Nipple discharge evaluation US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Nipple discharge evaluation. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Nipple discharge evaluation US Medical PG Question 1: A 33-year-old woman presents to her primary care physician for non-bloody nipple discharge. She states that it has been going on for the past month and that it sometimes soils her shirt. The patient drinks 2 to 3 alcoholic beverages per day and smokes 1 pack of cigarettes per day. She is currently seeking mental health treatment with an outpatient psychiatrist after a recent hospitalization for auditory hallucinations. Her psychiatrist prescribed her a medication that she can not recall. Otherwise, she complains of headaches that occur frequently. Her temperature is 98.6°F (37.0°C), blood pressure is 137/68 mmHg, pulse is 70/min, respirations are 13/min, and oxygen saturation is 98% on room air. Physical exam is notable for bilateral galactorrhea that can be expressed with palpation. Which of the following is the best next step in management?
- A. Ultrasound and biopsy
- B. Mammography
- C. Serum prolactin level (Correct Answer)
- D. CT scan of the head
- E. Discontinuation of current psychiatric medications
Nipple discharge evaluation Explanation: ***Serum prolactin level***
- The patient presents with **bilateral, non-bloody nipple discharge (galactorrhea)**, which is strongly suggestive of **hyperprolactinemia**. Given her psychiatric history and recent change in medication, a drug-induced cause (e.g., antipsychotics) is highly probable, making a serum prolactin level the most appropriate initial diagnostic step.
- Elevated prolactin can be caused by various factors, including **prolactinomas**, **hypothyroidism**, and **medications** (especially antipsychotics that block dopamine D2 receptors), and measuring this level helps differentiate between these causes and guides further management.
*Ultrasound and biopsy*
- This approach is typically indicated for suspicious **breast masses** or **unilateral, bloody nipple discharge** to rule out malignancy.
- The patient's symptoms are characteristic of galactorrhea, not a suspicious breast lesion requiring imaging and biopsy at this stage.
*Mammography*
- Mammography is primarily used for **breast cancer screening** or to investigate suspicious **breast lumps** or **bloody nipple discharge** in older women.
- Given the patient's age (33) and the bilateral, non-bloody nature of the discharge, mammography is not the initial investigation of choice for galactorrhea.
*CT scan of the head*
- A CT scan of the head (or MRI) would be indicated if the **serum prolactin level is significantly elevated** and suggests a **pituitary adenoma** (prolactinoma), or if other neurological symptoms point to an intracranial pathology.
- It is premature to order head imaging before confirming hyperprolactinemia, as the cause could be medication-related and not require imaging.
*Discontinuation of current psychiatric medications*
- While psychiatric medications, particularly **antipsychotics**, can cause hyperprolactinemia, discontinuing them should not be the *first* step without confirming the diagnosis and ruling out other serious causes.
- Abrupt discontinuation of psychiatric medication can lead to relapse of mental health symptoms and is usually done under strict medical supervision after a clear diagnosis.
Nipple discharge evaluation US Medical PG Question 2: A 37-year-old woman presents to her primary care physician for bilateral nipple discharge. The patient states that she has observed a milky discharge coming from her nipples for the past month. On review of systems, the patient states that she has felt fatigued lately and has experienced decreased libido. She also endorses headaches that typically resolve by the middle of the day and a 5 pound weight gain this past month. The patient has a past medical history of obesity, schizophrenia, and constipation. Her temperature is 99.5°F (37.5°C), blood pressure is 145/95 mmHg, pulse is 60/min, respirations are 15/min, and oxygen saturation is 98% on room air. On physical exam, you note an obese, fatigued-appearing woman. Dermatologic exam reveals fine, thin hair over her body. Cardiopulmonary exam is within normal limits. Neurological exam reveals cranial nerves II-XII as grossly intact. The patient exhibits 1+ sluggish reflexes. Which of the following is the most likely diagnosis?
- A. Dopamine blockade in the tuberoinfundibular pathway
- B. Protein-secreting CNS mass
- C. Normal pregnancy
- D. Viral infection of the thyroid gland
- E. Autoimmune destruction of the thyroid gland (Correct Answer)
Nipple discharge evaluation Explanation: ***Autoimmune destruction of the thyroid gland***
- The patient's symptoms of **fatigue**, **weight gain**, **constipation**, **bradycardia** (pulse 60/min), and **sluggish reflexes** are classic signs of **hypothyroidism**.
