Mediastinal masses evaluation and management US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Mediastinal masses evaluation and management. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Mediastinal masses evaluation and management US Medical PG Question 1: During a thoracotomy procedure, a surgeon needs to access the posterior mediastinum. Which of the following structures forms the anterior boundary of the posterior mediastinum?
- A. Descending thoracic aorta
- B. Pericardial sac (Correct Answer)
- C. Azygos vein
- D. Thoracic vertebrae
- E. Sternum
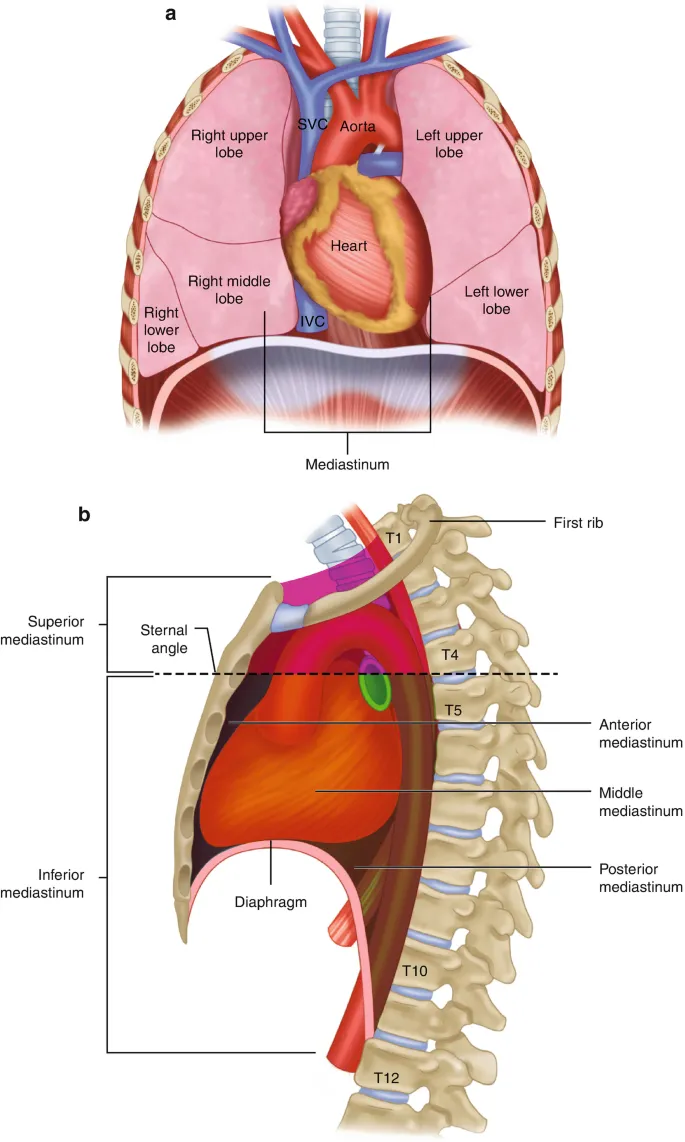
Mediastinal masses evaluation and management Explanation: ***Pericardial sac***
- The **pericardial sac** (and the diaphragm, inferiorly) forms the anterior boundary of the **posterior mediastinum** [1].
- This anatomical relationship is crucial for surgeons during thoracotomy to distinguish between the middle and posterior mediastinal compartments [1].
*Descending thoracic aorta*
- The **descending thoracic aorta** is a large vessel located *within* the posterior mediastinum itself, typically running along its left side [2].
- Therefore, it is a content of the posterior mediastinum, not a boundary.
*Azygos vein*
- The **azygos vein** is also a major structure *within* the posterior mediastinum, running along the right side of the vertebral column.
- It is a content, not a boundary, of this compartment.
*Thoracic vertebrae*
- The **thoracic vertebrae** form the *posterior* boundary of the posterior mediastinum [1].
- This anatomical landmark gives the posterior mediastinum its name and defines its dorsal limit.
