Breast biopsy techniques US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Breast biopsy techniques. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Breast biopsy techniques US Medical PG Question 1: A 32-year-old woman, gravida 2, para 2, comes to the physician for the evaluation of a palpable mass in her right breast that she first noticed 1 week ago. She has no associated pain. She has never had a mammogram previously. She has type II diabetes mellitus treated with metformin. She has no family history of breast cancer. She has smoked half a pack of cigarettes daily for 15 years. Her temperature is 37°C (98.6°F), pulse is 78/min, respirations are 14/min, and blood pressure is 125/75 mm Hg. Examination shows a firm, nonpainful, nonmobile mass in the right upper quadrant of the breast. There is no nipple discharge. Examination of the skin and lymph nodes shows no abnormalities. No masses are palpated in the left breast. Which of the following is the most appropriate next step in the management of this patient?
- A. MRI scan of the breast
- B. Core needle biopsy
- C. Monthly self-breast exams
- D. Breast ultrasound (Correct Answer)
- E. BRCA gene testing
Breast biopsy techniques Explanation: ***Breast ultrasound***
- In women under 40, **breast tissue is often dense**, making mammography less effective, hence ultrasound is the initial imaging modality of choice for characterising breast masses.
- Ultrasound can differentiate well between **solid and cystic masses**, providing crucial information for further management irrespective of the character of the mass.
*MRI scan of the breast*
- **MRI is typically reserved for high-risk screening** or for further evaluation after abnormal mammogram/ultrasound findings, not as a primary diagnostic tool for an initial palpable mass in a low-risk patient.
- It has a high sensitivity but can also have a **high false-positive rate**, leading to unnecessary biopsies.
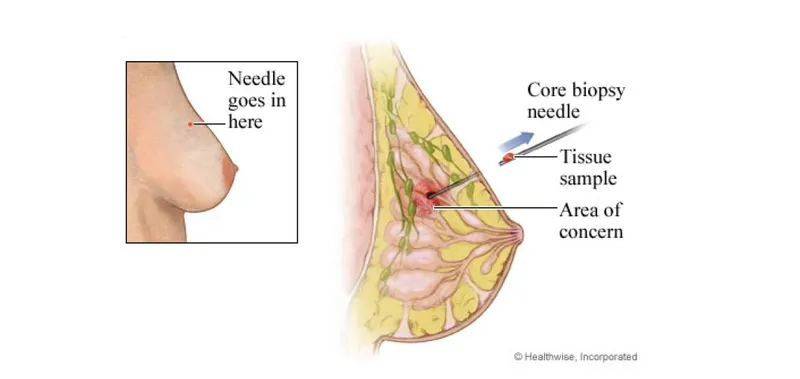
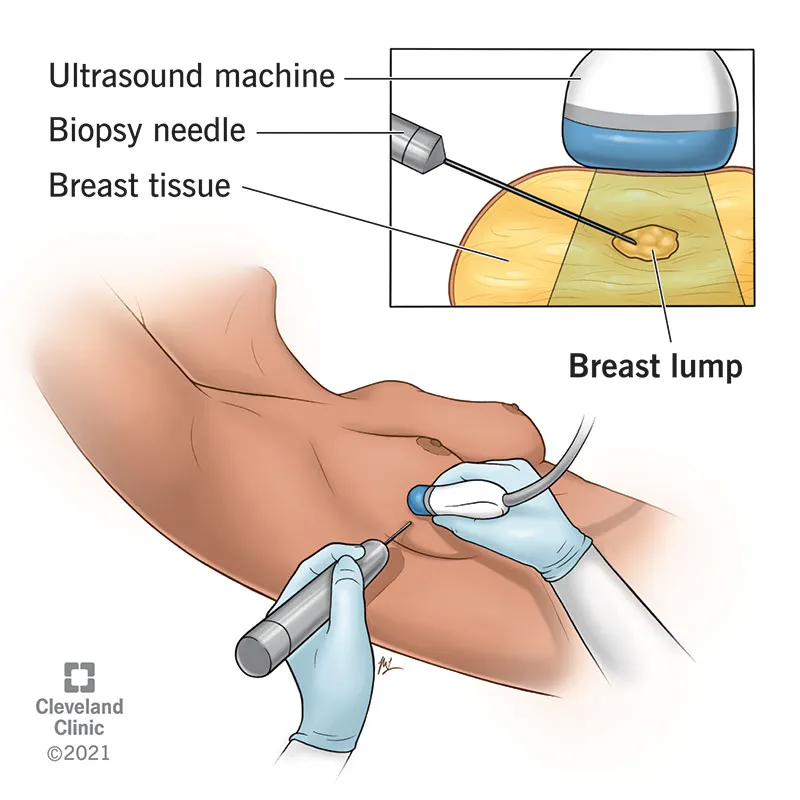
*Core needle biopsy*
- A biopsy is the **definitive diagnostic step** for characterizing a solid mass, but imaging, like an ultrasound, is usually performed *first* to determine the nature of the mass (solid vs. cystic) and to guide the biopsy.
