Chest tube insertion and management US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Chest tube insertion and management. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Chest tube insertion and management US Medical PG Question 1: A 22-year-old soldier sustains a gunshot wound to the left side of the chest during a deployment in Syria. The soldier and her unit take cover from gunfire in a nearby farmhouse, and a combat medic conducts a primary survey of her injuries. She is breathing spontaneously. Two minutes after sustaining the injury, she develops severe respiratory distress. On examination, she is agitated and tachypneic. There is an entrance wound at the midclavicular line at the 2nd rib and an exit wound at the left axillary line at the 4th rib. There is crepitus on the left side of the chest wall. Which of the following is the most appropriate next step in management?
- A. Endotracheal intubation
- B. Intravenous administration of fentanyl
- C. Ultrasonography of the chest
- D. Administration of supplemental oxygen
- E. Needle thoracostomy (Correct Answer)
Chest tube insertion and management Explanation: ***Needle thoracostomy***
- The patient presents with classic signs of **tension pneumothorax** developing after a penetrating chest injury (gunshot wound), including severe respiratory distress, agitation, tachypnea, and subcutaneous emphysema (crepitus).
- The combination of penetrating chest trauma with entrance and exit wounds, rapid onset of severe respiratory distress, and crepitus strongly suggests air accumulation under pressure in the pleural space.
- **Needle thoracostomy** is the most urgent and life-saving intervention to decompress the pressurized pleural space, allowing lung re-expansion and improved hemodynamics.
- In a combat or field setting with clinical diagnosis of tension pneumothorax, immediate needle decompression takes precedence over imaging or other interventions.
*Endotracheal intubation*
- While the patient is in severe respiratory distress, intubation is not the immediate solution for the underlying mechanical problem of a **tension pneumothorax**.
- Intubation with positive pressure ventilation without prior decompression can worsen a **tension pneumothorax** by increasing positive pressure within the chest, further impairing venous return and cardiac output.
*Intravenous administration of fentanyl*
- Administering an opioid like fentanyl would address pain but does not resolve the acute, life-threatening **respiratory compromise** caused by **tension pneumothorax**.
- Pain relief is secondary to addressing the cause of respiratory failure in this acute setting.
*Ultrasonography of the chest*
- **Point-of-care ultrasound (POCUS)** can diagnose a pneumothorax, but it is not the most appropriate *next step* in a patient presenting with clear clinical signs of **tension pneumothorax** where time is critical.
- Clinical diagnosis and immediate intervention like **needle thoracostomy** take precedence over diagnostic imaging when the diagnosis is highly probable and the patient is unstable.
*Administration of supplemental oxygen*
- Supplemental oxygen is a supportive measure for hypoxemia, which would be present, but it does not address the underlying mechanical cause of **tension pneumothorax** where air is trapped under pressure, preventing lung expansion.
- While oxygen should be administered, it is not the definitive "next step" to relieve the severe respiratory distress.
Chest tube insertion and management US Medical PG Question 2: An 18-year-old man is brought to the emergency department 30 minutes after being stabbed in the chest during a fight. He has no other injuries. His pulse is 120/min, blood pressure is 90/60 mm Hg, and respirations are 22/min. Examination shows a 4-cm deep, straight stab wound in the 4th intercostal space 2 cm medial to the right midclavicular line. The knife most likely passed through which of the following structures?
- A. Serratus anterior muscle, pleura, inferior vena cava
- B. External oblique muscle, superior epigastric artery, azygos vein
- C. Pectoralis minor muscle, dome of the diaphragm, right lobe of the liver
- D. Intercostal muscles, internal thoracic artery, right heart
- E. Pectoral fascia, transversus thoracis muscle, right lung (Correct Answer)
Chest tube insertion and management Explanation: ***Pectoral fascia, transversus thoracis muscle, right lung***
* The stab wound is in the **4th intercostal space**, 2 cm medial to the right midclavicular line, placing it over the anterior chest wall. This trajectory would first penetrate the **pectoral fascia**.
* Deeper structures in this region include the **transversus thoracis muscle** and, given the depth, the **right lung** as it extends superiorly behind the anterior chest wall.
* *Serratus anterior muscle, pleura, inferior vena cava*
* The **serratus anterior muscle** is more laterally positioned, typically covering the side of the rib cage.
