Breast conservation therapy US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Breast conservation therapy. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Breast conservation therapy US Medical PG Question 1: A 64-year-old woman presents to the surgical oncology clinic as a new patient for evaluation of recently diagnosed breast cancer. She has a medical history of type 2 diabetes mellitus for which she takes metformin. Her surgical history is a total knee arthroplasty 7 years ago. Her family history is insignificant. Physical examination is notable for an irregular nodule near the surface of her right breast. Her primary concern today is which surgical approach will be chosen to remove her breast cancer. Which of the following procedures involves the removal of a portion of a breast?
- A. Arthroplasty
- B. Lumpectomy (Correct Answer)
- C. Vasectomy
- D. Mastectomy
- E. Laminectomy
Breast conservation therapy Explanation: ***Lumpectomy***
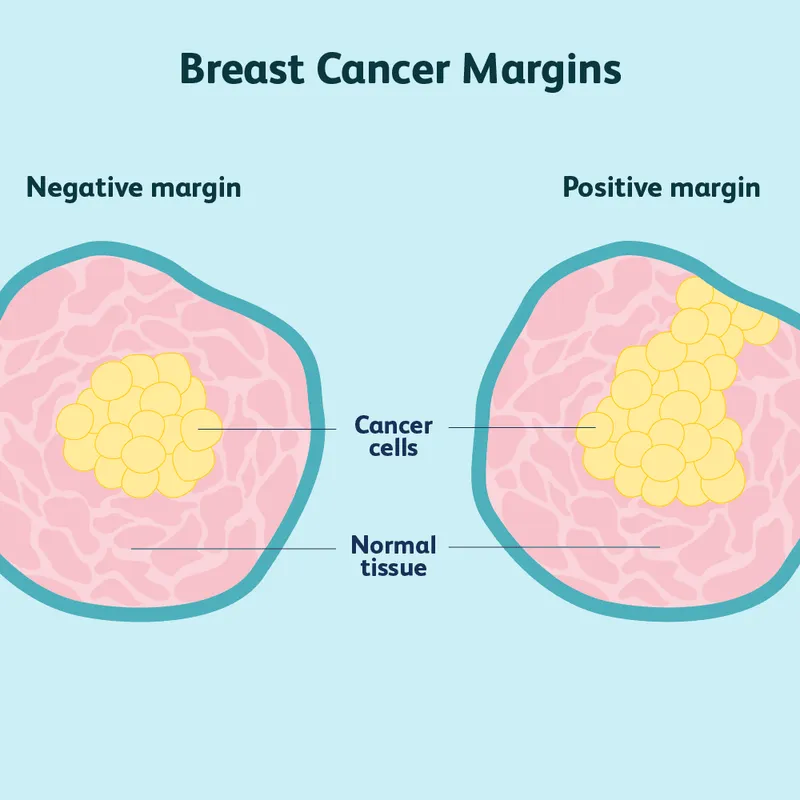
- A **lumpectomy** is a surgical procedure that removes the **breast cancer tumor** and a small margin of surrounding healthy tissue, preserving most of the breast.
- This procedure is a common treatment for early-stage breast cancer and is often followed by radiation therapy.
*Arthroplasty*
- **Arthroplasty** is a surgical procedure to **repair or replace a joint**, typically due to arthritis or injury.
- The patient's history of a total knee arthroplasty indicates this procedure was performed on her knee, not her breast.
*Vasectomy*
- A **vasectomy** is a surgical procedure for **male sterilization**, involving the cutting and sealing of the vas deferens.
- This procedure is unrelated to breast cancer treatment or breast surgery.
*Mastectomy*
- A **mastectomy** involves the **complete surgical removal of the entire breast**, often including the nipple and areola.
- While it is a breast surgery, it removes the *entire* breast, not just a portion.
*Laminectomy*
- A **laminectomy** is a surgical procedure that removes a portion of the **vertebra (lamina)** to relieve pressure on the spinal cord or nerves.
- This procedure is for spinal conditions and is entirely unrelated to breast cancer surgery.
