Breast cancer staging and surgical management US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Breast cancer staging and surgical management. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Breast cancer staging and surgical management US Medical PG Question 1: A 49-year-old woman presents to her physician with complaints of breast swelling and redness of the skin over her right breast for the past 1 month. She also mentions that the skin above her right breast appears to have thickened. She denies any pain or nipple discharge. The past medical history is significant for a total abdominal hysterectomy at 45 years of age. Her last mammogram 1 year ago was negative for any pathologic changes. On examination, the right breast was diffusely erythematous with gross edema and tenderness and appeared larger than the left breast. The right nipple was retracted and the right breast was warmer than the left breast. No localized mass was palpated. Which of the following statements best describes the patient’s most likely condition?
- A. It shows predominant lymphatic spread.
- B. The lesion expresses receptors for estrogen and progesterone.
- C. The lesion is due to Streptococcal infection.
- D. It is a benign lesion.
- E. The inflammation is due to obstruction of dermal lymphatic vessels. (Correct Answer)
Breast cancer staging and surgical management Explanation: ***The inflammation is due to obstruction of dermal lymphatic vessels.***
- The presentation of **rapid-onset breast swelling, redness, thickening of the skin, warmth, and nipple retraction** without a palpable mass is highly suggestive of **inflammatory breast cancer (IBC)**.
- IBC is characterized by the **obstruction of dermal lymphatic vessels by tumor cells**, leading to the classic inflammatory signs and **peau d'orange** appearance.
*It shows predominant lymphatic spread.*
- While IBC does involve **lymphatic spread**, this statement alone does not fully encompass the characteristic pathology of the condition causing the observed symptoms.
- The obstruction of the **dermal lymphatic vessels** is a more precise description of the immediate cause of the clinical presentation.
*The lesion expresses receptors for estrogen and progesterone.*
- Although some breast cancers are **hormone receptor-positive (ER/PR positive)**, there is no direct information in the vignette to suggest this specificity for the patient's condition.
- This statement refers to a **molecular characteristic** that is not a defining feature of the clinical presentation of IBC.
*The lesion is due to Streptococcal infection.*
- While a **bacterial infection** (like **streptococcal cellulitis**) can cause redness, swelling, and warmth, it typically presents with more acute symptoms, fever, and often a clearer response to antibiotics.
- The **thickening of the skin** and **nipple retraction** point away from a simple infection and towards a malignant process.
*It is a benign lesion.*
- The rapid progression of symptoms, pronounced skin changes, and nipple retraction are all **red flags for malignancy**, specifically inflammatory breast cancer.
- **Benign lesions** rarely cause such diffuse, severe, and rapidly progressing inflammatory signs.
Breast cancer staging and surgical management US Medical PG Question 2: The patient undergoes a mammogram, which shows a 6.5mm sized mass with an irregular border and spiculated margins. A subsequent core needle biopsy of the mass shows infiltrating ductal carcinoma with HER2-positive, estrogen-negative, and progesterone-negative immunohistochemistry staining. Blood counts and liver function tests are normal. Laboratory studies show:
Hemoglobin 12.5 g/dL
Serum
Na+ 140 mEq/L
Cl- 103 mEq/L
K+ 4.2 mEq/L
HCO3- 26 mEq/L
Ca2+ 8.9 mg/dL
Urea Nitrogen 12 mg/dL
Glucose 110 mg/dL
Alkaline Phosphatase 25 U/L
Alanine aminotransferase (ALT) 15 U/L
Aspartate aminotransferase (AST) 13 U/L
Which of the following is the most appropriate next step in management?
