 3: A 63-year-old man comes to the physician for evaluation of fever and a nonproductive cough for the past 2 weeks. During this period, he has also had fatigue, myalgia, and difficulty breathing. Five weeks ago, he underwent an aortic prosthetic valve replacement due to high-grade aortic stenosis. The patient has a history of hypertension, asthma, and type 2 diabetes mellitus. A colonoscopy 2 years ago was normal. The patient has smoked one pack of cigarettes daily for the past 40 years. He has never used illicit drugs. Current medications include aspirin, warfarin, lisinopril, metformin, inhaled albuterol, and a multivitamin. The patient appears lethargic. Temperature is 38.6°C (101.5°F), pulse is 105/min, and blood pressure is 140/60 mm Hg. Rales are heard on auscultation of the lungs. A grade 2/6, diastolic blowing murmur is heard over the left sternal border and radiates to the right sternal border. A photograph of his right index finger is shown. Laboratory studies show a leukocyte count of 13,800/mm3 and an erythrocyte sedimentation rate of 48 mm/h. Which of the following is the most likely causal organism?
- A. Staphylococcus epidermidis (Correct Answer)
- B. Enterococcus faecalis
- C. Streptococcus gallolyticus
- D. Streptococcus pyogenes
- E. Viridans streptococci
Valve replacement and repair procedures Explanation: ***Staphylococcus epidermidis***
- This patient's **recent prosthetic valve replacement** makes him highly susceptible to infective endocarditis caused by *Staphylococcus epidermidis*, a common pathogen in **nosocomial infections** and on implanted devices.
- **Early prosthetic valve endocarditis** (within 2 months post-surgery, as in this case at 5 weeks) is most commonly caused by coagulase-negative staphylococci, particularly *S. epidermidis*, which colonize the valve during the perioperative period.
- The symptoms of fever, cough, fatigue, myalgia, difficulty breathing, and a new diastolic murmur, along with peripheral manifestations (shown in the photograph) and elevated inflammatory markers, are all consistent with infective endocarditis.
*Enterococcus faecalis*
- While *Enterococcus faecalis* can cause endocarditis, it is more commonly associated with **gastrointestinal or genitourinary procedures**, which are not indicated here.
- No recent urinary tract infection or GI instrumentation (colonoscopy was 2 years ago) points away from this organism.
*Streptococcus gallolyticus*
- Previously known as *Streptococcus bovis*, this organism is strongly associated with **colon cancer, inflammatory bowel disease, and colonic polyps**.
- The patient had a normal colonoscopy recently (2 years ago), making this less likely.
*Streptococcus pyogenes*
- *Streptococcus pyogenes* is known for causing **pharyngitis, scarlet fever, and rheumatic fever**, but it is a relatively uncommon cause of infective endocarditis, especially on prosthetic valves.
- There is no history of a recent streptococcal infection to suggest this pathogen.
*Viridans streptococci*
- **Viridans streptococci** are the most common cause of **native valve endocarditis**, often following dental procedures, but are less common in early prosthetic valve endocarditis compared to *S. epidermidis*.
- This patient had a prosthetic valve replacement 5 weeks ago, pointing more towards a nosocomial organism like *S. epidermidis*.
Valve replacement and repair procedures US Medical PG Question 4: A 38-year-old female presents to the emergency room with fevers, fatigue, and anorexia for over a month. Past medical history includes mild mitral valve prolapse. She underwent an uncomplicated tooth extraction approximately 6 weeks ago. Her vital signs include a temperature of 100.8 F, pulse of 83, blood pressure of 110/77, and SpO2 of 97% on room air. On exam, you note a grade III/VI holosystolic murmur at the apex radiating to the axilla as well as several red, painful nodules on her fingers. Which of the following is the next best course of action?
