Post-mastectomy complications US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Post-mastectomy complications. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Post-mastectomy complications US Medical PG Question 1: A 76-year-old woman is brought to the physician because of lesions on her left arm. She first noticed them 3 months ago and they have grown larger since that time. She has not had any pain or pruritus in the area. She has a history of invasive ductal carcinoma of the left breast, which was treated with mastectomy and radiation therapy 27 years ago. Since that time, she has had lymphedema of the left arm. Physical examination shows extensive edema of the left arm. There are four coalescing, firm, purple-blue nodules on the left lateral axillary region and swelling of the surrounding skin. Which of the following is the most likely diagnosis?
- A. Thrombophlebitis
- B. Cellulitis
- C. Melanoma
- D. Angiosarcoma (Correct Answer)
- E. Kaposi sarcoma
Post-mastectomy complications Explanation: ***Angiosarcoma***
- The presence of **firm, purple-blue nodules** in a patient with **chronic lymphedema** following **mastectomy and radiation** for breast cancer is highly suggestive of **angiosarcoma (Stewart-Treves syndrome)**.
- This rare but aggressive vascular malignancy often presents as skin lesions in the setting of long-standing lymphedema, particularly in the upper extremity after breast cancer treatment.
*Thrombophlebitis*
- Typically presents with **erythema**, **tenderness**, and **pain** along the course of a superficial vein, which is not described here.
- The lesions would likely blanch with pressure and feel more like a cord or streak, rather than firm, discrete nodules.
*Cellulitis*
- Would present with **warmth**, **tenderness**, **erythema with ill-defined borders**, and often **fever**, none of which are mentioned.
- While lymphedema is a risk factor for cellulitis, the description of discrete, firm, purple-blue nodules growing over time is not characteristic.
*Melanoma*
- Although melanoma can present as a dark lesion, it often has **irregular borders**, **asymmetry**, and **color variegation**, and is typically associated with UV exposure.
- While it can be nodular, the specific context of chronic lymphedema and the description of purple-blue lesions are more indicative of a vascular tumor.
*Kaposi sarcoma*
- Characterized by **purple-brown skin lesions** and is primarily associated with **HIV infection** or **immunosuppression**, neither of which is indicated in this patient.
- While it is a vascular tumor, the unique presentation in the context of chronic lymphedema post-breast cancer therapy makes angiosarcoma a more fitting diagnosis.
Post-mastectomy complications US Medical PG Question 2: A 60-year-old woman is rushed to the emergency room after falling on her right elbow while walking down the stairs. She cannot raise her right arm. Her vital signs are stable, and the physical examination reveals loss of sensation over the upper lateral aspect of the right arm and shoulder. A radiologic evaluation shows a fracture of the surgical neck of the right humerus. Which of the following muscles is supplied by the nerve that is most likely damaged?
- A. Teres minor (Correct Answer)
- B. Teres major
- C. Subscapularis
- D. Infraspinatus
- E. Supraspinatus
Post-mastectomy complications Explanation: ***Teres minor***
- A fracture of the **surgical neck of the humerus** often damages the **axillary nerve**, which innervates the **teres minor**.
- The axillary nerve also supplies the **deltoid muscle** and provides cutaneous sensation to the **upper lateral arm**, consistent with the patient's sensory loss.
*Teres major*
- This muscle is innervated by the **lower subscapular nerve**, which is less likely to be damaged in a surgical neck fracture.
- Its primary action is **adduction** and **internal rotation** of the arm.
*Subscapularis*
- The **subscapularis** is innervated by the **upper and lower subscapular nerves**.
- While it contributes to internal rotation, its nerve supply is typically protected in this type of fracture.
*Infraspinatus*
- The **infraspinatus** muscle is innervated by the **suprascapular nerve**.
- This nerve is generally not affected by a fracture of the surgical neck of the humerus.
*Supraspinatus*
- Similar to the infraspinatus, the **supraspinatus** is also innervated by the **suprascapular nerve**.