- A. Breast-conserving therapy and sentinel lymph node biopsy (Correct Answer)
- B. Bilateral mastectomy with lymph node dissection
- C. Trastuzumab therapy
- D. Bone scan
- E. Whole-body PET/CT
Breast cancer staging and surgical management Explanation: ***Breast-conserving therapy and sentinel lymph node biopsy***
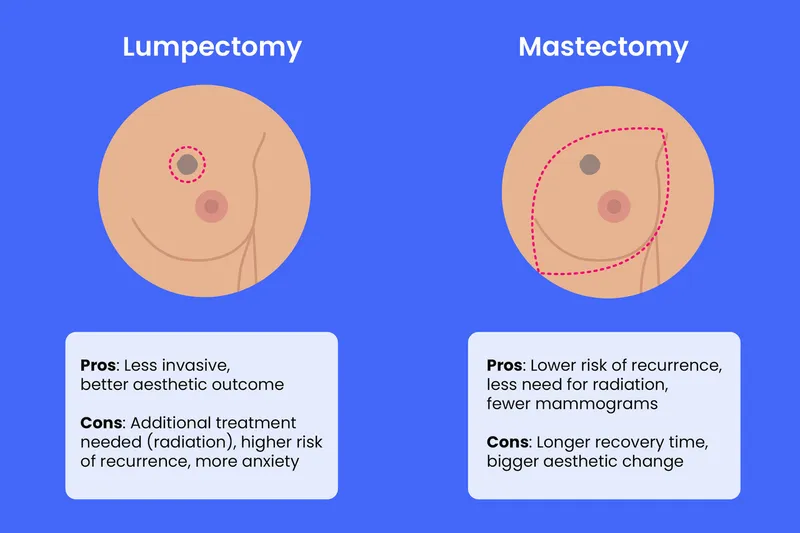
- The patient has **early-stage (T1) breast cancer** (6.5mm mass), which is amenable to **breast-conserving therapy (lumpectomy)** as the primary surgical approach.
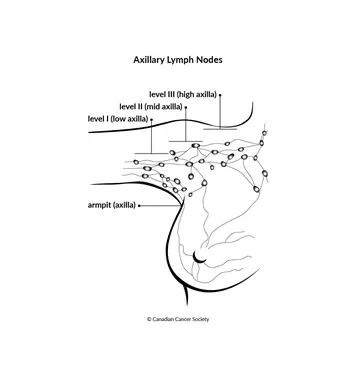
- A **sentinel lymph node biopsy** is essential to determine nodal status and guide further staging and adjuvant therapy, as the tumor size does not preclude nodal involvement.
*Bilateral mastectomy with lymph node dissection*
- This is an **overly aggressive surgical approach** for a small, unifocal tumor without evidence of multifocality or significant risk factors for recurrence in the contralateral breast.
- While **axillary lymph node dissection** may be indicated if the sentinel node is positive, it is not the initial preferred approach for all patients, especially with no current evidence of nodal metastasis.
*Trastuzumab therapy*
- **Trastuzumab** is a targeted therapy for **HER2-positive breast cancer**, but it is typically administered as **adjuvant therapy** (after surgery) or neoadjuvant therapy (before surgery).
- It is not the most appropriate *initial* next step before surgical management and comprehensive staging have been completed.
*Bone scan*
- A **bone scan** is used to detect **bone metastases**, but it is generally reserved for patients with **advanced-stage cancer** (e.g., T3/T4 tumor, N2/N3 nodes), symptoms suggestive of bony involvement, or significantly elevated alkaline phosphatase.
- Given the patient's small tumor size (6.5mm), normal labs, and lack of symptoms, a bone scan is not indicated as the *next* immediate step.
*Whole-body PET/CT*
- **Whole-body PET/CT** is primarily used for **staging advanced cancer** or investigating suspicious findings in symptomatic patients.
- For this small, early-stage breast cancer with no signs of distant metastasis indicated by normal blood tests, a PET/CT is **not recommended** as routine staging and carries unnecessary radiation exposure and cost.
Breast cancer staging and surgical management US Medical PG Question 3: A 42-year-old woman presents to the physician because of an abnormal breast biopsy report following suspicious findings on breast imaging. Other than being concerned about her report, she feels well. She has no history of any serious illnesses and takes no medications. She does not smoke. She consumes wine 1–2 times per week with dinner. There is no significant family history of breast or ovarian cancer. Vital signs are within normal limits. Physical examination shows no abnormal findings. The biopsy shows lobular carcinoma in situ (LCIS) in the left breast. Which of the following is the most appropriate next step in management?
- A. Careful observation + routine mammography (Correct Answer)
- B. Left mastectomy + axillary dissection + local irradiation
- C. Lumpectomy + routine screening
- D. Lumpectomy + breast irradiation
- E. Breast irradiation + tamoxifen
Breast cancer staging and surgical management Explanation: ***Careful observation + routine mammography***
- **Lobular carcinoma in situ (LCIS)** is considered a **non-obligate precursor** to invasive carcinoma, meaning it indicates an increased risk for developing invasive breast cancer in either breast (approximately 1-2% per year), but it is not itself invasive.
