Male breast cancer US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Male breast cancer. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Male breast cancer US Medical PG Question 1: A 42-year-old woman is seen by her primary care physician for her annual checkup. She has no current concerns and says that she has been healthy over the last year except for a bout of the flu in December. She has no significant past medical history and is not currently taking any medications. She has smoked 1 pack per day since she was 21 and drinks socially with her friends. Her family history is significant for prostate cancer in her dad when he was 51 years of age and ovarian cancer in her paternal aunt when she was 41 years of age. Physical exam reveals a firm, immobile, painless lump in the upper outer quadrant of her left breast as well as 2 smaller nodules in the lower quadrants of her right breast. Biopsy of these lesions shows small, atypical, glandular, duct-like cells with stellate morphology. Which of the following pathways is most likely abnormal in this patient?
- A. Nucleotide excision repair
- B. Base excision repair
- C. Non-homologous end joining
- D. Mismatch repair
- E. Homologous recombination (Correct Answer)
Male breast cancer Explanation: ***Homologous recombination***
- The patient's presentation with **multiple, bilateral breast lumps** and a strong family history of **early-onset breast, ovarian, and prostate cancers** suggests a hereditary cancer syndrome, most notably related to **BRCA1/2 mutations**.
- **BRCA1 and BRCA2 genes** are crucial for **homologous recombination**, a major pathway for repairing **double-strand DNA breaks**. Defects in this pathway lead to genomic instability and increased cancer risk.
*Nucleotide excision repair*
- This pathway primarily repairs bulky DNA adducts, such as **pyrimidine dimers** caused by UV radiation, and maintains DNA integrity by excising the damaged segment.
- Deficiencies in nucleotide excision repair are associated with diseases like **xeroderma pigmentosum**, which is characterized by extreme sensitivity to sunlight and skin cancers, not the pattern seen in this patient.
*Base excision repair*
- **Base excision repair** is responsible for repairing small, non-bulky DNA lesions, such as **oxidized or deaminated bases**, by removing the damaged base and replacing it.
- While essential for DNA integrity, its malfunction is not typically linked to the **hereditary breast and ovarian cancer syndrome** suggested by the patient's family history and clinical presentation.
*Non-homologous end joining*
- **Non-homologous end joining (NHEJ)** is an error-prone pathway for repairing **double-strand DNA breaks** by directly ligating the broken ends without a homologous template.
- While critical for DNA repair, defects in NHEJ are not the primary cause of hereditary breast and ovarian cancer, which is more specifically linked to the **BRCA1/2 genes** and the homologous recombination pathway.
*Mismatch repair*
- **Mismatch repair (MMR)** corrects errors that occur during DNA replication, such as mismatched bases or small insertions/deletions.
- Deficiencies in MMR lead to **microsatellite instability** and are characteristic of **Lynch syndrome (hereditary nonpolyposis colorectal cancer)**, which primarily increases the risk of colorectal, endometrial, and other specific cancers, but not the pattern of breast, ovarian, and prostate cancers seen here.
Male breast cancer US Medical PG Question 2: A previously healthy 13-year-old boy is brought to the physician because of a lump beneath his right nipple that he discovered 1 week ago while showering. He has allergic rhinitis treated with cetirizine. He is at the 65th percentile for height and 80th percentile for weight. Examination shows a mildly tender, firm, 2-cm subareolar mass in the right breast; there are no nipple or skin changes. The left breast shows no abnormalities. Sexual development is Tanner stage 3. Which of the following is the most likely explanation for this patient's breast lump?
- A. Adverse effect of medication
- B. Invasive ductal carcinoma
- C. Normal development (Correct Answer)
- D. Leydig cell tumor
- E. Hyperprolactinemia
Male breast cancer Explanation: **Normal development**
- The patient's age (13 years old) and Tanner stage 3 sexual development are consistent with **pubertal gynecomastia**, which is a common and normal finding in adolescent males.
- The presentation of a **mildly tender, firm, subareolar mass** in one or both breasts is characteristic of physiological gynecomastia during puberty.
*Adverse effect of medication*
- While certain medications can cause gynecomastia, **cetirizine (an antihistamine)** is not typically associated with this side effect.
- The clinical presentation aligns more strongly with a **physiological process** given the patient's age and pubertal stage.
