Hereditary breast cancer syndromes US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Hereditary breast cancer syndromes. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Hereditary breast cancer syndromes US Medical PG Question 1: A 33-year-old woman comes to the physician 1 week after noticing a lump in her right breast. Fifteen years ago, she was diagnosed with osteosarcoma of her left distal femur. Her father died of an adrenocortical carcinoma at the age of 41 years. Examination shows a 2-cm, firm, immobile mass in the lower outer quadrant of the right breast. A core needle biopsy of the mass shows adenocarcinoma. Genetic analysis in this patient is most likely to show a defect in which of the following genes?
- A. BRCA1
- B. KRAS
- C. TP53 (Correct Answer)
- D. Rb
- E. PTEN
Hereditary breast cancer syndromes Explanation: ***TP53***
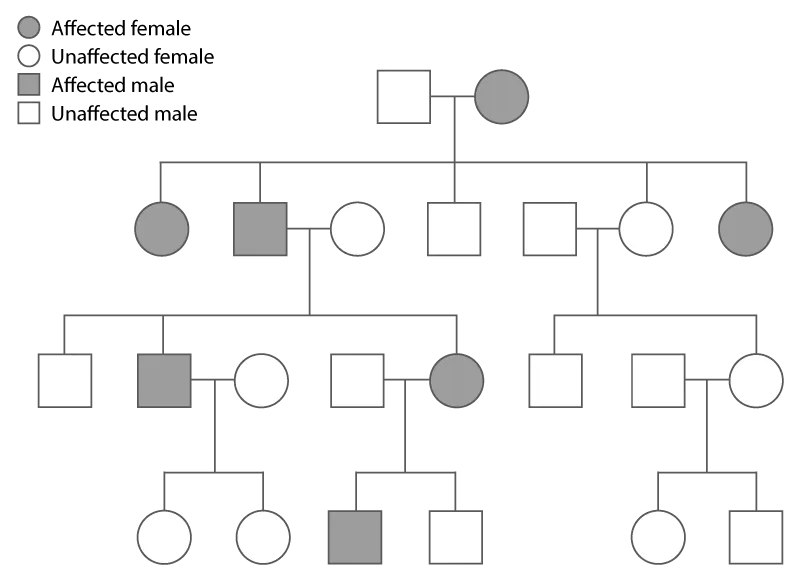
- This patient's presentation with **early-onset breast cancer**, a history of **osteosarcoma** at a young age, and a father's death from **adrenocortical carcinoma** at 41 years strongly suggests **Li-Fraumeni syndrome**.
- Li-Fraumeni syndrome is an autosomal dominant disorder caused by a germline mutation in the **tumor suppressor gene TP53**, increasing the risk for multiple primary cancers at a young age.
*BRCA1*
- While **BRCA1 mutations** are associated with an increased risk of breast and ovarian cancer, they are not typically linked to osteosarcoma or adrenocortical carcinoma.
- The constellation of cancers in this patient is more indicative of Li-Fraumeni syndrome than solely a BRCA1-related cancer syndrome.
*KRAS*
- **KRAS** is an oncogene commonly mutated in several cancers, including pancreatic, colorectal, and lung cancer, but is not primarily associated with either Li-Fraumeni syndrome or the specific tumors seen in this family history.
- Mutations in KRAS are typically somatic mutations acquired during a person's lifetime, not germline mutations causing inherited cancer syndromes like the one suggested here.
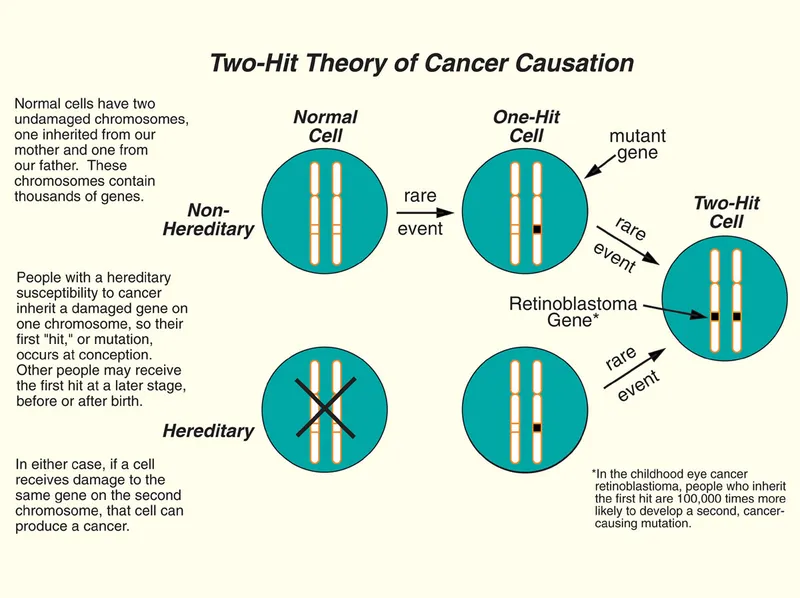
*Rb*
- Mutations in the **retinoblastoma (Rb) gene** are associated with retinoblastoma and an increased risk of osteosarcoma, but not typically with adrenocortical carcinoma or breast cancer as part of a classic inherited syndrome.