Breast conservation therapy US Medical PG Question 2: The patient undergoes a mammogram, which shows a 6.5mm sized mass with an irregular border and spiculated margins. A subsequent core needle biopsy of the mass shows infiltrating ductal carcinoma with HER2-positive, estrogen-negative, and progesterone-negative immunohistochemistry staining. Blood counts and liver function tests are normal. Laboratory studies show:
Hemoglobin 12.5 g/dL
Serum
Na+ 140 mEq/L
Cl- 103 mEq/L
K+ 4.2 mEq/L
HCO3- 26 mEq/L
Ca2+ 8.9 mg/dL
Urea Nitrogen 12 mg/dL
Glucose 110 mg/dL
Alkaline Phosphatase 25 U/L
Alanine aminotransferase (ALT) 15 U/L
Aspartate aminotransferase (AST) 13 U/L
Which of the following is the most appropriate next step in management?
- A. Breast-conserving therapy and sentinel lymph node biopsy (Correct Answer)
- B. Bilateral mastectomy with lymph node dissection
- C. Trastuzumab therapy
- D. Bone scan
- E. Whole-body PET/CT
Breast conservation therapy Explanation: ***Breast-conserving therapy and sentinel lymph node biopsy***
- The patient has **early-stage (T1) breast cancer** (6.5mm mass), which is amenable to **breast-conserving therapy (lumpectomy)** as the primary surgical approach.
- A **sentinel lymph node biopsy** is essential to determine nodal status and guide further staging and adjuvant therapy, as the tumor size does not preclude nodal involvement.
*Bilateral mastectomy with lymph node dissection*
- This is an **overly aggressive surgical approach** for a small, unifocal tumor without evidence of multifocality or significant risk factors for recurrence in the contralateral breast.
- While **axillary lymph node dissection** may be indicated if the sentinel node is positive, it is not the initial preferred approach for all patients, especially with no current evidence of nodal metastasis.
*Trastuzumab therapy*
- **Trastuzumab** is a targeted therapy for **HER2-positive breast cancer**, but it is typically administered as **adjuvant therapy** (after surgery) or neoadjuvant therapy (before surgery).
- It is not the most appropriate *initial* next step before surgical management and comprehensive staging have been completed.
*Bone scan*
- A **bone scan** is used to detect **bone metastases**, but it is generally reserved for patients with **advanced-stage cancer** (e.g., T3/T4 tumor, N2/N3 nodes), symptoms suggestive of bony involvement, or significantly elevated alkaline phosphatase.
- Given the patient's small tumor size (6.5mm), normal labs, and lack of symptoms, a bone scan is not indicated as the *next* immediate step.
*Whole-body PET/CT*
- **Whole-body PET/CT** is primarily used for **staging advanced cancer** or investigating suspicious findings in symptomatic patients.
- For this small, early-stage breast cancer with no signs of distant metastasis indicated by normal blood tests, a PET/CT is **not recommended** as routine staging and carries unnecessary radiation exposure and cost.
Breast conservation therapy US Medical PG Question 3: A 42-year-old woman presents to the physician because of an abnormal breast biopsy report following suspicious findings on breast imaging. Other than being concerned about her report, she feels well. She has no history of any serious illnesses and takes no medications. She does not smoke. She consumes wine 1–2 times per week with dinner. There is no significant family history of breast or ovarian cancer. Vital signs are within normal limits. Physical examination shows no abnormal findings. The biopsy shows lobular carcinoma in situ (LCIS) in the left breast. Which of the following is the most appropriate next step in management?
- A. Careful observation + routine mammography (Correct Answer)
- B. Left mastectomy + axillary dissection + local irradiation
- C. Lumpectomy + routine screening
- D. Lumpectomy + breast irradiation
- E. Breast irradiation + tamoxifen
Breast conservation therapy Explanation: ***Careful observation + routine mammography***
- **Lobular carcinoma in situ (LCIS)** is considered a **non-obligate precursor** to invasive carcinoma, meaning it indicates an increased risk for developing invasive breast cancer in either breast (approximately 1-2% per year), but it is not itself invasive.
- Management typically involves **careful surveillance** with routine clinical exams and **mammography**, as this is the most appropriate initial approach for classic LCIS.
- Surgical excision is often unnecessary due to LCIS's diffuse nature and the fact that it serves as a risk marker rather than a direct precancerous lesion requiring removal.