Mediastinal masses evaluation and management US Medical PG Question 2: A 35-year-old woman comes to the physician because of blurred vision for the past 2 months. During this period, she has also had difficulty chewing and swallowing. She reports that her symptoms worsen throughout the day and improve with rest. There is no personal or family history of serious illness. The patient works as a teacher and has had a great deal of stress lately. She does not smoke and drinks a glass of wine occasionally. She takes no medications. Her temperature is 37°C (98.6°F), pulse is 68/min, and blood pressure is 130/80 mm Hg. Physical examination shows bilateral ptosis and mask-like facies. Muscle strength is decreased in both lower extremities. The anti–acetylcholine receptor (AChR) antibody test is positive. Electromyography shows a decremental response following repetitive nerve stimulation. Which of the following is the most appropriate next step in the management of this patient?
- A. Serum ACTH and CRH levels
- B. Plasmapheresis
- C. Anti-VGCC antibody level
- D. Physostigmine therapy
- E. CT scan of the chest (Correct Answer)
Mediastinal masses evaluation and management Explanation: ***CT scan of the chest***
- The patient has symptoms suggestive of **myasthenia gravis**, including **ptosis**, **diplopia** (blurred vision), **dysphagia**, and **fatigue that worsens with activity and improves with rest**. The positive **anti-acetylcholine receptor (AChR) antibody** test and **decremental response on EMG** confirm the diagnosis. A computed tomography (CT) scan of the chest is crucial to evaluate for a **thymoma**, which is present in 10-15% of patients with myasthenia gravis and can be surgically resected, potentially leading to symptom improvement or remission.
- Approximately 85% of myasthenia gravis patients have detectable **AChR antibodies**, making this test highly specific for the condition. The presence of these antibodies, along with the characteristic clinical picture and electromyography findings, establishes the diagnosis of myasthenia gravis. Thymectomy is often considered in patients with generalized myasthenia gravis, even in the absence of a thymoma, due to potential therapeutic benefits.
*Serum ACTH and CRH levels*
- This test is primarily used to investigate conditions related to the **hypothalamic-pituitary-adrenal axis**, such as **Cushing's disease** or **Addison's disease**.
- There are no symptoms presented that would suggest altered ACTH or CRH levels, making this an inappropriate diagnostic step for the current patient's presentation.
*Plasmapheresis*
- **Plasmapheresis** is a treatment for **acute severe myasthenia gravis** or **myasthenic crisis**, involving the removal of plasma to eliminate circulating antibodies.
- While it is a treatment for myasthenia gravis, it is not the *next step* in initial workup after diagnosis for a stable patient as described; the priority is to investigate underlying causes like thymoma.
*Anti-VGCC antibody level*
- **Anti-voltage-gated calcium channel (VGCC) antibodies** are characteristic of **Lambert-Eaton Myasthenic Syndrome (LEMS)**, often associated with **small cell lung cancer**.
- The patient's symptoms (e.g., ptosis, worsening with activity) and the positive **AChR antibodies** are classic for myasthenia gravis, not LEMS, making this test unnecessary.
*Physostigmine therapy*
- **Physostigmine** is an **acetylcholinesterase inhibitor** that reverses anticholinergic effects and can be used in some contexts, but it's not a primary treatment for myasthenia gravis.
- The standard pharmacotherapy for myasthenia gravis includes other anticholinesterase inhibitors like **pyridostigmine**, or immunomodulatory agents. This is a treatment, not a diagnostic step in the workup.
Mediastinal masses evaluation and management US Medical PG Question 3: A 35-year-old man presents to his primary care provider complaining of dull pain in his scrotum and lower back pain over the last 3 months. He is a computer engineer working in a private IT company. He had an uncomplicated appendectomy at the age of 22 years, but is otherwise without a significant past medical history. He smokes 2–3 cigarettes on weekends and drinks alcohol occasionally. He is sexually active with his wife. Today his heart rate is 90/min and blood pressure is 132/76 mm Hg. Scrotal examination reveals a firm, small and painless nodule on the left testicle. Scrotal ultrasound reveals a 0.9 x 0.5 cm irregular, non-cystic mass. He undergoes a left radical orchiectomy and histopathological examination reveals uniform tumor cells with abundant clear cytoplasm and distinct cell borders, consistent with a seminoma. Subsequent PET/CT scans show supraclavicular and para-aortic lymph node involvement. Which is the next and most appropriate step in the management of this patient?