*Invasive ductal carcinoma*
- Breast cancer in adolescent males is **extremely rare** and usually presents with hard, irregular, fixed masses, often with skin dimpling or nipple discharge.
- The described mass is **mildly tender and subareolar**, which is more typical of benign gynecomastia.
*Leydig cell tumor*
- Leydig cell tumors can cause gynecomastia due to **increased estrogen production** or increased androgen-to-estrogen conversion.
- However, such tumors would typically present with other signs of **precocious puberty** or testicular abnormalities, which are not mentioned here.
*Hyperprolactinemia*
- High prolactin levels can cause gynecomastia, but they are also associated with **galactorrhea** (nipple discharge), which is not described in this patient.
- **Other causes of gynecomastia** are more common in adolescents than hyperprolactinemia.
Male breast cancer US Medical PG Question 3: A 35-year-old woman is presenting for a general wellness checkup. She is generally healthy and has no complaints. The patient does not smoke, drinks 1 alcoholic drink per day, and exercises 1 day per week. She recently had silicone breast implants placed 1 month ago. Her family history is notable for a heart attack in her mother and father at the age of 71 and 55 respectively. Her father had colon cancer at the age of 70. Her temperature is 99.0°F (37.2°C), blood pressure is 121/81 mmHg, pulse is 77/min, respirations are 14/min, and oxygen saturation is 98% on room air. Physical exam is unremarkable. Which of the following is the most appropriate initial step in management?
- A. Alcohol cessation
- B. Colonoscopy at age 60
- C. Mammography at age 50
- D. Colonoscopy at age 40 (Correct Answer)
- E. Mammography now
Male breast cancer Explanation: ***Colonoscopy at age 40***
- This patient has a **first-degree relative (father) diagnosed with colorectal cancer at age 70**, which increases her risk compared to the average population.
- Current **USPSTF and ACS guidelines** recommend that individuals with a first-degree relative diagnosed with colorectal cancer at **age 60 or older** should begin screening at **age 40** (or 10 years before the age of diagnosis in the relative, whichever is earlier).
- Since her father was diagnosed at age 70, she should start screening at age 40 (which is 10 years earlier and also the recommended age for those with family history).
- At age 35, she does **not yet need** colonoscopy, but should plan for screening in 5 years.
*Colonoscopy now*
- This is **too early** based on current guidelines.
- Immediate colonoscopy at age 35 is not indicated in an asymptomatic patient whose father was diagnosed at age 70.
- Screening at age 40 provides adequate time for early detection while avoiding unnecessary early intervention.
*Colonoscopy at age 60*
- This is **too late** and ignores the increased risk from family history.
- Delaying screening until age 60 would miss the recommended earlier screening window for patients with first-degree relatives with CRC.
*Alcohol cessation*
- The patient drinks **1 alcoholic drink per day**, which is within recommended limits for women.
- While reducing alcohol consumption has general health benefits, this is not the most urgent preventive measure given her family history of colon cancer.
*Mammography now*
- Screening mammography typically begins at **age 40-50** for average-risk women.
- At age 35 with no specific high-risk factors (no BRCA mutation, no strong early-onset breast cancer family history), mammography is not indicated now.
*Mammography at age 50*
- While this may be appropriate for breast cancer screening depending on guidelines followed, it is **not the priority** given her significant family history of colorectal cancer requiring earlier intervention.
Male breast cancer US Medical PG Question 4: Patient 1 – A 26-year-old woman presents to her primary care physician for an annual exam. She currently does not have any acute concerns and says her health has been generally well. Medical history is significant for asthma, which is managed with an albuterol inhaler. Her last pap smear was unremarkable. She is currently sexually active with one male and consistently uses condoms. She occasionally smokes marijuana and drinks wine once per week. Her mother recently passed away from advanced ovarian cancer. Her sister is 37-years-old and was recently diagnosed with breast cancer and ovarian cancer. Physical examination is remarkable for a mildly anxious woman.
Patient 2 – A 27-year-old woman presents to her primary care physician for an annual exam. She says that she would like to be screened for breast cancer since two of her close friends were recently diagnosed. She noticed she has a small and mobile mass on her left breast, which increases in size and becomes tender around her time of menses. Family history is remarkable for hypertension in the father. The physical exam is significant for a small, well-defined, and mobile mass on her left breast that is not tender to palpation.
