Thoracotomy approaches and techniques US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Thoracotomy approaches and techniques. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Thoracotomy approaches and techniques US Medical PG Question 1: A 79-year-old man is admitted to the intensive care unit for hospital acquired pneumonia, a COPD flare, and acute heart failure requiring intubation and mechanical ventilation. On his first night in the intensive care unit, his temperature is 99.7°F (37.6°C), blood pressure is 107/58 mm Hg, and pulse is 150/min which is a sudden change from his previous vitals. Physical exam is notable for jugular venous distension and a rapid heart rate. The ventilator is checked and is functioning normally. Which of the following is the best next step in management for the most likely diagnosis?
- A. Tube thoracostomy
- B. FAST exam
- C. Needle thoracostomy (Correct Answer)
- D. Chest radiograph
- E. Thoracotomy
Thoracotomy approaches and techniques Explanation: ***Needle thoracostomy***
- The patient's sudden deterioration with **tachycardia**, **hypotension**, and **jugular venous distension** (JVD) in the setting of positive pressure ventilation strongly suggests a **tension pneumothorax**.
- **Needle decompression** is the immediate life-saving intervention for suspected tension pneumothorax, as delaying treatment for diagnostic imaging could be fatal.
*Tube thoracostomy*
- While a **tube thoracostomy** (chest tube insertion) is the definitive treatment for pneumothorax, it requires more time and resources than needle decompression.
- In a true emergency with signs of tension, needle decompression should be performed first to stabilize the patient, followed by a chest tube.
*FAST exam*
- A **Focused Assessment with Sonography for Trauma (FAST) exam** is primarily used to detect free fluid (usually blood) in the abdomen or pericardium in trauma patients.
- While it can sometimes identify pneumothorax, it is not the fastest or most direct intervention for a suspected tension pneumothorax causing hemodynamic instability.
*Chest radiograph*
- A **chest radiograph (CXR)** is the standard diagnostic tool for pneumothorax, but obtaining and interpreting it would delay urgent intervention in a hemodynamically unstable patient with suspected tension pneumothorax.
- The diagnosis of tension pneumothorax is primarily clinical; treatment should not wait for imaging.
*Thoracotomy*
- A **thoracotomy** is a major surgical procedure involving opening the chest, typically reserved for severe trauma, massive hemorrhage, or complex thoracic issues.
- It is an overly aggressive and inappropriate initial intervention for a suspected tension pneumothorax.
Thoracotomy approaches and techniques US Medical PG Question 2: A 60-year-old man comes to the clinic complaining of a persistent cough for the last few months. His cough started gradually about a year ago, and it became more severe and persistent despite all his attempts to alleviate it. During the past year, he also noticed some weight loss and a decrease in his appetite. He also complains of progressive shortness of breath. He has a 40-pack-year smoking history but is a nonalcoholic. Physical examination findings are within normal limits. His chest X-ray shows a mass in the right lung. A chest CT shows a 5 cm mass with irregular borders near the lung hilum. A CT guided biopsy is planned. During the procedure, just after insertion of the needle, the patient starts to feel pain in his right shoulder. Which of the following nerves is responsible for his shoulder pain?
- A. Thoracic spinal nerves
- B. Phrenic nerve (Correct Answer)
- C. Vagus nerve
- D. Pulmonary plexus
- E. Intercostal nerves
Thoracotomy approaches and techniques Explanation: **Phrenic nerve**
- The **phrenic nerve** innervates the diaphragm and also carries sensory fibers from the **mediastinal and diaphragmatic pleura**, as well as the **pericardium**.
- Irritation of the phrenic nerve, due to its **C3-C5 cervical origin**, can cause **referred pain to the ipsilateral shoulder** or neck.
*Thoracic spinal nerves*
- These nerves primarily serve the **intercostal muscles** and skin of the chest wall.
- While they can transmit pain from the chest wall, they are not typically associated with **referred shoulder pain** from intrathoracic structures.
*Vagus nerve*
- The **vagus nerve** provides parasympathetic innervation to many thoracic and abdominal organs and carries visceral afferents.