- Damage to this nerve due to a humeral surgical neck fracture is uncommon.
Post-mastectomy complications US Medical PG Question 3: A 59-year-old woman presents to her primary care provider with a 6-month history of progressive left-arm swelling. Two years ago she had a partial mastectomy and axillary lymph node dissection for left breast cancer. She was also treated with radiotherapy at the time. Upon further questioning, she denies fever, pain, or skin changes, but reports difficulty with daily tasks because her hand feels heavy and weak. She is bothered by the appearance of her enlarged extremity and has stopped playing tennis. On physical examination, nonpitting edema of the left arm is noted with hyperkeratosis, papillomatosis, and induration of the skin. Limb elevation, exercise, and static compression bandaging are started. If the patient has no improvement, which of the following will be the best next step?
- A. Diethylcarbamazine
- B. Low molecular weight heparin
- C. Endovascular stenting
- D. Vascularized lymph node transfer (Correct Answer)
- E. Antibiotics
Post-mastectomy complications Explanation: ***Vascularized lymph node transfer***
- This patient presents with **secondary lymphedema** due to axillary dissection and radiotherapy, which has not responded to conservative management.
- **Vascularized lymph node transfer** is a surgical option that involves transplanting healthy lymph nodes to the affected area to re-establish lymphatic drainage pathways, offering a more definitive solution for refractory cases.
*Diethylcarbamazine*
- **Diethylcarbamazine** is an anti-filarial drug used to treat lymphedema caused by **parasitic infections**, specifically filariasis.
- The patient's lymphedema is secondary to breast cancer treatment, not parasitic infection, making this a **misdirected treatment**.
*Low molecular weight heparin*
- **Low molecular weight heparin** is an anticoagulant used to prevent or treat **venous thromboembolism (VTE)**.
- While patients with cancer are at increased risk for VTE, her symptoms are consistent with lymphedema and not thrombosis, which would typically present with more acute pain and swelling, making this an inappropriate treatment.
*Endovascular stenting*
- **Endovascular stenting** is a procedure used to open blocked or narrowed **blood vessels**, such as in peripheral artery disease or venous obstruction.
- Her condition is specifically lymphedema, a lymphatic circulation issue, not a vascular obstruction, so stenting would not address the underlying problem.
*Antibiotics*
- **Antibiotics** are used to treat **bacterial infections**, which can complicate lymphedema (e.g., cellulitis).
- While chronic lymphedema causes skin changes (hyperkeratosis, papillomatosis, induration), the patient shows no signs of **acute infection** such as fever, pain, erythema, or warmth, making empirical antibiotics unnecessary at this stage.
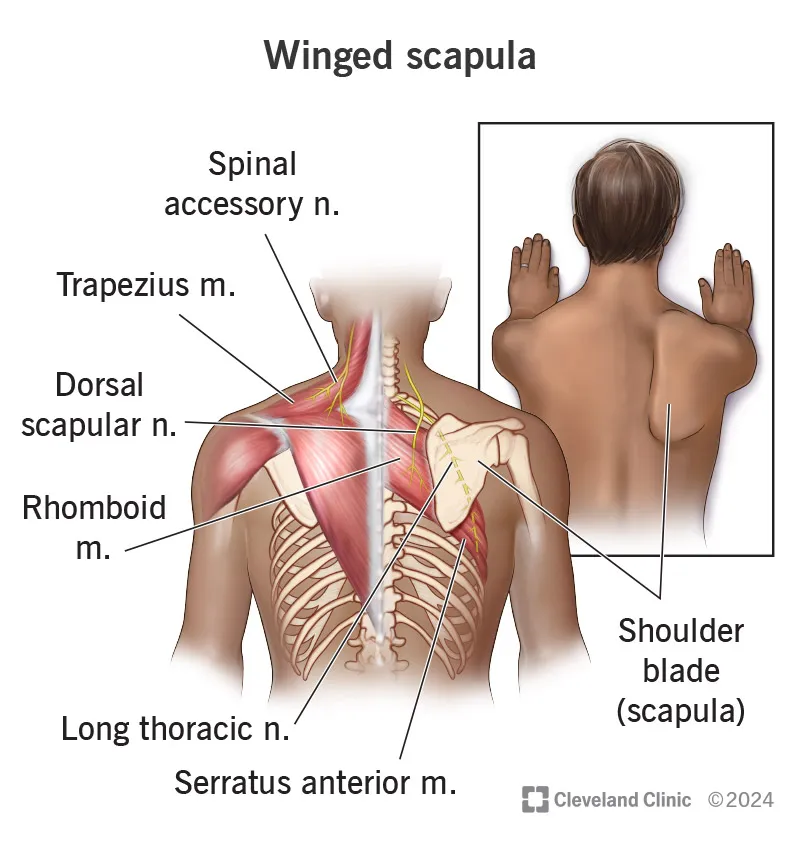
Post-mastectomy complications US Medical PG Question 4: A 40-year-old male presents to the physician's office complaining of an inability to push doors open. He has had this problem since he was playing football with his children and was tackled underneath his right arm on his lateral chest. On examination, he has a winged scapula on the right side. Which of the following nerves is most likely the cause of this presentation?