- Management typically involves **careful surveillance** with routine clinical exams and **mammography**, as this is the most appropriate initial approach for classic LCIS.
- Surgical excision is often unnecessary due to LCIS's diffuse nature and the fact that it serves as a risk marker rather than a direct precancerous lesion requiring removal.
*Left mastectomy + axillary dissection + local irradiation*
- This aggressive approach is reserved for **invasive breast cancer** and would be excessive for LCIS, which is a non-invasive lesion and a marker of increased risk rather than an immediate threat.
- **Axillary dissection** is performed to stage nodal involvement in invasive cancer, which is not applicable here as LCIS does not metastasize.
*Lumpectomy + routine screening*
- While a **lumpectomy (excision)** may be considered for **pleomorphic LCIS** or when there is diagnostic uncertainty, it is not the standard initial management for classic LCIS.
- Classic LCIS is often multifocal and bilateral, making localized excision less effective as a risk-reduction strategy.
*Lumpectomy + breast irradiation*
- **Radiation therapy** is typically used to reduce local recurrence risk after **lumpectomy for invasive breast cancer** or **ductal carcinoma in situ (DCIS)**.
- For LCIS, irradiation is generally not recommended as it is non-invasive and does not benefit from local radiation treatment.
*Breast irradiation + tamoxifen*
- **Tamoxifen** is a selective estrogen receptor modulator (SERM) that can be **offered for risk reduction** in women with LCIS, potentially reducing the risk of invasive breast cancer by approximately 50%.
- However, tamoxifen is typically discussed as an **additional preventive option** after initial diagnosis and counseling, not as the immediate next step.
- **Breast irradiation** is not indicated for LCIS, as it is non-invasive and does not require local radiation treatment, making this combination inappropriate.
Breast cancer staging and surgical management US Medical PG Question 4: A 40-year-old man presents with a painless firm mass in the right breast. Examination shows retraction of the nipple and the skin is fixed to the underlying mass. The axillary nodes are palpable. Which of the following statements is FALSE regarding the above condition?
- A. Lobular cancer is the most common breast cancer in males (Correct Answer)
- B. BRCA2 mutations are associated with increased risk
- C. These are positive for estrogen receptor
- D. Endocrine therapy plays an important role in treatment
- E. Gynecomastia may be caused by certain medications
Breast cancer staging and surgical management Explanation: ***Lobular cancer is the most common breast cancer in males***
- This statement is **FALSE** and is the correct answer. The most common type of breast cancer in males is **invasive ductal carcinoma (IDC)**, accounting for about 80-90% of cases.
- **Invasive lobular carcinoma** is rare in men because men have very few lobules in their breast tissue.
*Gynecomastia may be caused by certain medications*
- This statement is **TRUE**. Medications such as spironolactone, cimetidine, finasteride, antipsychotics, and anabolic steroids can cause gynecomastia.
- However, the clinical presentation described (firm mass, nipple retraction, skin fixation, axillary nodes) is consistent with **malignancy**, not gynecomastia.
*BRCA2 mutations are associated with increased risk*
- This statement is **TRUE**. Male breast cancer is strongly associated with **BRCA2 mutations** (and less commonly BRCA1), which are hereditary.
- Men with BRCA2 mutations have a 5-10% lifetime risk of developing breast cancer, compared to less than 0.1% in the general male population.
*These are positive for estrogen receptor*
- This statement is **TRUE**. A vast majority (over 90%) of male breast cancers are **estrogen receptor (ER) positive**, which makes them responsive to endocrine therapy.
- This high rate of ER positivity is even greater than in female breast cancers.
*Endocrine therapy plays an important role in treatment*
- This statement is **TRUE**. Given the high prevalence of ER positivity (over 90%), endocrine therapy such as **tamoxifen** or aromatase inhibitors is a cornerstone of treatment for male breast cancer.
- Endocrine therapy is used in both adjuvant and metastatic settings for hormone receptor-positive disease.