- It plays a role in regulating lung function but does not transmit sensory information that would be perceived as **shoulder pain** from diaphragmatic irritation.
*Pulmonary plexus*
- The **pulmonary plexus** is formed by branches of the vagus and sympathetic nerves, primarily involved in regulating **bronchial and vascular tone** in the lungs.
- It does not transmit sensory input that would cause referred pain to the shoulder.
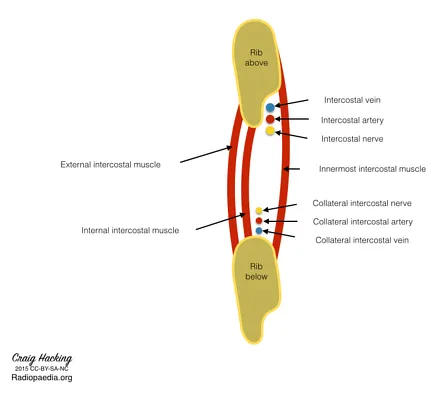
*Intercostal nerves*
- These nerves run along the ribs and innervate the **intercostal muscles** and skin of the **thoracic wall**.
- Pain from these nerves would typically be felt along the **rib cage** or chest wall, not as referred shoulder pain.
Thoracotomy approaches and techniques US Medical PG Question 3: A 27-year-old man presents to the emergency department with severe dyspnea and sharp chest pain that suddenly started an hour ago after he finished exercising. He has a history of asthma as a child, and he achieves good control of his acute attacks with Ventolin. On examination, his right lung field is hyperresonant along with diminished lung sounds. Chest wall motion during respiration is asymmetrical. His blood pressure is 105/67 mm Hg, respirations are 22/min, pulse is 78/min, and temperature is 36.7°C (98.0°F). The patient is supported with oxygen, given corticosteroids, and has had analgesic medications via a nebulizer. Considering the likely condition affecting this patient, what is the best step in management?
- A. CT scan
- B. ABG
- C. Chest X-rays (Correct Answer)
- D. Tube insertion
- E. Sonogram
Thoracotomy approaches and techniques Explanation: ***Chest X-rays***
- The patient's presentation with **sudden onset dyspnea** and **sharp chest pain** post-exercise, along with **hyperresonance** and **diminished lung sounds** in the right lung field, is highly suggestive of a **spontaneous pneumothorax**.
- However, the patient is **hemodynamically stable** (BP 105/67, HR 78/min) with no signs of tension physiology (no severe hypotension, marked tachycardia, or cardiovascular collapse).
- In a stable patient with suspected pneumothorax, **chest X-ray is the appropriate first step** to confirm the diagnosis, determine the size of the pneumothorax, and guide subsequent management (observation for small pneumothorax <20%, aspiration, or tube thoracostomy for larger pneumothoraces).
- Immediate intervention without imaging is reserved for unstable patients with tension pneumothorax.
*Tube insertion*
- Chest tube insertion is the definitive treatment for large pneumothoraces (>20%) or hemodynamically unstable patients with tension pneumothorax.
- In this **stable patient**, proceeding directly to tube insertion without imaging confirmation would be premature and not following standard of care.
- The diagnosis should be confirmed and the size estimated via chest X-ray before determining if tube thoracostomy is necessary.
*CT scan*
- CT scan is not indicated as the initial diagnostic test for suspected pneumothorax.
- It provides more detail than needed for this clinical scenario and causes unnecessary delay and radiation exposure when chest X-ray is sufficient.
- CT may be useful for detecting small pneumothoraces not visible on X-ray or evaluating underlying lung disease, but is not the first-line test.
*ABG*
- An Arterial Blood Gas (ABG) might show hypoxia and respiratory alkalosis, providing information about gas exchange.
- However, ABG does not confirm the diagnosis of pneumothorax or guide immediate management decisions.
- It is an adjunctive test that does not take priority over diagnostic imaging in this scenario.