- Direct biopsy without prior imaging might be less accurate if the mass is cystic or not well-localized.
*Monthly self-breast exams*
- While **self-breast exams** are encouraged for breast awareness, they are **not a diagnostic tool** for evaluating a new, palpable, non-regressing mass.
- A new, palpable mass requires immediate medical evaluation and diagnostic imaging rather than simply monitoring.
*BRCA gene testing*
- **BRCA testing** is indicated for individuals with a **strong family history of breast or ovarian cancer**, early-onset cancers, or other specific genetic predispositions.
- This patient has no reported family history of breast cancer and no other high-risk features to warrant genetic testing at this initial stage.
Breast biopsy techniques US Medical PG Question 2: A 44-year-old woman presents for her annual physical checkup. She says she first noticed a mass in her right breast while taking a shower 3 months ago, which has progressively increased in size. She denies any weight loss, fever, night sweats, discharge from or change in her nipples. Her family history is negative for breast, ovarian, and endometrial cancer. She is afebrile, and her vital signs are within normal limits. Physical examination reveals a smooth, multinodular, firm 5 cm x 5 cm mass in the right breast that is mobile and painless. The skin over the mass appears to be stretched and shiny without ulcerations, erythema, or vascular demarcation. On follow-up 6 weeks later, an interval ultrasound of the right breast reveals a well-circumscribed hypoechoic mass with some cystic components that now measures 8 cm x 7 cm. A core needle biopsy of the mass is performed. Which of the following diagnosis is most likely expected to be confirmed by the core needle biopsy in this patient?
- A. Fibroadenoma
- B. Breast abscess
- C. Fat necrosis
- D. Duct ectasia
- E. Phyllodes tumor (Correct Answer)
Breast biopsy techniques Explanation: ***Phyllodes tumor***
* The clinical presentation of a rapidly growing, large, **mobile, firm, and painless breast mass** in a middle-aged woman is highly suggestive of a phyllodes tumor.
* Ultrasound findings of a **well-circumscribed hypoechoic mass with cystic components** are also characteristic, as is the significant interval increase in size.
*Fibroadenoma*
* While fibroadenomas are typically **mobile and painless**, they usually grow more slowly and rarely reach the large size (8 cm) observed in this patient.
* Significant rapid growth and a multinodular appearance make fibroadenoma less likely, although phyllodes tumors can sometimes be mistaken for fibroadenomas on initial imaging.
*Breast abscess*
* A breast abscess typically presents with signs of **inflammation, pain, redness, warmth, and possibly fever**, which are absent in this case.
* Ultrasound would show a fluid-filled collection with internal debris, often with surrounding inflammatory changes.
*Fat necrosis*
* Fat necrosis usually occurs after **trauma or surgery** to the breast and often presents as a firm, fixed mass that can mimic malignancy.
* The absence of trauma history and the rapid, significant growth are inconsistent with fat necrosis.
*Duct ectasia*
* Duct ectasia commonly causes **nipple discharge**, subareolar masses, and sometimes nipple retraction.
* The patient denies nipple discharge, and the mass characteristics do not align with typical duct ectasia.