Breast cancer staging and surgical management US Medical PG Question 5: A 30-year-old woman presents to the office with complaints of pain in her right breast for 5 days. The pain is moderate-to-intense and is localized to the upper quadrant of the right breast, and mainly to the areola for the past 48 hours. She adds that there is some nipple discharge on the same side and that the right breast is red. She was diagnosed with type 1 diabetes at the age of 10 years of age, for which she takes insulin. The family history is negative for breast and ovarian cancers, and endometrial disorders. She smokes one-half pack of cigarettes every day and binge drinks alcohol on the weekends. Two weeks ago she was hit by a volleyball while playing at the beach. There is no history of fractures or surgical procedures. The physical examination reveals a swollen, erythematous, and warm right breast with periareolar tenderness and nipple discharge. There are no palpable masses or lymphadenopathy. Which of the following is the most important risk factor for the development of this patient’s condition?
- A. Age
- B. Trauma
- C. Diabetes
- D. Smoking (Correct Answer)
- E. Parity
Breast cancer staging and surgical management Explanation: ***Smoking***
- This patient presents with symptoms highly suggestive of **periductal mastitis**, including breast pain, erythema, tenderness, and nipple discharge, particularly around the periareolar region. **Smoking** is a significant and dose-dependent risk factor for periductal mastitis.
- The chemicals in cigarette smoke are thought to have a **toxic effect on the lactiferous ducts**, leading to inflammation and obstruction.
*Age*
- While age can influence breast conditions, periductal mastitis typically affects **younger and premenopausal women**, corresponding to this patient's age.
- Being 30 years old is not an independent risk factor for the development of periductal mastitis in the same way that smoking is; rather, it falls within the typical age range for the condition.
*Trauma*
- Although the patient sustained a volleyball injury, **trauma** to the breast itself is not a direct or significant risk factor for infectious or inflammatory conditions like periductal mastitis.
- Trauma is more likely to cause hematoma or fat necrosis, which would present differently from the described symptoms.
*Diabetes*
- **Diabetes** can increase the risk of infections in general due to impaired immune function, but it is not a specific or primary risk factor for periductal mastitis as defined by the inflammatory changes in the ducts.
- While diabetic patients may be prone to complications, there is no direct mechanistic link between diabetes and the development of this specific lobular mastitis.
*Parity*
- **Parity** (the number of times a woman has given birth) is largely irrelevant to the development of periductal mastitis in non-lactating women.
- Conditions related to parity often involve mastitis during lactation, which is not the case here, as this type of mastitis is an inflammatory condition of the ducts unrelated to breastfeeding.
Breast cancer staging and surgical management US Medical PG Question 6: A 39-year-old African American woman is admitted to the hospital following a seizure with a severe post-ictal headache. She was diagnosed with breast cancer 1 year ago when she presented with a hard, rock-like, immobile mass with irregular borders accompanied by changes in the breast skin, including erythema and dimpling. She had ipsilateral mobile axillary lymphadenopathy at that time. A biopsy confirmed the diagnosis of stage 2B invasive breast cancer. Her mother died at 42 years of age due to the same type of breast cancer. A CT scan done during this admission reveals multiple metastatic lesions in the brain and liver, along with the involvement of supra- and infra-clavicular lymph nodes. Which of the following molecular profile most likely characterizes this patient?
- A. PR, ER, HER2 positive
- B. HER2 positive
- C. Progesterone receptor (PR) positive
- D. ER, PR, HER2 negative (Correct Answer)
- E. Estrogen receptor (ER) positive
Breast cancer staging and surgical management Explanation: ***ER, PR, HER2 negative***
- This patient's presentation with aggressive breast cancer at a relatively young age (39 years old), family history of early-onset breast cancer, rapid progression to metastatic disease in the brain and liver, and involvement of multiple lymph nodes (axillary, supra- and infra-clavicular) are all highly suggestive of a **triple-negative breast cancer (TNBC)**.
- TNBC is characterized by the absence of **estrogen receptors (ER)**, **progesterone receptors (PR)**, and **human epidermal growth factor receptor 2 (HER2)** overexpression, making it an aggressive subtype with limited targeted treatment options and a poor prognosis, consistent with the patient's rapidly worsening condition.