- **Nipple discharge** can occur due to secondary **hyperprolactinemia** caused by increased TRH (thyrotropin-releasing hormone) from the hypothalamus in an attempt to stimulate the underactive thyroid. **Autoimmune destruction** (e.g., Hashimoto's thyroiditis) is the most common cause of hypothyroidism.
*Dopamine blockade in the tuberoinfundibular pathway*
- This could lead to **hyperprolactinemia** and nipple discharge, especially if she is on **antipsychotic medications** for schizophrenia.
- However, it does not explain the other prominent symptoms of **hypothyroidism** such as fatigue, weight gain, constipation, and bradycardia.
*Protein-secreting CNS mass*
- A **prolactinoma** (a type of protein-secreting CNS mass) can cause **galactorrhea**, headaches, and decreased libido.
- However, it would not typically cause the systemic symptoms of **hypothyroidism** like constipation, weight gain, fatigue, and bradycardia.
*Normal pregnancy*
- **Pregnancy** can cause nipple discharge and fatigue, but vital signs indicate **bradycardia** (pulse of 60/min) rather than the typical tachycardia of pregnancy.
- There is no mention of missed periods or other classic signs of pregnancy; therefore, it is less likely given the full symptom constellation.
*Viral infection of the thyroid gland*
- A viral infection of the thyroid gland (e.g., **subacute thyroiditis**) can initially present with **hyperthyroidism** followed by a hypothyroid phase.
- However, the patient's symptoms are primarily hypothyroid from the onset, and the presentation does not suggest an acute inflammatory process typical of viral thyroiditis.
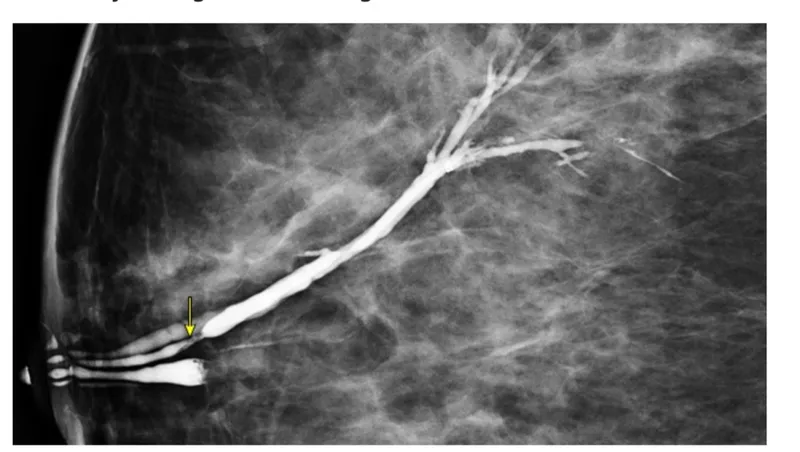
Nipple discharge evaluation US Medical PG Question 3: A 29-year-old nulligravid woman comes to the physician because of a 10-day history of small quantities of intermittent, blood-tinged discharge from her left nipple. There is no personal or family history of serious illness. She has smoked 1 pack of cigarettes daily for 5 years. Her last menstrual period was 12 days ago. She is sexually active and uses condoms inconsistently. Physical examination shows scant serosanguinous fluid expressible from the left nipple. There is no palpable breast mass or axillary lymphadenopathy. Examination shows no other abnormalities. Which of the following is the most appropriate next step in management?
- A. Image-guided core biopsy of the affected duct
- B. Subareolar ultrasound (Correct Answer)
- C. Nipple discharge cytology
- D. Reassurance
- E. Breast MRI
Nipple discharge evaluation Explanation: ***Subareolar ultrasound***
- This patient presents with **unilateral**, **spontaneous**, **single-duct bloody nipple discharge**, which is characteristic of an **intraductal papilloma** or early malignancy.
- A **subareolar ultrasound** is the most appropriate initial imaging step to evaluate the ductal system for a mass or obstruction, especially in a young woman with dense breasts where mammography may be less sensitive.
*Image-guided core biopsy of the affected duct*
- A biopsy would be considered if imaging (like ultrasound) reveals a suspicious lesion, but it is not the **initial diagnostic step**.
- **Image guidance** is necessary for biopsy of non-palpable lesions, but first, the lesion needs to be identified and characterized by imaging.
*Nipple discharge cytology*
- **Cytology of nipple discharge** has a **low sensitivity** for identifying malignancy and is generally not recommended as a primary diagnostic tool.