- The combination of breast cancer, osteosarcoma, and adrenocortical carcinoma points more specifically to TP53.
*PTEN*
- **PTEN mutations** are associated with Cowden syndrome, which increases the risk for breast cancer, thyroid cancer, and endometrial cancer, along with benign growths.
- However, Cowden syndrome does not typically include osteosarcoma or adrenocortical carcinoma as prominent features, making PTEN less likely than TP53 for this specific family history.
Hereditary breast cancer syndromes US Medical PG Question 2: A 38-year-old female presents to her primary care physician with complaints of several episodes of palpitations accompanied by panic attacks over the last month. She also is concerned about many instances over the past few weeks where food has been getting stuck in her throat and she has had trouble swallowing. She denies any prior medical problems and reports a family history of cancer in her mother and maternal grandfather but cannot recall any details regarding the type of cancer(s) or age of diagnosis. Her vital signs at today's visit are as follows: T 37.6 deg C, HR 106, BP 158/104, RR 16, SpO2 97%. Physical examination is significant for a nodule on the anterior portion of the neck that moves with swallowing, accompanied by mild lymphadenopathy. A preliminary work-up is initiated, which shows hypercalcemia, elevated baseline calcitonin, and an inappropriately elevated PTH level. Diagnostic imaging shows bilateral adrenal lesions on an MRI of the abdomen/pelvis. Which of the following is the most likely diagnosis in this patient?
- A. Familial medullary thyroid cancer (FMTC)
- B. Li-Fraumeni syndrome
- C. Multiple endocrine neoplasia (MEN) IIa (Correct Answer)
- D. Multiple endocrine neoplasia (MEN) I
- E. Multiple endocrine neoplasia (MEN) IIb
Hereditary breast cancer syndromes Explanation: ***Multiple endocrine neoplasia (MEN) IIa***
- This patient presents with **medullary thyroid cancer** (due to the thyroid nodule, elevated calcitonin, and family history of cancer), **pheochromocytoma** (indicated by palpitations, panic attacks, hypertension, and adrenal lesions), and **primary hyperparathyroidism** (evidenced by hypercalcemia and inappropriately elevated PTH). These three conditions are the classic triad of MEN IIa.
- The symptoms of food getting stuck in her throat are also consistent with the presence of a **thyroid nodule**.
*Familial medullary thyroid cancer (FMTC)*
- While the patient has **medullary thyroid cancer**, FMTC is typically characterized solely by medullary thyroid carcinoma without the associated pheochromocytoma or primary hyperparathyroidism seen in this case.
- This patient's presentation includes **adrenal lesions** and **hyperparathyroidism**, which are not features of isolated FMTC.
*Li-Fraumeni syndrome*
- This syndrome is associated with a high risk of various cancers, including sarcomas, breast cancer, brain tumors, and adrenocortical carcinoma, but it is not typically associated with **medullary thyroid cancer, pheochromocytoma, or primary hyperparathyroidism** as a primary presentation.
- The genetic basis is a mutation in the **TP53 gene**, and the clinical picture does not match the specific endocrine tumors observed here.
*Multiple endocrine neoplasia (MEN) I*
- MEN I is characterized by tumors of the **parathyroid, pituitary, and pancreas** (the 3 Ps).
- This patient's presentation of medullary thyroid cancer, pheochromocytoma, and primary hyperparathyroidism does not include pituitary or pancreatic tumors, and medullary thyroid cancer and pheochromocytoma are not part of the MEN I spectrum.