*PR, ER, HER2 positive*
- This molecular profile (also known as triple-positive breast cancer) generally indicates a more favorable prognosis due to the availability of **hormonal therapy** (for ER/PR positivity) and **anti-HER2 targeted therapy**.
- The aggressive course and rapid metastatic spread described in the patient are less typical for triple-positive disease, which often responds well to various targeted treatments.
*HER2 positive*
- HER2-positive breast cancer can be aggressive, but the presence of HER2 positivity allows for **HER2-targeted therapies** (e.g., trastuzumab, pertuzumab), which significantly improve outcomes.
- While HER2-positive cancers can metastasize to the brain, the overall clinical picture, especially the aggressive growth and lack of other receptor expression, aligns more with triple-negative disease.
*Progesterone receptor (PR) positive*
- PR positivity, often alongside ER positivity, indicates a **hormone-sensitive breast cancer**, which typically has a better prognosis and is amenable to **endocrine therapy**.
- The aggressive and rapid metastatic progression to multiple sites, including brain and liver, is not characteristic of a purely PR-positive tumor without other aggressive features.
*Estrogen receptor (ER) positive*
- ER-positive breast cancer is the most common subtype and is generally associated with a **better prognosis** and responsiveness to **endocrine therapy**.
- The patient's aggressive disease course, including early metastasis and family history of early-onset, aggressive breast cancer, does not align with the typical presentation of an exclusively ER-positive tumor.
Breast cancer staging and surgical management US Medical PG Question 7: A 61-year-old woman presents to a surgical oncologist for consideration of surgical removal of biopsy-confirmed breast cancer. The mass is located in the tail of Spence along the superolateral aspect of the left breast extending into the axilla. The surgical oncologist determines that the optimal treatment for this patient involves radical mastectomy including removal of the axillary lymph nodes. The patient undergoes all appropriate preoperative tests and is cleared for surgery. During the operation, multiple enlarged axillary lymph nodes are present along the superolateral chest wall. While exposing the lymph nodes, the surgeon accidentally nicks a nerve. Which of the following physical examination findings will most likely be seen in this patient following the operation?
- A. Internal rotation, adduction, and extension of the arm
- B. Weakness in arm flexion at the elbow and numbness over the lateral forearm
- C. Weakness in shoulder abduction and numbness over the lateral shoulder
- D. Scapular protrusion while pressing against a wall (Correct Answer)
- E. Weakness in wrist extension and numbness over the dorsal hand
Breast cancer staging and surgical management Explanation: ***Scapular protrusion while pressing against a wall***
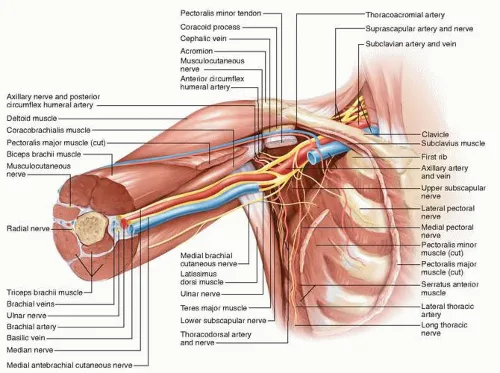
- Damage to the **long thoracic nerve** during axillary dissection (common in radical mastectomy) paralyzes the **serratus anterior muscle**.
- Paralysis of the serratus anterior causes **scapular winging** (protrusion) and inability to effectively protract the scapula, especially when pushing against a wall.
*Internal rotation, adduction, and extension of the arm*
- This constellation of findings, sometimes called **"policeman's tip"**, is characteristic of an **Erb's palsy**, involving the C5-C6 roots of the brachial plexus.
- Erb's palsy typically results from birth trauma or severe shoulder injury, not commonly from axillary lymph node dissection.
*Weakness in arm flexion at the elbow and numbness over the lateral forearm*
- This symptom complex indicates injury to the **musculocutaneous nerve**, affecting the biceps brachii and brachialis muscles and sensation to the lateral forearm.
- While theoretically possible in deep axillary dissection, it is less common than long thoracic nerve injury during routine axillary node removal.
*Weakness in shoulder abduction and numbness over the lateral shoulder*
- This presentation suggests damage to the **axillary nerve**, which innervates the deltoid and teres minor muscles and provides sensation over the "regimental badge" area of the shoulder.