*Left mastectomy + axillary dissection + local irradiation*
- This aggressive approach is reserved for **invasive breast cancer** and would be excessive for LCIS, which is a non-invasive lesion and a marker of increased risk rather than an immediate threat.
- **Axillary dissection** is performed to stage nodal involvement in invasive cancer, which is not applicable here as LCIS does not metastasize.
*Lumpectomy + routine screening*
- While a **lumpectomy (excision)** may be considered for **pleomorphic LCIS** or when there is diagnostic uncertainty, it is not the standard initial management for classic LCIS.
- Classic LCIS is often multifocal and bilateral, making localized excision less effective as a risk-reduction strategy.
*Lumpectomy + breast irradiation*
- **Radiation therapy** is typically used to reduce local recurrence risk after **lumpectomy for invasive breast cancer** or **ductal carcinoma in situ (DCIS)**.
- For LCIS, irradiation is generally not recommended as it is non-invasive and does not benefit from local radiation treatment.
*Breast irradiation + tamoxifen*
- **Tamoxifen** is a selective estrogen receptor modulator (SERM) that can be **offered for risk reduction** in women with LCIS, potentially reducing the risk of invasive breast cancer by approximately 50%.
- However, tamoxifen is typically discussed as an **additional preventive option** after initial diagnosis and counseling, not as the immediate next step.
- **Breast irradiation** is not indicated for LCIS, as it is non-invasive and does not require local radiation treatment, making this combination inappropriate.
Breast conservation therapy US Medical PG Question 4: A 56-year-old woman is referred to your office with mammography results showing a dense, spiculated mass with clustered microcalcifications. The family history is negative for breast, endometrial, and ovarian cancers. She was formerly a flight attendant and since retirement, she has started a strict Mediterranean diet because she was "trying to compensate for her lack of physical activity". She is the mother of two. She breastfed each infant for 18 months, as recommended by her previous physician. Her only two surgical procedures have been a breast augmentation with implants and tubal ligation. The physical examination is unremarkable. There are no palpable masses and no nipple or breast skin abnormalities. The patient lacks a family history of breast cancer. Which of the following is the most significant risk factor for the development of breast cancer in this patient?
- A. Breast implants
- B. Sedentarism
- C. Age >50 years
- D. Nulliparity
- E. Occupation (Correct Answer)
Breast conservation therapy Explanation: ***Occupation***
- Historically, **flight attendants** have a higher risk of breast cancer due to increased exposure to **ionizing radiation** at high altitudes and circadian rhythm disruption.
- This chronic exposure to known carcinogens makes it a more significant risk factor compared to general lifestyle or age for this specific patient.
*Breast implants*
- **Breast implants** are not associated with an increased risk of breast cancer, although they can sometimes make mammographic interpretation more challenging.
- While there's a rare association with **anaplastic large cell lymphoma (ALCL)**, it's not breast cancer.
*Sedentarism*
- While a **sedentary lifestyle** is a general risk factor for various cancers, including breast cancer, it is a less specific and potent risk compared to direct occupational exposure to radiation.
- Her recent adoption of a Mediterranean diet to compensate suggests it might not be a lifelong, primary risk factor in this context.
*Age >50 years*
- **Increasing age** is a well-established, non-modifiable risk factor for breast cancer, with incidence rising significantly after age 50.
- However, for this patient, the **occupational exposure** is a more specific and potent risk given her profession, placing it above general age-related risk.
*Nulliparity*
- **Nulliparity** (never having given birth) is a risk factor for breast cancer, as pregnancy and breastfeeding offer some protective effects.
- This patient is a mother of two and breastfed both infants, indicating she is **not nulliparous** and has likely mitigated this risk factor.
Breast conservation therapy US Medical PG Question 5: Patient 1 – A 26-year-old woman presents to her primary care physician for an annual exam. She currently does not have any acute concerns and says her health has been generally well. Medical history is significant for asthma, which is managed with an albuterol inhaler. Her last pap smear was unremarkable. She is currently sexually active with one male and consistently uses condoms. She occasionally smokes marijuana and drinks wine once per week. Her mother recently passed away from advanced ovarian cancer. Her sister is 37-years-old and was recently diagnosed with breast cancer and ovarian cancer. Physical examination is remarkable for a mildly anxious woman.