Which of the following is the best next step in management for patient 1 and 2?
- A. Patient 1 – Breast ultrasound. Patient 2 – Return in 3 months for a clinical breast exam
- B. Patient 1 – Reassurance. Patient 2 – Breast ultrasound
- C. Patient 1 – CA-125 testing. Patient 2 – BRCA testing
- D. Patient 1 – BRCA testing. Patient 2 – Breast ultrasound (Correct Answer)
- E. Patient 1 – Breast and ovarian ultrasound. Patient 2 – Mammography
Male breast cancer Explanation: ***Patient 1 – BRCA testing. Patient 2 – Breast ultrasound***
- Patient 1 has a strong family history of early-onset **breast and ovarian cancer** (**mother and sister**), suggesting a high probability of an inherited genetic mutation, such as **BRCA1/2**, which warrants genetic testing.
- Patient 2 presents with a **small, mobile, well-defined breast mass** that is likely benign, and a **breast ultrasound** is the appropriate initial imaging for further characterization in a young woman.
*Patient 1 – Breast ultrasound. Patient 2 – Return in 3 months for a clinical breast exam*
- Patient 1's primary concern is genetic predisposition due to family history, an **ultrasound** is not the initial or primary screening method for future cancer risk.
- Patient 2 has a palpable mass; waiting 3 months for a **clinical breast exam** without initial imaging (ultrasound) is not appropriate for evaluating a new breast lump.
*Patient 1 – Reassurance. Patient 2 – Breast ultrasound*
- Patient 1's family history of **early-onset breast and ovarian cancer** is a significant risk factor; therefore, simple **reassurance** without further investigation is inappropriate.
- While a **breast ultrasound** is appropriate for Patient 2, the recommendation for Patient 1 is incorrect.
*Patient 1 – CA-125 testing. Patient 2 – BRCA testing*
- **CA-125** is a tumor marker primarily used for monitoring ovarian cancer treatment or recurrence, not for initial screening in asymptomatic individuals, especially in a young woman with no active symptoms.
- **BRCA testing** is indicated for Patient 1 due to family history, but not for Patient 2 who has a likely benign breast mass and no significant family history.
*Patient 1 – Breast and ovarian ultrasound. Patient 2 – Mammography*
- Regular **breast and ovarian ultrasounds** are not recommended as primary screening tools for genetic risk in asymptomatic high-risk individuals like Patient 1.
- **Mammography** is less sensitive in young women (under 30) due to higher breast tissue density, making **ultrasound** the preferred initial imaging for Patient 2.
Male breast cancer US Medical PG Question 5: A 36-year-old man comes to the clinic for "bumps under his nipples." He is anxious that this could be breast cancer as his sister was just recently diagnosed. Past medical history is unremarkable except for an appendectomy at age 13. He currently works as a personal trainer and reports a diet that consists mainly of lean meat. The patient reports drinking 1-2 beers over the weekends. Physical examination demonstrates a muscular physique with mobile smooth masses below the areola bilaterally with no discharge. What other physical exam finding is most likely to be seen in this individual?
- A. Palmar erythema
- B. Testicular atrophy (Correct Answer)
- C. Bitemporal hemianopsia
- D. Fluid wave
- E. Spider angiomas
Male breast cancer Explanation: ***Testicular atrophy***
- The bilateral subareolar masses suggest **gynecomastia**, which can be caused by an **imbalance of estrogens and androgens**.
- **Androgen abuse** (e.g., anabolic steroids for muscle building as a personal trainer) can suppress endogenous testosterone production, leading to secondary hypogonadism and consequently, **testicular atrophy**.
*Palmar erythema*
- **Palmar erythema** is typically associated with **chronic liver disease**, which is not indicated by the patient's history or presenting symptoms.
- While liver disease can cause gynecomastia due to impaired estrogen metabolism, there are no other signs pointing to liver dysfunction.
*Bitemporal hemianopsia*
- **Bitemporal hemianopsia** is a visual field defect caused by compression of the **optic chiasm**, commonly by a **pituitary adenoma**.