*Sonogram*
- Lung ultrasound can rapidly detect pneumothorax by showing absent lung sliding and is increasingly used in emergency settings, particularly for bedside evaluation.
- While potentially useful, **chest X-ray remains the standard initial imaging modality** for suspected pneumothorax in most emergency departments, as it provides clear documentation of pneumothorax size and is more universally available and interpreted.
- Ultrasound may be preferred in specific situations (unstable patients, point-of-care evaluation), but chest X-ray is the conventional first-line imaging test.
Thoracotomy approaches and techniques US Medical PG Question 4: A 24-year-old man is brought to the emergency department after being involved in a motor vehicle accident as an unrestrained driver. He was initially found unconscious at the scene but, after a few minutes, he regained consciousness. He says he is having difficulty breathing and has right-sided pleuritic chest pain. A primary trauma survey reveals multiple bruises and lacerations on the anterior chest wall. His temperature is 36.8°C (98.2°F), blood pressure is 100/60 mm Hg, pulse is 110/min, and respiratory rate is 28/min. Physical examination reveals a penetrating injury just below the right nipple. Cardiac examination is significant for jugular venous distention. There is also an absence of breath sounds on the right with hyperresonance to percussion. A bedside chest radiograph reveals evidence of a collapsed right lung with depression of the right hemidiaphragm and tracheal deviation to the left. Which of the following is the most appropriate next step in the management of this patient?
- A. Tube thoracostomy at the 2nd intercostal space, midclavicular line
- B. Tube thoracostomy at the 5th intercostal space, midclavicular line
- C. Tube thoracostomy at the 5th intercostal space, anterior axillary line
- D. Needle thoracostomy at the 5th intercostal space, midclavicular line
- E. Needle thoracostomy at the 2nd intercostal space, midclavicular line (Correct Answer)
Thoracotomy approaches and techniques Explanation: **Needle thoracostomy at the 2nd intercostal space, midclavicular line**
- The patient presents with classic signs of **tension pneumothorax**, including respiratory distress, hypotension, tachycardia, jugular venous distention, absent breath sounds, hyperresonance to percussion, tracheal deviation away from the affected side, and mediastinal shift.
- **Needle thoracostomy** in the 2nd intercostal space at the midclavicular line is the most appropriate *initial* life-saving intervention for tension pneumothorax, as it rapidly decompresses the pleural space.
*Tube thoracostomy at the 2nd intercostal space, midclavicular line*
- While a **tube thoracostomy (chest tube insertion)** is the definitive treatment for pneumothorax, it is not the immediate first step for a **tension pneumothorax** due to the time constraint and the need for immediate decompression.
- The 2nd intercostal space, midclavicular line, is an appropriate site for needle decompression, but a chest tube is typically inserted at a different location (5th intercostal space, anterior axillary line).
*Tube thoracostomy at the 5th intercostal space, midclavicular line*
- This location is not the standard site for either needle decompression or definitive chest tube insertion. The **midaxillary or anterior axillary line** is preferred for chest tube placement to avoid neurovascular bundles.
- Again, while a chest tube is needed, it is not the *immediate* first step for a **tension pneumothorax**.
*Tube thoracostomy at the 5th intercostal space, anterior axillary line*
- This is the **correct anatomical location** for definitive chest tube insertion for a pneumothorax or hemothorax.
- However, in the setting of acute **tension pneumothorax**, **needle decompression** is required first to rapidly decompress the intrathoracic pressure and stabilize the patient before a chest tube can be placed.
*Needle thoracostomy at the 5th intercostal space, midclavicular line*
- The **5th intercostal space** is too low for an effective needle decompression of a tension pneumothorax.
- The standard site for needle decompression of a tension pneumothorax is the **2nd intercostal space, midclavicular line**, due to its safety and effectiveness in accessing the pleural space.
Thoracotomy approaches and techniques US Medical PG Question 5: A 14-year-old boy is brought to the emergency department because of acute left-sided chest pain and dyspnea following a motor vehicle accident. His pulse is 122/min and blood pressure is 85/45 mm Hg. Physical examination shows distended neck veins and tracheal displacement to the right side. The left chest is hyperresonant to percussion and there are decreased breath sounds. This patient would most benefit from needle insertion at which of the following anatomical sites?