Breast biopsy techniques US Medical PG Question 3: A 29-year-old woman, gravida 1, para 1, comes to the physician for the evaluation of a painful mass in her left breast for several days. She has no fevers or chills. She has not noticed any changes in the right breast. She has no history of serious illness. Her last menstrual period was 3 weeks ago. She appears anxious. Her temperature is 37°C (98.6°F), pulse is 80/min, respirations are 13/min, and blood pressure is 130/75 mm Hg. Examination shows a palpable, mobile, tender mass in the left upper quadrant of the breast. Ultrasound shows a 1.75-cm, well-circumscribed anechoic mass with posterior acoustic enhancement. The patient says that she is very concerned that she may have breast cancer and wishes further diagnostic testing. Which of the following is the most appropriate next step in the management of this patient?
- A. Core needle biopsy
- B. MRI scan of the left breast
- C. Reassurance and clinical follow-up
- D. Fine needle aspiration (Correct Answer)
- E. Mammogram
Breast biopsy techniques Explanation: ***Fine needle aspiration***
- This patient presents with a **palpable, mobile, tender mass** in the breast, and ultrasound reveals a **well-circumscribed anechoic mass with posterior acoustic enhancement**, which is highly suggestive of a **simple cyst**.
- **Fine needle aspiration** is the most appropriate next step for a symptomatic simple cyst; it can be both diagnostic and therapeutic, relieving patient anxiety and pain.
*Core needle biopsy*
- **Core needle biopsy** is typically reserved for lesions that are suspicious for malignancy, such as solid masses with **irregular margins** or **architectural distortion**, which are not present in this case.
- Performing a core needle biopsy on a likely simple cyst is excessively invasive and carries risks like bleeding and infection without clear indication.
*MRI scan of the left breast*
- An **MRI scan** is generally used for screening high-risk patients, evaluating the extent of known cancer, or further characterizing complex lesions not clearly defined by mammography and ultrasound.
- It is not indicated for a lesion that is highly characteristic of a **simple cyst** on ultrasound, as it would be an unnecessary and costly procedure.
*Reassurance and clinical follow-up*
- While the ultrasound findings are reassuring, her symptoms (painful mass) and anxiety warrant intervention. **Reassurance alone** is insufficient, as aspiration would confirm the diagnosis and relieve symptoms.
- Dismissing the patient's concerns without further action, especially with a symptomatic mass, is not the best practice and may cause undue stress.
*Mammogram*
- A **mammogram** would be less helpful in this young woman with dense breast tissue, and ultrasound has already characterized the lesion as a cyst.
- Furthermore, for a clearly cystic lesion, mammography provides little additional diagnostic information and exposes the patient to unnecessary radiation.
Breast biopsy techniques US Medical PG Question 4: A 32-year-old woman presents to her physician concerned about wet spots on the inside part of her dress shirts, which she thinks may be coming from one of her breasts. She states that it is painless and that the discharge is usually blood-tinged. She denies any history of malignancy in her family and states that she has been having regular periods since they first started at age 13. She does not have any children. The patient has normal vitals and denies any cough, fever. On exam, there are no palpable masses, and the patient does not have any erythema or induration. What is the most likely diagnosis?
- A. Intraductal papilloma (Correct Answer)
- B. Ductal carcinoma
- C. Paget's disease
- D. Breast abscess
- E. Fibrocystic changes
Breast biopsy techniques Explanation: ***Intraductal papilloma***
- This condition commonly presents as **unilateral, bloody, spontaneous, and painless nipple discharge** from a single duct, often without a palpable mass, which perfectly matches the patient's symptoms.
- It involves a benign tumor growing within a **milk duct**, which can cause bleeding due to its friable nature.
*Ductal carcinoma*
- While it can cause bloody nipple discharge, **ductal carcinoma** is more frequently associated with a palpable **mass**, skin changes, or axillary lymphadenopathy, none of which are noted here.
- Given the patient's young age and absence of other high-risk features, it is a less likely initial diagnosis compared to a benign condition.
*Paget's disease*
- **Paget's disease of the breast** primarily presents as an eczematous lesion on the nipple and/or areola, often with **itching, burning, and ulceration**, rather than solely bloody nipple discharge.
- It is typically associated with an underlying **invasive ductal carcinoma** or ductal carcinoma in situ, which is not suggested by the current findings.