*Multiple endocrine neoplasia (MEN) IIb*
- MEN IIb includes **medullary thyroid cancer** and **pheochromocytoma**, which are present in this patient.
- However, MEN IIb also classically presents with characteristic **mucosal neuromas** and a **marfanoid habitus**, and *lacks* primary hyperparathyroidism, which this patient clearly exhibits.
Hereditary breast cancer syndromes US Medical PG Question 3: Patient 1 – A 26-year-old woman presents to her primary care physician for an annual exam. She currently does not have any acute concerns and says her health has been generally well. Medical history is significant for asthma, which is managed with an albuterol inhaler. Her last pap smear was unremarkable. She is currently sexually active with one male and consistently uses condoms. She occasionally smokes marijuana and drinks wine once per week. Her mother recently passed away from advanced ovarian cancer. Her sister is 37-years-old and was recently diagnosed with breast cancer and ovarian cancer. Physical examination is remarkable for a mildly anxious woman.
Patient 2 – A 27-year-old woman presents to her primary care physician for an annual exam. She says that she would like to be screened for breast cancer since two of her close friends were recently diagnosed. She noticed she has a small and mobile mass on her left breast, which increases in size and becomes tender around her time of menses. Family history is remarkable for hypertension in the father. The physical exam is significant for a small, well-defined, and mobile mass on her left breast that is not tender to palpation.
Which of the following is the best next step in management for patient 1 and 2?
- A. Patient 1 – Breast ultrasound. Patient 2 – Return in 3 months for a clinical breast exam
- B. Patient 1 – Reassurance. Patient 2 – Breast ultrasound
- C. Patient 1 – CA-125 testing. Patient 2 – BRCA testing
- D. Patient 1 – BRCA testing. Patient 2 – Breast ultrasound (Correct Answer)
- E. Patient 1 – Breast and ovarian ultrasound. Patient 2 – Mammography
Hereditary breast cancer syndromes Explanation: ***Patient 1 – BRCA testing. Patient 2 – Breast ultrasound***
- Patient 1 has a strong family history of early-onset **breast and ovarian cancer** (**mother and sister**), suggesting a high probability of an inherited genetic mutation, such as **BRCA1/2**, which warrants genetic testing.
- Patient 2 presents with a **small, mobile, well-defined breast mass** that is likely benign, and a **breast ultrasound** is the appropriate initial imaging for further characterization in a young woman.
*Patient 1 – Breast ultrasound. Patient 2 – Return in 3 months for a clinical breast exam*
- Patient 1's primary concern is genetic predisposition due to family history, an **ultrasound** is not the initial or primary screening method for future cancer risk.
- Patient 2 has a palpable mass; waiting 3 months for a **clinical breast exam** without initial imaging (ultrasound) is not appropriate for evaluating a new breast lump.
*Patient 1 – Reassurance. Patient 2 – Breast ultrasound*
- Patient 1's family history of **early-onset breast and ovarian cancer** is a significant risk factor; therefore, simple **reassurance** without further investigation is inappropriate.
- While a **breast ultrasound** is appropriate for Patient 2, the recommendation for Patient 1 is incorrect.
*Patient 1 – CA-125 testing. Patient 2 – BRCA testing*
- **CA-125** is a tumor marker primarily used for monitoring ovarian cancer treatment or recurrence, not for initial screening in asymptomatic individuals, especially in a young woman with no active symptoms.
- **BRCA testing** is indicated for Patient 1 due to family history, but not for Patient 2 who has a likely benign breast mass and no significant family history.
*Patient 1 – Breast and ovarian ultrasound. Patient 2 – Mammography*
- Regular **breast and ovarian ultrasounds** are not recommended as primary screening tools for genetic risk in asymptomatic high-risk individuals like Patient 1.
- **Mammography** is less sensitive in young women (under 30) due to higher breast tissue density, making **ultrasound** the preferred initial imaging for Patient 2.
Hereditary breast cancer syndromes US Medical PG Question 4: A 34-year-old woman comes to the physician for a routine health maintenance examination. She has gastroesophageal reflux disease. She recently moved to a new city. Her father was diagnosed with colon cancer at age 46. Her father's brother died because of small bowel cancer. Her paternal grandfather died because of stomach cancer. She takes a vitamin supplement. Current medications include esomeprazole and a multivitamin. She smoked one pack of cigarettes daily for 6 years but quit 2 years ago. She drinks one to two alcoholic beverages on weekends. She appears healthy. Vital signs are within normal limits. Physical examination shows no abnormalities. Colonoscopy is unremarkable. Germline testing via DNA sequencing in this patient shows mutations in DNA repair genes MLH1 and MSH2. Which of the following will this patient most likely require at some point in her life?