- It can be helpful in some cases, but imaging is usually preferred for initial evaluation of suspicious discharge.
*Reassurance*
- **Bloody nipple discharge**, even in small quantities, is a **concerning symptom** that requires further investigation to rule out malignancy and cannot simply be dismissed.
- While many cases are benign (e.g., intraductal papilloma), serious pathology must be excluded.
*Breast MRI*
- **Breast MRI** is a highly sensitive imaging modality but is typically reserved for **further evaluation** after initial mammography and ultrasound, especially in high-risk patients or for assessing the extent of known disease.
- It is **not the first-line imaging** for isolated bloody nipple discharge without other suspicious findings on initial assessment.
Nipple discharge evaluation US Medical PG Question 4: A 36-year-old woman comes to the gynecologist because of a 4-month history of irregular menstrual cycles. Menses occur at irregular 15 to 45-day intervals and last 1–2 days with minimal flow. She also reports a milk-like discharge from her nipples for 3 months, as well as a history of fatigue and muscle and joint pain. She does not have abdominal pain, fever, or headache. She has recently gained 2.5 kg (5.5 lb) of weight. She was diagnosed with schizophrenia and started on aripiprazole by a psychiatrist 8 months ago. She has hypothyroidism but has not been taking levothyroxine for 6 months. She does not smoke or consume alcohol. She appears healthy and anxious. Her vital signs are within normal limits. Pelvic examination shows vaginal atrophy. Visual field and skin examination are normal. Laboratory studies show:
Hemoglobin 12.7 g/dL
Serum
Glucose 88 mg/dL
Creatinine 0.7 mg/dL
Thyroid-stimulating hormone 16.3 μU/mL
Cortisol (8AM) 18 μg/dL
Prolactin 88 ng/mL
Urinalysis is normal. An x-ray of the chest and ultrasound of the pelvis show no abnormalities. Which of the following is the most likely explanation for the nipple discharge in this patient?
- A. Prolactinoma
- B. Hypothyroidism (Correct Answer)
- C. Thyrotropic pituitary adenoma
- D. Cushing disease
- E. Ectopic prolactin production
Nipple discharge evaluation Explanation: ***Hypothyroidism***
- The patient has a significantly elevated **TSH (16.3 μU/mL)** and a history of non-compliance with **levothyroxine** for 6 months, strongly indicating uncontrolled hypothyroidism.
- **Hypothyroidism** can lead to **increased TRH** (thyrotropin-releasing hormone) from the hypothalamus, which stimulates not only TSH but also **prolactin** release, causing galactorrhea.
- Note: **Aripiprazole** is a partial dopamine agonist and typically does **not** cause hyperprolactinemia (unlike typical antipsychotics or risperidone), making hypothyroidism the primary driver here.
*Prolactinoma*
- While the patient has **hyperprolactinemia (prolactin 88 ng/mL)** and galactorrhea, a prolactinoma usually presents with prolactin levels **significantly higher** (often >200 ng/mL, or >100 ng/mL in microadenomas) than observed here.
- The primary driver for the hyperprolactinemia in this case is more likely the **uncorrected hypothyroidism**, which can also cause moderate elevation of prolactin.
*Thyrotropic pituitary adenoma*
- A **thyrotropic pituitary adenoma** (TSH-secreting adenoma) would cause elevated TSH accompanied by **elevated thyroid hormone levels** (hyperthyroidism), which contradicts this patient's clinical picture of hypothyroidism.
- This patient exhibits **hypothyroidism** due to non-adherence to medication, not hyperthyroidism induced by a TSH-secreting tumor.
*Cushing disease*
- **Cushing disease** is characterized by elevated **cortisol** due to an ACTH-secreting pituitary adenoma, leading to symptoms like central obesity, moon facies, and striae; these are not reported.
- While some forms of Cushing syndrome can cause menstrual irregularities, it does not typically cause **galactorrhea** or significantly elevated prolactin levels as seen in this patient.
*Ectopic prolactin production*
- **Ectopic prolactin production** is a rare cause of hyperprolactinemia, typically associated with large tumors, most commonly **renal cell carcinoma** or other neuroendocrine tumors (e.g., lung carcinoid).
- Given the patient's severe **hypothyroidism**, it is a far more common and likely explanation for her hyperprolactinemia and galactorrhea than ectopic production.