Patient 2 – A 27-year-old woman presents to her primary care physician for an annual exam. She says that she would like to be screened for breast cancer since two of her close friends were recently diagnosed. She noticed she has a small and mobile mass on her left breast, which increases in size and becomes tender around her time of menses. Family history is remarkable for hypertension in the father. The physical exam is significant for a small, well-defined, and mobile mass on her left breast that is not tender to palpation.
Which of the following is the best next step in management for patient 1 and 2?
- A. Patient 1 – Breast ultrasound. Patient 2 – Return in 3 months for a clinical breast exam
- B. Patient 1 – Reassurance. Patient 2 – Breast ultrasound
- C. Patient 1 – CA-125 testing. Patient 2 – BRCA testing
- D. Patient 1 – BRCA testing. Patient 2 – Breast ultrasound (Correct Answer)
- E. Patient 1 – Breast and ovarian ultrasound. Patient 2 – Mammography
Breast conservation therapy Explanation: ***Patient 1 – BRCA testing. Patient 2 – Breast ultrasound***
- Patient 1 has a strong family history of early-onset **breast and ovarian cancer** (**mother and sister**), suggesting a high probability of an inherited genetic mutation, such as **BRCA1/2**, which warrants genetic testing.
- Patient 2 presents with a **small, mobile, well-defined breast mass** that is likely benign, and a **breast ultrasound** is the appropriate initial imaging for further characterization in a young woman.
*Patient 1 – Breast ultrasound. Patient 2 – Return in 3 months for a clinical breast exam*
- Patient 1's primary concern is genetic predisposition due to family history, an **ultrasound** is not the initial or primary screening method for future cancer risk.
- Patient 2 has a palpable mass; waiting 3 months for a **clinical breast exam** without initial imaging (ultrasound) is not appropriate for evaluating a new breast lump.
*Patient 1 – Reassurance. Patient 2 – Breast ultrasound*
- Patient 1's family history of **early-onset breast and ovarian cancer** is a significant risk factor; therefore, simple **reassurance** without further investigation is inappropriate.
- While a **breast ultrasound** is appropriate for Patient 2, the recommendation for Patient 1 is incorrect.
*Patient 1 – CA-125 testing. Patient 2 – BRCA testing*
- **CA-125** is a tumor marker primarily used for monitoring ovarian cancer treatment or recurrence, not for initial screening in asymptomatic individuals, especially in a young woman with no active symptoms.
- **BRCA testing** is indicated for Patient 1 due to family history, but not for Patient 2 who has a likely benign breast mass and no significant family history.
*Patient 1 – Breast and ovarian ultrasound. Patient 2 – Mammography*
- Regular **breast and ovarian ultrasounds** are not recommended as primary screening tools for genetic risk in asymptomatic high-risk individuals like Patient 1.
- **Mammography** is less sensitive in young women (under 30) due to higher breast tissue density, making **ultrasound** the preferred initial imaging for Patient 2.
Breast conservation therapy US Medical PG Question 6: A 40-year-old man presents with a painless firm mass in the right breast. Examination shows retraction of the nipple and the skin is fixed to the underlying mass. The axillary nodes are palpable. Which of the following statements is FALSE regarding the above condition?
- A. Lobular cancer is the most common breast cancer in males (Correct Answer)
- B. BRCA2 mutations are associated with increased risk
- C. These are positive for estrogen receptor
- D. Endocrine therapy plays an important role in treatment
- E. Gynecomastia may be caused by certain medications
Breast conservation therapy Explanation: ***Lobular cancer is the most common breast cancer in males***
- This statement is **FALSE** and is the correct answer. The most common type of breast cancer in males is **invasive ductal carcinoma (IDC)**, accounting for about 80-90% of cases.
- **Invasive lobular carcinoma** is rare in men because men have very few lobules in their breast tissue.
*Gynecomastia may be caused by certain medications*
- This statement is **TRUE**. Medications such as spironolactone, cimetidine, finasteride, antipsychotics, and anabolic steroids can cause gynecomastia.