- A. Immunotherapy
- B. Radiotherapy
- C. Chemotherapy (Correct Answer)
- D. Observation
- E. Surgery
Mediastinal masses evaluation and management Explanation: ***Chemotherapy***
- The patient has **metastatic seminoma** (supraclavicular and para-aortic lymph node involvement) following orchiectomy, which requires **systemic treatment**.
- **Chemotherapy** is the primary treatment for metastatic seminoma due to its high cure rates, especially with regimens like BEP (bleomycin, etoposide, cisplatin).
*Immunotherapy*
- **Immunotherapy** is generally not a first-line treatment for seminoma and is primarily used in refractory or metastatic cases of other solid tumors, not typically germ cell tumors.
- While research is ongoing, current guidelines do not recommend immunotherapy as the initial treatment for this stage of seminoma.
*Radiotherapy*
- **Radiotherapy** can be effective for localized seminoma involving lymph nodes, but it is typically reserved for local control and not for widespread metastatic disease involving both supraclavicular and para-aortic nodes.
- Systemic disease with involvement of distant lymph nodes (like supraclavicular) necessitates a systemic approach like chemotherapy rather than localized radiation.
*Observation*
- **Observation** is only appropriate for Stage I seminoma following orchiectomy, where there is no evidence of metastatic spread.
- In this case, the patient has clear evidence of **metastasis** to supraclavicular and para-aortic lymph nodes, making observation an inappropriate and dangerous choice.
*Surgery*
- **Surgery** (radical orchiectomy) has already been performed to remove the primary tumor.
- While surgical resection of residual masses after chemotherapy may be considered in some cases, it is not the primary next step for initial management of widespread lymph node metastases.
Mediastinal masses evaluation and management US Medical PG Question 4: A 65-year-old man with a 40-pack-year smoking history presents with hemoptysis and a persistent cough. Chest CT shows a 3.5 cm centrally located mass in the right main bronchus. Positron emission tomography confirms a malignant nodule. Bronchoscopy with transbronchial biopsy is performed and a specimen sample of the nodule is sent for frozen section analysis. The tissue sample is most likely to show which of the following tumor types?
- A. Carcinoid tumor
- B. Metastasis of colorectal cancer
- C. Small cell lung carcinoma
- D. Large cell carcinoma
- E. Squamous cell carcinoma (Correct Answer)
Mediastinal masses evaluation and management Explanation: ***Squamous cell carcinoma***
- This is the most likely diagnosis given the **central location** in the main bronchus, **heavy smoking history**, and presentation with **hemoptysis**.
- **Squamous cell carcinoma** accounts for 25-30% of lung cancers and characteristically arises in **central/proximal airways**, making it readily accessible by **bronchoscopy**.
- Histologically, it shows **keratin pearls** and **intercellular bridges** on biopsy.
- The **central endobronchial location** and ability to obtain tissue via transbronchial biopsy strongly favor squamous cell over peripheral tumors.
*Carcinoid tumor*
- **Carcinoid tumors** are **neuroendocrine tumors** that can present as central endobronchial masses and cause hemoptysis.
- However, they are typically **slow-growing** with more indolent presentation, and PET scans show **variable uptake** (often less intense than aggressive carcinomas).
- They represent only **1-2% of lung tumors** and occur more commonly in **younger, non-smoking patients**.
*Metastasis of colorectal cancer*
- While lung is a common site for **colorectal metastases**, these typically present as **multiple peripheral nodules** rather than a solitary central endobronchial mass.