- While some pituitary adenomas can secrete prolactin (leading to hypogonadism and sometimes gynecomastia), bitemporal hemianopsia is not the most likely finding associated with the probable cause of gynecomastia in this patient.
*Fluid wave*
- A **fluid wave** is a physical exam sign of **ascites**, which indicates significant fluid accumulation in the peritoneal cavity, usually due to **severe liver disease** or heart failure.
- There are no clinical signs or symptoms in the patient's presentation to suggest ascites or these underlying conditions.
*Spider angiomas*
- **Spider angiomas** (or spider nevi) are small, arteriolar lesions commonly found on the trunk, neck, and face. They are classically associated with **chronic liver disease** or conditions with high estrogen levels (like pregnancy).
- Similar to palmar erythema, there is no evidence of liver disease in this patient, making spider angiomas an unlikely finding.
Male breast cancer US Medical PG Question 6: A 40-year-old man presents with a painless firm mass in the right breast. Examination shows retraction of the nipple and the skin is fixed to the underlying mass. The axillary nodes are palpable. Which of the following statements is FALSE regarding the above condition?
- A. Lobular cancer is the most common breast cancer in males (Correct Answer)
- B. BRCA2 mutations are associated with increased risk
- C. These are positive for estrogen receptor
- D. Endocrine therapy plays an important role in treatment
- E. Gynecomastia may be caused by certain medications
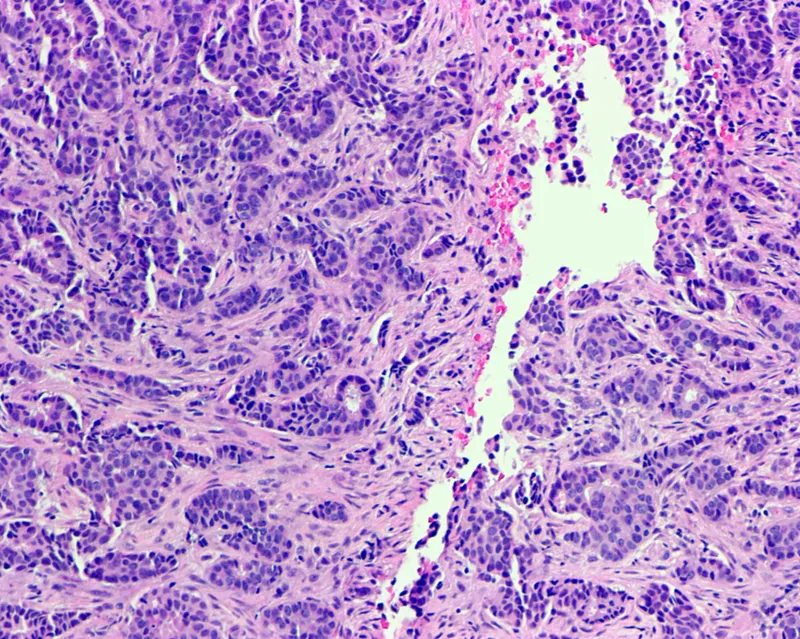
Male breast cancer Explanation: ***Lobular cancer is the most common breast cancer in males***
- This statement is **FALSE** and is the correct answer. The most common type of breast cancer in males is **invasive ductal carcinoma (IDC)**, accounting for about 80-90% of cases.
- **Invasive lobular carcinoma** is rare in men because men have very few lobules in their breast tissue.
*Gynecomastia may be caused by certain medications*
- This statement is **TRUE**. Medications such as spironolactone, cimetidine, finasteride, antipsychotics, and anabolic steroids can cause gynecomastia.
- However, the clinical presentation described (firm mass, nipple retraction, skin fixation, axillary nodes) is consistent with **malignancy**, not gynecomastia.
*BRCA2 mutations are associated with increased risk*
- This statement is **TRUE**. Male breast cancer is strongly associated with **BRCA2 mutations** (and less commonly BRCA1), which are hereditary.
- Men with BRCA2 mutations have a 5-10% lifetime risk of developing breast cancer, compared to less than 0.1% in the general male population.
*These are positive for estrogen receptor*
- This statement is **TRUE**. A vast majority (over 90%) of male breast cancers are **estrogen receptor (ER) positive**, which makes them responsive to endocrine therapy.
- This high rate of ER positivity is even greater than in female breast cancers.
*Endocrine therapy plays an important role in treatment*
- This statement is **TRUE**. Given the high prevalence of ER positivity (over 90%), endocrine therapy such as **tamoxifen** or aromatase inhibitors is a cornerstone of treatment for male breast cancer.
- Endocrine therapy is used in both adjuvant and metastatic settings for hormone receptor-positive disease.
Male breast cancer US Medical PG Question 7: A 29-year-old nulligravid woman comes to the physician because of a 10-day history of small quantities of intermittent, blood-tinged discharge from her left nipple. There is no personal or family history of serious illness. She has smoked 1 pack of cigarettes daily for 5 years. Her last menstrual period was 12 days ago. She is sexually active and uses condoms inconsistently. Physical examination shows scant serosanguinous fluid expressible from the left nipple. There is no palpable breast mass or axillary lymphadenopathy. Examination shows no other abnormalities. Which of the following is the most appropriate next step in management?
- A. Image-guided core biopsy of the affected duct
- B. Subareolar ultrasound (Correct Answer)
- C. Nipple discharge cytology
- D. Reassurance
- E. Breast MRI
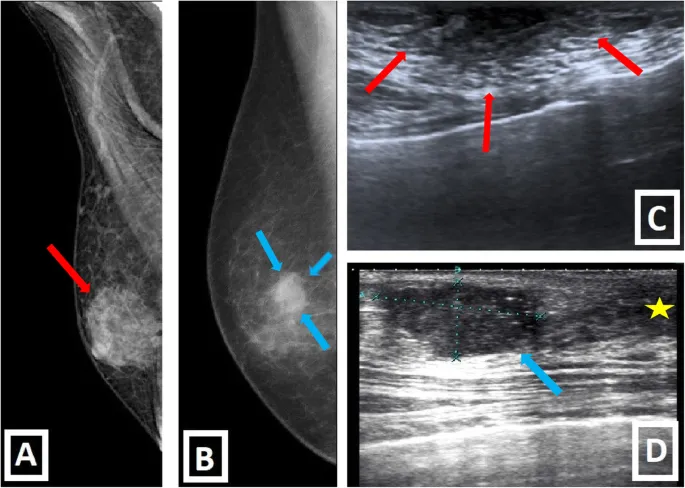
Male breast cancer Explanation: ***Subareolar ultrasound***
- This patient presents with **unilateral**, **spontaneous**, **single-duct bloody nipple discharge**, which is characteristic of an **intraductal papilloma** or early malignancy.
- A **subareolar ultrasound** is the most appropriate initial imaging step to evaluate the ductal system for a mass or obstruction, especially in a young woman with dense breasts where mammography may be less sensitive.
*Image-guided core biopsy of the affected duct*
- A biopsy would be considered if imaging (like ultrasound) reveals a suspicious lesion, but it is not the **initial diagnostic step**.
- **Image guidance** is necessary for biopsy of non-palpable lesions, but first, the lesion needs to be identified and characterized by imaging.
*Nipple discharge cytology*
- **Cytology of nipple discharge** has a **low sensitivity** for identifying malignancy and is generally not recommended as a primary diagnostic tool.
- It can be helpful in some cases, but imaging is usually preferred for initial evaluation of suspicious discharge.
*Reassurance*
- **Bloody nipple discharge**, even in small quantities, is a **concerning symptom** that requires further investigation to rule out malignancy and cannot simply be dismissed.
- While many cases are benign (e.g., intraductal papilloma), serious pathology must be excluded.
*Breast MRI*
- **Breast MRI** is a highly sensitive imaging modality but is typically reserved for **further evaluation** after initial mammography and ultrasound, especially in high-risk patients or for assessing the extent of known disease.
- It is **not the first-line imaging** for isolated bloody nipple discharge without other suspicious findings on initial assessment.
Male breast cancer US Medical PG Question 8: A 32-year-old woman presented for her annual physical examination. She mentioned that her family history had changed since her last visit: her mother was recently diagnosed with breast cancer and her sister tested positive for the BRCA2 mutation. The patient, therefore, requested testing as well. If the patient tests positive for the BRCA1 or BRCA2 mutation, which of the following is the best screening approach?