- However, the clinical presentation described (firm mass, nipple retraction, skin fixation, axillary nodes) is consistent with **malignancy**, not gynecomastia.
*BRCA2 mutations are associated with increased risk*
- This statement is **TRUE**. Male breast cancer is strongly associated with **BRCA2 mutations** (and less commonly BRCA1), which are hereditary.
- Men with BRCA2 mutations have a 5-10% lifetime risk of developing breast cancer, compared to less than 0.1% in the general male population.
*These are positive for estrogen receptor*
- This statement is **TRUE**. A vast majority (over 90%) of male breast cancers are **estrogen receptor (ER) positive**, which makes them responsive to endocrine therapy.
- This high rate of ER positivity is even greater than in female breast cancers.
*Endocrine therapy plays an important role in treatment*
- This statement is **TRUE**. Given the high prevalence of ER positivity (over 90%), endocrine therapy such as **tamoxifen** or aromatase inhibitors is a cornerstone of treatment for male breast cancer.
- Endocrine therapy is used in both adjuvant and metastatic settings for hormone receptor-positive disease.
Breast conservation therapy US Medical PG Question 7: A 47-year-old woman comes to the physician for a mass in her left breast she noticed 2 days ago during breast self-examination. She has hypothyroidism treated with levothyroxine. There is no family history of breast cancer. Examination shows large, moderately ptotic breasts. The mass in her left breast is small (approximately 1 cm x 0.5 cm), firm, mobile, and painless. It is located 4 cm from her nipple-areolar complex at the 7 o'clock position. There are no changes in the skin or nipple, and there is no palpable axillary adenopathy. No masses are palpable in her right breast. A urine pregnancy test is negative. Mammogram showed a soft tissue mass with poorly defined margins. Core needle biopsy confirms a low-grade infiltrating ductal carcinoma. The pathological specimen is positive for estrogen receptors and negative for progesterone and human epidermal growth factor receptor 2 (HER2) receptors. Staging shows no distant metastatic disease. Which of the following is the most appropriate next step in management?
- A. Lumpectomy with sentinel lymph node biopsy followed by hormone therapy
- B. Nipple-sparing mastectomy with axillary lymph node dissection followed by hormone therapy
- C. Nipple-sparing mastectomy with axillary lymph node dissection, followed by radiation and hormone therapy
- D. Radical mastectomy followed by hormone therapy
- E. Lumpectomy with sentinel lymph node biopsy, followed by radiation and hormone therapy (Correct Answer)
Breast conservation therapy Explanation: **Lumpectomy with sentinel lymph node biopsy, followed by radiation and hormone therapy**
- The patient has **early-stage (T1N0M0) estrogen receptor (ER)-positive, HER2-negative invasive ductal carcinoma** suitable for **breast-conserving surgery (lumpectomy)**.
- **Lumpectomy** must be followed by **radiation therapy** to the remaining breast tissue to reduce the risk of local recurrence, and **endocrine therapy** (due to ER positivity) is indicated to reduce systemic recurrence risk.
- **Sentinel lymph node biopsy** is performed to stage the axilla; if positive, an axillary lymph node dissection may be indicated. However, in this case, the mass is small, and there is no palpable axillary adenopathy, making sentinel lymph node biopsy the appropriate initial step.
*Lumpectomy with sentinel lymph node biopsy followed by hormone therapy*
- While **lumpectomy with sentinel lymph node biopsy** and **hormone therapy** are part of the appropriate management, **radiation therapy** to the conserved breast is a critical component that is missing from this option.
- Omitting **radiation therapy** after lumpectomy for invasive breast cancer significantly increases the risk of local recurrence.
*Nipple-sparing mastectomy with axillary lymph node dissection followed by hormone therapy*
- A **nipple-sparing mastectomy** is a more aggressive surgical approach than typically required for a **small, early-stage tumor** like this, which is amenable to breast-conserving surgery.
- **Axillary lymph node dissection** is usually reserved for cases with clinically positive lymph nodes or a positive sentinel lymph node biopsy, not as an initial step when there is no palpable axillary adenopathy.
*Nipple-sparing mastectomy with axillary lymph node dissection, followed by radiation and hormone therapy*
- This option involves an **unnecessarily extensive surgical procedure (nipple-sparing mastectomy with axillary lymph node dissection)** for a **small (1cm x 0.5cm) early-stage tumor** that can be managed with breast-conserving therapy.