- A. 5th left intercostal space along the midclavicular line
- B. 8th left intercostal space along the posterior axillary line
- C. 2nd left intercostal space along the midclavicular line (Correct Answer)
- D. Subxiphoid space in the left sternocostal margin
- E. 5th left intercostal space along the midaxillary line
Thoracotomy approaches and techniques Explanation: ***2nd left intercostal space along the midclavicular line***
- The patient's symptoms (chest pain, dyspnea, hypotension, distended neck veins, tracheal deviation, hyperresonance, and decreased breath sounds on the left) are classic signs of a **tension pneumothorax**.
- Immediate treatment for **tension pneumothorax** involves needle decompression at the **2nd intercostal space** in the midclavicular line to relieve pressure and restore hemodynamic stability.
*5th left intercostal space along the midclavicular line*
- This location is typically used for **chest tube insertion** in a more controlled setting, not for emergent needle decompression of a tension pneumothorax.
- While it's a safe location for pleural access, it is not the **first-line site** for immediate life-saving decompression.
*8th left intercostal space along the posterior axillary line*
- This site is too low and posterior for effective needle decompression of a tension pneumothorax, which requires rapid access to the **apex of the lung**.
- It is more commonly used for **thoracentesis** to drain fluid from the pleural cavity.
*Subxiphoid space in the left sternocostal margin*
- This location is primarily used for **pericardiocentesis** to drain fluid from the pericardial sac in cases of cardiac tamponade.
- It is not appropriate for addressing a **pneumothorax**, which involves air in the pleural space.
*5th left intercostal space along the midaxillary line*
- This site is a common alternative for **chest tube insertion** but is not the preferred or most immediate site for needle decompression of a tension pneumothorax.
- While it offers pleural access, the **2nd intercostal space** anteriorly is chosen for expediency and safety in an emergency.
Thoracotomy approaches and techniques US Medical PG Question 6: An 18-year-old man is brought to the emergency department 30 minutes after being stabbed in the chest during a fight. He has no other injuries. His pulse is 120/min, blood pressure is 90/60 mm Hg, and respirations are 22/min. Examination shows a 4-cm deep, straight stab wound in the 4th intercostal space 2 cm medial to the right midclavicular line. The knife most likely passed through which of the following structures?
- A. Serratus anterior muscle, pleura, inferior vena cava
- B. External oblique muscle, superior epigastric artery, azygos vein
- C. Pectoralis minor muscle, dome of the diaphragm, right lobe of the liver
- D. Intercostal muscles, internal thoracic artery, right heart
- E. Pectoral fascia, transversus thoracis muscle, right lung (Correct Answer)
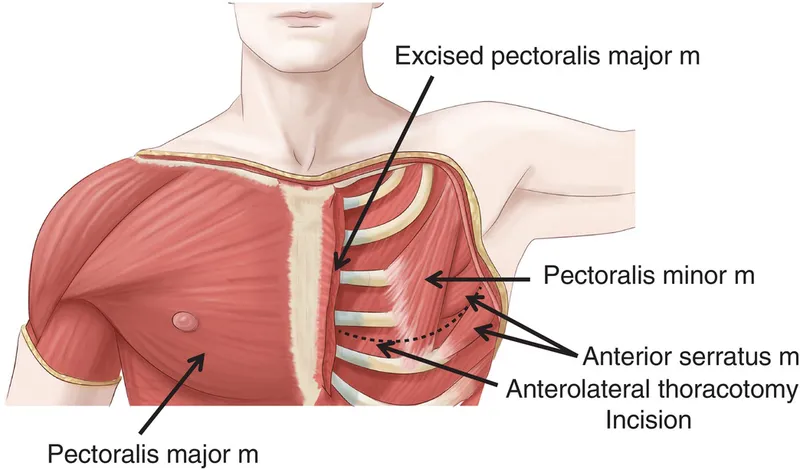
Thoracotomy approaches and techniques Explanation: ***Pectoral fascia, transversus thoracis muscle, right lung***
* The stab wound is in the **4th intercostal space**, 2 cm medial to the right midclavicular line, placing it over the anterior chest wall. This trajectory would first penetrate the **pectoral fascia**.