*Breast abscess*
- A **breast abscess** typically causes **pain, fever, erythema, and induration**, pointing towards an infectious process, none of which are present in this patient's symptoms or physical exam.
- The discharge from an abscess would usually be **purulent**, not blood-tinged.
*Fibrocystic changes*
- **Fibrocystic changes** in the breast often cause **cyclic breast pain, tenderness, and multiple palpable masses** that fluctuate with the menstrual cycle.
- While some forms can cause discharge, it is typically **serous or clear**, not bloody, and rarely unilateral from a single duct.
Breast biopsy techniques US Medical PG Question 5: A 29-year-old nulligravid woman comes to the physician because of a 10-day history of small quantities of intermittent, blood-tinged discharge from her left nipple. There is no personal or family history of serious illness. She has smoked 1 pack of cigarettes daily for 5 years. Her last menstrual period was 12 days ago. She is sexually active and uses condoms inconsistently. Physical examination shows scant serosanguinous fluid expressible from the left nipple. There is no palpable breast mass or axillary lymphadenopathy. Examination shows no other abnormalities. Which of the following is the most appropriate next step in management?
- A. Image-guided core biopsy of the affected duct
- B. Subareolar ultrasound (Correct Answer)
- C. Nipple discharge cytology
- D. Reassurance
- E. Breast MRI
Breast biopsy techniques Explanation: ***Subareolar ultrasound***
- This patient presents with **unilateral**, **spontaneous**, **single-duct bloody nipple discharge**, which is characteristic of an **intraductal papilloma** or early malignancy.
- A **subareolar ultrasound** is the most appropriate initial imaging step to evaluate the ductal system for a mass or obstruction, especially in a young woman with dense breasts where mammography may be less sensitive.
*Image-guided core biopsy of the affected duct*
- A biopsy would be considered if imaging (like ultrasound) reveals a suspicious lesion, but it is not the **initial diagnostic step**.
- **Image guidance** is necessary for biopsy of non-palpable lesions, but first, the lesion needs to be identified and characterized by imaging.
*Nipple discharge cytology*
- **Cytology of nipple discharge** has a **low sensitivity** for identifying malignancy and is generally not recommended as a primary diagnostic tool.
- It can be helpful in some cases, but imaging is usually preferred for initial evaluation of suspicious discharge.
*Reassurance*
- **Bloody nipple discharge**, even in small quantities, is a **concerning symptom** that requires further investigation to rule out malignancy and cannot simply be dismissed.
- While many cases are benign (e.g., intraductal papilloma), serious pathology must be excluded.
*Breast MRI*
- **Breast MRI** is a highly sensitive imaging modality but is typically reserved for **further evaluation** after initial mammography and ultrasound, especially in high-risk patients or for assessing the extent of known disease.
- It is **not the first-line imaging** for isolated bloody nipple discharge without other suspicious findings on initial assessment.
Breast biopsy techniques US Medical PG Question 6: A 27-year-old female presents to her OB/GYN for a check-up. During her visit, a pelvic exam and Pap smear are performed. The patient does not have any past medical issues and has had routine gynecologic care with normal pap smears every 3 years since age 21. The results of the Pap smear demonstrate atypical squamous cells of undetermined significance (ASCUS). Which of the following is the next best step in the management of this patient?
- A. Repeat Pap smear in 1 year
- B. Perform colposcopy
- C. Perform an HPV DNA test (Correct Answer)
- D. Perform a Loop Electrosurgical Excision Procedure (LEEP)
- E. Repeat Pap smear in 3 years
Breast biopsy techniques Explanation: ***Perform an HPV DNA test***
- For women aged 25-29 with an **ASCUS Pap smear result**, the recommended next step is to perform an **HPV DNA test** to triage the finding.
- If the HPV test is positive, a colposcopy is indicated. If negative, routine screening can resume.
*Repeat Pap smear in 1 year*
- This approach is typically recommended for adolescents (age < 21) with an ASCUS result or for women aged 21-24 if HPV testing is not available.
- For women aged 25-29, **HPV testing** is preferred to determine the need for colposcopy.