- A. Celecoxib or sulindac therapy
- B. Bilateral prophylactic mastectomy
- C. Surgical removal of a desmoid tumor
- D. Prophylactic proctocolectomy with ileoanal anastomosis
- E. Hysterectomy and bilateral salpingo-oophorectomy (Correct Answer)
Hereditary breast cancer syndromes Explanation: ***Hysterectomy and bilateral salpingo-oophorectomy***
- The patient's family history of multiple cancers (colon, small bowel, stomach) at a young age, along with positive germline mutations in **MLH1** and **MSH2**, is highly indicative of **Lynch syndrome (hereditary nonpolyposis colorectal cancer)**.
- Women with Lynch syndrome have a significantly increased risk of developing **endometrial cancer** (up to 60%) and **ovarian cancer** (up to 12%), making prophylactic hysterectomy and bilateral salpingo-oophorectomy a recommended risk-reducing surgery after childbearing is complete.
*Celecoxib or sulindac therapy*
- **NSAIDs** like celecoxib and sulindac are sometimes used for chemoprevention in patients with **Familial Adenomatous Polyposis (FAP)** to reduce polyp burden, but their role in Lynch syndrome is less established and not the primary prophylactic measure for gynecologic cancers.
- While Lynch syndrome does increase colorectal cancer risk, the immediate and most concerning risk for women with cancer predisposition in MLH1 and MSH2 genes is gynecologic.
*Surgical removal of a desmoid tumor*
- **Desmoid tumors** are characteristic extracolonic manifestations of **Familial Adenomatous Polyposis (FAP)**, not Lynch syndrome.
- The mutations in MLH1 and MSH2 are associated with Lynch syndrome, which has a different spectrum of extracolonic malignancies.
*Prophylactic proctocolectomy with ileoanal anastomosis*
- This procedure is primarily recommended for patients with **Familial Adenomatous Polyposis (FAP)** due to the near 100% lifetime risk of colorectal cancer development from numerous polyps.
- While Lynch syndrome also carries a high risk of colorectal cancer, the typical approach involves intensive surveillance (colonoscopy every 1-2 years) rather than universal prophylactic colectomy, unless specific high-risk features or advanced lesions are found.
Hereditary breast cancer syndromes US Medical PG Question 5: A 74-year-old retired female teacher is referred to the endocrinology clinic. She is very concerned about a large mass in her neck that has progressively enlarged over the past 2 weeks. She also reports a 15 pound weight loss over the last 3 months. She now has hoarseness and difficulty swallowing her food, giving her a sensation that food gets stuck in her windpipe when she swallows. There is no pain associated with swallowing. Her speech is monotonous. No other gait or language articulation problems are noted. Testing for cranial nerve lesions is unremarkable. On palpation, a large, fixed and non-tender mass in the thyroid is noted. Cervical lymph nodes are palpable bilaterally. The patient is urgently scheduled for an ultrasound-guided fine needle aspiration to guide management. Which of the following is the most likely gene mutation to be found in this mass?
- A. Activating mutation of the Ras protooncogene
- B. Inactivating mutation of the p53 tumor suppressor gene (Correct Answer)
- C. RET/PTC rearrangement
- D. BRAF mutation
- E. RET gene mutation
Hereditary breast cancer syndromes Explanation: ***Inactivating mutation of the p53 tumor suppressor gene***
- The patient's presentation with a **rapidly enlarging, fixed, non-tender thyroid mass**, *hoarseness*, *dysphagia*, *weight loss*, and *palpable cervical lymph nodes* is highly suggestive of **anaplastic thyroid carcinoma (ATC)**, an aggressive malignancy.
- Inactivating mutations of the **p53 tumor suppressor gene** are frequently associated with the development and progression of ATC, contributing to its uncontrolled growth and poor prognosis.
*Activating mutation of the Ras protooncogene*
- **Ras mutations** are more commonly found in *follicular thyroid carcinoma* and *follicular variants of papillary thyroid carcinoma*.
- While they can indicate malignancy, they are not typically the primary genetic driver for the highly aggressive features seen in anaplastic carcinoma.
