Congenital heart surgery principles US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Congenital heart surgery principles. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Congenital heart surgery principles US Medical PG Question 1: A 15-month-old boy is brought to the pediatrician for immunizations and assessment. His parents report that he is eating well and produces several wet diapers every day. He is occasionally fussy, but overall a happy and curious child. The boy was born at 39 weeks gestation via spontaneous vaginal delivery. On physical examination his vital signs are stable. His weight and height are above the 85th percentile for his age and sex. On chest auscultation, the pediatrician detects a loud harsh holosystolic murmur over the left lower sternal border. The first and second heart sounds are normal. An echocardiogram confirms the diagnosis of the muscular ventricular septal defect without pulmonary hypertension. Which of the following is the best management strategy for this patient?
- A. Surgical closure of the defect using cardiopulmonary bypass
- B. Reassurance of the parents and regular follow-up (Correct Answer)
- C. Oral digoxin and regular follow-up
- D. Antibiotic prophylaxis against infective endocarditis
- E. Transcatheter occlusion closure of the defect
Congenital heart surgery principles Explanation: **Reassurance of the parents and regular follow-up**
- Most **small muscular VSDs (Ventricular Septal Defects)**, especially in asymptomatic children with normal growth and no signs of heart failure or pulmonary hypertension, **close spontaneously**.
- Given the patient's normal development, stable vital signs, good feeding, and lack of pulmonary hypertension, a conservative approach with **monitoring for spontaneous closure** is appropriate.
*Surgical closure of the defect using cardiopulmonary bypass*
- **Surgical VSD closure** is typically reserved for large defects causing **symptoms, growth failure, pulmonary hypertension**, or those that fail to close spontaneously.
- The patient in the scenario is asymptomatic and thriving, which does not warrant an invasive procedure at this time.
*Oral digoxin and regular follow-up*
- **Digoxin** is a medication used to improve **cardiac contractility** and manage symptoms of **heart failure**, which this patient does not exhibit.
- It would only be considered if there were signs of **congestive heart failure** due to a large VSD, which is not the case here.
*Antibiotic prophylaxis against infective endocarditis*
- Current guidelines from the American Heart Association (AHA) generally **do not recommend routine antibiotic prophylaxis** for VSDs unless there's a history of infective endocarditis or uncorrected cyanotic heart disease.
- The risk of **infective endocarditis** is very low in isolated VSDs and the potential side effects of prophylactic antibiotics outweigh the benefits.
*Transcatheter occlusion closure of the defect*
- **Transcatheter closure** is an option for certain types of VSDs, often **muscular VSDs**, but typically for those that are **larger, symptomatic**, and have not closed spontaneously.
- Similar to surgical closure, this invasive procedure is not indicated for an **asymptomatic, thriving child** with a muscular VSD that is likely to close on its own.
Congenital heart surgery principles US Medical PG Question 2: A newborn is rushed to the neonatal ICU after becoming cyanotic shortly after birth. An ultrasound is performed which shows the aorta coming off the right ventricle and lying anterior to the pulmonary artery. The newborn is given prostaglandin E1 and surgery is planned to correct the anatomic defect. Which of the following developmental processes failed to occur in the newborn?
- A. Failure of the membranous ventricular septum to fuse with the muscular interventricular septum
- B. Failure of the septum primum to fuse with the septum secundum
- C. Failure of the aorticopulmonary septum to spiral (Correct Answer)
- D. Failure of the ductus venosus to close
- E. Failure of the ductus arteriosus to close
Congenital heart surgery principles Explanation: ***Failure of the aorticopulmonary septum to spiral***
- **Transposition of the great arteries (TGA)**, characterized by the aorta originating from the right ventricle and the pulmonary artery from the left ventricle, results from the **aorticopulmonary septum** failing to spiral properly during embryological development.
- This defect leads to two separate circulatory systems, causing severe **cyanosis** shortly after birth and requiring **prostaglandin E1** to maintain a patent ductus arteriosus for mixing of oxygenated and deoxygenated blood.
- This is a ductal-dependent lesion requiring urgent intervention.
*Failure of the membranous ventricular septum to fuse with the muscular interventricular septum*
- This specific failure leads to a **ventricular septal defect (VSD)**, which allows blood to shunt between ventricles.