Nipple discharge evaluation US Medical PG Question 5: A 47-year-old woman comes to the physician for a mass in her left breast she noticed 2 days ago during breast self-examination. She has hypothyroidism treated with levothyroxine. There is no family history of breast cancer. Examination shows large, moderately ptotic breasts. The mass in her left breast is small (approximately 1 cm x 0.5 cm), firm, mobile, and painless. It is located 4 cm from her nipple-areolar complex at the 7 o'clock position. There are no changes in the skin or nipple, and there is no palpable axillary adenopathy. No masses are palpable in her right breast. A urine pregnancy test is negative. Mammogram showed a soft tissue mass with poorly defined margins. Core needle biopsy confirms a low-grade infiltrating ductal carcinoma. The pathological specimen is positive for estrogen receptors and negative for progesterone and human epidermal growth factor receptor 2 (HER2) receptors. Staging shows no distant metastatic disease. Which of the following is the most appropriate next step in management?
- A. Lumpectomy with sentinel lymph node biopsy followed by hormone therapy
- B. Nipple-sparing mastectomy with axillary lymph node dissection followed by hormone therapy
- C. Nipple-sparing mastectomy with axillary lymph node dissection, followed by radiation and hormone therapy
- D. Radical mastectomy followed by hormone therapy
- E. Lumpectomy with sentinel lymph node biopsy, followed by radiation and hormone therapy (Correct Answer)
Nipple discharge evaluation Explanation: **Lumpectomy with sentinel lymph node biopsy, followed by radiation and hormone therapy**
- The patient has **early-stage (T1N0M0) estrogen receptor (ER)-positive, HER2-negative invasive ductal carcinoma** suitable for **breast-conserving surgery (lumpectomy)**.
- **Lumpectomy** must be followed by **radiation therapy** to the remaining breast tissue to reduce the risk of local recurrence, and **endocrine therapy** (due to ER positivity) is indicated to reduce systemic recurrence risk.
- **Sentinel lymph node biopsy** is performed to stage the axilla; if positive, an axillary lymph node dissection may be indicated. However, in this case, the mass is small, and there is no palpable axillary adenopathy, making sentinel lymph node biopsy the appropriate initial step.
*Lumpectomy with sentinel lymph node biopsy followed by hormone therapy*
- While **lumpectomy with sentinel lymph node biopsy** and **hormone therapy** are part of the appropriate management, **radiation therapy** to the conserved breast is a critical component that is missing from this option.
- Omitting **radiation therapy** after lumpectomy for invasive breast cancer significantly increases the risk of local recurrence.
*Nipple-sparing mastectomy with axillary lymph node dissection followed by hormone therapy*
- A **nipple-sparing mastectomy** is a more aggressive surgical approach than typically required for a **small, early-stage tumor** like this, which is amenable to breast-conserving surgery.
- **Axillary lymph node dissection** is usually reserved for cases with clinically positive lymph nodes or a positive sentinel lymph node biopsy, not as an initial step when there is no palpable axillary adenopathy.
*Nipple-sparing mastectomy with axillary lymph node dissection, followed by radiation and hormone therapy*
- This option involves an **unnecessarily extensive surgical procedure (nipple-sparing mastectomy with axillary lymph node dissection)** for a **small (1cm x 0.5cm) early-stage tumor** that can be managed with breast-conserving therapy.
- While radiation and hormone therapy are relevant, the initial surgical choice is too aggressive given the clinical presentation.
*Radical mastectomy followed by hormone therapy*
- **Radical mastectomy** (which includes removal of the breast, underlying chest muscle, and axillary lymph nodes) is rarely performed today due to its significant morbidity and is not indicated for this **early-stage tumor**.
- **Modified radical mastectomy**, which removes the breast and axillary lymph nodes while preserving the chest muscle, is typically only considered if breast-conserving surgery is not feasible or desired, and **hormone therapy** would be indicated, but **radiation** may also be needed depending on other factors.
Nipple discharge evaluation US Medical PG Question 6: A 50-year-old obese woman presents for a follow-up appointment regarding microcalcifications found in her left breast on a recent screening mammogram. The patient denies any recent associated symptoms. The past medical history is significant for polycystic ovarian syndrome (PCOS), for which she takes metformin. Her menarche occurred at age 11, and the patient still has regular menstrual cycles. The family history is significant for breast cancer in her mother at the age of 72. The review of systems is notable for a 6.8 kg (15 lb) weight loss in the past 2 months. The vital signs include: temperature 37.0°C (98.6°F), blood pressure 130/70 mm Hg, pulse 82/min, respiratory rate 17/min, and oxygen saturation 98% on room air. On physical examination, the patient is alert and cooperative. The breast examination reveals no palpable masses, lymphadenopathy, or evidence of skin retraction. A biopsy of the left breast is performed, and histologic examination demonstrates evidence of non-invasive malignancy. Which of the following is the most appropriate definitive treatment for this patient?