- A. Phrenic nerve
- B. Spinal accessory nerve
- C. Long thoracic nerve (Correct Answer)
- D. Greater auricular nerve
- E. Musculocutaneous nerve
Post-mastectomy complications Explanation: ***Long thoracic nerve***
- The **long thoracic nerve** innervates the **serratus anterior muscle**, which is responsible for scapular protraction and upward rotation.
- Damage to this nerve, often from trauma to the lateral chest wall (tackled underneath the arm), leads to paralysis of the serratus anterior and a characteristic **winged scapula** with lateral and inferior prominence.
- Patients have difficulty with **pushing movements** (protraction) and overhead activities.
*Phrenic nerve*
- The **phrenic nerve** primarily innervates the **diaphragm** and is crucial for respiration.
- Damage to the phrenic nerve would cause respiratory compromise, not a winged scapula or difficulty pushing doors.
*Spinal accessory nerve*
- The **spinal accessory nerve (cranial nerve XI)** innervates the **sternocleidomastoid** and **trapezius muscles**.
- Injury to this nerve can cause scapular winging due to **trapezius paralysis**, but the winging is typically **medial** with the inferior angle moving medially, unlike the lateral winging from serratus anterior paralysis.
- The mechanism of injury (lateral chest trauma during tackling) and inability to push are classic for **long thoracic nerve** injury, not spinal accessory nerve.
*Greater auricular nerve*
- The **greater auricular nerve** is a cutaneous nerve that provides sensation to the skin over the parotid gland, mastoid process, and auricle.
- Damage to this nerve would result in sensory loss in these areas and is unrelated to muscle weakness or a winged scapula.
*Musculocutaneous nerve*
- The **musculocutaneous nerve** innervates the **biceps brachii**, **brachialis**, and **coracobrachialis muscles**, responsible for elbow flexion and forearm supination.
- Damage to this nerve would primarily affect these movements and sensation in the lateral forearm, not leading to a winged scapula.
Post-mastectomy complications US Medical PG Question 5: A patient presents to the emergency department with arm pain. The patient recently experienced an open fracture of his radius when he fell from a ladder while cleaning his house. Surgical reduction took place and the patient's forearm was put in a cast. Since then, the patient has experienced worsening pain in his arm. The patient has a past medical history of hypertension and asthma. His current medications include albuterol, fluticasone, loratadine, and lisinopril. His temperature is 99.5°F (37.5°C), blood pressure is 150/95 mmHg, pulse is 90/min, respirations are 19/min, and oxygen saturation is 99% on room air. The patient's cast is removed. On physical exam, the patient's left arm is tender to palpation. Passive motion of the patient's wrist and fingers elicits severe pain. The patient's left radial and ulnar pulse are both palpable and regular. The forearm is soft and does not demonstrate any bruising but is tender to palpation. Which of the following is the next best step in management?