- The clinical presentation strongly suggests **primary lung cancer** rather than metastatic disease.
- Without history of colorectal cancer, this is unlikely.
*Small cell lung carcinoma*
- **Small cell lung carcinoma** (SCLC) represents 15% of lung cancers and typically presents as a **large central mass** with early mediastinal involvement.
- However, SCLC is usually **too extensive at presentation** for transbronchial biopsy alone and often requires mediastinoscopy or CT-guided biopsy.
- Histology shows **small cells with scant cytoplasm**, **salt-and-pepper chromatin**, and **oat-cell morphology**.
- While possible, the single accessible endobronchial mass is more characteristic of squamous cell.
*Large cell carcinoma*
- **Large cell carcinoma** is a **diagnosis of exclusion** made when tumors lack features of adenocarcinoma, squamous cell, or small cell differentiation.
- It typically presents as **large peripheral masses** rather than central endobronchial lesions.
- It represents only **10% of lung cancers** and is less common than squamous cell carcinoma in this clinical scenario.
Mediastinal masses evaluation and management US Medical PG Question 5: A 54-year-old man comes to the emergency department because of a 3-week history of intermittent swelling of his left arm and feeling of fullness in his head that is exacerbated by lying down and bending over to tie his shoes. Physical examination shows left-sided facial edema and distention of superficial veins in the neck and left chest wall. Which of the following is the most likely cause of this patient's symptoms?
- A. Cervical rib
- B. Mediastinal lymphoma
- C. Subclavian steal syndrome
- D. Apical lung tumor (Correct Answer)
- E. Right heart failure
Mediastinal masses evaluation and management Explanation: ***Apical lung tumor***
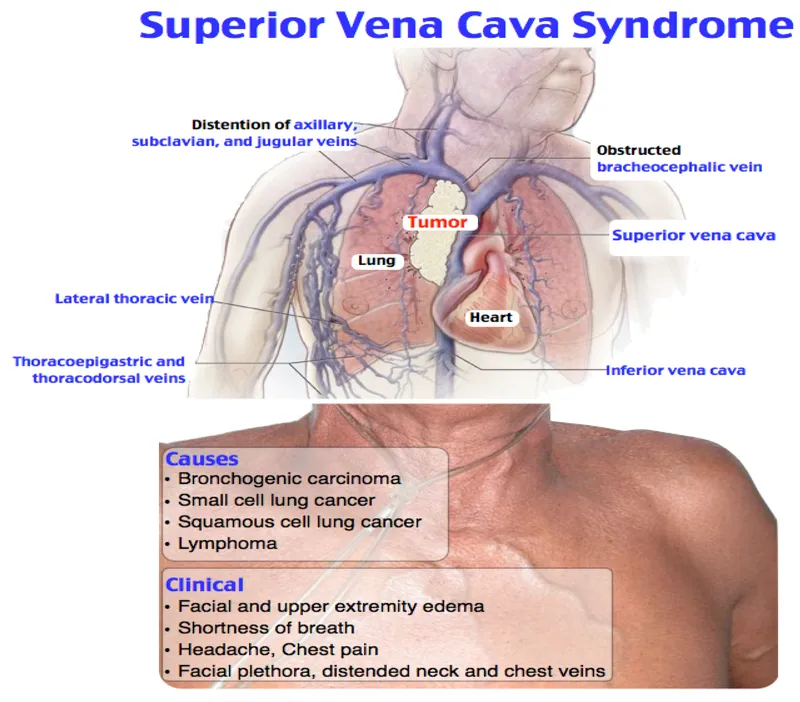
- The symptoms of **facial edema**, **neck vein distention**, and **swelling of the left arm**, particularly when exacerbated by positional changes such as lying down or bending over, are classic signs of **superior vena cava (SVC) syndrome**.
- An **apical lung tumor (Pancoast tumor)** is a common cause of SVC syndrome due to its proximity to the SVC and surrounding structures, leading to compression.