- A. Order magnetic resonance imaging of the breast
- B. Annual ultrasound, annual mammography, and monthly self-breast exams
- C. Twice-yearly clinical breast exams, annual mammography, annual breast MRI, and breast self-exams (Correct Answer)
- D. Annual clinical breast exams, annual mammography, and monthly self-breast exams
- E. Refer to radiation therapy
Male breast cancer Explanation: ***Twice-yearly clinical breast exams, annual mammography, annual breast MRI, and breast self-exams***
- For patients with **BRCA1 or BRCA2 mutations**, an intensive breast cancer screening protocol is recommended due to their highly increased lifetime risk of breast cancer.
- This typically includes **semiannual clinical breast exams**, **annual mammography**, and **annual breast MRI**, often starting at a young age.
*Order magnetic resonance imaging of the breast*
- While MRI is a crucial part of screening for high-risk individuals, it is **not sufficient as a standalone screening modality**.
- A comprehensive approach combining multiple screening methods is needed to maximize detection rates.
*Annual ultrasound, annual mammography, and monthly self-breast exams*
- **Breast ultrasound** is generally used as an adjunct to mammography when specific abnormalities are found or in women with dense breasts, not as a routine primary screening tool for BRCA carriers.
- While **mammography** and **self-breast exams** are included, this option lacks the crucial **annual MRI** and **twice-yearly clinical breast exams** recommended for BRCA carriers.
*Annual clinical breast exams, annual mammography, and monthly self-breast exams*
- This protocol is **less intensive** than what is recommended for women with BRCA mutations.
- It omits the essential **annual breast MRI** and the **twice-yearly clinical breast exams** that are critical for early detection in this high-risk population.
*Refer to radiation therapy*
- **Radiation therapy** is a treatment modality for existing cancer, not a screening approach for cancer prevention or early detection.
- Referring for radiation therapy would be appropriate only after a diagnosis of breast cancer, not as a primary screening strategy.
Male breast cancer US Medical PG Question 9: A 57-year-old nulliparous woman comes to the physician 2 weeks after noticing a lump in her right breast. Her last mammogram was performed 4 years ago and showed no abnormalities. Menopause began 2 years ago, during which time the patient was prescribed hormone replacement therapy for severe hot flashes and vaginal dryness. Vital signs are within normal limits. Examination of the right breast shows a firm, nontender mass close to the nipple. There are no changes in the skin or nipple, and there is no palpable axillary adenopathy. The abdomen is soft and nontender; there is no organomegaly. Mammography shows a suspicious 2-cm mass adjacent to the nipple. Which of the following is the most appropriate next step in management?
- A. Mastectomy
- B. Measurement of serum CA 15–3
- C. Core needle biopsy (Correct Answer)
- D. Fine needle aspiration
- E. Bone scan
Male breast cancer Explanation: ***Core needle biopsy***
- A **core needle biopsy** is the most appropriate next step to obtain a definitive diagnosis for a suspicious breast mass identified on mammography and clinical exam.
- It provides **tissue for histopathological examination**, allowing for precise classification of the tumor (e.g., invasive ductal carcinoma, lobular carcinoma), grading, and receptor status analysis (estrogen, progesterone, HER2), which are crucial for treatment planning.
*Mastectomy*
- **Mastectomy** is a surgical procedure for breast cancer removal but should only be performed **after a definitive diagnosis** has been established through biopsy.
- Proceeding directly to mastectomy without a biopsy risks unnecessary surgery if the mass proves to be benign.
*Measurement of serum CA 15–3*
- **CA 15-3** is a tumor marker that may be elevated in some patients with **advanced breast cancer**, but it is generally *not* sensitive or specific enough for diagnosis or initial staging.
- Its utility is primarily in **monitoring treatment response** or recurrence in patients with known metastatic disease, not for initial evaluation of a suspicious mass.
*Fine needle aspiration*
- **Fine needle aspiration** (FNA) can differentiate between solid and cystic masses and *may* provide cytological diagnosis, but it often does not provide enough tissue to determine invasiveness or perform complete receptor status analysis.
- A **core needle biopsy** is preferred as it yields more tissue for comprehensive pathology, which is critical for treatment decisions.