- A. Replace the cast with a sling
- B. Measurement of compartment pressure (Correct Answer)
- C. Ibuprofen and reassurance
- D. Emergency fasciotomy
- E. Radiography
Post-mastectomy complications Explanation: ***Measurement of compartment pressure***
- The patient exhibits classic signs of **compartment syndrome**, including severe pain out of proportion to injury, pain with passive stretching, and a history of trauma followed by casting. Measuring compartment pressure is crucial for diagnosis despite palpable pulses.
- Early measurement of compartment pressures can confirm the diagnosis and guide the decision for an **emergency fasciotomy** to prevent irreversible tissue damage.
*Replace the cast with a sling*
- This action would likely worsen the patient's condition by delaying the diagnosis and treatment of potential **compartment syndrome**.
- A sling does not address the underlying issue of increased pressure within the muscle compartments.
*Ibuprofen and reassurance*
- Administering **Ibuprofen (NSAID)** might mask the pain but will not resolve the increased pressure within the compartment, which is a surgical emergency.
- Reassurance without proper assessment of compartment syndrome could lead to irreversible muscle and nerve damage.
*Emergency fasciotomy*
- While a fasciotomy is the definitive treatment for confirmed compartment syndrome, it should only be performed **after compartment pressures have been measured** and the diagnosis confirmed, unless the clinical suspicion is extremely high and pressures cannot be obtained.
- Performing a fasciotomy without objective confirmation is generally not the immediate next step, as it is an invasive procedure with its own risks.
*Radiography*
- **Radiography** would be useful to assess the healing of the fracture or rule out new fractures, but it will not provide information about the soft tissue pressure changes characteristic of compartment syndrome.
- The patient's symptoms are more indicative of a circulatory or soft tissue issue rather than a new bony problem.
Post-mastectomy complications US Medical PG Question 6: A 29-year-old G1P1 woman presents to her primary care physician with unilateral breast pain. She is currently breastfeeding her healthy 3-month-old baby boy. She has been breastfeeding since her child's birth without any problems. However, 3 days prior to presentation, she developed left breast pain, purulent nipple discharge, and malaise. Her past medical history is notable for obesity and generalized anxiety disorder. She takes sertraline. She does not smoke or drink alcohol. Her temperature is 100.8°F (38.2°C), blood pressure is 128/78 mmHg, pulse is 91/min, and respirations are 17/min. On exam, she appears lethargic but is able to answer questions appropriately. Her right breast appears normal. Her left breast is tender to palpation, warm to the touch, and swollen relative to the right breast. There is a visible fissure in the left nipple that expresses minimal purulent discharge. Which of the following pathogens is the most likely cause of this patient's condition?
- A. Staphylococcus epidermidis
- B. Candida albicans
- C. Staphylococcus aureus (Correct Answer)
- D. Bacteroides fragilis
- E. Streptococcus pyogenes
Post-mastectomy complications Explanation: ***Staphylococcus aureus***
- The patient's unilateral breast pain, purulent nipple discharge, fever, and localized warmth along with a fissure strongly suggest **mastitis**, commonly caused by bacterial infection in breastfeeding women.
- **_Staphylococcus aureus_** is the most common pathogen responsible for infectious mastitis due to its prevalence on the skin and ability to enter through nipple fissures.
*Staphylococcus epidermidis*
- While **_Staphylococcus epidermidis_** is a common skin commensal, it is less frequently implicated alone in significant, symptomatic mastitis with purulent discharge and fever.
- It is more often associated with biofilm-related infections on medical devices or opportunistic infections in immunocompromised individuals.
*Candida albicans*
- **_Candida albicans_** can cause fungal mastitis, often presenting with burning pain in both breasts and nipples, radiating to the back or armpit, typically without purulent discharge or significant fever unless there's a secondary bacterial infection.