- The **left-sided predominance** (left arm swelling, left facial edema, left chest wall venous distention) specifically points to a left apical mass compressing the left brachiocephalic vein and/or SVC.
*Cervical rib*
- A cervical rib can cause **thoracic outlet syndrome**, leading to neurovascular compression, but it typically presents with neurological symptoms (pain, numbness, weakness in the arm/hand) or arterial insufficiency rather than widespread facial and neck edema.
- While it can cause *venous compression*, resulting in arm swelling, the **facial edema and neck vein distention** suggest a more central venous obstruction like SVC syndrome rather than peripheral thoracic outlet compression.
*Mediastinal lymphoma*
- Malignancies in the mediastinum, such as lymphoma, can indeed cause SVC syndrome by compressing the SVC.
- However, mediastinal lymphomas typically cause **bilateral** symptoms due to their central location, whereas this patient has **predominant left-sided findings** (left arm swelling, left facial edema, left chest wall veins), which more specifically suggests a left apical lung mass.
- Additionally, lymphoma commonly presents with systemic "B symptoms" (fever, night sweats, weight loss) and generalized lymphadenopathy, which are not mentioned here.
*Subclavian steal syndrome*
- This syndrome results from **subclavian artery stenosis** proximal to the vertebral artery origin, causing **retrograde blood flow** in the vertebral artery to supply the arm.
- It presents with **arm claudication**, dizziness, and syncope, especially with arm exercise, rather than venous congestion and swelling of the face, neck, and arm.
- This is an **arterial** syndrome, not a **venous** syndrome.
*Right heart failure*
- **Right heart failure** causes systemic venous congestion, leading to symptoms like **peripheral edema** (especially in the lower extremities), **jugular venous distention**, and **hepatomegaly**.
- While it can cause jugular venous distension, it typically presents with **bilateral lower extremity edema** and *rarely* causes unilateral arm swelling or predominant facial edema, as seen here.
- The **positional exacerbation** and **unilateral left-sided findings** are not characteristic of right heart failure.
Mediastinal masses evaluation and management US Medical PG Question 6: A 55-year-old male smoker presents to your office with hemoptysis, central obesity, and a round face with a "moon-like" appearance. He is found to have a neoplasm near the hilum of his left lung. A biopsy of the tumor reveals small basophilic cells with finely granular nuclear chromatin (a "salt and pepper" pattern). Which of the following is the most appropriate treatment for this patient?
- A. Tamoxifen
- B. Cisplatin and radiotherapy (Correct Answer)
- C. Watchful waiting
- D. Surgical resection
- E. Prednisone
Mediastinal masses evaluation and management Explanation: ***Cisplatin and radiotherapy***
- The patient presents with symptoms highly suggestive of **small cell lung carcinoma (SCLC)** due to his smoking history, central hilar mass, and paraneoplastic syndrome (Cushing's syndrome from **ACTH production**, causing central obesity and moon facies).
- SCLC is characterized by its **aggressive nature** and poor prognosis, and it is **highly responsive to chemotherapy** (e.g., cisplatin/etoposide) and **radiotherapy**, which are the mainstays of treatment.
*Tamoxifen*
- **Tamoxifen** is an **estrogen receptor modulator** used primarily in the treatment of **hormone-sensitive breast cancer**.
- It has no role in the treatment of small cell lung carcinoma, which is not typically hormone-sensitive.
*Watchful waiting*
- **Watchful waiting** is an inappropriate approach for SCLC, as it is a **rapidly growing** and highly metastatic cancer.
- Delaying treatment would lead to rapid disease progression and significantly worsen the patient's already poor prognosis.
*Surgical resection*
- **Surgical resection** is generally **not indicated for SCLC** because it tends to be widely metastatic at presentation, even if not clinically evident.
- It is typically considered only for very early-stage SCLC, which is rare, and often followed by adjuvant chemotherapy.
*Prednisone*
- **Prednisone** is a corticosteroid that might be used to manage some symptoms of Cushing's syndrome, but it **does not treat the underlying SCLC**.