- The axillary nerve is located more inferiorly and posteriorly in the axilla and is less prone to injury during standard anterior axillary lymph node dissection compared to the long thoracic nerve.
*Weakness in wrist extension and numbness over the dorsal hand*
- These are signs of **radial nerve injury**, which affects the extensor muscles of the wrist and fingers and sensation over the dorsal hand.
- The radial nerve runs more posteriorly in the axilla and arm, making it less susceptible to injury during an anterior axillary lymph node dissection.
Breast cancer staging and surgical management US Medical PG Question 8: A 45-year-old woman undergoes a modified radical mastectomy for breast cancer. Following the procedure, she experiences numbness in the medial aspect of her upper arm. Which of the following nerves was most likely injured during the surgery?
- A. Musculocutaneous nerve
- B. Thoracodorsal nerve
- C. Long thoracic nerve
- D. Intercostobrachial nerve (Correct Answer)
Breast cancer staging and surgical management Explanation: ***Intercostobrachial nerve***
- The **intercostobrachial nerve** provides sensory innervation to the **medial aspect of the upper arm** and is vulnerable to injury during **axillary dissection** in a modified radical mastectomy [1].
- Injury typically results in **numbness** or **paresthesia** in this specific dermatomal distribution [1].
*Musculocutaneous nerve*
- The **musculocutaneous nerve** innervates the muscles of the **anterior compartment of the arm** (e.g., biceps brachii) and provides sensation to the **lateral forearm**.
- Damage would primarily affect **forearm sensation** and arm flexion, not medial upper arm sensation.
*Thoracodorsal nerve*
- The **thoracodorsal nerve** innervates the **latissimus dorsi muscle**, a large muscle of the back and shoulder [1].
- Injury would lead to **weakness in adduction, extension, and internal rotation** of the arm, with no sensory deficit in the upper arm [1].
*Long thoracic nerve*
- The **long thoracic nerve** innervates the **serratus anterior muscle**, which stabilizes the scapula and allows for arm abduction above 90 degrees.
- Injury results in **"winged scapula,"** making it difficult to raise the arm overhead, without sensory loss in the upper arm.
Breast cancer staging and surgical management US Medical PG Question 9: A 47-year-old woman comes to the physician for a mass in her left breast she noticed 2 days ago during breast self-examination. She has hypothyroidism treated with levothyroxine. There is no family history of breast cancer. Examination shows large, moderately ptotic breasts. The mass in her left breast is small (approximately 1 cm x 0.5 cm), firm, mobile, and painless. It is located 4 cm from her nipple-areolar complex at the 7 o'clock position. There are no changes in the skin or nipple, and there is no palpable axillary adenopathy. No masses are palpable in her right breast. A urine pregnancy test is negative. Mammogram showed a soft tissue mass with poorly defined margins. Core needle biopsy confirms a low-grade infiltrating ductal carcinoma. The pathological specimen is positive for estrogen receptors and negative for progesterone and human epidermal growth factor receptor 2 (HER2) receptors. Staging shows no distant metastatic disease. Which of the following is the most appropriate next step in management?
- A. Lumpectomy with sentinel lymph node biopsy followed by hormone therapy
- B. Nipple-sparing mastectomy with axillary lymph node dissection followed by hormone therapy
- C. Nipple-sparing mastectomy with axillary lymph node dissection, followed by radiation and hormone therapy
- D. Radical mastectomy followed by hormone therapy
- E. Lumpectomy with sentinel lymph node biopsy, followed by radiation and hormone therapy (Correct Answer)
Breast cancer staging and surgical management Explanation: **Lumpectomy with sentinel lymph node biopsy, followed by radiation and hormone therapy**
- The patient has **early-stage (T1N0M0) estrogen receptor (ER)-positive, HER2-negative invasive ductal carcinoma** suitable for **breast-conserving surgery (lumpectomy)**.
- **Lumpectomy** must be followed by **radiation therapy** to the remaining breast tissue to reduce the risk of local recurrence, and **endocrine therapy** (due to ER positivity) is indicated to reduce systemic recurrence risk.
- **Sentinel lymph node biopsy** is performed to stage the axilla; if positive, an axillary lymph node dissection may be indicated. However, in this case, the mass is small, and there is no palpable axillary adenopathy, making sentinel lymph node biopsy the appropriate initial step.