- The presence of **purulent discharge** and fever points away from a primary candidal infection in this case.
*Bacteroides fragilis*
- **_Bacteroides fragilis_** is an anaerobic bacterium, usually associated with infections of the abdominal cavity or female genital tract after surgery or trauma, and rarely causes primary breast infections.
- The clinical picture of acute infectious mastitis in a breastfeeding woman is not consistent with **_Bacteroides fragilis_** as a primary pathogen.
*Streptococcus pyogenes*
- **_Streptococcus pyogenes_** can cause skin infections like cellulitis, but it is a relatively rare cause of acute infectious mastitis compared to **_Staphylococcus aureus_**.
- While it can cause severe infections, **_S. aureus_** remains the predominant pathogen in this clinical scenario.
Post-mastectomy complications US Medical PG Question 7: A 24-year-old woman presents to her primary care physician for unilateral breast pain. The patient states that she has been breastfeeding her son but has been experiencing worsening pain recently. Her pain is severe enough that she is now struggling to breastfeed her son with her left breast. The patient's past medical history is notable for gestational diabetes which was controlled with diet and exercise. Her temperature is 101°F (38.3°C), blood pressure is 137/69 mmHg, pulse is 100/min, respirations are 13/min, and oxygen saturation is 97% on room air. Physical exam reveals an erythematous breast with a 3-cm tender and fluctuant mass of the left breast. Which of the following is the best next step in management?
- A. No intervention necessary
- B. Ultrasound and fine needle aspiration (Correct Answer)
- C. Incision and drainage
- D. Ice packs and breast pumping
- E. Vancomycin and discharge home
Post-mastectomy complications Explanation: ***Ultrasound and fine needle aspiration***
- The presence of a **tender**, **fluctuant breast mass** with accompanying **fever** in a breastfeeding woman is highly suggestive of a **breast abscess**.
- **Ultrasound-guided needle aspiration** is the **first-line treatment** for breast abscess according to current guidelines (ACOG, WHO).
- This approach is **less invasive** than incision and drainage, allows for better cosmetic outcomes, and enables easier continuation of breastfeeding.
- Aspiration can be **repeated if necessary**, and most abscesses (80-90%) resolve with aspiration plus antibiotics.
*Incision and drainage*
- While this was historically the standard treatment, it is now considered **second-line therapy** for breast abscesses.
- Reserved for cases where **needle aspiration fails**, or for **complex/multiloculated abscesses**.
- More invasive with greater tissue disruption and potentially more difficult breastfeeding recovery.
*No intervention necessary*
- The patient presents with clear signs of **infection** (fever, pain, erythema) and a **palpable abscess**, indicating urgent need for intervention.
- Ignoring these symptoms could lead to worsening infection, systemic sepsis, or more complex surgical intervention.
*Ice packs and breast pumping*
- **Ice packs** and **breast pumping** are supportive measures for managing **mastitis** or engorgement but will not resolve a formed **abscess**.
- These interventions would delay appropriate treatment and potentially worsen the infection.
*Vancomycin and discharge home*
- **Antibiotics** like vancomycin are crucial adjunctive therapy for breast abscesses, especially considering potential **MRSA involvement**.
- However, for a **fluctuant abscess**, antibiotics alone are insufficient without **drainage** (aspiration or incision); discharging without drainage is inappropriate.
Post-mastectomy complications US Medical PG Question 8: A 28-year-old male presents to his primary care physician with complaints of intermittent abdominal pain and alternating bouts of constipation and diarrhea. His medical chart is not significant for any past medical problems or prior surgeries. He is not prescribed any current medications. Which of the following questions would be the most useful next question in eliciting further history from this patient?
- A. "Does the diarrhea typically precede the constipation, or vice-versa?"
- B. "Is the diarrhea foul-smelling?"