- While it may offer symptomatic relief for certain paraneoplastic effects, it is not a primary cancer treatment and would not impact tumor growth or progression.
Mediastinal masses evaluation and management US Medical PG Question 7: A 72-year-old woman is brought to the emergency department because of lethargy and weakness for the past 5 days. During this period, she has had a headache that worsens when she leans forward or lies down. Her arms and face have appeared swollen over the past 2 weeks. She has a history of hypertension and invasive ductal carcinoma of the left breast. She underwent radical amputation of the left breast followed by radiation therapy 4 years ago. She has smoked two packs of cigarettes daily for 40 years. Current medications include aspirin, hydrochlorothiazide, and tamoxifen. Her temperature is 37.2°C (99°F), pulse is 103/min, and blood pressure is 98/56 mm Hg. Examination shows jugular venous distention, a mastectomy scar over the left thorax, and engorged veins on the anterior chest wall. There is no axillary or cervical lymphadenopathy. There is 1+ pitting edema in both arms. Which of the following is the most likely cause of this patient's symptoms?
- A. Pulmonary embolism
- B. Pulmonary tuberculosis
- C. Lung cancer (Correct Answer)
- D. Nephrotic syndrome
- E. Constrictive pericarditis
Mediastinal masses evaluation and management Explanation: ***Lung cancer***
- The patient's history of **heavy smoking** and prior **breast cancer with radiation therapy** significantly increases her risk for developing **lung cancer**.
- Symptoms like **headache worsened by bending/lying down**, **facial/arm swelling**, **jugular venous distention**, and **engorged chest wall veins** are classic signs of **superior vena cava (SVC syndrome)**, commonly caused by lung cancer compressing the SVC.
*Pulmonary embolism*
- This typically presents with **acute onset dyspnea**, **pleuritic chest pain**, and **tachycardia**, often without the progressive facial and arm swelling or engorged chest veins seen here.
- While a possibility in a bedridden patient, the constellation of symptoms strongly points away from a primary pulmonary embolism.
*Pulmonary tuberculosis*
- Characterized by **chronic cough**, **fever**, **night sweats**, and **weight loss**, symptoms not predominantly featured in this patient's presentation.
- While it can cause lymphadenopathy and venous obstruction in rare cases, the patient's risk factors and specific symptoms are more indicative of malignancy.
*Nephrotic syndrome*
- Primarily causes widespread **edema** (anasarca) due to **severe proteinuria** and **hypoalbuminemia**, which would present as generalized swelling rather than localized facial and arm swelling with prominent venous engorgement.
- It would not typically explain the headache worsened by position or localized SVC syndrome signs.
*Constrictive pericarditis*
- Presents with signs of right-sided heart failure, including **jugular venous distention**, **ascites**, and peripheral edema, but without the specific facial/arm swelling or engorged superficial chest veins characteristic of SVC syndrome.
- It usually results from chronic inflammation of the pericardium and is less likely to cause positional headaches or localized upper body venous obstruction.
Mediastinal masses evaluation and management US Medical PG Question 8: A 72-year-old man presents to his physician’s office with complaints of a cough and painful breathing for the last 2 months. He says that he has also observed a 5 kg (11 lb) weight loss during the past month. He is relatively healthy but the sudden change in his health worries him. Another problem that he has been facing is the swelling of his face and arms at unusual times of the day. He says that the swelling is more prominent when he is supine. He has also lately been experiencing difficulty with his vision. He consumes alcohol occasionally and quit smoking last year following a 25-year history of smoking. On examination, the patient is noted to have distended veins in the chest and arms. His jugular veins are distended. Physical examination shows ptosis of the right eye and miosis of the right pupil. His lungs are clear to auscultation. He is sent for an X-ray for further evaluation of his condition. Which of the following is the most likely site for the detection of the nodule on CT scan?