- While VSDs can cause cyanosis if large and associated with pulmonary hypertension (Eisenmenger syndrome), the description of **great artery transposition** is not caused by this developmental failure.
*Failure of the septum primum to fuse with the septum secundum*
- This developmental anomaly results in a **patent foramen ovale (PFO)** or an **atrial septal defect (ASD)**.
- These defects typically cause a left-to-right shunt and present with symptoms later in life, not with severe immediate cyanosis.
- In TGA, an ASD may actually be beneficial as it allows some mixing of blood.
*Failure of the ductus venosus to close*
- The **ductus venosus** shunts oxygenated blood from the umbilical vein directly to the inferior vena cava, bypassing the fetal liver during intrauterine life.
- Persistent patency of the ductus venosus after birth is rare and does not cause the severe cyanosis and specific great artery anatomy seen in TGA.
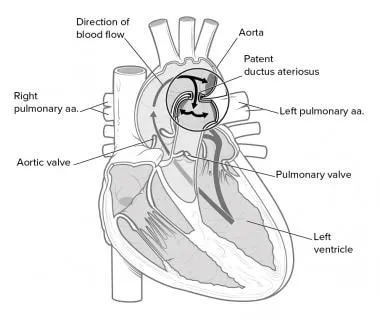
*Failure of the ductus arteriosus to close*
- A **patent ductus arteriosus (PDA)** allows blood to flow from the aorta to the pulmonary artery after birth, which can lead to pulmonary overcirculation.
- In **transposition of the great arteries**, a PDA is actually crucial for survival as it provides a pathway for mixing of oxygenated and deoxygenated blood; maintaining PDA patency with PGE1 is the initial management, not a cause of the condition.
Congenital heart surgery principles US Medical PG Question 3: A 2-week-old male newborn is brought to the physician because his mother has noticed her son has occasional bouts of ""turning blue in the face"" while crying. He also tires easily and sweats while feeding. He weighed 2150 g (4 lb 11 oz) at birth and has gained 200 g (7 oz). The baby appears mildly cyanotic. Examination shows a 3/6 systolic ejection murmur heard over the left upper sternal border. A single S2 is present. An echocardiography confirms the diagnosis. Which of the following factors is the main determinant of the severity of this patient's cyanosis?
- A. Left ventricular outflow obstruction
- B. Right ventricular outflow obstruction (Correct Answer)
- C. Atrial septal defect
- D. Right ventricular hypertrophy
- E. Ventricular septal defect
Congenital heart surgery principles Explanation: **Right ventricular outflow obstruction**
- This clinical scenario describes a **cyanotic heart defect**, most likely **Tetralogy of Fallot**, given the cyanosis, exertion intolerance, and murmur at the left upper sternal border with a single S2.
- The severity of **right ventricular outflow tract obstruction (RVOTO)** directly dictates the amount of right-to-left shunting across a ventricular septal defect, which in turn determines the degree of **cyanosis**.
- More severe RVOTO → greater resistance to pulmonary blood flow → more deoxygenated blood shunted right-to-left through the VSD → worse cyanosis.
*Left ventricular outflow obstruction*
- **Left ventricular outflow obstruction** typically causes symptoms related to **heart failure** or **syncope** due to reduced systemic blood flow, rather than cyanosis.
- Examples include **aortic stenosis** or **coarctation of the aorta**, which do not present with significant cyanosis as a primary symptom.
*Atrial septal defect*
- An **atrial septal defect (ASD)** usually presents as a **left-to-right shunt**, leading to **acyanotic heart disease** and often symptoms of pulmonary overload.
- Cyanosis in an ASD only occurs if there is **pulmonary hypertension** leading to shunt reversal (Eisenmenger syndrome), which is unlikely in a 2-week-old.
*Right ventricular hypertrophy*
- **Right ventricular hypertrophy** is a consequence of increased workload on the right ventricle, often due to **pulmonary hypertension** or **right ventricular outflow obstruction**.
- While present in conditions causing cyanosis (like Tetralogy of Fallot), it is the *result* of the outflow obstruction, not the primary determinant of cyanosis severity itself.