- A. Tamoxifen
- B. Observation with bilateral mammograms every 6 months
- C. Lumpectomy (Correct Answer)
- D. Radiotherapy
- E. Bilateral mastectomy
Nipple discharge evaluation Explanation: ***Lumpectomy***
- This patient has **non-invasive malignancy**, likely **ductal carcinoma in situ (DCIS)**, identified through microcalcifications and confirmed by excisional biopsy. For DCIS without gross invasion, the primary treatment is **surgical excision**, often a lumpectomy.
- A lumpectomy, also known as **breast-conserving surgery**, aims to remove the cancerous tissue with a margin of healthy tissue while preserving the rest of the breast.
*Tamoxifen*
- **Tamoxifen** is an **estrogen receptor modulator** used as **adjuvant therapy** for hormone-receptor-positive breast cancer, primarily after surgical removal of the tumor. It is not a primary treatment for removing the malignancy itself.
- While it might be considered after surgery depending on receptor status, it does not address the need for initial excision of the non-invasive malignancy.
*Observation with bilateral mammograms every 6 months*
- **Observation** is insufficient for confirmed non-invasive malignancy, which carries a risk of progression if untreated. **Active intervention** is required once malignancy is histologically confirmed.
- This approach might be considered for high-risk lesions or atypical hyperplasia, but not for confirmed carcinoma in situ.
*Radiotherapy*
- **Radiotherapy** is often used as **adjuvant therapy** after lumpectomy for DCIS to reduce the risk of local recurrence. It is not a standalone primary treatment for removing the initial non-invasive malignancy.
- The first step is always surgical removal of the cancerous tissue.
*Bilateral mastectomy*
- **Bilateral mastectomy** is a more aggressive surgical intervention, typically reserved for **invasive breast cancer**, widespread DCIS, or cases with very high genetic risk (e.g., BRCA mutations).
- For localized non-invasive malignancy identified through microcalcifications, a lumpectomy is generally the **most appropriate and less invasive initial surgical approach**.
Nipple discharge evaluation US Medical PG Question 7: A 58-year-old woman underwent mastectomy for multicentric DCIS. Final pathology shows high-grade DCIS with comedonecrosis, margins negative by 3 mm, no invasion identified in 40 tissue blocks examined. Sentinel lymph node biopsy shows isolated tumor cells (0.1 mm cluster) positive for cytokeratin. The medical oncologist requests input on systemic therapy. Evaluate the significance of the nodal finding and recommendations.
- A. Upstage to invasive cancer, recommend chemotherapy and endocrine therapy
- B. Perform completion axillary dissection to assess additional nodal involvement
- C. Consider isolated tumor cells clinically insignificant, node-negative staging, endocrine therapy only if ER-positive (Correct Answer)
- D. Recommend axillary radiation and systemic chemotherapy
- E. Repeat pathology review to identify occult invasion
Nipple discharge evaluation Explanation: ***Consider isolated tumor cells clinically insignificant, node-negative staging, endocrine therapy only if ER-positive***
- Per AJCC guidelines, **isolated tumor cells (ITCs)** (clusters ≤ 0.2 mm or < 200 cells) are staged as **pN0(i+)**, which is considered node-negative disease.
- In the setting of pure **DCIS**, ITCs do not warrant staging as invasive cancer nor do they justify **systemic chemotherapy**; management depends solely on the tumor's **ER-status** for endocrine therapy.
*Upstage to invasive cancer, recommend chemotherapy and endocrine therapy*
- Staging cannot be upgraded to invasive cancer unless a **pathological focus of invasion** is identified in the breast tissue (T category).
- **Chemotherapy** is never indicated for pure DCIS, regardless of high-grade features or the presence of ITCs in the lymph nodes.
*Perform completion axillary dissection to assess additional nodal involvement*
- **Completion axillary lymph node dissection (ALND)** is not indicated for ITCs, as they do not carry the same prognostic weight as macro-metastases.