- A. Blood cultures are not needed. Start empiric antibiotics
- B. Start anticoagulation with heparin
- C. Consult cardiothoracic surgery for mitral valve replacement
- D. Obtain blood cultures x3 sites over 24 hours and start antibiotics after culture results are available
- E. Obtain blood cultures x3 sites over 1 hour and start empiric antibiotics (Correct Answer)
Valve replacement and repair procedures Explanation: ***Obtain blood cultures x3 sites over 1 hour and start empiric antibiotics***
- The patient's presentation with **fever, fatigue, anorexia, new murmur, and painful finger nodules (Osler's nodes)** after a recent dental procedure strongly suggests **infective endocarditis**. Prompt initiation of **empiric antibiotics** after obtaining adequate blood cultures is crucial to improve outcomes and prevent further complications like septic emboli or valvular damage.
- Obtaining **multiple blood cultures rapidly (e.g., three sets over 1 hour)** from different sites maximizes the chance of isolating the causative organism before antibiotics are given, enabling targeted therapy later, while minimizing delay to treatment.
*Blood cultures are not needed. Start empiric antibiotics*
- **Blood cultures are essential** for diagnosing infective endocarditis, identifying the causative organism, and guiding appropriate antibiotic therapy. Skipping blood cultures could lead to inappropriate antibiotic selection and treatment failure.
- While empiric antibiotics are warranted, they should always be initiated **after blood cultures** have been drawn to avoid sterilizing the blood and making microbial identification difficult.
*Start anticoagulation with heparin*
- **Anticoagulation is generally contraindicated** in infective endocarditis due to the increased risk of hemorrhagic complications, especially in cases of septic emboli to the brain.
- While patients with endocarditis can form vegetations that may embolize, the risks of **bleeding outweigh the benefits** of routine anticoagulation.
*Consult cardiothoracic surgery for mitral valve replacement*
- While **mitral valve prolapse** is a risk factor for endocarditis and severe valvular damage may eventually require surgery, primary management involves **antibiotic therapy**.
- Surgical intervention is typically reserved for cases with **severe valvular regurgitation/stenosis leading to heart failure**, uncontrolled infection despite antibiotics, or recurrent emboli, and is not the immediate next step.
*Obtain blood cultures x3 sites over 24 hours and start antibiotics after culture results are available*
- Waiting for **24 hours to collect blood cultures** would significantly delay the initiation of antibiotics, which is dangerous in a potentially life-threatening infection like endocarditis.
- Delaying antibiotics until **culture results are available** could take several days, leading to worsening infection, organ damage, and increased mortality. **Empiric antibiotics** must be started promptly after initial blood collection.
Valve replacement and repair procedures US Medical PG Question 5: Blood cultures are sent to the laboratory. Intravenous antibiotic therapy is started. Transesophageal echocardiography shows a large, oscillating vegetation attached to the tricuspid valve. There are multiple small vegetations attached to tips of the tricuspid valve leaflets. There is moderate tricuspid regurgitation. The left side of the heart and the ejection fraction are normal. Which of the following is the most likely causal organism of this patient's condition?
- A. Streptococcus sanguinis
- B. Staphylococcus aureus (Correct Answer)
- C. Enterococcus faecalis
- D. Neisseria gonorrhoeae
- E. Staphylococcus epidermidis
Valve replacement and repair procedures Explanation: ***Staphylococcus aureus***
- **_Staphylococcus aureus_** is the most common cause of **acute infective endocarditis**, particularly in intravenous drug users, which often affects the **tricuspid valve**.
- The presence of large, oscillating vegetations and **multiple small vegetations** on the tricuspid valve strongly suggests an aggressive infection, typical of _S. aureus_.
*Streptococcus sanguinis*
- _Streptococcus sanguinis_ is a common cause of **subacute infective endocarditis** in patients with pre-existing valvular disease but rarely causes acute, aggressive right-sided endocarditis.
- It's typically associated with **dental procedures** and usually affects the left side of the heart.
*Enterococcus faecalis*
- _Enterococcus faecalis_ can cause endocarditis, often associated with **genitourinary or gastrointestinal procedures**, and typically affects older men.
- While it can cause virulent endocarditis, it is less commonly associated with acute right-sided disease in this demographic compared to _S. aureus_.
*Neisseria gonorrhoeae*
- **_Neisseria gonorrhoeae_** is a rare cause of endocarditis, usually seen in younger, sexually active individuals, and often involves the aortic valve.
- While it can be acute, it is an extremely uncommon cause of **tricuspid valve endocarditis**.