*RET/PTC rearrangement*
- **RET/PTC rearrangements** are characteristic genetic alterations found in **papillary thyroid carcinoma (PTC)**.
- PTC typically presents with a *slower growth rate* and *less aggressive features* compared to the rapid progression described in the patient.
*BRAF mutation*
- The **BRAF V600E mutation** is the most common genetic alteration in **papillary thyroid carcinoma (PTC)**, especially the conventional and tall-cell variants.
- While it indicates a more aggressive subset of PTC, it is generally not the primary mutation associated with the extremely aggressive and rapidly progressing features of anaplastic thyroid carcinoma.
*RET gene mutation*
- **Germline RET mutations** are primarily associated with **medullary thyroid carcinoma (MTC)**, often occurring as part of Multiple Endocrine Neoplasia type 2 (MEN2).
- The clinical presentation with a *rapidly growing, fixed mass* and *compressive symptoms* is less typical for MTC, which can also be aggressive but usually presents differently.
Hereditary breast cancer syndromes US Medical PG Question 6: A 39-year-old female presents to her gynecologist complaining of a breast lump. Two weeks ago, while performing a breast self-examination she noticed a small firm nodule in her left breast. She is otherwise healthy and takes no medications. Her family history is notable for a history of breast cancer in her mother and maternal aunt. On physical examination, there is a firm immobile nodular mass in the superolateral quadrant of her left breast. A mammogram of her left breast is shown. Genetic analysis reveals a mutation on chromosome 17. This patient is at increased risk for which of the following conditions?
- A. Invasive lobular carcinoma
- B. Ductal carcinoma in situ (DCIS)
- C. Inflammatory breast cancer
- D. Invasive ductal carcinoma
- E. Medullary carcinoma (Correct Answer)
Hereditary breast cancer syndromes Explanation: ***Medullary carcinoma***
- This patient's presentation with a **firm, immobile breast mass** and a **strong family history of breast cancer**, along with a **mutation on chromosome 17 (BRCA1 gene)**, strongly suggests an increased risk for **medullary carcinoma**. Medullary carcinoma is more common in BRCA1 mutation carriers.
- While medullary carcinoma is a subtype of invasive ductal carcinoma, its specific association with BRCA1 and distinct histologic features (e.g., syncytial growth pattern, prominent lymphoid infiltrate) make it the most precise answer in this context.
*Invasive lobular carcinoma*
- This type of carcinoma is characterized by **loss of E-cadherin** expression, leading to a single-file growth pattern.
- While it is an invasive breast cancer, it is **not specifically linked to BRCA1 mutations** as strongly as medullary carcinoma.
*Ductal carcinoma in situ (DCIS)*
- **DCIS is a non-invasive breast cancer** where abnormal cells are confined to the breast ducts and have not spread to surrounding tissue.
- The patient's presentation with a palpable, firm mass suggests an **invasive lesion**, making DCIS less likely as the primary concern for future risk.
*Inflammatory breast cancer*
- This is a rare and aggressive form of breast cancer characterized by **skin erythema, edema, and a "peau d'orange" appearance**, often without a palpable lump.
- The patient's physical examination findings of a **firm, immobile nodular mass** do not align with the typical presentation of inflammatory breast cancer.
*Invasive ductal carcinoma*
- While **invasive ductal carcinoma (IDC)** is the most common type of breast cancer and a possible diagnosis for the current lump, the question asks about **increased risk** given the specific genetic mutation.
- Of the various types of IDC, **medullary carcinoma** has a particularly strong association with **BRCA1 mutations**, making it a more specific and accurate answer for future risk in this scenario.
Hereditary breast cancer syndromes US Medical PG Question 7: A 40-year-old man presents with an episode of rectal bleeding. He is concerned because his mother died of colorectal cancer at 50 years of age. He has no further information about his family history. Physical examination and digital rectal examination are normal. He undergoes a colonoscopy and is found to have innumerable adenomas in the left side of the colon ranging in size from 4–15 mm. Which of the following is the most likely underlying mechanism of this patient illness?
- A. Mutation in DNA mismatch repair genes
- B. Inactivation of RB1 gene
- C. Alterations in STK11 gene
- D. Inactivation of BRCA1 and BRCA2 genes
- E. Mutations of the APC gene (Correct Answer)
Hereditary breast cancer syndromes Explanation: ***Mutations of the APC gene***
- The description of **innumerable adenomas** in the colon, particularly at a relatively young age and with a family history of early-onset colorectal cancer, is highly suggestive of **familial adenomatous polyposis (FAP)**.