* The **inferior vena cava** is located more medially and posteriorly within the mediastinum, deep to the diaphragm, making it an unlikely target for an anterior 4th intercostal stab.
* *External oblique muscle, superior epigastric artery, azygos vein*
* The **external oblique muscle** is part of the abdominal wall and would not be penetrated in the 4th intercostal space.
* The **superior epigastric artery** is lower, typically extending into the abdominal wall, and the **azygos vein** is in the posterior mediastinum, not in the path of this superficial anterior stab wound.
* *Pectoralis minor muscle, dome of the diaphragm, right lobe of the liver*
* The **pectoralis minor muscle** is located deep to the pectoralis major, which would be penetrated. However, a stab at the 4th intercostal space would be too high to directly involve the **dome of the diaphragm** or the **right lobe of the liver**, which are typically below the 5th intercostal space, especially in forced expiration.
* *Intercostal muscles, internal thoracic artery, right heart*
* The **intercostal muscles** would certainly be traversed.
* However, the **internal thoracic artery** runs paramedially (about 1-2 cm from the sternum), and getting to the **right heart** would require a more medial and deeper trajectory, potentially causing immediate tamponade or severe hemorrhage.
Chest tube insertion and management US Medical PG Question 3: A 57-year-old man presents to the clinic for a chronic cough over the past 4 months. The patient reports a productive yellow/green cough that is worse at night. He denies any significant precipitating event prior to his symptoms. He denies fever, chest pain, palpitations, weight changes, or abdominal pain, but endorses some difficulty breathing that waxes and wanes. He denies alcohol usage but endorses a 35 pack-year smoking history. A physical examination demonstrates mild wheezes, bibasilar crackles, and mild clubbing of his fingertips. A pulmonary function test is subsequently ordered, and partial results are shown below:
Tidal volume: 500 mL
Residual volume: 1700 mL
Expiratory reserve volume: 1500 mL
Inspiratory reserve volume: 3000 mL
What is the functional residual capacity of this patient?
- A. 4500 mL
- B. 2000 mL
- C. 2200 mL
- D. 3200 mL (Correct Answer)
- E. 3500 mL
Chest tube insertion and management Explanation: ***3200 mL***
- The **functional residual capacity (FRC)** is the volume of air remaining in the lungs after a normal expiration.
- It is calculated as the sum of the **expiratory reserve volume (ERV)** and the **residual volume (RV)**. In this case, 1500 mL (ERV) + 1700 mL (RV) = 3200 mL.
*4500 mL*
- This value represents the sum of the **inspiratory reserve volume (3000 mL)** and the **residual volume (1700 mL)**, which does not correspond to a standard lung volume or capacity.
- It does not logically relate to the definition of functional residual capacity.
*2000 mL*
- This value represents the sum of the **tidal volume (500 mL)** and the **expiratory reserve volume (1500 mL)**, which is incorrect for FRC.
- This would represent the inspiratory capacity minus the inspiratory reserve volume, which is not a standard measurement used in pulmonary function testing.
*2200 mL*
- This value could be obtained by incorrectly adding the **tidal volume (500 mL)** and the **residual volume (1700 mL)**, which is not the correct formula for FRC.
- This calculation represents a miscombination of lung volumes that does not correspond to any standard pulmonary capacity measurement.
*3500 mL*
- This value is the sum of the **tidal volume (500 mL)**, the **expiratory reserve volume (1500 mL)**, and the **residual volume (1700 mL)**.
- This would represent the FRC plus the tidal volume, which is not a standard measurement and does not represent the functional residual capacity.
Chest tube insertion and management US Medical PG Question 4: A 27-year-old man presents to the emergency department with severe dyspnea and sharp chest pain that suddenly started an hour ago after he finished exercising. He has a history of asthma as a child, and he achieves good control of his acute attacks with Ventolin. On examination, his right lung field is hyperresonant along with diminished lung sounds. Chest wall motion during respiration is asymmetrical. His blood pressure is 105/67 mm Hg, respirations are 22/min, pulse is 78/min, and temperature is 36.7°C (98.0°F). The patient is supported with oxygen, given corticosteroids, and has had analgesic medications via a nebulizer. Considering the likely condition affecting this patient, what is the best step in management?
- A. CT scan
- B. ABG
- C. Chest X-rays (Correct Answer)
- D. Tube insertion
- E. Sonogram
Chest tube insertion and management Explanation: ***Chest X-rays***
- The patient's presentation with **sudden onset dyspnea** and **sharp chest pain** post-exercise, along with **hyperresonance** and **diminished lung sounds** in the right lung field, is highly suggestive of a **spontaneous pneumothorax**.
- However, the patient is **hemodynamically stable** (BP 105/67, HR 78/min) with no signs of tension physiology (no severe hypotension, marked tachycardia, or cardiovascular collapse).
- In a stable patient with suspected pneumothorax, **chest X-ray is the appropriate first step** to confirm the diagnosis, determine the size of the pneumothorax, and guide subsequent management (observation for small pneumothorax <20%, aspiration, or tube thoracostomy for larger pneumothoraces).
- Immediate intervention without imaging is reserved for unstable patients with tension pneumothorax.
*Tube insertion*
- Chest tube insertion is the definitive treatment for large pneumothoraces (>20%) or hemodynamically unstable patients with tension pneumothorax.
- In this **stable patient**, proceeding directly to tube insertion without imaging confirmation would be premature and not following standard of care.
- The diagnosis should be confirmed and the size estimated via chest X-ray before determining if tube thoracostomy is necessary.
*CT scan*
- CT scan is not indicated as the initial diagnostic test for suspected pneumothorax.
- It provides more detail than needed for this clinical scenario and causes unnecessary delay and radiation exposure when chest X-ray is sufficient.
- CT may be useful for detecting small pneumothoraces not visible on X-ray or evaluating underlying lung disease, but is not the first-line test.
*ABG*
- An Arterial Blood Gas (ABG) might show hypoxia and respiratory alkalosis, providing information about gas exchange.
- However, ABG does not confirm the diagnosis of pneumothorax or guide immediate management decisions.
- It is an adjunctive test that does not take priority over diagnostic imaging in this scenario.
*Sonogram*
- Lung ultrasound can rapidly detect pneumothorax by showing absent lung sliding and is increasingly used in emergency settings, particularly for bedside evaluation.
- While potentially useful, **chest X-ray remains the standard initial imaging modality** for suspected pneumothorax in most emergency departments, as it provides clear documentation of pneumothorax size and is more universally available and interpreted.
- Ultrasound may be preferred in specific situations (unstable patients, point-of-care evaluation), but chest X-ray is the conventional first-line imaging test.
Chest tube insertion and management US Medical PG Question 5: A 63-year-old man is brought to the emergency department, 30 minutes after being involved in a high-speed motor vehicle collision. He is obtunded on arrival. He is intubated and mechanical ventilation is begun. The ventilator is set at a FiO2 of 60%, tidal volume of 440 mL, and positive end-expiratory pressure of 4 cm H2O. On the third day of intubation, his temperature is 37.3°C (99.1°F), pulse is 91/min, and blood pressure is 103/60 mm Hg. There are decreased breath sounds over the left lung base. Cardiac examination shows no abnormalities. The abdomen is soft and not distended. Arterial blood gas analysis shows:
pH 7.49
pCO2 29 mm Hg
pO2 73 mm Hg
HCO3- 20 mEq/L
O2 saturation 89%
Monitoring shows a sudden increase in the plateau airway pressure. An x-ray of the chest shows deepening of the costophrenic angle on the left side. Which of the following is the most appropriate next step in management?
- A. CT scan of the chest
- B. Administer levofloxacin
- C. Close observation
- D. Increase the PEEP
- E. Insertion of a chest tube (Correct Answer)
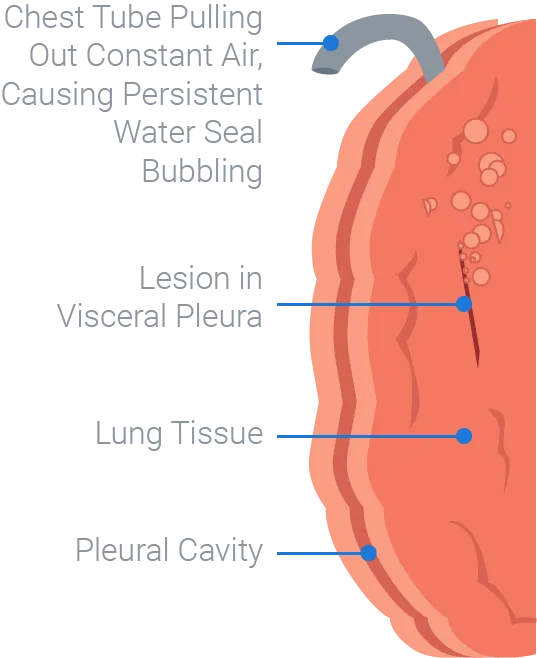
Chest tube insertion and management Explanation: ***Insertion of a chest tube***
- The sudden increase in **plateau airway pressure**, decreased breath sounds over the left lung base, worsening hypoxemia (O2 sat 89%) despite high FiO2, and **deepening of the costophrenic angle on the left side** indicate a **traumatic hemothorax**.
- Deepening of the costophrenic angle on chest X-ray is a classic sign of **pleural fluid accumulation** (hemothorax or pleural effusion), not pneumothorax.
- In a trauma patient (high-speed motor vehicle collision) on day 3 of mechanical ventilation, this represents a **delayed hemothorax** requiring immediate drainage.
- **Chest tube insertion** is the definitive management to evacuate blood, re-expand the lung, and improve ventilation and oxygenation.
*CT scan of the chest*
- While CT scan would provide detailed anatomical information, the clinical presentation with sudden respiratory decompensation and clear chest X-ray findings of hemothorax requires **immediate intervention**.
- Delaying treatment to obtain CT imaging in an unstable ventilated patient could worsen hypoxemia and lead to cardiovascular compromise.
- CT scan may be obtained later if needed to evaluate for ongoing bleeding or other injuries.
*Administer levofloxacin*
- Antibiotics would be appropriate for **pneumonia or empyema**, but the patient has no clear signs of infection (afebrile at 37.3°C, acute presentation over hours not days).
- The primary problem is **mechanical compression** from pleural fluid accumulation, not infection.
- Antibiotics do not address the life-threatening respiratory compromise from hemothorax.
*Close observation*
- Close observation is inappropriate given the acute deterioration with increased plateau pressures and worsening hypoxemia.
- The patient requires urgent intervention to prevent further respiratory failure and potential cardiovascular collapse.
- Expectant management would be negligent in this clinical scenario.
*Increase the PEEP*
- Increasing **Positive End-Expiratory Pressure (PEEP)** would worsen the situation by increasing intrathoracic pressure against an already compressed lung.
- Higher PEEP could impair venous return, decrease cardiac output, and potentially convert a simple hemothorax to a tension physiology.
- PEEP adjustments do not address the underlying problem of pleural space fluid accumulation requiring drainage.
Chest tube insertion and management US Medical PG Question 6: A 75-year-old man is brought to the emergency department because of a 5-hour history of worsening chest pain and dyspnea. Six days ago, he fell in the shower and since then has had mild pain in his left chest. He appears pale and anxious. His temperature is 36.5°C (97.7°F), pulse is 108/min, respirations are 30/min, and blood pressure is 115/58 mm Hg. Pulse oximetry on room air shows an oxygen saturation of 88%. Examination shows decreased breath sounds and dullness to percussion over the left lung base. There is a 3-cm (1.2-in) hematoma over the left lower chest. An x-ray of the chest shows fractures of the left 8th and 9th rib, increased opacity of the left lung, and mild tracheal deviation to the right. Which of the following is the most appropriate next step in management?
- A. Pericardiocentesis
- B. Emergency thoracotomy
- C. Admission to the ICU and observation
- D. Needle thoracentesis in the eighth intercostal space at the posterior axillary line
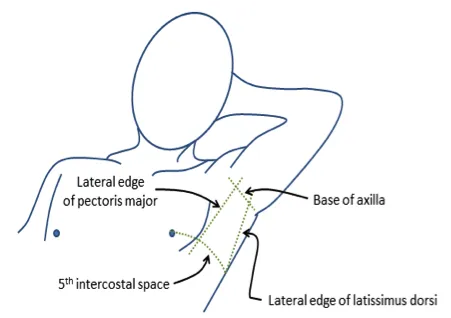
- E. Chest tube insertion in the fifth intercostal space at the midaxillary line (Correct Answer)
Chest tube insertion and management Explanation: ***Chest tube insertion in the fifth intercostal space at the midaxillary line***
- The patient's symptoms (worsening chest pain, dyspnea, pallor, anxiety, tachycardia, tachypnea, hypotension, hypoxemia) and signs (decreased breath sounds, dullness to percussion, increased opacity on X-ray, rib fractures) are highly suggestive of a **hemothorax** secondary to trauma, which requires urgent drainage.
- Placement of a **large-bore chest tube** in the **fifth intercostal space at the midaxillary line** is the appropriate intervention for evacuating blood and air from the pleural space, allowing lung re-expansion and improving respiratory and hemodynamic status.
*Pericardiocentesis*
- This procedure is indicated for **cardiac tamponade**, which is characterized by jugular venous distension, muffled heart sounds, and pulsus paradoxus, none of which are classic findings here.
- The patient's symptoms are more consistent with a pleural space issue rather than pericardial compression.
*Emergency thoracotomy*
- This is an invasive surgical procedure typically reserved for patients with severe, life-threatening thoracic trauma, such as massive hemorrhage or penetrating cardiac injury, who are unresponsive to less invasive resuscitation efforts.
- While the patient is unstable, a chest tube is the initial, less invasive, and often sufficient intervention for hemothorax.
*Admission to the ICU and observation*
- The patient's **hemodynamic instability** (ongoing hypotension, tachycardia), **respiratory distress** (tachypnea, hypoxemia), and clear radiographic evidence of a significant pleural effusion/hemothorax (increased opacity, tracheal deviation) indicate an urgent need for intervention, not just observation.
- Delaying definitive treatment for a large hemothorax can lead to further decompensation and poor outcomes.
*Needle thoracentesis in the eighth intercostal space at the posterior axillary line*
- While needle thoracentesis can be used for pleural fluid sampling or temporary relief of tension pneumothorax, it is insufficient for draining a significant **hemothorax**, which involves large volumes of blood and often clots.
- A chest tube is required for adequate drainage in such cases. The eighth intercostal space is also lower than the typical placement for chest tube insertion in trauma for drainage of general fluid/air and might be less effective for complete drainage or carry a higher risk of abdominal organ injury if fluid levels are typical.
Chest tube insertion and management US Medical PG Question 7: A 19-year-old man is brought to the emergency department 35 minutes after being involved in a high-speed motor vehicle collision. On arrival, he is alert, has mild chest pain, and minimal shortness of breath. He has one episode of vomiting in the hospital. His temperature is 37.3°C (99.1°F), pulse is 108/min, respirations are 23/min, and blood pressure is 90/70 mm Hg. Pulse oximetry on room air shows an oxygen saturation of 92%. Examination shows multiple abrasions over his trunk and right upper extremity. There are coarse breath sounds over the right lung base. Cardiac examination shows no murmurs, rubs, or gallop. Infusion of 0.9% saline is begun. He subsequently develops increasing shortness of breath. Arterial blood gas analysis on 60% oxygen shows:
pH 7.36
pCO2 39 mm Hg
pO2 68 mm Hg
HCO3- 18 mEq/L
O2 saturation 81%
An x-ray of the chest shows patchy, irregular infiltrates over the right lung fields. Which of the following is the most likely diagnosis?
- A. Pneumothorax
- B. Pulmonary contusion (Correct Answer)
- C. Aspiration pneumonia
- D. Acute respiratory distress syndrome
- E. Pulmonary embolism
Chest tube insertion and management Explanation: ***Pulmonary contusion***
- The patient's presentation with **hypoxia**, increasing shortness of breath after a high-speed motor vehicle collision, and **patchy, irregular infiltrates** on chest x-ray despite initial hydration, are highly suggestive of **pulmonary contusion**.
- The coarse breath sounds over the right lung base further support the presence of parenchymal injury and hemorrhage in the lung tissue.
*Pneumothorax*
- While a pneumothorax is common after trauma, the chest x-ray would typically show a **collapsed lung** and **absence of lung markings** in the affected area, which is not described.
- The presence of coarse breath sounds suggests air entry, not a complete absence due to collapsed lung.
*Aspiration pneumonia*
- Although the patient had one episode of vomiting, **aspiration pneumonia** typically develops hours to days after aspiration, presenting with fever and signs of infection.
- The acute onset of symptoms within minutes of trauma and the lack of fever make aspiration pneumonia less likely as the primary diagnosis immediately following the accident.
*Acute respiratory distress syndrome*
- **Acute respiratory distress syndrome (ARDS)** is a severe inflammatory lung injury that typically develops **24 to 72 hours** after an initial insult, not immediately.
- While the patient has hypoxia, the diffuse bilateral infiltrates characteristic of ARDS are not seen, and his symptoms are too acute for ARDS to be the primary cause at 35 minutes post-injury.
*Pulmonary embolism*
- A **pulmonary embolism** would typically present with sudden onset of shortness of breath and pleuritic chest pain, often without significant findings on chest x-ray or presenting with a **wedge-shaped infiltrate**.
- Given the direct chest trauma and immediate onset of respiratory compromise, a pulmonary contusion is a more direct and acute consequence.
Chest tube insertion and management US Medical PG Question 8: A 70-year-old man with severe ischemic cardiomyopathy (EF 25%) has recurrent ventricular tachycardia despite optimal medical therapy and ICD placement. Cardiac MRI shows a large anteroseptal scar with viable myocardium in the lateral and inferior walls. He has three-vessel coronary disease. His daughter is advocating for heart transplantation, but he has multiple comorbidities including obesity (BMI 37) and active tobacco use. Evaluate the management priority and rationale.
- A. Left ventricular assist device as destination therapy
- B. Catheter ablation of VT with continued ICD monitoring
- C. Cardiac resynchronization therapy upgrade and medication adjustment
- D. List for heart transplantation immediately given severe cardiomyopathy
- E. CABG with surgical ventricular reconstruction and continued medical optimization (Correct Answer)
Chest tube insertion and management Explanation: ***CABG with surgical ventricular reconstruction and continued medical optimization***
- The patient has **three-vessel disease** and **viable myocardium** in the lateral and inferior walls; **CABG** addresses the ischemic substrate and potentially improves **LVEF**.
- **Surgical ventricular reconstruction (SVR)** addresses the large **anteroseptal scar**, reducing left ventricular volume and providing better geometric stability to mitigate **ventricular tachycardia** (VT).
*Left ventricular assist device as destination therapy*
- While **LVAD** is an option for end-stage heart failure, the presence of **active tobacco use** and **obesity** (BMI 37) are significant relative contraindications.
- **Surgical revascularization** is prioritized when significant **viable myocardium** is present and surgical targets are available.
*Catheter ablation of VT with continued ICD monitoring*
- **VT ablation** target-treats the arrhythmia but does not address the underlying **remodelling** or **ischemia** causing the progressive cardiomyopathy.
- Given the **three-vessel disease**, surgical intervention is more comprehensive for long-term prognosis compared to percutaneous ablation alone.
*Cardiac resynchronization therapy upgrade and medication adjustment*
- The patient is already on **optimal medical therapy** with an **ICD**; simple medication adjustment is unlikely to control recurrent VT in the setting of structural scar and ischemia.
- **CRT** provides limited benefit if the primary issue is a large **anteroseptal scar** and **active ischemia** requiring revascularization.
*List for heart transplantation immediately given severe cardiomyopathy*
- Direct listing is contraindicated due to **active tobacco use** and a **BMI >35**, which are standard exclusion criteria for transplant programs.
- Heart transplantation is considered a last resort after maximizing options like **revascularization** and addressing **modifiable risk factors**.
Chest tube insertion and management US Medical PG Question 9: A 49-year-old woman with myasthenia gravis undergoes CT chest showing a 5 cm anterior mediastinal mass with irregular borders. Biopsy confirms thymoma (WHO type B2). She has well-controlled myasthenic symptoms on pyridostigmine. Staging shows no distant metastases, but the mass abuts the pericardium without clear invasion. Evaluate the optimal treatment approach.
- A. Thymectomy with possible en bloc pericardial resection, followed by adjuvant radiation (Correct Answer)
- B. Increase immunosuppression then delayed surgery in 6 months
- C. Radiation therapy alone to preserve myasthenia control
- D. Immediate thymectomy followed by observation
- E. Neoadjuvant chemotherapy, then thymectomy and adjuvant radiation
Chest tube insertion and management Explanation: ***Thymectomy with possible en bloc pericardial resection, followed by adjuvant radiation***
- Complete **surgical resection (R0)** is the cornerstone of treatment for **WHO type B2 thymomas**, especially when the mass is resectable despite abutting local structures like the **pericardium**.
- **Adjuvant radiation** is indicated for **Masaoka Stage II/III** disease or high-risk B2 histology to minimize the risk of **local recurrence**.
*Increase immunosuppression then delayed surgery in 6 months*
- Delaying surgery for a 5 cm **potentially invasive thymoma** allows for tumor progression and increases the risk of higher-stage disease.
- **Myasthenia gravis** symptoms are already **well-controlled**, making immediate surgical intervention safe and the preferred priority.
*Radiation therapy alone to preserve myasthenia control*
- **Radiation alone** is not a curative intent treatment for resectable thymoma and is usually reserved for **unresectable** or medically unfit patients.
- Thymectomy is actually a therapeutic part of managing **myasthenia gravis**, often leading to symptomatic improvement or remission.
*Immediate thymectomy followed by observation*
- Observation alone after surgery is insufficient for **B2 thymomas** that show irregular borders or high-risk features like **pericardial involvement**.
- The size over 5 cm and contact with the **pericardium** (Stage IIb/III) necessitate **postoperative radiotherapy** to improve oncologic outcomes.
*Neoadjuvant chemotherapy, then thymectomy and adjuvant radiation*
- **Neoadjuvant chemotherapy** is typically reserved for tumors deemed **primarily unresectable** on imaging, which is not the case here.
- Since the mass only **abuts** the pericardium and has no distant metastases, it is considered **upfront resectable**.
Chest tube insertion and management US Medical PG Question 10: A 58-year-old man with coronary artery disease requires CABG. Preoperative angiography shows 90% left main stenosis, 95% proximal LAD stenosis, 80% circumflex stenosis, and chronic total occlusion of the RCA with collaterals. He has diabetes, renal insufficiency (Cr 2.1), and previous stroke. Evaluate the optimal grafting strategy to maximize long-term patency and outcomes.
- A. Bilateral internal mammary arteries with supplemental vein grafts
- B. Off-pump CABG with sequential vein grafts only
- C. LIMA to LAD, radial artery to circumflex, vein graft to RCA (Correct Answer)
- D. All saphenous vein grafts to minimize operative time
- E. LIMA to LAD, saphenous vein grafts to remaining vessels
Chest tube insertion and management Explanation: ***LIMA to LAD, radial artery to circumflex, vein graft to RCA***
- The **LIMA-to-LAD** graft is the gold standard, providing the best long-term patency and survival outcomes in multi-vessel **CABG**.
- Using a **radial artery** for the circumflex system (high-grade stenosis) offers superior patency over vein grafts while avoiding the high risk of **sternal wound infection** associated with **BIMA** in diabetic patients.
*Bilateral internal mammary arteries with supplemental vein grafts*
- While **BIMA** provides excellent patency, it is associated with a significantly increased risk of **sternal dehiscence** and infection in patients with **Diabetes Mellitus**.
- The benefit of a second arterial graft is better achieved with the **radial artery** in this high-risk comorbid profile.
*Off-pump CABG with sequential vein grafts only*
- **Sequential vein grafts** have lower long-term patency compared to arterial conduits and do not capitalize on the survival benefit of the **LIMA-to-LAD**.
- Off-pump surgery might reduce some risks but using only vein grafts is suboptimal for a 58-year-old with **long-term** survival goals.
*All saphenous vein grafts to minimize operative time*
- **Saphenous vein grafts (SVG)** have much higher failure rates (approx. 50% at 10 years) compared to **internal mammary arteries**.
- Minimizing operative time does not justify the poor long-term clinical outcomes and higher **re-intervention rates** associated with an all-SVG strategy.
*LIMA to LAD, saphenous vein grafts to remaining vessels*
- This is a standard approach, but the addition of a second arterial conduit like the **radial artery** is preferred for younger patients with high-grade stenosis to maximize **patency**.
- In the setting of **90% left main** and **80% circumflex** stenosis, the radial artery is more durable than a vein graft for the circumflex target.
More Chest tube insertion and management US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.