*Lumpectomy with sentinel lymph node biopsy followed by hormone therapy*
- While **lumpectomy with sentinel lymph node biopsy** and **hormone therapy** are part of the appropriate management, **radiation therapy** to the conserved breast is a critical component that is missing from this option.
- Omitting **radiation therapy** after lumpectomy for invasive breast cancer significantly increases the risk of local recurrence.
*Nipple-sparing mastectomy with axillary lymph node dissection followed by hormone therapy*
- A **nipple-sparing mastectomy** is a more aggressive surgical approach than typically required for a **small, early-stage tumor** like this, which is amenable to breast-conserving surgery.
- **Axillary lymph node dissection** is usually reserved for cases with clinically positive lymph nodes or a positive sentinel lymph node biopsy, not as an initial step when there is no palpable axillary adenopathy.
*Nipple-sparing mastectomy with axillary lymph node dissection, followed by radiation and hormone therapy*
- This option involves an **unnecessarily extensive surgical procedure (nipple-sparing mastectomy with axillary lymph node dissection)** for a **small (1cm x 0.5cm) early-stage tumor** that can be managed with breast-conserving therapy.
- While radiation and hormone therapy are relevant, the initial surgical choice is too aggressive given the clinical presentation.
*Radical mastectomy followed by hormone therapy*
- **Radical mastectomy** (which includes removal of the breast, underlying chest muscle, and axillary lymph nodes) is rarely performed today due to its significant morbidity and is not indicated for this **early-stage tumor**.
- **Modified radical mastectomy**, which removes the breast and axillary lymph nodes while preserving the chest muscle, is typically only considered if breast-conserving surgery is not feasible or desired, and **hormone therapy** would be indicated, but **radiation** may also be needed depending on other factors.
Breast cancer staging and surgical management US Medical PG Question 10: A 56-year-old woman comes to the physician because she palpated a mass in her right breast during self-examination a week ago. Menarche was at the age of 14, and her last menstrual period was at the age of 51. Vital signs are within normal limits. Examination shows a nontender, firm and hard mass in the upper outer quadrant of the right breast. Mammography shows large, dense breasts, with a 1.7-cm mass in the right upper outer quadrant. The patient undergoes right upper outer quadrant lumpectomy with subsequent sentinel node biopsy, which reveals moderately differentiated invasive ductal carcinoma and micrometastasis to one axillary lymph node. There is no evidence of extranodal metastasis. The tumor tests positive for both estrogen and progesterone receptors and does not show human epidermal growth factor receptor 2 (HER2) over-expression. Flow-cytometry reveals aneuploid tumor cells. Which of the following factors has the greatest effect on this patient's prognosis?
- A. Age
- B. Tumor size
- C. Hormone receptor status
- D. Nodal status (Correct Answer)
- E. HER2 receptor status
Breast cancer staging and surgical management Explanation: **Nodal status**
- The presence of **micrometastasis to one axillary lymph node** is the *most significant prognostic indicator* in this patient's case.
- **Lymph node involvement** signifies systemic spread and is the strongest predictor of recurrence and overall survival in breast cancer.
*Age*
- While **age** can influence treatment choices and comorbidity, it is generally *less impactful on long-term prognosis* than nodal status.
- Very young or very old age can sometimes be associated with more aggressive disease or worse outcomes, but it is not the primary determinant.
*Tumor size*
- The **tumor size of 1.7 cm** is a prognostic factor, with larger tumors generally having a worse prognosis.
- However, for this patient, the **presence of lymph node metastasis** is a more powerful indicator of systemic disease than the primary tumor size alone.
*Hormone receptor status*
- **Positive estrogen and progesterone receptors** indicate that the tumor is likely to respond to endocrine therapies.
- This is a *favorable prognostic factor* as it opens up additional treatment options, but it does not outweigh the negative impact of nodal involvement.
*HER2 receptor status*
- **Absence of HER2 overexpression** is a positive factor, as HER2-positive cancers are generally more aggressive and require targeted therapy.
- However, while HER2 status guides treatment, the presence of **lymph node metastasis** still holds greater weight in determining overall prognosis.
More Breast cancer staging and surgical management US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.