*Staphylococcus epidermidis*
- **_Staphylococcus epidermidis_** is primarily associated with **prosthetic valve endocarditis** or foreign bodies, often presenting as a subacute infection.
- It rarely causes natural valve endocarditis, especially acute right-sided disease in this context.
Valve replacement and repair procedures US Medical PG Question 6: A 32-year-old woman is supposed to undergo tooth extraction surgery. Physical examination is unremarkable, and she has a blood pressure of 126/84 mm Hg and regular pulse of 72/min. She takes no medications. Which of the following cardiac conditions would warrant antibiotic prophylaxis to prevent infective endocarditis in this patient?
- A. Hypertrophic obstructive cardiomyopathy (HOCM)
- B. Mitral regurgitation
- C. Past history of infective endocarditis (Correct Answer)
- D. Ventricular septal defect (VSD)
- E. Implantable cardioverter defibrillator (ICD)
Valve replacement and repair procedures Explanation: ***Past history of infective endocarditis***
- A **history of infective endocarditis** is a definite indication for **antibiotic prophylaxis** before dental procedures that involve manipulation of gingival tissue, periapical region of teeth, or perforation of the oral mucosa due to the high risk of recurrence.
- This condition creates a predisposition to subsequent episodes of endocarditis, even with minor bacteremia.
*Hypertrophic obstructive cardiomyopathy (HOCM)*
- While HOCM is a significant cardiac condition, it is **no longer an indication** for routine infective endocarditis prophylaxis in the absence of other high-risk features like a prosthetic valve.
- Current guidelines have narrowed the criteria for prophylaxis due to the low absolute risk and potential for side effects from antibiotics.
*Mitral regurgitation*
- **Mitral valve regurgitation**, in the absence of a prosthetic valve or a previous history of endocarditis, generally **does not warrant antibiotic prophylaxis** for routine dental procedures.
- Only specific types of valvular heart disease with high risk (e.g., prosthetic valves, certain congenital heart diseases) require prophylaxis.
*Ventricular septal defect (VSD)*
- **Most ventricular septal defects do not require prophylaxis**. Only **unrepaired cyanotic VSD** or **repaired VSD with residual defects adjacent to prosthetic material** would warrant prophylaxis.
- Completely repaired VSDs without residual defects do not require prophylaxis after the initial 6 months post-repair.
- In this case, with an unremarkable physical examination and normal vital signs, there is no indication of cyanotic heart disease.
*Implantable cardioverter defibrillator (ICD)*
- An **implantable cardioverter defibrillator (ICD)** itself is a device and does not inherently increase the risk for infective endocarditis to warrant prophylaxis for dental procedures.
- The risk of infection is primarily associated with the device insertion procedure itself, not with subsequent dental interventions.
Valve replacement and repair procedures US Medical PG Question 7: A 61-year-old white man presents to the emergency department because of progressive fatigue and shortness of breath on exertion and while lying down. He has had type 2 diabetes mellitus for 25 years and hypertension for 15 years. He is taking metformin and captopril for his diabetes and hypertension. He has smoked 10 cigarettes per day for the past 12 years and drinks alcohol occasionally. His temperature is 36.7°C (98.0°F) and blood pressure is 130/60 mm Hg. On physical examination, his arterial pulse shows a rapid rise and a quick collapse. An early diastolic murmur is audible over the left upper sternal border. Echocardiography shows severe chronic aortic regurgitation with a left ventricular ejection fraction of 55%–60% and mild left ventricular hypertrophy. Which of the following is an indication for aortic valve replacement in this patient?
- A. Old age
- B. Ejection fraction > 55%
- C. Long history of diabetes mellitus
- D. Presence of symptoms of left ventricular dysfunction (Correct Answer)
- E. Long history of systemic hypertension
Valve replacement and repair procedures Explanation: ***Presence of symptoms of left ventricular dysfunction***
- The patient's symptoms of **progressive fatigue**, **shortness of breath on exertion**, and **orthopnea** (shortness of breath while lying down) are clear indicators of **left ventricular dysfunction** due to severe aortic regurgitation.