- A. Right upper lobe (Correct Answer)
- B. Brain stem metastasis
- C. Left upper lobe
- D. Central hilar region
- E. Peripheral bronchial region
Mediastinal masses evaluation and management Explanation: ***Right upper lobe***
- The patient's symptoms, including **Ptosis**, **Miosis**, and **Anhidrosis** of the right side of the face, are indicative of **Horner's syndrome**.
- **Horner's syndrome** in a patient with a smoking history, cough, weight loss, and edema of the face and arms (suggesting **SVC syndrome**) points strongly to a **Pancoast tumor** (superior sulcus tumor).
- The tumor is located in the **right upper lobe** specifically because the **Horner's syndrome is right-sided** (right ptosis, right miosis). Pancoast tumors cause **ipsilateral** Horner's syndrome by invading the sympathetic chain on the same side as the tumor.
*Brain stem metastasis*
- While a brain stem lesion could cause vision difficulties and neurological deficits, it does not explain the **SVC syndrome** (facial/arm swelling, distended veins) or the pulmonary symptoms like cough and weight loss.
- **Pancoast tumors** can cause vision changes due to **Horner's syndrome**, not necessarily brain metastasis.
*Left upper lobe*
- Although a tumor in the left upper lobe could cause similar symptoms to a right upper lobe tumor, the examination findings of **ptosis** and **miosis** on the **right side** localize the lesion to the **right apex**.
- **Horner's syndrome** develops on the **ipsilateral side** of the sympathetic chain disruption.
*Central hilar region*
- A tumor in the central hilar region would typically cause symptoms related to bronchial obstruction or compression of central structures, such as a persistent cough, hemoptysis, or SVC syndrome if it's large enough.
- However, it is less likely to directly cause **Horner's syndrome** with ptosis and miosis localized to one eye, which is a hallmark of an apical (Pancoast) tumor affecting the sympathetic chain.
*Peripheral bronchial region*
- A peripheral bronchial nodule would usually present with a cough, possibly hemoptysis, or be asymptomatic until it grows large enough to cause obstructive symptoms or pleural involvement.
- It is unlikely to cause both **SVC syndrome** and **Horner's syndrome** simultaneously, which are characteristic of an apical lung tumor.
Mediastinal masses evaluation and management US Medical PG Question 9: A 39-year-old man presents with painless swelling of the right testis and a sensation of heaviness. The physical examination revealed an intra-testicular solid mass that could not be felt separately from the testis. After a thorough evaluation, he was diagnosed with testicular seminoma. Which of the following group of lymph nodes are most likely involved?
- A. Superficial inguinal lymph nodes (lateral group)
- B. Deep inguinal lymph nodes
- C. Superficial inguinal lymph nodes (medial group)
- D. Para-rectal lymph nodes
- E. Para-aortic lymph nodes (Correct Answer)
Mediastinal masses evaluation and management Explanation: ***Para-aortic lymph nodes***
- The **testes** develop in the abdomen and descend into the scrotum, retaining their original lymphatic drainage. Therefore, **testicular cancer** typically metastasizes to the **para-aortic** (or retroperitoneal) lymph nodes, which are located near the renal veins at the level of L1-L2.
- This is the primary lymphatic drainage pathway for the testes.
*Superficial inguinal lymph nodes (lateral group)*
- These lymph nodes primarily drain the skin of the **scrotum**, perineum, and lower limbs, but not the **testes** themselves.
- Involvement would suggest spread to the scrotal skin or compromised lymphatic flow due to prior scrotal surgery or infection, which is not indicated here.
*Deep inguinal lymph nodes*
- **Deep inguinal lymph nodes** drain structures deeper in the leg and gluteal region, as well as receiving efferent vessels from the superficial inguinal nodes.
- They are not the primary drainage site for the **testes**.
*Superficial inguinal lymph nodes (medial group)*
- Similar to the lateral group, the **medial superficial inguinal lymph nodes** primarily drain the external genitalia (excluding the testes), perineum, and lower abdominal wall.
- They are not the direct drainage route for **testicular cancer**.