- FAP is an autosomal dominant condition caused by germline mutations in the **adenomatous polyposis coli (APC) gene**, a tumor suppressor gene, leading to the development of hundreds to thousands of adenomatous polyps and an almost 100% lifetime risk of colorectal cancer.
*Mutation in DNA mismatch repair genes*
- Mutations in **DNA mismatch repair genes** (e.g., MLH1, MSH2, MSH6, PMS2) are associated with **Lynch syndrome (hereditary nonpolyposis colorectal cancer)**.
- Lynch syndrome typically presents with fewer polyps (though an increased risk of colorectal cancer, especially right-sided) and other extracolonic cancers, which is less consistent with "innumerable adenomas."
*Inactivation of RB1 gene*
- The **RB1 gene** is a tumor suppressor gene primarily associated with **retinoblastoma** and has a role in other cancers like osteosarcoma.
- It is not the primary genetic mechanism for the development of multiple colonic adenomas described in this patient.
*Alterations in STK11 gene*
- Alterations in the **STK11 gene** are associated with **Peutz-Jeghers syndrome**, an autosomal dominant disorder characterized by the development of multiple **hamartomatous polyps** mainly in the gastrointestinal tract, especially the small intestine, and characteristic **mucocutaneous pigmentation**.
- These polyps are hamartomatous, not adenomatous, and while they carry a cancer risk, the presentation of innumerable adenomas points away from Peutz-Jeghers syndrome.
*Inactivation of BRCA1 and BRCA2 genes*
- **BRCA1 and BRCA2 genes** are critical tumor suppressor genes primarily associated with an increased risk of **breast cancer** and **ovarian cancer**, as well as some other cancers like prostate and pancreatic cancer.
- While these genes are important in cancer development, they are not directly implicated in the pathogenesis of familial adenomatous polyposis or the significant number of colonic adenomas described.
Hereditary breast cancer syndromes US Medical PG Question 8: A 65-year-old African American man presents for follow-up examination with a 6-month history of urinary hesitancy, weak stream, and terminal dribbling, which is refractory to a combination therapy of finasteride and tamsulosin. The patient’s past medical history is otherwise unremarkable. His father and brother were diagnosed with prostate cancer at the age of 55 years. His vital signs are within normal limits. The patient has a normal anal sphincter tone and a bulbocavernosus muscle reflex. Digital rectal exam (DRE) reveals a prostate size equivalent to 2 finger pads with a hard nodule and without fluctuance or tenderness. Serum prostate-specific antigen (PSA) level is 5 ng/mL. Which of the following investigations is most likely to establish a definitive diagnosis?
- A. Magnetic resonance imaging (MRI)
- B. 4Kscore test
- C. Prostate Health Index (PHI)
- D. Image-guided needle biopsy (Correct Answer)
- E. PSA in 3 months
Hereditary breast cancer syndromes Explanation: ***Image-guided needle biopsy***
- A definitive diagnosis of **prostate cancer** requires histological confirmation, which is achieved through a **biopsy**.
- The patient's presentation with a **hard nodule** on DRE, elevated PSA, and a strong family history of prostate cancer, despite treatment for BPH, strongly indicates the need for a biopsy.
*Magnetic resonance imaging (MRI)*
- While MRI can help in **staging prostate cancer** and guiding biopsies, it does not provide a definitive diagnosis on its own.
- An MRI may identify suspicious lesions but **cannot confirm malignancy** without tissue sampling.
*4Kscore test*
- The 4Kscore test estimates the **risk of high-grade prostate cancer** but does not provide a definitive diagnosis.
- It uses a panel of four prostate-specific kallikrein proteins, along with patient age, DRE status, and prior biopsy results, to calculate a risk score.
*Prostate Health Index (PHI)*
- The PHI is a blood test that combines total PSA, free PSA, and [-2]proPSA to assess the **probability of prostate cancer**.
- It helps in deciding whether a biopsy is needed, but like the 4Kscore, it is not a diagnostic tool in itself.
*PSA in 3 months*
- Re-checking PSA in 3 months would **delay definitive diagnosis** and treatment for a potentially aggressive cancer, especially given the palpable nodule and family history.
- The current PSA of 5 ng/mL, although not extremely high, combined with the suspicious DRE finding, warrants more immediate action.