* Deeper structures in this region include the **transversus thoracis muscle** and, given the depth, the **right lung** as it extends superiorly behind the anterior chest wall.
* *Serratus anterior muscle, pleura, inferior vena cava*
* The **serratus anterior muscle** is more laterally positioned, typically covering the side of the rib cage.
* The **inferior vena cava** is located more medially and posteriorly within the mediastinum, deep to the diaphragm, making it an unlikely target for an anterior 4th intercostal stab.
* *External oblique muscle, superior epigastric artery, azygos vein*
* The **external oblique muscle** is part of the abdominal wall and would not be penetrated in the 4th intercostal space.
* The **superior epigastric artery** is lower, typically extending into the abdominal wall, and the **azygos vein** is in the posterior mediastinum, not in the path of this superficial anterior stab wound.
* *Pectoralis minor muscle, dome of the diaphragm, right lobe of the liver*
* The **pectoralis minor muscle** is located deep to the pectoralis major, which would be penetrated. However, a stab at the 4th intercostal space would be too high to directly involve the **dome of the diaphragm** or the **right lobe of the liver**, which are typically below the 5th intercostal space, especially in forced expiration.
* *Intercostal muscles, internal thoracic artery, right heart*
* The **intercostal muscles** would certainly be traversed.
* However, the **internal thoracic artery** runs paramedially (about 1-2 cm from the sternum), and getting to the **right heart** would require a more medial and deeper trajectory, potentially causing immediate tamponade or severe hemorrhage.
Thoracotomy approaches and techniques US Medical PG Question 7: A 68-year-old man comes to the physician because of a 4-month history of difficulty swallowing. During this time, he has also had a 7-kg (15-lb) weight loss. Esophagogastroduodenoscopy shows an exophytic mass in the distal third of the esophagus. Histological examination of a biopsy specimen shows a well-differentiated adenocarcinoma. The patient is scheduled for surgical resection of the tumor. During the procedure, the surgeon damages a structure that passes through the diaphragm along with the esophagus at the level of the tenth thoracic vertebra (T10). Which of the following structures was most likely damaged?
- A. Azygos vein
- B. Vagus nerve (Correct Answer)
- C. Right phrenic nerve
- D. Inferior vena cava
- E. Thoracic duct
Thoracotomy approaches and techniques Explanation: ***Vagus nerve***
- The **esophagus** passes through the diaphragm at the level of the **T10 vertebra**, accompanied by the **anterior and posterior vagal trunks**. Damage to these nerves is a known complication of esophageal surgery.
- The vagus nerves provide **parasympathetic innervation** to the gastrointestinal tract, and their close proximity to the esophagus makes them vulnerable during tumor resection.
*Azygos vein*
- The **azygos vein** typically passes through the diaphragm at the level of **T12** through the **aortic hiatus**, not with the esophagus at T10.
- It drains into the superior vena cava and is located more posteriorly in the mediastinum.
*Right phrenic nerve*
- The **right phrenic nerve** passes through the diaphragm with the **inferior vena cava** at the level of **T8**, innervating the diaphragm.
- It is located more anteriorly and laterally to the esophagus, making direct damage during esophageal surgery less likely than the vagus nerves.
*Inferior vena cava*
- The **inferior vena cava (IVC)** passes through its own opening in the central tendon of the diaphragm at the level of **T8**, not with the esophagus at T10.
- Damage to the IVC would result in significant hemorrhage and is typically a separate surgical concern.
*Thoracic duct*
- The **thoracic duct** passes through the **aortic hiatus** at the level of **T12** along with the aorta, collecting lymph from most of the body.
- Its location makes it less likely to be damaged during a standard esophageal resection at T10 compared to the vagus nerves.