*Para-rectal lymph nodes*
- **Para-rectal lymph nodes** are located near the rectum and are involved in the drainage of the rectum and lower sigmoid colon.
- They have no direct connection to the lymphatic drainage of the **testes**.
Mediastinal masses evaluation and management US Medical PG Question 10: An obese 52-year-old man is brought to the emergency department because of increasing shortness of breath for the past 8 hours. Two months ago, he noticed a mass on the right side of his neck and was diagnosed with laryngeal cancer. He has smoked two packs of cigarettes daily for 27 years. He drinks two pints of rum daily. He appears ill. He is oriented to person, place, and time. His temperature is 37°C (98.6°F), pulse is 111/min, respirations are 34/min, and blood pressure is 140/90 mm Hg. Pulse oximetry on room air shows an oxygen saturation of 89%. Examination shows a 9-cm, tender, firm subglottic mass on the right side of the neck. Cervical lymphadenopathy is present. His breathing is labored and he has audible inspiratory stridor but is able to answer questions. The lungs are clear to auscultation. Arterial blood gas analysis on room air shows:
pH 7.36
PCO2 45 mm Hg
PO2 74 mm Hg
HCO3- 25 mEq/L
He has no advanced directive. Which of the following is the most appropriate next step in management?
- A. Comfort care measures
- B. Cricothyroidotomy (Correct Answer)
- C. Tracheostomy
- D. Intramuscular epinephrine
- E. Tracheal stenting
Mediastinal masses evaluation and management Explanation: ***Correct: Cricothyroidotomy***
- This patient has **impending complete airway obstruction** evidenced by inspiratory stridor, severe tachypnea (34/min), hypoxia (O2 sat 89%), and a large obstructing laryngeal mass
- **Cricothyroidotomy** is the emergent surgical airway procedure of choice when there is **imminent or actual complete upper airway obstruction** and endotracheal intubation cannot be safely performed
- The subglottic mass makes endotracheal intubation **extremely dangerous** - instrumentation could precipitate complete obstruction and inability to ventilate
- Cricothyroidotomy provides **immediate airway access** (can be performed in 30-60 seconds) below the level of obstruction, making it life-saving in this emergency
- In the "cannot intubate, cannot ventilate" scenario, cricothyroidotomy is the definitive emergency intervention per ATLS and airway management guidelines
*Incorrect: Tracheostomy*
- While tracheostomy provides definitive airway management, it is a **controlled, elective procedure** typically performed in the OR that takes 20-30 minutes
- This patient requires **immediate airway access** - waiting for OR setup and performing tracheostomy risks complete airway collapse and death
- Tracheostomy may be performed later as a planned procedure once the airway is secured with cricothyroidotomy
- The presence of stridor indicates **critical airway narrowing** requiring emergency intervention, not elective surgery
*Incorrect: Comfort care measures*
- The patient is **alert and oriented** without an advanced directive indicating wishes for comfort care only
- This is an **acute, reversible condition** with appropriate emergency airway intervention
- Presumed consent applies in life-threatening emergencies when the patient cannot formally consent but intervention would be life-saving
- Comfort care would be inappropriate without documented patient wishes or irreversible terminal condition
*Incorrect: Intramuscular epinephrine*
- Epinephrine is indicated for **anaphylaxis** or angioedema causing airway edema from allergic/inflammatory mechanisms
- This patient has **mechanical obstruction** from a solid tumor mass, which will not respond to epinephrine
- Epinephrine causes vasoconstriction and reduces mucosal edema but cannot reduce tumor mass
- Would delay definitive airway management and not address the underlying problem
*Incorrect: Tracheal stenting*
- Tracheal stenting requires **bronchoscopy** in a controlled setting and is used for palliation of tracheal narrowing
- Cannot be performed emergently in an unstable patient with impending airway obstruction
- The obstruction is at the **laryngeal/subglottic level**, not typically amenable to emergency stenting
- Requires time for procedure setup and sedation, which this patient cannot afford given the critical airway emergency
More Mediastinal masses evaluation and management US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.