- In pure DCIS, the presence of ITCs is often attributed to **mechanical transport** of cells during biopsy rather than true metastatic potential.
*Recommend axillary radiation and systemic chemotherapy*
- **Axillary radiation** is reserved for patients with significant nodal burden and is inappropriate for **pN0(i+)** status.
- Because DCIS is a non-invasive, **pre-cancerous lesion** contained within the basement membrane, systemic chemotherapy provides no benefit and unnecessary toxicity.
*Repeat pathology review to identify occult invasion*
- While high-grade DCIS increases the risk of occult invasion, the examination of **40 tissue blocks** is considered exhaustive and standard for ruling out invasion.
- Persistent searching for micro-invasion after comprehensive sampling is unlikely to change the clinical management dictated by the **pN0(i+)** finding.
Nipple discharge evaluation US Medical PG Question 8: A 36-year-old woman with BRCA2 mutation and strong family history of breast and ovarian cancer desires risk-reducing surgery. She has 2 young children and plans to have one more child in 2 years. She asks about timing of risk-reducing mastectomy and oophorectomy. Her mother died of ovarian cancer at age 45, and sister diagnosed with breast cancer at age 38. Evaluate the optimal counseling regarding surgical timing.
- A. Perform both risk-reducing mastectomy and oophorectomy immediately
- B. Defer both surgeries until after childbearing is complete
- C. Risk-reducing mastectomy now, oophorectomy after completion of childbearing
- D. Risk-reducing oophorectomy now, mastectomy after completion of childbearing (Correct Answer)
- E. Annual screening only until age 40, then reconsider surgery
Nipple discharge evaluation Explanation: ***Risk-reducing oophorectomy now, mastectomy after completion of childbearing***
- **BRCA2** carriers are recommended to undergo **risk-reducing salpingo-oophorectomy (RRSO)** by age 40-45 as ovarian cancer has a high mortality rate and lacks effective **screening methods**.
- High-risk breast screening with **MRI** and **mammography** can safely defer **bilateral mastectomy** until the patient completes childbearing and breastfeeding, balancing life-saving prevention with reproductive goals.
*Perform both risk-reducing mastectomy and oophorectomy immediately*
- Performing an **immediate oophorectomy** would cause surgical menopause and permanent **infertility**, preventing the patient's plan to have one more child in 2 years.
- While medically aggressive, this approach disregards the patient's **reproductive autonomy** and psychosocial needs without providing a curative benefit that outweighs the loss of fertility at this stage.
*Defer both surgeries until after childbearing is complete*
- Deferring all surgery increases the window of risk for **ovarian cancer**, which is difficult to detect early and has a significantly poor prognosis compared to breast cancer.
- This approach ignores the strong **family history** (mother died at 45) which suggests a high risk for early-onset malignancy in this specific pedigree.
*Risk-reducing mastectomy now, oophorectomy after completion of childbearing*
- Undergoing **bilateral mastectomy** now would prevent the patient from **breastfeeding** her future child, which may be a significant personal goal.
- Prioritizing mastectomy over oophorectomy is often less critical because **breast surveillance** (MRI/Mammogram) is more reliable than current **ovarian cancer screening** (CA-125/Ultrasound).
*Annual screening only until age 40, then reconsider surgery*
- Relying solely on **screening** is risky for **BRCA2** patients, especially for ovarian cancer where screening has not been proven to reduce mortality or detect early-stage disease reliably.
- Given the family history of a death at age 45, waiting until age 40 to even consider surgery may delay intervention past the point of **clinical benefit** for cancer prevention.
Nipple discharge evaluation US Medical PG Question 9: A 42-year-old premenopausal woman with newly diagnosed 2.5 cm triple-negative breast cancer and 3 positive axillary lymph nodes completed neoadjuvant chemotherapy. Post-treatment MRI shows residual 1 cm mass in breast and 1 abnormal lymph node. She desires breast conservation. The tumor board must evaluate the surgical plan considering residual disease burden and emerging data on post-neoadjuvant therapy.
- A. Mastectomy with reconstruction, no additional systemic therapy
- B. Additional neoadjuvant chemotherapy until complete response
- C. Lumpectomy, sentinel node biopsy only, regional nodal radiation
- D. Lumpectomy, completion axillary dissection, standard adjuvant radiation
- E. Lumpectomy, axillary dissection, and consider pembrolizumab based on residual disease (Correct Answer)
Nipple discharge evaluation Explanation: ***Lumpectomy, axillary dissection, and consider pembrolizumab based on residual disease***
- In high-risk **triple-negative breast cancer (TNBC)** with residual disease after neoadjuvant chemotherapy, the **KEYNOTE-522** trial supports continuing adjuvant **pembrolizumab** to improve event-free survival.