Thoracotomy approaches and techniques US Medical PG Question 8: A 45-year-old woman undergoes a modified radical mastectomy for breast cancer. Following the procedure, she experiences numbness in the medial aspect of her upper arm. Which of the following nerves was most likely injured during the surgery?
- A. Musculocutaneous nerve
- B. Thoracodorsal nerve
- C. Long thoracic nerve
- D. Intercostobrachial nerve (Correct Answer)
Thoracotomy approaches and techniques Explanation: ***Intercostobrachial nerve***
- The **intercostobrachial nerve** provides sensory innervation to the **medial aspect of the upper arm** and is vulnerable to injury during **axillary dissection** in a modified radical mastectomy [1].
- Injury typically results in **numbness** or **paresthesia** in this specific dermatomal distribution [1].
*Musculocutaneous nerve*
- The **musculocutaneous nerve** innervates the muscles of the **anterior compartment of the arm** (e.g., biceps brachii) and provides sensation to the **lateral forearm**.
- Damage would primarily affect **forearm sensation** and arm flexion, not medial upper arm sensation.
*Thoracodorsal nerve*
- The **thoracodorsal nerve** innervates the **latissimus dorsi muscle**, a large muscle of the back and shoulder [1].
- Injury would lead to **weakness in adduction, extension, and internal rotation** of the arm, with no sensory deficit in the upper arm [1].
*Long thoracic nerve*
- The **long thoracic nerve** innervates the **serratus anterior muscle**, which stabilizes the scapula and allows for arm abduction above 90 degrees.
- Injury results in **"winged scapula,"** making it difficult to raise the arm overhead, without sensory loss in the upper arm.
Thoracotomy approaches and techniques US Medical PG Question 9: A 62-year-old man comes to the physician for a follow-up examination after having been diagnosed with stage II adenocarcinoma of the left lower lung lobe without evidence of distant metastases 1 week ago following an evaluation for a chronic cough. He has hypertension and type 2 diabetes mellitus. He has smoked one pack of cigarettes daily for the past 40 years. His current medications include metformin, sitagliptin, and enalapril. He is 177 cm (5 ft 10 in) tall and weighs 65 kg (143 lb); BMI is 20.7 kg/m2. He appears lethargic. Vital signs are within normal limits. Pulse oximetry shows an oxygen saturation of 98%. Examination shows inspiratory wheezing at the left lung base. The remainder of the examination shows no abnormalities. A complete blood count and serum concentrations of electrolytes, creatinine, glucose, and liver enzymes are within the reference range. Spirometry shows an FEV1 of 1.6 L. The diffusing lung capacity for carbon monoxide (DLCO) is 66% of predicted. Which of the following is the most appropriate next step in the management of this patient?
- A. Schedule lobectomy (Correct Answer)
- B. Administer cisplatin and vinorelbine
- C. Schedule a wedge resection
- D. Administer cisplatin and etoposide
- E. Radiation therapy
Thoracotomy approaches and techniques Explanation: ***Schedule lobectomy***
- The patient has **stage II non-small cell lung cancer (adenocarcinoma)** without distant metastases, making surgical resection with **lobectomy** the treatment of choice for curative intent.
- While pulmonary function is somewhat impaired (FEV1 and DLCO), his overall status, age, and normal labs suggest he can likely tolerate the procedure.
*Administer cisplatin and vinorelbine*
- This combination is a common regimen for **adjuvant chemotherapy** following surgical resection in certain stages of NSCLC, or for advanced unresectable disease.
- It is not the primary treatment for a resectable stage II cancer; **surgery is preferred for cure**.
*Schedule a wedge resection*
- A **wedge resection** (sublobar resection) is typically reserved for patients with very small, peripheral tumors or those with severe comorbidities that preclude lobectomy due to poor pulmonary function.
- Given the patient's stage II disease and potentially curative intent, a **lobectomy is generally preferred** for better oncologic outcomes.