*Ventricular septal defect*
- A **ventricular septal defect (VSD)** alone typically causes a **left-to-right shunt**, leading to **acyanotic heart disease** and symptoms of pulmonary overcirculation.
- In Tetralogy of Fallot, a VSD is present, but it's the **pulmonary stenosis (RVOTO)** that forces deoxygenated blood through the VSD into the systemic circulation, causing cyanosis.
Congenital heart surgery principles US Medical PG Question 4: Over the course of a year, 5 children with identical congenital heart defects were referred to a pediatric cardiac surgeon for evaluation. All 5 children had stable vital signs and were on appropriate medication. Upon review of medical records, all of them had a loud holosystolic murmur over the third intercostal space at the left sternal border. The surgeon ordered echocardiograms for all 5 children and recommended surgical closure of the defect in one of them. Which of the following patients required surgical repair of their defect?
- A. A 7-year-old boy with an 11-mm muscular defect and severe pulmonary vascular disease non-responsive to pulmonary vasodilators
- B. An 11-month-old female infant with a 6-mm membranous defect, without heart failure, pulmonary hypertension, or growth failure
- C. A 4-month-old male infant with a 12-mm muscular defect, without heart failure, pulmonary hypertension or growth failure
- D. A 5-year-old girl with a 2-mm membranous defect, no heart failure, a Qp:Qs ratio less than 2:1, and no growth failure
- E. A 2-year-old boy with a 2-mm supracristal defect, without heart failure, pulmonary hypertension, or growth failure (Correct Answer)
Congenital heart surgery principles Explanation: ***A 2-year-old boy with a 2-mm supracristal defect, without heart failure, pulmonary hypertension, or growth failure***
- This patient description most closely matches the criteria for requiring surgical repair. **Supracristal VSDs** are more prone to **aortic valve prolapse** and **aortic regurgitation**, even with small defects and absent or mild symptoms, thus warranting early surgical consideration.
- While other symptomatic VSDs might require surgery, this specific type of VSD carries a unique risk to the aortic valve, making surgical intervention often necessary to prevent future complications.
*A 7-year-old boy with an 11-mm muscular defect and severe pulmonary vascular disease non-responsive to pulmonary vasodilators*
- This patient likely has **Eisenmenger syndrome**, characterized by **irreversible pulmonary vascular disease** and right-to-left shunting.
- Surgical repair of the VSD is **contraindicated** in such cases and would likely worsen the patient's condition.
*An 11-month-old female infant with a 6-mm membranous defect, without heart failure, pulmonary hypertension, or growth failure*
- Small to moderate membranous VSDs in asymptomatic infants often **close spontaneously**, especially in the first year of life.
- Without signs of **heart failure**, **pulmonary hypertension**, or **growth failure**, a watch-and-wait approach is typically preferred over immediate surgery.
*A 4-month-old male infant with a 12-mm muscular defect, without heart failure, pulmonary hypertension or growth failure*
- Although this is a **large muscular VSD**, the infant is currently **asymptomatic** without heart failure, pulmonary hypertension, or growth failure.
- In the **absence of symptoms or hemodynamic compromise**, initial management includes close observation with medical therapy as needed. Surgery would be indicated if symptoms develop or significant shunting occurs.
- Note: While small muscular VSDs (<5mm) often close spontaneously, large defects like this require vigilant monitoring as they may eventually require intervention.
*A 5-year-old girl with a 2-mm membranous defect, no heart failure, a Qp:Qs ratio less than 2:1, and no growth failure*
- A 2-mm membranous defect is considered a **small VSD**, and a Qp:Qs ratio less than 2:1 indicates an **insignificant shunt**.
- Small VSDs, particularly in older children who are asymptomatic, very often close spontaneously or remain hemodynamically insignificant, and typically do not require surgical intervention.
Congenital heart surgery principles US Medical PG Question 5: A 4-year-old Caucasian male suffers from cyanosis and dyspnea relieved by squatting. Which of the following abnormalities is most likely present?
- A. Atrial septal defect
- B. Coarctation of the aorta
- C. Bicuspid aortic valve
- D. Ventricular septal defect
- E. Tetralogy of Fallot (Correct Answer)
Congenital heart surgery principles Explanation: ***Tetralogy of Fallot***
- **Cyanosis** and **dyspnea relieved by squatting** are the hallmark clinical features of **Tetralogy of Fallot**, making this the correct diagnosis.