- C. "Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life"
- D. "Are the symptoms worse in the morning or at night?"
- E. "Can you tell me more about the symptoms you have been experiencing?" (Correct Answer)
Post-mastectomy complications Explanation: ***Can you tell me more about the symptoms you have been experiencing?***
- This **open-ended question** encourages the patient to provide a **comprehensive narrative** of their symptoms, including details about onset, frequency, duration, alleviating/aggravating factors, and associated symptoms, which is crucial for diagnosis.
- In a patient presenting with vague, intermittent symptoms like alternating constipation and diarrhea, allowing them to elaborate freely can reveal important clues that might not be captured by more targeted questions.
*Does the diarrhea typically precede the constipation, or vice-versa?*
- While knowing the sequence of symptoms can be helpful in understanding the **pattern of bowel dysfunction**, it is a very specific question that might overlook other important aspects of the patient's experience.
- It prematurely narrows the focus without first obtaining a broad understanding of the patient's overall symptomatic picture.
*Is the diarrhea foul-smelling?*
- Foul-smelling diarrhea can indicate **malabsorption** or **bacterial overgrowth**, which are important to consider in some gastrointestinal conditions.
- However, this is a **specific symptom inquiry** that should follow a more general exploration of the patient's symptoms, as it may not be relevant if other crucial details are missed.
*Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life*
- Quantifying pain intensity is useful for assessing the **severity of discomfort** and monitoring changes over time.
- However, for a patient with intermittent rather than acute, severe pain, understanding the **character, location, and triggers** of the pain is often more diagnostically valuable than just a numerical rating initially.
*Are the symptoms worse in the morning or at night?*
- Diurnal variation can be relevant in certain conditions, such as inflammatory bowel diseases where nocturnal symptoms might be more concerning, or functional disorders whose symptoms might be stress-related.
- This is another **specific question** that should come after gathering a more complete initial picture of the patient's symptoms to ensure no key information is overlooked.
Post-mastectomy complications US Medical PG Question 9: Five days after undergoing right knee arthroplasty for osteoarthritis, a 68-year-old man has severe pain in his right knee preventing him from participating in physical therapy. On the third postoperative day when the dressing was changed, the surgical wound appeared to be intact, slightly swollen, and had a clear secretion. He has a history of diabetes, hyperlipidemia, and hypertension. Current medications include metformin, enalapril, and simvastatin. His temperature is 37.3°C (99.1°F), pulse is 94/min, and blood pressure is 130/88 mm Hg. His right knee is swollen, erythematous, and tender to palpation. There is pain on movement of the joint. The medial parapatellar skin incision appears superficially opened in its proximal and distal part with yellow-green discharge. There is blackening of the skin on both sides of the incision. Which of the following is the next best step in the management of this patient?
- A. Vacuum dressing
- B. Antiseptic dressing
- C. Nafcillin therapy
- D. Removal of prostheses
- E. Surgical debridement (Correct Answer)
Post-mastectomy complications Explanation: ***Surgical debridement***
- The patient presents with classic signs of **necrotizing fasciitis** or a severe wound infection: rapidly worsening pain, erythema, swelling, **yellow-green discharge**, and crucially, **blackening of the skin** (indicating tissue necrosis).
- Immediate **surgical debridement** is critical for source control, removal of necrotic tissue, and preventing further spread of infection, which can be life-threatening.
*Vacuum dressing*
- A vacuum-assisted closure (VAC) dressing is used for wound management after adequate debridement or for wounds without signs of aggressive infection to promote healing.
- Applying a VAC dressing to a wound with widespread necrosis and active infection, especially necrotizing fasciitis, without prior debridement would be ineffective and potentially harmful.
*Antiseptic dressing*
- While antiseptic dressings can help reduce bacterial load in some superficial wounds, they are entirely insufficient for deep-seated, rapidly spreading infections with tissue necrosis.
- This approach fails to address the underlying necrotic tissue and the extent of the infection, leading to rapid deterioration.