- While radiation and hormone therapy are relevant, the initial surgical choice is too aggressive given the clinical presentation.
*Radical mastectomy followed by hormone therapy*
- **Radical mastectomy** (which includes removal of the breast, underlying chest muscle, and axillary lymph nodes) is rarely performed today due to its significant morbidity and is not indicated for this **early-stage tumor**.
- **Modified radical mastectomy**, which removes the breast and axillary lymph nodes while preserving the chest muscle, is typically only considered if breast-conserving surgery is not feasible or desired, and **hormone therapy** would be indicated, but **radiation** may also be needed depending on other factors.
Breast conservation therapy US Medical PG Question 8: A 50-year-old woman presents to the outpatient clinic because of a swollen and enlarged right breast. Clinical examination shows no evidence of mass or axillary lymphadenopathy. There is no history of trauma or inflammation. Her past medical and surgical history is positive for breast augmentation with a textured implant 15 years ago. Magnetic resonance imaging (MRI) shows an accumulation of fluid around the right breast implant with intact implant integrity. Which of the following is the most appropriate next step in the management?
- A. Chemotherapy
- B. Mastectomy
- C. Surgical replacement of textured implant with a smooth implant
- D. Mammogram
- E. Cytological analysis for CD30 and ALK (Correct Answer)
Breast conservation therapy Explanation: ***Cytological analysis for CD30 and ALK***
- The presentation of a **swollen and enlarged breast** with an **accumulation of fluid around a textured breast implant**, particularly 15 years after implantation, is highly suggestive of **Breast Implant-Associated Anaplastic Large Cell Lymphoma (BIA-ALCL)**.
- **Cytological analysis of the periprosthetic fluid** for **CD30** (a surface marker expressed by BIA-ALCL cells) and **ALK** (typically negative in BIA-ALCL) is crucial for diagnosis.
*Chemotherapy*
- This is a treatment, not a diagnostic step, and is not the initial appropriate action for a suspected periprosthetic fluid accumulation without a definitive diagnosis.
- The specific type of chemotherapy would also depend on the confirmed diagnosis and staging of the lymphoma, if present.
*Mastectomy*
- While mastectomy might be part of the treatment for advanced BIA-ALCL, it is an aggressive surgical intervention and not the initial diagnostic step in this scenario.
- A definitive diagnosis is required before considering such a radical procedure.
*Surgical replacement of textured implant with a smooth implant*
- This option addresses the implant itself but does not diagnose or treat the underlying cause of the fluid accumulation, especially if it is indeed BIA-ALCL.
- Surgical intervention might be part of the treatment, but only after a diagnosis is confirmed.
*Mammogram*
- A mammogram is primarily used to detect breast masses and calcifications indicative of breast cancer, not typically for evaluating periprosthetic fluid or lymphoma.
- While imaging is useful, an MRI has already been performed, and the key diagnostic step now is to analyze the fluid.
Breast conservation therapy US Medical PG Question 9: A 50-year-old obese woman presents for a follow-up appointment regarding microcalcifications found in her left breast on a recent screening mammogram. The patient denies any recent associated symptoms. The past medical history is significant for polycystic ovarian syndrome (PCOS), for which she takes metformin. Her menarche occurred at age 11, and the patient still has regular menstrual cycles. The family history is significant for breast cancer in her mother at the age of 72. The review of systems is notable for a 6.8 kg (15 lb) weight loss in the past 2 months. The vital signs include: temperature 37.0°C (98.6°F), blood pressure 130/70 mm Hg, pulse 82/min, respiratory rate 17/min, and oxygen saturation 98% on room air. On physical examination, the patient is alert and cooperative. The breast examination reveals no palpable masses, lymphadenopathy, or evidence of skin retraction. A biopsy of the left breast is performed, and histologic examination demonstrates evidence of non-invasive malignancy. Which of the following is the most appropriate definitive treatment for this patient?