- The condition consists of four anatomic abnormalities: **ventricular septal defect (VSD)**, **right ventricular outflow tract obstruction**, **right ventricular hypertrophy**, and **overriding aorta**.
- The right-to-left shunt across the VSD causes **deoxygenated blood** to enter systemic circulation, producing **cyanosis**.
- **Squatting increases systemic vascular resistance (SVR)**, which decreases the right-to-left shunt, improves pulmonary blood flow, and relieves cyanosis and dyspnea during **"tet spells"**.
*Atrial septal defect*
- ASDs typically cause **left-to-right shunts** and are **acyanotic lesions**.
- Patients may be asymptomatic or present with **exertional dyspnea** and **fatigue** in later childhood or adulthood.
- Cyanosis would only occur if **Eisenmenger syndrome** develops (reversal to right-to-left shunt due to pulmonary hypertension), which is rare at age 4 and does not improve with squatting.
*Coarctation of the aorta*
- This is an **acyanotic** lesion characterized by **narrowing of the descending aorta**.
- Classic findings include **upper extremity hypertension**, **diminished or delayed femoral pulses**, and **lower extremity hypotension**.
- Does not cause cyanosis or squatting relief.
*Bicuspid aortic valve*
- A common **acyanotic** congenital abnormality that may lead to **aortic stenosis** or **regurgitation** over time.
- Usually asymptomatic in childhood; may present with **murmur**, chest pain, or syncope in adulthood.
- Does not cause cyanosis or relief with squatting.
*Ventricular septal defect*
- Isolated VSDs typically cause **left-to-right shunts** and are **acyanotic**.
- May present with **heart failure symptoms** (tachypnea, poor feeding, failure to thrive) in infancy if the defect is large.
- Cyanosis occurs only if **Eisenmenger syndrome** develops (usually takes years to decades), and symptoms are not relieved by squatting.
Congenital heart surgery principles US Medical PG Question 6: A 66-year-old female with hypertension and a recent history of acute ST-elevation myocardial infarction (STEMI) 6 days previous, treated with percutaneous transluminal angioplasty (PTA), presents with sudden onset chest pain, shortness of breath, diaphoresis, and syncope. Vitals are temperature 37°C (98.6°F), blood pressure 80/50 mm Hg, pulse 125/min, respirations 12/min, and oxygen saturation 92% on room air. On physical examination, the patient is pale and unresponsive. Cardiac exam reveals tachycardia and a pronounced holosystolic murmur loudest at the apex and radiates to the back. Lungs are clear to auscultation. Chest X-ray shows cardiomegaly with clear lung fields. ECG is significant for ST elevations in the precordial leads (V2-V4) and low-voltage QRS complexes. Emergency transthoracic echocardiography shows a left ventricular wall motion abnormality along with a significant pericardial effusion. The patient is intubated, and aggressive fluid resuscitation is initiated. What is the next best step in management?
- A. Immediate cardiac catheterization
- B. Immediate transfer to the operating room (Correct Answer)
- C. Emergency pericardiocentesis
- D. Intra-aortic balloon counterpulsation
- E. Administer dobutamine 5-10 mcg/kg/min IV
Congenital heart surgery principles Explanation: ***Immediate transfer to the operating room***
- The patient's presentation with sudden onset chest pain, shortness of breath, profound cardiogenic shock, and a new **holosystolic murmur at the apex radiating to the back** in the context of a recent **STEMI**, strongly suggests **acute papillary muscle rupture** causing severe mitral regurgitation. This is a surgical emergency requiring immediate intervention.
- The holosystolic murmur at the apex is pathognomonic for acute mitral regurgitation, distinguishing this from ventricular free wall rupture (which would present with tamponade physiology without a murmur).
- The patient requires urgent surgical repair (mitral valve replacement or repair) to address this mechanical complication of **myocardial infarction (MI)**, which is causing severe hemodynamic compromise.
*Immediate cardiac catheterization*
- While cardiac catheterization is essential for diagnosing coronary artery disease and revascularization, in this emergent situation with profound shock and a mechanical complication (papillary muscle rupture), the primary issue is structural cardiac damage requiring surgical repair, not ongoing ischemia alone.