*Perform colposcopy*
- **Colposcopy** is indicated if the HPV DNA test is positive following an ASCUS result in women 25-29, or for persistent ASCUS or low-grade squamous intraepithelial lesion (LSIL) results in younger women.
- It is not the immediate next step for ASCUS in this age group without prior HPV status.
*Perform a Loop Electrosurgical Excision Procedure (LEEP)*
- **LEEP** is a treatment for high-grade cervical dysplasia (HSIL) or recurrent/persistent LSIL, not a diagnostic step for initial ASCUS.
- Performing a LEEP based solely on an **ASCUS result** would be overly aggressive and may lead to unnecessary complications.
*Repeat Pap smear in 3 years*
- **Repeating a Pap smear in 3 years** is the recommendation for women with a normal Pap smear and negative HPV test, or for those who had an ASCUS/LSIL result with negative HPV testing and subsequent normal screening.
- It is not appropriate for an initial ASCUS finding in a 27-year-old.
Breast biopsy techniques US Medical PG Question 7: A 59-year-old woman presents to the family medicine clinic with a lump in her breast for the past 6 months. She states that she has been doing breast self-examinations once a month. She has a medical history significant for generalized anxiety disorder and systemic lupus erythematosus. She takes sertraline and hydroxychloroquine for her medical conditions. The heart rate is 102/min, and the rest of the vital signs are stable. On physical examination, the patient appears anxious and tired. Her lungs are clear to auscultation bilaterally. Capillary refill is 2 seconds. There is no axillary lymphadenopathy present. Palpation of the left breast reveals a 2 x 2 cm mass. What is the most appropriate next step given the history of the patient?
- A. Mammography (Correct Answer)
- B. Continue breast self-examinations
- C. Referral to general surgery
- D. Biopsy of the mass
- E. Lumpectomy
Breast biopsy techniques Explanation: ***Mammography***
- The presence of a **new breast mass** in a 59-year-old woman warrants immediate investigation to rule out malignancy.
- **Mammography** is the initial imaging modality of choice for evaluating breast lumps, especially in women over 40, and represents the most appropriate **first diagnostic step** after clinical examination.
- Standard workup follows the **triple assessment approach**: clinical examination (completed), imaging (mammography ± ultrasound), and tissue diagnosis (biopsy if imaging is suspicious).
- While this mass has been present for 6 months and will ultimately require biopsy if suspicious features are found, mammography is the appropriate initial imaging study to characterize the lesion and guide further management.
*Continue breast self-examinations*
- Continuing breast self-examinations alone is insufficient given the presence of a **palpable mass** that has persisted for 6 months.
- While self-exams are important for awareness, a new, persistent lump necessitates diagnostic evaluation, not just continued monitoring.
*Referral to general surgery*
- While surgical consultation may be necessary later, it is usually not the **immediate first step** before radiological evaluation.
- Referral to surgery without prior imaging would be premature and does not follow standard diagnostic algorithms.
*Biopsy of the mass*
- A **biopsy** is typically performed after initial imaging (mammography ± ultrasound) has characterized the mass.
- While biopsy will likely be needed given the 6-month duration of this palpable mass, mammography is the standard initial imaging study to perform first.
- Direct biopsy without imaging would miss the opportunity to evaluate the entire breast and axilla for multifocal disease or lymph node involvement.
*Lumpectomy*
- **Lumpectomy** is a therapeutic surgical procedure for excising a mass, not a diagnostic step.
- It is performed after a definitive diagnosis of cancer has been established via imaging and biopsy, along with appropriate staging.
- Performing a lumpectomy without prior diagnostic workup would be inappropriate and does not allow for proper surgical planning.
Breast biopsy techniques US Medical PG Question 8: An excisional biopsy is performed and the diagnosis of superficial spreading melanoma is confirmed. The lesion is 1.1 mm thick. Which of the following is the most appropriate next step in management?
- A. Surgical excision with 0.5-1 cm safety margins only
- B. Surgical excision with 1 cm safety margins only
- C. Surgical excision with 1-2 cm safety margins only
- D. Surgical excision with 0.5-1 cm safety margins and sentinel lymph node study
- E. