Aortic surgery basics US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Aortic surgery basics. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Aortic surgery basics US Medical PG Question 1: A 23-year-old man comes to the emergency department with an open wound on his right hand. He states that he got into a bar fight about an hour ago. He appears heavily intoxicated and does not remember the whole situation, but he does recall lying on the ground in front of the bar after the fight. He does not recall any history of injuries but does remember a tetanus shot he received 6 years ago. His temperature is 37°C (98.6°F), pulse is 77/min, and blood pressure is 132/78 mm Hg. Examination shows a soft, nontender abdomen. His joints have no bony deformities and display full range of motion. There is a 4-cm (1.6-in) lesion on his hand with the skin attached only on the ulnar side. The wound, which appears to be partly covered with soil and dirt, is irrigated and debrided by the hospital staff. Minimal erythema and no purulence is observed in the area surrounding the wound. What is the most appropriate next step in management?
- A. Apposition of wound edges under tension + rifampin
- B. Surgical treatment with skin flap + ciprofloxacin
- C. Surgical treatment with skin graft + tetanus vaccine
- D. Tension-free apposition of wound edges + sterile dressing
- E. Application of moist sterile dressing + tetanus vaccine (Correct Answer)
Aortic surgery basics Explanation: ***Application of moist sterile dressing + tetanus vaccine***
- This approach is appropriate for a **contaminated, high-risk avulsion wound** to prevent infection and promote healing by secondary intention.
- The patient needs an updated **tetanus vaccine** because his last one was six years ago, and he has a contaminated wound.
*Apposition of wound edges under tension + rifampin*
- **Closing a contaminated wound under tension** is contraindicated as it increases the risk of infection and necrosis.
- **Rifampin is generally not the first-line prophylactic antibiotic** for this type of wound injury and is not needed if the wound has been thoroughly cleaned.
*Surgical treatment with skin flap + ciprofloxacin*
- This is an **overly aggressive initial approach** for an acute, contaminated wound, as the priority is preventing infection before definitive closure or reconstruction.
- **Ciprofloxacin** is not typically the first-choice prophylactic antibiotic for contaminated soft tissue wounds.
*Surgical treatment with skin graft + tetanus vaccine*
- A **skin graft** is a definitive reconstructive procedure and is not indicated as the immediate next step for a fresh, contaminated avulsion wound.
- The wound first needs to be thoroughly cleaned and monitored for infection before considering graft options.
*Tension-free apposition of wound edges + sterile dressing*
- While **tension-free closure** is ideal, this wound is **heavily contaminated with soil and dirt** and has some avulsion, making primary closure risky due to a high infection rate.
- **Allowing the wound to heal by secondary intention** with a moist dressing is safer in this situation.
Aortic surgery basics US Medical PG Question 2: A 58-year-old man is brought to the emergency department by his family because of severe upper back pain, which he describes as ripping. The pain started suddenly 1 hour ago while he was watching television. He has hypertension for 13 years, but he is not compliant with his medications. He denies the use of nicotine, alcohol or illicit drugs. His temperature is 36.5°C (97.7°F), the heart rate is 110/min and the blood pressure is 182/81 mm Hg in the right arm and 155/71 mm Hg in the left arm. CT scan of the chest shows an intimal flap limited to the descending aorta. Intravenous opioid analgesia is started. Which of the following is the best next step in the management of this patient condition?
- A. Intravascular ultrasound
- B. Emergency surgical intervention
- C. Sublingual nitroglycerin
- D. Intravenous esmolol (Correct Answer)
- E. Oral metoprolol and/or enalapril
Aortic surgery basics Explanation: ***Intravenous esmolol***
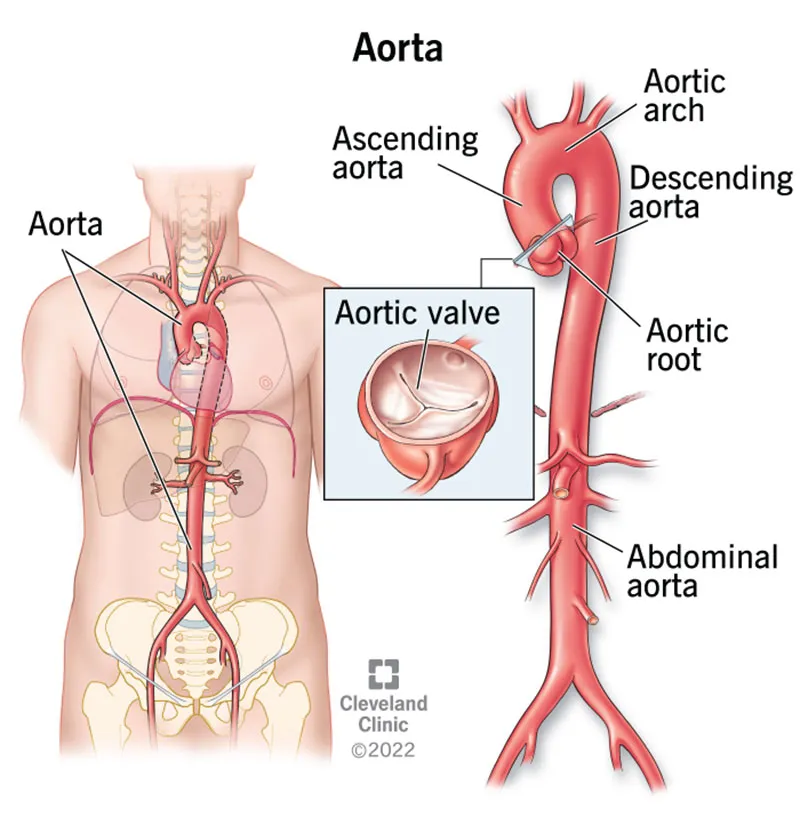
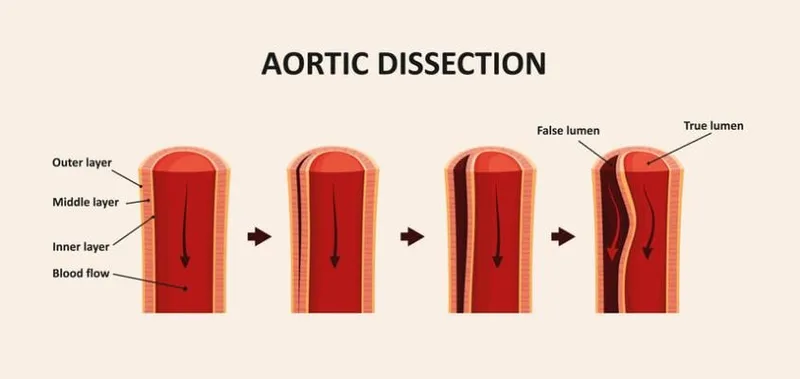
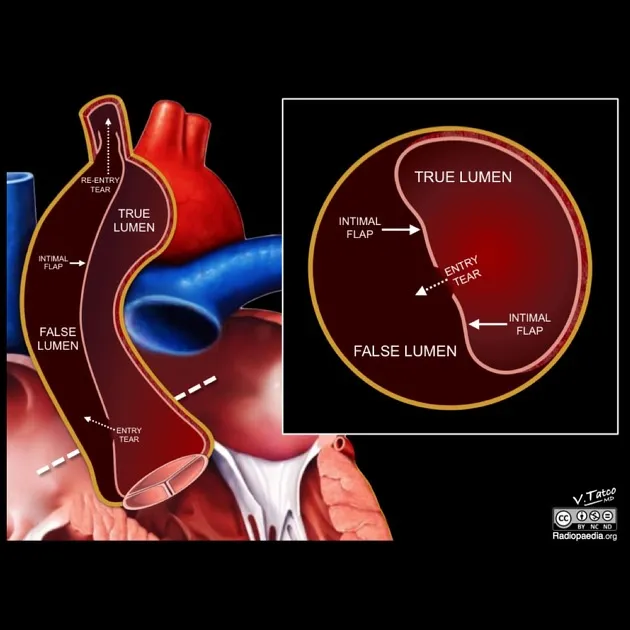
- This patient presents with an **acute aortic dissection** (descending aorta, Type B), characterized by sudden severe ripping back pain and a significant blood pressure difference between the arms [1]. The immediate priority is to reduce **heart rate** and **blood pressure** to decrease shear stress on the aortic wall and prevent progression of the dissection.
- **Intravenous beta-blockers** like esmolol are the first-line medical treatment for uncomplicated Type B aortic dissections, as they rapidly decrease heart rate and blood pressure, which helps to mitigate further aortic injury.
*Intravascular ultrasound*
- While intravascular ultrasound can provide detailed imaging of the aorta, it is an **invasive procedure** and not the immediate next step in managing an acute, hemodynamically unstable condition like aortic dissection where rapid blood pressure control is paramount.
- The patient already has a diagnostic CT scan confirming the intimal flap; thus, additional imaging during the acute stabilization phase is not typically the first priority over medical management [2].
*Emergency surgical intervention*
- **Emergency surgical intervention** is primarily indicated for **Type A aortic dissections** (involving the ascending aorta) or for complicated Type B dissections (e.g., malperfusion, rupture, rapid expansion) [1].
- This patient has an **uncomplicated Type B dissection** (limited to the descending aorta) that is initially managed medically with aggressive heart rate and blood pressure control.
*Sublingual nitroglycerin*
- **Nitroglycerin** primarily causes **vasodilation**, which can lower blood pressure but also induces reflex tachycardia, potentially increasing shear stress on the dissected aorta.
- It is **contraindicated** in acute aortic dissection as the increase in heart rate can worsen the dissection.
*Oral metoprolol and/or enalapril*
- **Oral medications** like metoprolol and enalapril are not suitable for the **initial acute management** of aortic dissection because their onset of action is too slow to achieve rapid and precise control of heart rate and blood pressure.
- **Intravenous agents** are required for immediate and titratable blood pressure and heart rate reduction in this emergency setting.
Aortic surgery basics US Medical PG Question 3: A 68-year-old man presents for a screening ultrasound scan. He has been feeling well and is in his usual state of good health. His medical history is notable for mild hypertension and a 100-pack-year tobacco history. He has a blood pressure of 128/86 and heart rate of 62/min. Physical examination is clear lung sounds and regular heart sounds. On ultrasound, an infrarenal aortic aneurysm of 4 cm in diameter is identified. Which of the following is the best initial step for this patient?
- A. Reassurance
- B. Beta-blockers
- C. Urgent repair
- D. Surveillance (Correct Answer)
- E. Elective repair
Aortic surgery basics Explanation: **Surveillance**
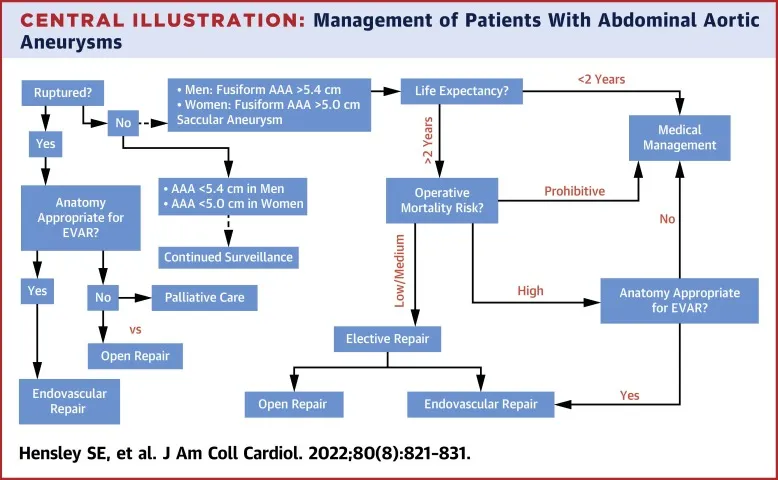
- An **infrarenal aortic aneurysm** of 4 cm in diameter in an asymptomatic patient is typically managed with **regular surveillance** to monitor for growth.
- Surgical intervention is generally reserved for aneurysms larger than 5.5 cm or those that are rapidly expanding or symptomatic.
*Reassurance*
- While it's important to provide reassurance, simply doing so without a concrete plan for follow-up would be inappropriate given the potential for **aneurysm expansion** and rupture.
- The patient's **tobacco history** is a significant risk factor for aneurysm progression and warrants monitoring.
*Beta-blockers*
- Beta-blockers may be part of the medical management for **hypertension** and could theoretically slow aneurysm growth by reducing pulsatile stress.
- However, they are not the primary **initial step** for an asymptomatic aneurysm of this size and do not replace the need for surveillance.
*Urgent repair*
- **Urgent repair** is indicated for symptomatic aneurysms, those that are rapidly expanding, or those showing signs of rupture or impending rupture, none of which are present here.
- A 4 cm aneurysm in an asymptomatic patient does not meet the criteria for **urgent intervention**.
*Elective repair*
- **Elective repair** is typically considered for aneurysms exceeding 5.5 cm in diameter or those that are symptomatic or rapidly growing.
- A 4 cm aneurysm is below the threshold for **elective repair** in an asymptomatic patient without other high-risk features.
Aortic surgery basics US Medical PG Question 4: A 64-year-old woman has progressively worsening abdominal pain 5 hours after an open valve replacement with cardiopulmonary bypass. The pain is crampy and associated with an urge to defecate. The patient reports having had 2 bloody bowel movements in the last hour. Her operation was complicated by significant intraoperative blood loss, which prolonged the operation and necessitated 2 transfusions of red blood cells. She has hypercholesterolemia and type 2 diabetes mellitus. The patient received prophylactic perioperative antibiotics and opioid pain management during recovery. Her temperature is 37.9°C (98.9°F), pulse is 95/min, and blood pressure is 115/69 mm Hg. Examination shows a soft abdomen with mild tenderness to palpation in the left quadrants but no rebound tenderness or guarding. Bowel sounds are decreased. Rectal examination shows blood on the examining finger. Which of the following is the most likely underlying cause of this patient's symptoms?
- A. Embolization of superior mesenteric artery
- B. Atherosclerotic narrowing of the intestinal vessels
- C. Small outpouchings in the sigmoid wall
- D. Infection with Clostridioides difficile
- E. Decreased blood flow to the splenic flexure (Correct Answer)
Aortic surgery basics Explanation: ***Decreased blood flow to the splenic flexure***
- This patient's symptoms are highly suggestive of **ischemic colitis**, which often affects the **splenic flexure** due to its "watershed" area vulnerability. **Cardiopulmonary bypass** and significant **intraoperative blood loss** (leading to hypotension and hypoperfusion) are major risk factors for this condition.
- The presentation with **crampy abdominal pain**, **urgent defecation**, and **bloody bowel movements** shortly after cardiac surgery points to colonic ischemia.
*Embolization of superior mesenteric artery*
- While an acute **SMA embolism** could cause severe abdominal pain and bloody stools, it typically presents with **more diffuse and severe abdominal tenderness**, often with marked tenderness disproportionate to examination findings early on, and rapid progression to peritonitis.
- The patient's history of valvular disease and hypercholesterolemia increases the risk of embolization, but the **mild tenderness confined to left quadrants** and decreased bowel sounds are less typical of an acute SMA occlusion.
*Atherosclerotic narrowing of the intestinal vessels*
- This describes **chronic mesenteric ischemia**, which typically causes **postprandial abdominal pain** (intestinal angina) and weight loss, not acute abdominal pain and bloody diarrhea in the immediate postoperative period.
- While the patient has risk factors for atherosclerosis (hypercholesterolemia, diabetes), the acute onset of symptoms following cardiac surgery points to an acute ischemic event rather than chronic narrowing.
*Small outpouchings in the sigmoid wall*
- This refers to **diverticulitis** or **diverticular bleeding**. While diverticular bleeding can cause painless or painful bleeding, and diverticulitis can cause abdominal pain, the acute onset post-cardiac surgery in the setting of hypoperfusion makes ischemic colitis a more likely diagnosis.
- Diverticulitis typically presents with **localized left lower quadrant pain**, fever, and leukocytosis, but the systemic context of recent cardiac surgery and hypoperfusion strongly favors ischemia.
*Infection with Clostridioides difficile*
- **_Clostridioides difficile_ infection** typically causes **watery diarrhea**, often after antibiotic use, and usually takes several days to develop symptoms after exposure or antibiotic initiation.
- Although the patient received perioperative antibiotics, the onset of symptoms within hours of surgery and the presence of **frank bloody stools** are less characteristic of _C. difficile_ infection, which is more commonly associated with non-bloody diarrhea.
Aortic surgery basics US Medical PG Question 5: A 56-year-old man is brought to the emergency department 25 minutes after the sudden onset of severe pain in the middle of his chest. He describes the pain as tearing in quality; it radiates to his jaw. He has hypertension. He has smoked one pack of cigarettes daily for the 25 years. Current medications include enalapril. His blood pressure is 154/95 mm Hg in his right arm and 181/105 mm Hg in his left arm. A CT scan of the chest is shown. The structure indicated by the arrow is a derivative of which of the following?
- A. Right horn of sinus venosus
- B. Primitive atrium
- C. Right common cardinal vein
- D. Truncus arteriosus (Correct Answer)
- E. Bulbus cordis
Aortic surgery basics Explanation: ***Truncus arteriosus***
- This clinical scenario describes an **aortic dissection**, suggested by the sudden onset of **tearing chest pain radiating to the jaw**, significant **blood pressure differential** between arms, and presenting in a patient with **hypertension and smoking history**.
- The image likely shows a dilated aorta or an aortic dissection. The **truncus arteriosus** is the embryonic precursor to the **ascending aorta** and the **pulmonary trunk**, making it the correct derivative for the affected structure.
*Right horn of sinus venosus*
- The **right horn of the sinus venosus** primarily contributes to the formation of the **smooth-walled part of the right atrium** (sinus venarum).
- It does not give rise to the aorta, which is the structure involved in the described pathology.
*Primitive atrium*
- The **primitive atrium** develops into the **trabeculated parts** of both the **right and left atria** (atrial appendages).
- It is not involved in the formation of the great arteries like the aorta.
*Right common cardinal vein*
- The **right common cardinal vein** contributes to the formation of the **superior vena cava**.
- It is not a developmental source for the aorta.
*Bulbus cordis*
- The **bulbus cordis** gives rise to the **conus arteriosus** (infundibulum) of the right ventricle, the **aortic vestibule** of the left ventricle, and part of the **right ventricle**.
- While it is a component of the outflow tract, the primary structure from which the ascending aorta develops is the truncus arteriosus.
Aortic surgery basics US Medical PG Question 6: A 70-year-old male comes to the emergency department complaining of severe back pain. The pain started 20 minutes ago when he was sitting and watching TV. He describes the pain as intense, epigastric, and radiating to his back. His vitals on presentation to the emergency department are blood pressure is 150/75 mmHg, pulse is 110/min, and respirations are 24/min with an oxygen saturation of 98% on room air. His body mass index is 35 kg/m^2 and he appears pale and in visible pain. On abdominal exam, his abdomen is tender and a pulsatile mass is felt in the midline during deep palpation. His past medical history includes diabetes, hypertension well-controlled on medications, and a history of benign prostatic hyperplasia. His social history is notable for consuming 2-3 beers per night and a smoking history of ½ pack per day. Which of the following is considered the greatest risk factor for this patient's condition?
- A. Smoking (Correct Answer)
- B. Benign prostatic hyperplasia
- C. Obesity
- D. Diabetes
- E. Alcohol consumption
Aortic surgery basics Explanation: ***Smoking***
- **Smoking** is the single most significant modifiable risk factor for the development and expansion of **abdominal aortic aneurysms (AAAs)** due to its detrimental effects on arterial wall integrity.
- Nicotine and other toxins in smoke contribute to **inflammation**, **oxidative stress**, and **elastin degradation** within the aortic wall.
*Benign prostatic hyperplasia*
- **Benign prostatic hyperplasia (BPH)** is not a risk factor for abdominal aortic aneurysm formation or rupture.
- It is a condition of the prostate gland causing urinary symptoms and has no pathophysiological link to aortic disease.
*Obesity*
- While **obesity** is a risk factor for many cardiovascular diseases, its association with **abdominal aortic aneurysms (AAAs)** is less direct than other factors, often mediated through related conditions like hypertension.
- Some studies suggest a **protective effect** or no significant association between obesity and AAA, although this remains an area of ongoing research.
*Diabetes*
- **Diabetes** is generally considered to have a **paradoxical or even protective effect** against the development of **abdominal aortic aneurysms (AAAs)**, although it significantly increases the risk of other vascular complications.
- The exact mechanism is not fully understood but may involve changes in the aortic wall's structural properties or reduced inflammation in diabetic patients with AAAs.
*Alcohol consumption*
- **Moderate alcohol consumption** has not been consistently linked to an increased risk of **abdominal aortic aneurysms (AAAs)**.
- **Excessive alcohol consumption** can contribute to overall cardiovascular disease risk, but it is not identified as a primary or strong independent risk factor for AAA formation or rupture.
Aortic surgery basics US Medical PG Question 7: A 58-year-old man presents to the emergency department for evaluation of intermittent chest pain over the past 6 months. His history reveals that he has had moderate exertional dyspnea and 2 episodes of syncope while working at his factory job. These episodes of syncope were witnessed by others and lasted roughly 30 seconds. The patient states that he did not have any seizure activity. His vital signs include: blood pressure 121/89 mm Hg, heart rate 89/min, temperature 37.0°C (98.6°F), and respiratory rate 16/min. Physical examination reveals a crescendo-decrescendo systolic murmur in the right second intercostal area. An electrocardiogram is performed, which shows left ventricular hypertrophy. Which of the following is the best next step for this patient?
- A. Transthoracic echocardiography (Correct Answer)
- B. Chest radiograph
- C. Computed tomography (CT) chest scan without contrast
- D. Cardiac chamber catheterization
- E. Transesophageal echocardiography
Aortic surgery basics Explanation: ***Transthoracic echocardiography***
- The patient's symptoms (chest pain, exertional dyspnea, syncope) and physical exam findings (**crescendo-decrescendo systolic murmur at the right second intercostal space**, ECG showing **left ventricular hypertrophy**) are highly suggestive of **aortic stenosis**.
- **Transthoracic echocardiography** is the gold standard for diagnosing and assessing the severity of valvular heart diseases like aortic stenosis, quantifying valve area, pressure gradients, and ventricular function.
*Chest radiograph*
- A chest radiograph provides information about lung fields, cardiac size, and aortic calcification, but it cannot directly visualize or assess the function of heart valves.
- While it may show signs of heart failure (e.g., **pulmonary congestion**) or **cardiomegaly**, it is insufficient for a definitive diagnosis or severity assessment of valvular lesions.
*Computed tomography (CT) chest scan without contrast*
- A CT scan can detect calcification of the aortic valve, but it is not the primary imaging modality for assessing valvular function or the severity of stenotic lesions.
- CT is more useful for evaluating the **aorta for aneurysm** or dissection, or for **pulmonary pathology**, neither of which is the most likely diagnosis given the presenting symptoms.
*Cardiac chamber catheterization*
- Cardiac catheterization is an **invasive procedure** that is typically reserved for cases where non-invasive imaging is inconclusive or when planning for intervention (e.g., prior to valve replacement).
- It involves risks and is not the initial best step for diagnosis when a less invasive and highly informative test like echocardiography is available.
*Transesophageal echocardiography*
- **Transesophageal echocardiography (TEE)** provides more detailed images of the heart and valves compared to TTE because it avoids acoustic shadowing from the ribs and lungs.
- However, TEE is more invasive than TTE and is usually reserved for situations where TTE is inadequate or when a higher resolution view is needed, such as for infective endocarditis, prosthetic valve dysfunction, or before/during surgical procedures.
Aortic surgery basics US Medical PG Question 8: A 67-year-old man presents to the emergency department with abdominal pain that started 1 hour ago. The patient has a past medical history of diabetes and hypertension as well as a 40 pack-year smoking history. His blood pressure is 107/58 mmHg, pulse is 130/min, respirations are 23/min, and oxygen saturation is 98% on room air. An abdominal ultrasound demonstrates focal dilation of the aorta with peri-aortic fluid. Which of the following is the best next step in management?
- A. Serial annual abdominal ultrasounds
- B. Emergent surgical intervention (Correct Answer)
- C. Administer labetalol
- D. Counsel the patient in smoking cessation
- E. Urgent surgery within the next day
Aortic surgery basics Explanation: ***Emergent surgical intervention***
- The patient's presentation with acute **abdominal pain**, **hypotension**, and **tachycardia** combined with ultrasound findings of focal aortic dilation and peri-aortic fluid strongly suggests a **ruptured abdominal aortic aneurysm (AAA)**.
- A ruptured AAA is a life-threatening emergency requiring immediate surgical repair to prevent further hemorrhage and death.
*Serial annual abdominal ultrasounds*
- This approach is appropriate for asymptomatic patients with smaller, stable AAAs (typically <5.5 cm) to monitor for growth.
- In this case, the patient is symptomatic with signs of rupture, making surveillance an inappropriate and dangerous management strategy.
*Administer labetalol*
- Medications like labetalol are used to control blood pressure in conditions like aortic dissection or to slow the progression of AAAs, but they are contraindicated in hypotensive patients with a ruptured AAA.
- In this patient, labetalol would worsen the existing hypotension and could lead to cardiovascular collapse.
*Counsel the patient in smoking cessation*
- Smoking cessation is a crucial long-term intervention to reduce the risk of AAA expansion and rupture.
- While important, it does not address the immediate, life-threatening emergency of a ruptured AAA.
*Urgent surgery within the next day*
- Waiting until the next day for surgery in a patient with a suspected ruptured AAA is unacceptable.
- The patient's hemodynamic instability (hypotension, tachycardia) indicates active bleeding, and any delay significantly increases morbidity and mortality.
Aortic surgery basics US Medical PG Question 9: A 72-year-old woman comes to the physician for follow-up care. One year ago, she was diagnosed with a 3.8-cm infrarenal aortic aneurysm found incidentally on abdominal ultrasound. She has no complaints. She has hypertension, type 2 diabetes mellitus, and COPD. Current medications include hydrochlorothiazide, lisinopril, glyburide, and an albuterol inhaler. She has smoked a pack of cigarettes daily for 45 years. Her temperature is 37°C (98.6°F), pulse is 90/min, respirations are 12/min, and blood pressure is 145/85 mm Hg. Examination shows a faint abdominal bruit on auscultation. Ultrasonography of the abdomen shows a 4.9-cm saccular dilation of the infrarenal aorta. Which of the following is the most appropriate next step in management?
- A. Elective endovascular aneurysm repair (Correct Answer)
- B. Adjustment of cardiovascular risk factors and follow-up ultrasound in 12 months
- C. Adjustment of cardiovascular risk factors and follow-up ultrasound in 6 months
- D. Elective open aneurysm repair
- E. Adjustment of cardiovascular risk factors and follow-up CT in 6 months
Aortic surgery basics Explanation: ***Elective endovascular aneurysm repair***
- The patient's **infrarenal aortic aneurysm** has grown from 3.8 cm to 4.9 cm in one year, approaching the **5.0 cm threshold for intervention in women** (compared to 5.5 cm for men). The **rapid growth rate of 1.1 cm/year** (normal is <0.5 cm/year) significantly increases rupture risk and is an indication for intervention even before reaching the absolute size threshold.
- Given her multiple comorbidities (hypertension, diabetes, COPD, 45 pack-year smoking history), **endovascular aneurysm repair (EVAR)** is preferred over open repair due to lower perioperative morbidity and mortality in high-risk surgical candidates.
- The combination of near-threshold size and rapid growth makes elective repair appropriate now rather than continued surveillance.
*Adjustment of cardiovascular risk factors and follow-up ultrasound in 12 months*
- While **risk factor modification** (smoking cessation, blood pressure control) is essential, it is insufficient as the primary management given the aneurysm's significant growth and imminent rupture risk.
- A 12-month follow-up interval is too long for a rapidly growing aneurysm (grew 1.1 cm in the past year), as this increases the risk of rupture without intervention.
*Adjustment of cardiovascular risk factors and follow-up ultrasound in 6 months*
- **Risk factor management** is important but does not address the immediate need for intervention due to the aneurysm's size approaching the threshold and concerning growth rate.
- While 6-month surveillance might be considered for smaller aneurysms with slower growth, this aneurysm's rapid expansion rate suggests it will exceed 5.0 cm well before the next surveillance interval, increasing rupture risk unnecessarily.
*Elective open aneurysm repair*
- **Open aneurysm repair** is an effective treatment but carries significantly higher perioperative risks (30-day mortality 3-5% vs 1-2% for EVAR) compared to endovascular repair, especially in patients with multiple comorbidities.
- Given this patient's COPD, smoking history, and cardiovascular risk factors, EVAR is the preferred approach to minimize surgical stress and improve perioperative outcomes.
*Adjustment of cardiovascular risk factors and follow-up CT in 6 months*
- **Risk factor modification** alone is insufficient given the aneurysm's proximity to intervention threshold and rapid growth rate.
- While CT provides more detailed anatomic imaging for surgical planning, continued surveillance is inappropriate when the patient already meets criteria for intervention. Additionally, CT involves radiation exposure and is typically reserved for pre-operative planning rather than routine surveillance.
Aortic surgery basics US Medical PG Question 10: A 32-year-old man is brought to the emergency department 15 minutes after falling 7 feet onto a flat-top wooden post. On arrival, he is in severe pain and breathing rapidly. His pulse is 135/min, respirations are 30/min, and blood pressure is 80/40 mm Hg. There is an impact wound in the left fourth intercostal space at the midaxillary line. Auscultation shows tracheal deviation to the right and absent breath sounds over the left lung. There is dullness to percussion over the left chest. Neck veins are flat. Cardiac examination shows no abnormalities. Two large-bore intravenous catheters are placed and intravenous fluid resuscitation is begun. Which of the following is the most likely diagnosis?
- A. Bronchial rupture
- B. Cardiac tamponade
- C. Flail chest
- D. Hemothorax (Correct Answer)
- E. Tension pneumothorax
Aortic surgery basics Explanation: ***Hemothorax***
- The combination of **absent breath sounds**, **dullness to percussion** on the left, and **hypotension with flat neck veins** following trauma strongly suggests a massive hemothorax causing **hypovolemic shock** from significant blood loss into the pleural space.
- The injury site at the **left fourth intercostal space** (midaxillary line) is a common location for vascular injury. Dullness to percussion indicates fluid (blood) accumulation, not air.
- **Flat neck veins** are the key finding distinguishing hypovolemic shock (blood loss) from obstructive shock (tension pneumothorax or tamponade would cause distended neck veins).
- Tracheal deviation away from the affected side can occur with massive hemothorax due to mediastinal shift from fluid accumulation.
*Bronchial rupture*
- While possible with severe trauma, bronchial rupture typically presents with significant **air leak**, leading to subcutaneous emphysema and persistent pneumothorax, rather than **dullness to percussion** (which indicates fluid, not air).
- Usually causes **hyperresonance** on percussion, not dullness. Does not typically cause immediate massive hypovolemic shock with flat neck veins.
*Cardiac tamponade*
- Characterized by **Beck's triad**: hypotension, muffled heart sounds, and **distended neck veins** (due to impaired venous return).
- This patient has **flat neck veins**, which rules out tamponade. Additionally, cardiac examination shows no abnormalities (would expect muffled heart sounds in tamponade).
*Flail chest*
- Involves **paradoxical chest wall movement** due to multiple rib fractures creating a free-floating segment. While it causes pain and respiratory distress, it does not explain absent breath sounds, dullness to percussion, tracheal deviation, or hypovolemic shock.
- The primary issue is usually underlying pulmonary contusion, not massive blood loss into the pleural space.
*Tension pneumothorax*
- Classic presentation includes **absent breath sounds**, **hyperresonance to percussion** (air accumulation), **tracheal deviation** away from affected side, and **distended neck veins** (obstructive shock).
- This patient has **dullness to percussion** (fluid, not air) and **flat neck veins** (hypovolemic, not obstructive shock), making tension pneumothorax incompatible with the clinical picture.
More Aortic surgery basics US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.