*Nafcillin therapy*
- **Antibiotic therapy** is essential for treating severe infections; however, it must be combined with source control, especially when necrosis is present.
- Giving antibiotics alone without **surgical debridement** in cases of necrotizing fasciitis is inadequate and will not prevent progression of the infection or improve patient outcomes.
*Removal of prostheses*
- While **prosthesis removal** may be necessary in some cases of established periprosthetic joint infection, it is a definitive and often late measure.
- The immediate priority in a rapidly progressing, necrotic wound infection is **surgical debridement** to remove devitalized tissue and control the local infection, prior to considering implant removal unless the infection is directly on the implant.
Post-mastectomy complications US Medical PG Question 10: A 25-year-old man presents with pain and a limited range of motion in his right shoulder. He is a collegiate baseball player and says he has not been playing for approx. 1 week because his shoulder hurts when he throws. He also noticed trouble raising his arm over his head. He describes the pain as moderate, dull, and aching in character and worse when he moves his arm above his shoulder or when he lays in bed on his side. He denies any recent acute trauma to the shoulder or other joint pain. The medical history is significant for asthma, which is managed medically. The current medications include albuterol inhaled and fluticasone. He reports a 5-year history of chewing tobacco but denies smoking, alcohol, or drug use. The temperature is 37.0°C (98.6°F); blood pressure is 110/85 mm Hg; pulse is 97/min; respiratory rate is 15/min, and oxygen saturation is 99% on room air. The physical examination is significant for tenderness to palpation on the anterolateral aspect of the right shoulder. The active range of motion on abduction of the right shoulder is decreased. The passive range of motion is intact. No swelling, warmth, or erythema is noted. The sensation is intact. The deep tendon reflexes are 2+ bilaterally. The peripheral pulses are 2+. The laboratory results are all within normal limits. A plain radiograph of the right shoulder shows no evidence of fracture or bone deformities. An MRI of the right shoulder shows increased T1 and T2 signals in the rotator cuff tendon. Which of the following is the best initial course of treatment for this patient?
- A. No further treatment is needed
- B. Acromioplasty
- C. Intra-articular corticosteroid injection
- D. NSAIDs and conservative measures (Correct Answer)
- E. Conservative measures (rest and ice)
Post-mastectomy complications Explanation: ***NSAIDs and conservative measures***
- The patient presents with symptoms and MRI findings consistent with **rotator cuff tendinitis**, common in overhead athletes. Initial treatment should focus on **reducing inflammation** and pain, and promoting healing.
- **NSAIDs** combined with conservative measures like **rest from inciting activities** and **ice application** are the mainstay of initial treatment for tendinitis, aiming to alleviate pain and improve function.
*No further treatment is needed*
- This option is incorrect because the patient is experiencing significant pain, limitation in his sport, and MRI findings of **tendinitis**, which warrants intervention.
- Doing nothing would likely lead to worsening symptoms and potentially chronic issues, especially given his athletic demands.
*Acromioplasty*
- **Acromioplasty** is a surgical procedure typically reserved for cases of **subacromial impingement syndrome** that have failed extensive conservative management, or for larger, more symptomatic tears.
- The patient's presentation suggests **tendinitis** without clear evidence of chronic impingement or a full-thickness tear requiring immediate surgical intervention.
*Intra-articular corticosteroid injection*
- **Corticosteroid injections** can provide temporary pain relief but are generally reserved for cases that have failed conservative therapy with oral NSAIDs and physical therapy.
- They also carry risks like **tendon weakening** and potential for rupture, which is particularly concerning in an athlete with tendinitis.
*Conservative measures (rest and ice)*
- While **rest and ice** are crucial components of conservative management, this option is incomplete as it omits the important role of **NSAIDs** in managing the inflammatory component of tendinitis.
- Simply resting and icing might not be sufficient for adequate pain control and inflammation reduction in an active individual with this degree of symptoms.
More Post-mastectomy complications US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.