Hereditary breast cancer syndromes US Medical PG Question 9: A 64-year-old woman presents to the surgical oncology clinic as a new patient for evaluation of recently diagnosed breast cancer. She has a medical history of type 2 diabetes mellitus for which she takes metformin. Her surgical history is a total knee arthroplasty 7 years ago. Her family history is insignificant. Physical examination is notable for an irregular nodule near the surface of her right breast. Her primary concern today is which surgical approach will be chosen to remove her breast cancer. Which of the following procedures involves the removal of a portion of a breast?
- A. Arthroplasty
- B. Lumpectomy (Correct Answer)
- C. Vasectomy
- D. Mastectomy
- E. Laminectomy
Hereditary breast cancer syndromes Explanation: ***Lumpectomy***
- A **lumpectomy** is a surgical procedure that removes the **breast cancer tumor** and a small margin of surrounding healthy tissue, preserving most of the breast.
- This procedure is a common treatment for early-stage breast cancer and is often followed by radiation therapy.
*Arthroplasty*
- **Arthroplasty** is a surgical procedure to **repair or replace a joint**, typically due to arthritis or injury.
- The patient's history of a total knee arthroplasty indicates this procedure was performed on her knee, not her breast.
*Vasectomy*
- A **vasectomy** is a surgical procedure for **male sterilization**, involving the cutting and sealing of the vas deferens.
- This procedure is unrelated to breast cancer treatment or breast surgery.
*Mastectomy*
- A **mastectomy** involves the **complete surgical removal of the entire breast**, often including the nipple and areola.
- While it is a breast surgery, it removes the *entire* breast, not just a portion.
*Laminectomy*
- A **laminectomy** is a surgical procedure that removes a portion of the **vertebra (lamina)** to relieve pressure on the spinal cord or nerves.
- This procedure is for spinal conditions and is entirely unrelated to breast cancer surgery.
Hereditary breast cancer syndromes US Medical PG Question 10: An excisional biopsy is performed and the diagnosis of superficial spreading melanoma is confirmed. The lesion is 1.1 mm thick. Which of the following is the most appropriate next step in management?
- A. Surgical excision with 0.5-1 cm safety margins only
- B. Surgical excision with 1 cm safety margins only
- C. Surgical excision with 1-2 cm safety margins only
- D. Surgical excision with 0.5-1 cm safety margins and sentinel lymph node study
- E. Surgical excision with 1-2 cm safety margins and sentinel lymph node study (Correct Answer)
Hereditary breast cancer syndromes Explanation: ***Surgical excision with 1-2 cm safety margins and sentinel lymph node study***
- A melanoma with a **Breslow thickness between 1.01 mm and 2.0 mm** (like this 1.1 mm lesion) requires a recommended surgical margin of **1 to 2 cm**.
- For melanomas **≥0.8 mm thickness** (or those with ulceration), a **sentinel lymph node biopsy (SLNB)** is recommended to assess for micrometastasis, as it helps in staging and prognosis.
*Surgical excision with 0.5-1 cm safety margins only*
- A 0.5 cm margin is typically reserved for melanoma *in situ* or extremely thin melanomas (less than or equal to 0.5 mm), and 1 cm for lesions 0.51 to 1.0 mm, which is too narrow for a 1.1 mm lesion.
- This option incorrectly omits the **sentinel lymph node study**, which is indicated for a melanoma of this thickness.
*Surgical excision with 1 cm safety margins only*
- While 1 cm is a common margin for lesions up to 1.0 mm, a 1.1 mm melanoma usually warrants a slightly wider margin, ideally 1-2 cm.
- This option also fails to include the **sentinel lymph node study**, which is crucial for staging melanomas ≥0.8 mm thickness.
*Surgical excision with 0.5-1 cm safety margins and sentinel lymph node study*
- The recommended surgical margin for a 1.1 mm melanoma is at least **1 cm, preferably between 1 and 2 cm**, making a 0.5-1 cm range insufficient.
- Although it correctly includes the sentinel lymph node study, the **surgical margin is inadequate** for the given Breslow thickness.
*Surgical excision with 1-2 cm safety margins only*
- While the **1-2 cm surgical margin** is appropriate for a 1.1 mm melanoma, this option **incorrectly excludes the sentinel lymph node study**.
- The sentinel lymph node biopsy is a critical part of the staging and management plan for melanomas of this thickness to detect potential nodal involvement.
More Hereditary breast cancer syndromes US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.