- A. Tamoxifen
- B. Observation with bilateral mammograms every 6 months
- C. Lumpectomy (Correct Answer)
- D. Radiotherapy
- E. Bilateral mastectomy
Breast conservation therapy Explanation: ***Lumpectomy***
- This patient has **non-invasive malignancy**, likely **ductal carcinoma in situ (DCIS)**, identified through microcalcifications and confirmed by excisional biopsy. For DCIS without gross invasion, the primary treatment is **surgical excision**, often a lumpectomy.
- A lumpectomy, also known as **breast-conserving surgery**, aims to remove the cancerous tissue with a margin of healthy tissue while preserving the rest of the breast.
*Tamoxifen*
- **Tamoxifen** is an **estrogen receptor modulator** used as **adjuvant therapy** for hormone-receptor-positive breast cancer, primarily after surgical removal of the tumor. It is not a primary treatment for removing the malignancy itself.
- While it might be considered after surgery depending on receptor status, it does not address the need for initial excision of the non-invasive malignancy.
*Observation with bilateral mammograms every 6 months*
- **Observation** is insufficient for confirmed non-invasive malignancy, which carries a risk of progression if untreated. **Active intervention** is required once malignancy is histologically confirmed.
- This approach might be considered for high-risk lesions or atypical hyperplasia, but not for confirmed carcinoma in situ.
*Radiotherapy*
- **Radiotherapy** is often used as **adjuvant therapy** after lumpectomy for DCIS to reduce the risk of local recurrence. It is not a standalone primary treatment for removing the initial non-invasive malignancy.
- The first step is always surgical removal of the cancerous tissue.
*Bilateral mastectomy*
- **Bilateral mastectomy** is a more aggressive surgical intervention, typically reserved for **invasive breast cancer**, widespread DCIS, or cases with very high genetic risk (e.g., BRCA mutations).
- For localized non-invasive malignancy identified through microcalcifications, a lumpectomy is generally the **most appropriate and less invasive initial surgical approach**.
Breast conservation therapy US Medical PG Question 10: A 56-year-old woman comes to the physician because she palpated a mass in her right breast during self-examination a week ago. Menarche was at the age of 14, and her last menstrual period was at the age of 51. Vital signs are within normal limits. Examination shows a nontender, firm and hard mass in the upper outer quadrant of the right breast. Mammography shows large, dense breasts, with a 1.7-cm mass in the right upper outer quadrant. The patient undergoes right upper outer quadrant lumpectomy with subsequent sentinel node biopsy, which reveals moderately differentiated invasive ductal carcinoma and micrometastasis to one axillary lymph node. There is no evidence of extranodal metastasis. The tumor tests positive for both estrogen and progesterone receptors and does not show human epidermal growth factor receptor 2 (HER2) over-expression. Flow-cytometry reveals aneuploid tumor cells. Which of the following factors has the greatest effect on this patient's prognosis?
- A. Age
- B. Tumor size
- C. Hormone receptor status
- D. Nodal status (Correct Answer)
- E. HER2 receptor status
Breast conservation therapy Explanation: **Nodal status**
- The presence of **micrometastasis to one axillary lymph node** is the *most significant prognostic indicator* in this patient's case.
- **Lymph node involvement** signifies systemic spread and is the strongest predictor of recurrence and overall survival in breast cancer.
*Age*
- While **age** can influence treatment choices and comorbidity, it is generally *less impactful on long-term prognosis* than nodal status.
- Very young or very old age can sometimes be associated with more aggressive disease or worse outcomes, but it is not the primary determinant.
*Tumor size*
- The **tumor size of 1.7 cm** is a prognostic factor, with larger tumors generally having a worse prognosis.
- However, for this patient, the **presence of lymph node metastasis** is a more powerful indicator of systemic disease than the primary tumor size alone.
*Hormone receptor status*
- **Positive estrogen and progesterone receptors** indicate that the tumor is likely to respond to endocrine therapies.
- This is a *favorable prognostic factor* as it opens up additional treatment options, but it does not outweigh the negative impact of nodal involvement.
*HER2 receptor status*
- **Absence of HER2 overexpression** is a positive factor, as HER2-positive cancers are generally more aggressive and require targeted therapy.
- However, while HER2 status guides treatment, the presence of **lymph node metastasis** still holds greater weight in determining overall prognosis.
More Breast conservation therapy US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.