*Administer cisplatin and etoposide*
- This chemotherapy regimen is more commonly used for **small cell lung cancer (SCLC)** or for some advanced NSCLC cases, not typically for resectable stage II adenocarcinoma as a primary treatment.
- Even if used in NSCLC, it would usually be in the context of advanced disease or as part of a neoadjuvant/adjuvant approach with surgery, not as a standalone initial treatment for resectable disease.
*Radiation therapy*
- **Radiation therapy** is often used for inoperable tumors, for patients who refuse surgery, or as an adjuvant treatment.
- For a resectable stage II NSCLC, **surgery offers the best chance for cure**, making radiation therapy alone less appropriate as the first-line definitive treatment strategy.
Thoracotomy approaches and techniques US Medical PG Question 10: A 63-year-old man is brought to the emergency department, 30 minutes after being involved in a high-speed motor vehicle collision. He is obtunded on arrival. He is intubated and mechanical ventilation is begun. The ventilator is set at a FiO2 of 60%, tidal volume of 440 mL, and positive end-expiratory pressure of 4 cm H2O. On the third day of intubation, his temperature is 37.3°C (99.1°F), pulse is 91/min, and blood pressure is 103/60 mm Hg. There are decreased breath sounds over the left lung base. Cardiac examination shows no abnormalities. The abdomen is soft and not distended. Arterial blood gas analysis shows:
pH 7.49
pCO2 29 mm Hg
pO2 73 mm Hg
HCO3- 20 mEq/L
O2 saturation 89%
Monitoring shows a sudden increase in the plateau airway pressure. An x-ray of the chest shows deepening of the costophrenic angle on the left side. Which of the following is the most appropriate next step in management?
- A. CT scan of the chest
- B. Administer levofloxacin
- C. Close observation
- D. Increase the PEEP
- E. Insertion of a chest tube (Correct Answer)
Thoracotomy approaches and techniques Explanation: ***Insertion of a chest tube***
- The sudden increase in **plateau airway pressure**, decreased breath sounds over the left lung base, worsening hypoxemia (O2 sat 89%) despite high FiO2, and **deepening of the costophrenic angle on the left side** indicate a **traumatic hemothorax**.
- Deepening of the costophrenic angle on chest X-ray is a classic sign of **pleural fluid accumulation** (hemothorax or pleural effusion), not pneumothorax.
- In a trauma patient (high-speed motor vehicle collision) on day 3 of mechanical ventilation, this represents a **delayed hemothorax** requiring immediate drainage.
- **Chest tube insertion** is the definitive management to evacuate blood, re-expand the lung, and improve ventilation and oxygenation.
*CT scan of the chest*
- While CT scan would provide detailed anatomical information, the clinical presentation with sudden respiratory decompensation and clear chest X-ray findings of hemothorax requires **immediate intervention**.
- Delaying treatment to obtain CT imaging in an unstable ventilated patient could worsen hypoxemia and lead to cardiovascular compromise.
- CT scan may be obtained later if needed to evaluate for ongoing bleeding or other injuries.
*Administer levofloxacin*
- Antibiotics would be appropriate for **pneumonia or empyema**, but the patient has no clear signs of infection (afebrile at 37.3°C, acute presentation over hours not days).
- The primary problem is **mechanical compression** from pleural fluid accumulation, not infection.
- Antibiotics do not address the life-threatening respiratory compromise from hemothorax.
*Close observation*
- Close observation is inappropriate given the acute deterioration with increased plateau pressures and worsening hypoxemia.
- The patient requires urgent intervention to prevent further respiratory failure and potential cardiovascular collapse.
- Expectant management would be negligent in this clinical scenario.
*Increase the PEEP*
- Increasing **Positive End-Expiratory Pressure (PEEP)** would worsen the situation by increasing intrathoracic pressure against an already compressed lung.
- Higher PEEP could impair venous return, decrease cardiac output, and potentially convert a simple hemothorax to a tension physiology.
- PEEP adjustments do not address the underlying problem of pleural space fluid accumulation requiring drainage.
More Thoracotomy approaches and techniques US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.