- Since the patient remains **node-positive** after neoadjuvant therapy, a **completion axillary lymph node dissection (ALND)** is indicated rather than sentinel node biopsy alone.
*Mastectomy with reconstruction, no additional systemic therapy*
- **Breast conservation** (lumpectomy) is an appropriate option if negative margins can be achieved, and the patient specifically desires it.
- Patients with **residual disease** after neoadjuvant therapy for TNBC require further systemic treatment, such as **capecitabine** or pembrolizumab, to reduce recurrence risk.
*Additional neoadjuvant chemotherapy until complete response*
- Chemotherapy is not typically continued indefinitely until a **pathologic complete response (pCR)** is achieved; surgical resection is the necessary next step once the standard regimen is completed.
- Delaying surgery for additional rounds of the same chemotherapy in a patient with **residual disease** may allow for further tumor progression or increase toxicity.
*Lumpectomy, sentinel node biopsy only, regional nodal radiation*
- **Sentinel node biopsy** alone is insufficient here because the patient has persistent, biopsy-proven or radiologically **abnormal lymph nodes** after neoadjuvant chemotherapy.
- Current standards for patients who remain **node-positive** after chemotherapy typically require a formal **axillary lymph node dissection** to control regional disease.
*Lumpectomy, completion axillary dissection, standard adjuvant radiation*
- While this address the surgical components, it fails to include the critical **adjuvant systemic therapy** required for residual TNBC.
- Omitting post-neoadjuvant systemic treatment ignores data from the **CREATE-X** or **KEYNOTE-522** trials which show survival benefits for patients with residual TNBC.
Nipple discharge evaluation US Medical PG Question 10: A 70-year-old woman with multiple comorbidities (COPD, CHF, DM) presents with a 3 cm palpable breast mass. Core biopsy shows invasive ductal carcinoma, ER-positive (95%), PR-positive (90%), HER2-negative, grade 1, Ki-67 5%. Staging shows no metastases. Her surgical risk is assessed as high (ASA class 4). Analyze the optimal treatment approach.
- A. Primary endocrine therapy with aromatase inhibitor alone (Correct Answer)
- B. Neoadjuvant chemotherapy followed by surgery
- C. Lumpectomy under local anesthesia with sedation
- D. Modified radical mastectomy under general anesthesia
- E. Observation with serial imaging
Nipple discharge evaluation Explanation: ***Primary endocrine therapy with aromatase inhibitor alone***
- For elderly patients with **multiple comorbidities** and **high surgical risk (ASA class 4)**, the risks of invasive surgery may outweigh the benefits of local control.
- The tumor's biology (**highly ER/PR positive**, **low Ki-67**, and **low grade**) indicates it is extremely responsive to **endocrine therapy**, making it a viable primary treatment to manage disease progression without surgery.
*Neoadjuvant chemotherapy followed by surgery*
- **Chemotherapy** is generally poorly tolerated in patients with **COPD, CHF, and DM**, and is not indicated for low-grade, highly hormone-responsive HER2-negative tumors.
- This approach still necessitates **surgery**, which has been determined to be high risk for this patient.
*Lumpectomy under local anesthesia with sedation*
- While less invasive than general anesthesia, even **minor surgery** and sedation carry significant risks for an **ASA 4** patient with unstable medical conditions.
- **Surgical margins** and follow-up radiation (usually required after lumpectomy) would impose additional burdens that may not improve survival in this clinical context.
*Modified radical mastectomy under general anesthesia*
- **General anesthesia** carries an unacceptably high risk of perioperative mortality and complications in a patient with **severe COPD and CHF**.
- **Modified radical mastectomy** is unnecessarily aggressive for a 3 cm, low-grade tumor that can be managed with less morbid systemic options.
*Observation with serial imaging*
- **Observation alone** allows for uncontrolled local growth of the **invasive ductal carcinoma**, which could eventually lead to skin ulceration or pain.
- Unlike simple observation, **primary endocrine therapy** actively treats the cancer and provides **disease control** with minimal toxicity compared to surgical intervention.
More Nipple discharge evaluation US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.