- In patients with **severe chronic aortic regurgitation**, the development of symptoms is a Class I indication for **aortic valve replacement**, regardless of the ejection fraction.
*Old age*
- While age can influence surgical risk, it is **not an independent indication** for aortic valve replacement in the absence of severe symptoms or significant ventricular dysfunction.
- The decision for surgery is primarily based on **symptom status** and objective measures of cardiac function.
*Ejection fraction > 55%*
- An ejection fraction of 55%-60% is considered **normal** or mildly reduced, indicating that the left ventricle still effectively pumps blood.
- Aortic valve replacement is typically indicated when the **ejection fraction falls below 50%**, even in asymptomatic patients, or with symptoms.
*Long history of diabetes mellitus*
- A long history of diabetes mellitus is a significant **comorbidity** that increases surgical risk and cardiovascular complications but is **not an independent indication** for valve replacement itself.
- The decision to operate is based on valve disease severity and its impact on cardiac function, not the duration of other chronic illnesses.
*Long history of systemic hypertension*
- Similar to diabetes, hypertension is a significant **comorbidity** that can exacerbate cardiac disease and increase surgical risk but does **not directly indicate** the need for aortic valve replacement.
- Hypertension management is crucial, but the primary indication for surgery stems from the **severity of aortic regurgitation** and its symptomatic consequences.
Valve replacement and repair procedures US Medical PG Question 8: A 45-year-old male is brought into the emergency room by emergency medical services due to a stab wound in the chest. The wound is located superior and medial to the left nipple. Upon entry, the patient appears alert and is conversational, but soon becomes confused and loses consciousness. The patient's blood pressure is 80/40 mmHg, pulse 110/min, respirations 26/min, and temperature 97.0 deg F (36.1 deg C). On exam, the patient has distended neck veins with distant heart sounds. What is the next best step to increase this patient's survival?
- A. Heparin
- B. Intravenous fluids
- C. Aspirin
- D. Intravenous colloids
- E. Pericardiocentesis (Correct Answer)
Valve replacement and repair procedures Explanation: ***Pericardiocentesis***
- The patient's presentation with **hypotension**, **tachycardia**, **distended neck veins**, and **distant heart sounds** after a chest stab wound is classic for **cardiac tamponade** (Beck's triad).
- **Pericardiocentesis** is the immediate life-saving procedure to drain the pericardial fluid and relieve pressure on the heart, improving cardiac output.
- In penetrating trauma, this serves as a **bridge to definitive surgical management** (thoracotomy or sternotomy).
*Heparin*
- **Heparin** is an anticoagulant and would worsen the situation by increasing bleeding into the pericardial space due to the stab wound.
- It is contraindicated in active bleeding and traumatic injury.
*Intravenous fluids*
- While **IV fluid resuscitation is recommended** in cardiac tamponade to maintain preload and support cardiac output, fluids alone **do not address the underlying mechanical obstruction**.
- The primary issue is **extrinsic compression of the heart** requiring drainage, not hypovolemia alone.
- Fluids are supportive but not definitive—**pericardiocentesis is the life-saving intervention**.
*Aspirin*
- **Aspirin** is an antiplatelet agent and would increase the risk of bleeding, exacerbating the patient's condition.
- It is used for conditions like myocardial infarction or stroke prevention, not for acute traumatic bleeding.
*Intravenous colloids*
- Similar to crystalloid fluids, **colloids** may provide temporary hemodynamic support but do not relieve the mechanical compression of the heart.
- They are supportive measures that **do not substitute for definitive pericardial drainage**.
Valve replacement and repair procedures US Medical PG Question 9: A 67-year-old man presents to the emergency department with abdominal pain that started 1 hour ago. The patient has a past medical history of diabetes and hypertension as well as a 40 pack-year smoking history. His blood pressure is 107/58 mmHg, pulse is 130/min, respirations are 23/min, and oxygen saturation is 98% on room air. An abdominal ultrasound demonstrates focal dilation of the aorta with peri-aortic fluid. Which of the following is the best next step in management?