- Delaying surgical intervention for catheterization in this hemodynamically unstable patient would be detrimental and potentially fatal.
*Emergency pericardiocentesis*
- Although there is a **pericardial effusion** on echocardiography, the patient's presentation with a new holosystolic murmur and profound shock after STEMI indicates **papillary muscle rupture with acute mitral regurgitation**, not cardiac tamponade.
- The presence of a loud murmur excludes ventricular free wall rupture as the primary cause. The effusion is likely reactive or incidental.
- Pericardiocentesis would not address the underlying mitral valve pathology causing the hemodynamic collapse.
*Intra-aortic balloon counterpulsation*
- **Intra-aortic balloon pump (IABP)** can improve cardiac output and reduce afterload, which may provide temporary hemodynamic support in cardiogenic shock.
- However, in cases of **papillary muscle rupture** with severe acute mitral regurgitation, IABP provides only temporary support and does not fix the underlying structural problem.
- It could be considered as a bridge to surgery, but the definitive treatment is surgical repair, which should be expedited without delay.
*Administer dobutamine 5-10 mcg/kg/min IV*
- **Dobutamine** is an inotrope that increases cardiac contractility. While it might improve cardiac output in some forms of cardiogenic shock, in the setting of **acute severe mitral regurgitation from papillary muscle rupture**, it cannot resolve the structural valvular incompetence.
- Increasing contractility may paradoxically worsen the regurgitant fraction and further compromise forward cardiac output.
- Medical management alone cannot resolve this mechanical complication, necessitating urgent surgical intervention.
Congenital heart surgery principles US Medical PG Question 7: A 2-year-old boy is brought to a pediatrician because his parents have noticed that he seems to be getting tired very easily at home. Specifically, they have noticed that he is often panting for breath after walking around the house for a few minutes and that he needs to take naps fairly often throughout the day. He has otherwise been well, and his parents do not recall any recent infections. He was born at home, and his mom did not receive any prenatal care prior to birth. Physical exam reveals a high-pitched, harsh, holosystolic murmur that is best heard at the lower left sternal border. No cyanosis is observed. Which of the following oxygen tension profiles would most likely be seen in this patient? (LV = left ventricle, RV = right ventricle, and SC = systemic circulation).
- A. LV: normal, RV: normal, SC: normal
- B. LV: normal, RV: increased, SC: normal (Correct Answer)
- C. LV: decreased, RV: increased, SC: decreased
- D. LV: decreased, RV: normal, SC: decreased
- E. LV: normal, RV: normal, SC: decreased
Congenital heart surgery principles Explanation: ***LV: normal, RV: increased, SC: normal***
- The patient's presentation with easy fatigability, dyspnea on exertion, and a **holosystolic murmur** at the **lower left sternal border** strongly suggests a **ventricular septal defect (VSD)**. These symptoms result from a **left-to-right shunt**, leading to increased blood flow and pressure in the **right ventricle (RV)** and pulmonary circulation.
- In a VSD, highly oxygenated blood from the **left ventricle (LV)** shunts into the RV. This increases the **oxygen tension** in the RV, while the LV and systemic circulation (SC) typically maintain normal oxygen tension if the shunt is not so large that it causes **pulmonary hypertension** with **Eisenmenger syndrome**.
*LV: normal, RV: normal, SC: normal*
- This profile would indicate a **normal cardiovascular system** without any significant shunting or cardiac anomaly.
- It does not align with the patient's symptoms of easy fatigability, dyspnea, and the presence of a pathological murmur.
*LV: decreased, RV: increased, SC: decreased*
- A **decreased oxygen tension in the left ventricle** and **systemic circulation** typically indicates a **right-to-left shunt** or severe **pulmonary disease**, often associated with **cyanosis**, which is noted as absent in this patient.
- While RV oxygen tension *could* be increased in some complex congenital heart diseases with right-to-left shunting (e.g., mixing lesions), the overall profile does not fit the characteristic presentation of a VSD without cyanosis.
*LV: decreased, RV: normal, SC: decreased*
- This profile with **decreased oxygen tension in the left ventricle** and **systemic circulation** suggests a condition where oxygenated blood supply to the systemic circulation is compromised, such as severe **left ventricular dysfunction** or a **right-to-left shunt**.
- A **normal RV oxygen tension** without **cyanosis** makes this unlikely in the context of the patient's symptoms.
*LV: normal, RV: normal, SC: decreased*
- A **decreased oxygen tension in the systemic circulation** with **normal LV and RV oxygen tension** is inconsistent with a **VSD**.
- This profile might be observed in conditions like severe **anemia** or **hypoxia** without a primary cardiac shunt.
Congenital heart surgery principles US Medical PG Question 8: A newborn infant comes to the attention of the neonatal care unit because he started having heavy and rapid breathing. In addition, he was found to be very irritable with pale skin and profuse sweating. Finally, he was found to have cold feet with diminished lower extremity pulses. Cardiac auscultation reveals a harsh systolic murmur along the left sternal border. Notably, the patient is not observed to have cyanosis. Which of the following treatments would most likely be effective for this patient's condition?
- A. Prostaglandin I2
- B. Leukotriene E4
- C. Prostaglandin E2
- D. Prostaglandin E1 (Correct Answer)
- E. Thromboxane A2
Congenital heart surgery principles Explanation: ***Prostaglandin E1***
- The newborn's presentation with **respiratory distress, irritability, pale skin, profuse sweating, cold feet, diminished lower extremity pulses**, and a **harsh systolic murmur** without cyanosis is highly suggestive of **coarctation of the aorta**.
- **Prostaglandin E1 (PGE1)** is critical in maintaining the **patency of the ductus arteriosus**, which allows for blood flow to the lower body when there is severe obstruction like coarctation.
*Prostaglandin I2*
- **Prostaglandin I2 (PGI2)**, or **prostacyclin**, is a potent **vasodilator** and **platelet aggregation inhibitor**.
- While it has vascular effects, it is not the primary prostaglandin used to maintain ductal patency in newborns with critical congenital heart disease.
*Leukotriene E4*
- **Leukotrienes** are mediators of inflammation and allergic reactions, primarily involved in bronchoconstriction and vascular permeability.
- They do not play a significant role in the management of congenital heart defects requiring ductal patency.
*Prostaglandin E2*
- While **prostaglandin E2 (PGE2)** also contributes to maintaining ductal patency, **PGE1** is the preferred and more commonly used agent for this purpose in clinical practice.
- Both PGE1 and PGE2 are members of the E-series prostaglandins, but PGE1 is the standard pharmaceutical intervention.
*Thromboxane A2*
- **Thromboxane A2 (TXA2)** is a potent **vasoconstrictor** and promotes **platelet aggregation**.
- Its effects are opposite to what is desired in this patient, where maintained vessel patency (ductus arteriosus) is crucial.
Congenital heart surgery principles US Medical PG Question 9: A 63-year-old man is brought to the emergency department, 30 minutes after being involved in a high-speed motor vehicle collision. He is obtunded on arrival. He is intubated and mechanical ventilation is begun. The ventilator is set at a FiO2 of 60%, tidal volume of 440 mL, and positive end-expiratory pressure of 4 cm H2O. On the third day of intubation, his temperature is 37.3°C (99.1°F), pulse is 91/min, and blood pressure is 103/60 mm Hg. There are decreased breath sounds over the left lung base. Cardiac examination shows no abnormalities. The abdomen is soft and not distended. Arterial blood gas analysis shows:
pH 7.49
pCO2 29 mm Hg
pO2 73 mm Hg
HCO3- 20 mEq/L
O2 saturation 89%
Monitoring shows a sudden increase in the plateau airway pressure. An x-ray of the chest shows deepening of the costophrenic angle on the left side. Which of the following is the most appropriate next step in management?
- A. CT scan of the chest
- B. Administer levofloxacin
- C. Close observation
- D. Increase the PEEP
- E. Insertion of a chest tube (Correct Answer)
Congenital heart surgery principles Explanation: ***Insertion of a chest tube***
- The sudden increase in **plateau airway pressure**, decreased breath sounds over the left lung base, worsening hypoxemia (O2 sat 89%) despite high FiO2, and **deepening of the costophrenic angle on the left side** indicate a **traumatic hemothorax**.
- Deepening of the costophrenic angle on chest X-ray is a classic sign of **pleural fluid accumulation** (hemothorax or pleural effusion), not pneumothorax.
- In a trauma patient (high-speed motor vehicle collision) on day 3 of mechanical ventilation, this represents a **delayed hemothorax** requiring immediate drainage.
- **Chest tube insertion** is the definitive management to evacuate blood, re-expand the lung, and improve ventilation and oxygenation.
*CT scan of the chest*
- While CT scan would provide detailed anatomical information, the clinical presentation with sudden respiratory decompensation and clear chest X-ray findings of hemothorax requires **immediate intervention**.
- Delaying treatment to obtain CT imaging in an unstable ventilated patient could worsen hypoxemia and lead to cardiovascular compromise.
- CT scan may be obtained later if needed to evaluate for ongoing bleeding or other injuries.
*Administer levofloxacin*
- Antibiotics would be appropriate for **pneumonia or empyema**, but the patient has no clear signs of infection (afebrile at 37.3°C, acute presentation over hours not days).
- The primary problem is **mechanical compression** from pleural fluid accumulation, not infection.
- Antibiotics do not address the life-threatening respiratory compromise from hemothorax.
*Close observation*
- Close observation is inappropriate given the acute deterioration with increased plateau pressures and worsening hypoxemia.
- The patient requires urgent intervention to prevent further respiratory failure and potential cardiovascular collapse.
- Expectant management would be negligent in this clinical scenario.
*Increase the PEEP*
- Increasing **Positive End-Expiratory Pressure (PEEP)** would worsen the situation by increasing intrathoracic pressure against an already compressed lung.
- Higher PEEP could impair venous return, decrease cardiac output, and potentially convert a simple hemothorax to a tension physiology.
- PEEP adjustments do not address the underlying problem of pleural space fluid accumulation requiring drainage.
Congenital heart surgery principles US Medical PG Question 10: A 45-year-old male is brought into the emergency room by emergency medical services due to a stab wound in the chest. The wound is located superior and medial to the left nipple. Upon entry, the patient appears alert and is conversational, but soon becomes confused and loses consciousness. The patient's blood pressure is 80/40 mmHg, pulse 110/min, respirations 26/min, and temperature 97.0 deg F (36.1 deg C). On exam, the patient has distended neck veins with distant heart sounds. What is the next best step to increase this patient's survival?
- A. Heparin
- B. Intravenous fluids
- C. Aspirin
- D. Intravenous colloids
- E. Pericardiocentesis (Correct Answer)
Congenital heart surgery principles Explanation: ***Pericardiocentesis***
- The patient's presentation with **hypotension**, **tachycardia**, **distended neck veins**, and **distant heart sounds** after a chest stab wound is classic for **cardiac tamponade** (Beck's triad).
- **Pericardiocentesis** is the immediate life-saving procedure to drain the pericardial fluid and relieve pressure on the heart, improving cardiac output.
- In penetrating trauma, this serves as a **bridge to definitive surgical management** (thoracotomy or sternotomy).
*Heparin*
- **Heparin** is an anticoagulant and would worsen the situation by increasing bleeding into the pericardial space due to the stab wound.
- It is contraindicated in active bleeding and traumatic injury.
*Intravenous fluids*
- While **IV fluid resuscitation is recommended** in cardiac tamponade to maintain preload and support cardiac output, fluids alone **do not address the underlying mechanical obstruction**.
- The primary issue is **extrinsic compression of the heart** requiring drainage, not hypovolemia alone.
- Fluids are supportive but not definitive—**pericardiocentesis is the life-saving intervention**.
*Aspirin*
- **Aspirin** is an antiplatelet agent and would increase the risk of bleeding, exacerbating the patient's condition.
- It is used for conditions like myocardial infarction or stroke prevention, not for acute traumatic bleeding.
*Intravenous colloids*
- Similar to crystalloid fluids, **colloids** may provide temporary hemodynamic support but do not relieve the mechanical compression of the heart.
- They are supportive measures that **do not substitute for definitive pericardial drainage**.
More Congenital heart surgery principles US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.