*Bone scan*
- A **bone scan** is used to detect **bone metastases** in patients with established breast cancer, particularly those with higher stages or symptoms suggestive of bone involvement.
- It is **not indicated as an initial diagnostic step** for a suspicious breast mass before a definitive diagnosis of cancer has been made and staging initiated.
Male breast cancer US Medical PG Question 10: A 47-year-old woman comes to the physician for a mass in her left breast she noticed 2 days ago during breast self-examination. She has hypothyroidism treated with levothyroxine. There is no family history of breast cancer. Examination shows large, moderately ptotic breasts. The mass in her left breast is small (approximately 1 cm x 0.5 cm), firm, mobile, and painless. It is located 4 cm from her nipple-areolar complex at the 7 o'clock position. There are no changes in the skin or nipple, and there is no palpable axillary adenopathy. No masses are palpable in her right breast. A urine pregnancy test is negative. Mammogram showed a soft tissue mass with poorly defined margins. Core needle biopsy confirms a low-grade infiltrating ductal carcinoma. The pathological specimen is positive for estrogen receptors and negative for progesterone and human epidermal growth factor receptor 2 (HER2) receptors. Staging shows no distant metastatic disease. Which of the following is the most appropriate next step in management?
- A. Lumpectomy with sentinel lymph node biopsy followed by hormone therapy
- B. Nipple-sparing mastectomy with axillary lymph node dissection followed by hormone therapy
- C. Nipple-sparing mastectomy with axillary lymph node dissection, followed by radiation and hormone therapy
- D. Radical mastectomy followed by hormone therapy
- E. Lumpectomy with sentinel lymph node biopsy, followed by radiation and hormone therapy (Correct Answer)
Male breast cancer Explanation: **Lumpectomy with sentinel lymph node biopsy, followed by radiation and hormone therapy**
- The patient has **early-stage (T1N0M0) estrogen receptor (ER)-positive, HER2-negative invasive ductal carcinoma** suitable for **breast-conserving surgery (lumpectomy)**.
- **Lumpectomy** must be followed by **radiation therapy** to the remaining breast tissue to reduce the risk of local recurrence, and **endocrine therapy** (due to ER positivity) is indicated to reduce systemic recurrence risk.
- **Sentinel lymph node biopsy** is performed to stage the axilla; if positive, an axillary lymph node dissection may be indicated. However, in this case, the mass is small, and there is no palpable axillary adenopathy, making sentinel lymph node biopsy the appropriate initial step.
*Lumpectomy with sentinel lymph node biopsy followed by hormone therapy*
- While **lumpectomy with sentinel lymph node biopsy** and **hormone therapy** are part of the appropriate management, **radiation therapy** to the conserved breast is a critical component that is missing from this option.
- Omitting **radiation therapy** after lumpectomy for invasive breast cancer significantly increases the risk of local recurrence.
*Nipple-sparing mastectomy with axillary lymph node dissection followed by hormone therapy*
- A **nipple-sparing mastectomy** is a more aggressive surgical approach than typically required for a **small, early-stage tumor** like this, which is amenable to breast-conserving surgery.
- **Axillary lymph node dissection** is usually reserved for cases with clinically positive lymph nodes or a positive sentinel lymph node biopsy, not as an initial step when there is no palpable axillary adenopathy.
*Nipple-sparing mastectomy with axillary lymph node dissection, followed by radiation and hormone therapy*
- This option involves an **unnecessarily extensive surgical procedure (nipple-sparing mastectomy with axillary lymph node dissection)** for a **small (1cm x 0.5cm) early-stage tumor** that can be managed with breast-conserving therapy.
- While radiation and hormone therapy are relevant, the initial surgical choice is too aggressive given the clinical presentation.
*Radical mastectomy followed by hormone therapy*
- **Radical mastectomy** (which includes removal of the breast, underlying chest muscle, and axillary lymph nodes) is rarely performed today due to its significant morbidity and is not indicated for this **early-stage tumor**.
- **Modified radical mastectomy**, which removes the breast and axillary lymph nodes while preserving the chest muscle, is typically only considered if breast-conserving surgery is not feasible or desired, and **hormone therapy** would be indicated, but **radiation** may also be needed depending on other factors.
More Male breast cancer US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.