- A. Serial annual abdominal ultrasounds
- B. Emergent surgical intervention (Correct Answer)
- C. Administer labetalol
- D. Counsel the patient in smoking cessation
- E. Urgent surgery within the next day
Valve replacement and repair procedures Explanation: ***Emergent surgical intervention***
- The patient's presentation with acute **abdominal pain**, **hypotension**, and **tachycardia** combined with ultrasound findings of focal aortic dilation and peri-aortic fluid strongly suggests a **ruptured abdominal aortic aneurysm (AAA)**.
- A ruptured AAA is a life-threatening emergency requiring immediate surgical repair to prevent further hemorrhage and death.
*Serial annual abdominal ultrasounds*
- This approach is appropriate for asymptomatic patients with smaller, stable AAAs (typically <5.5 cm) to monitor for growth.
- In this case, the patient is symptomatic with signs of rupture, making surveillance an inappropriate and dangerous management strategy.
*Administer labetalol*
- Medications like labetalol are used to control blood pressure in conditions like aortic dissection or to slow the progression of AAAs, but they are contraindicated in hypotensive patients with a ruptured AAA.
- In this patient, labetalol would worsen the existing hypotension and could lead to cardiovascular collapse.
*Counsel the patient in smoking cessation*
- Smoking cessation is a crucial long-term intervention to reduce the risk of AAA expansion and rupture.
- While important, it does not address the immediate, life-threatening emergency of a ruptured AAA.
*Urgent surgery within the next day*
- Waiting until the next day for surgery in a patient with a suspected ruptured AAA is unacceptable.
- The patient's hemodynamic instability (hypotension, tachycardia) indicates active bleeding, and any delay significantly increases morbidity and mortality.
Valve replacement and repair procedures US Medical PG Question 10: A 70-year-old man with severe ischemic cardiomyopathy (EF 25%) has recurrent ventricular tachycardia despite optimal medical therapy and ICD placement. Cardiac MRI shows a large anteroseptal scar with viable myocardium in the lateral and inferior walls. He has three-vessel coronary disease. His daughter is advocating for heart transplantation, but he has multiple comorbidities including obesity (BMI 37) and active tobacco use. Evaluate the management priority and rationale.
- A. Left ventricular assist device as destination therapy
- B. Catheter ablation of VT with continued ICD monitoring
- C. Cardiac resynchronization therapy upgrade and medication adjustment
- D. List for heart transplantation immediately given severe cardiomyopathy
- E. CABG with surgical ventricular reconstruction and continued medical optimization (Correct Answer)
Valve replacement and repair procedures Explanation: ***CABG with surgical ventricular reconstruction and continued medical optimization***
- The patient has **three-vessel disease** and **viable myocardium** in the lateral and inferior walls; **CABG** addresses the ischemic substrate and potentially improves **LVEF**.
- **Surgical ventricular reconstruction (SVR)** addresses the large **anteroseptal scar**, reducing left ventricular volume and providing better geometric stability to mitigate **ventricular tachycardia** (VT).
*Left ventricular assist device as destination therapy*
- While **LVAD** is an option for end-stage heart failure, the presence of **active tobacco use** and **obesity** (BMI 37) are significant relative contraindications.
- **Surgical revascularization** is prioritized when significant **viable myocardium** is present and surgical targets are available.
*Catheter ablation of VT with continued ICD monitoring*
- **VT ablation** target-treats the arrhythmia but does not address the underlying **remodelling** or **ischemia** causing the progressive cardiomyopathy.
- Given the **three-vessel disease**, surgical intervention is more comprehensive for long-term prognosis compared to percutaneous ablation alone.
*Cardiac resynchronization therapy upgrade and medication adjustment*
- The patient is already on **optimal medical therapy** with an **ICD**; simple medication adjustment is unlikely to control recurrent VT in the setting of structural scar and ischemia.
- **CRT** provides limited benefit if the primary issue is a large **anteroseptal scar** and **active ischemia** requiring revascularization.
*List for heart transplantation immediately given severe cardiomyopathy*
- Direct listing is contraindicated due to **active tobacco use** and a **BMI >35**, which are standard exclusion criteria for transplant programs.
- Heart transplantation is considered a last resort after maximizing options like **revascularization** and addressing **modifiable risk factors**.
More Valve replacement and repair procedures US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.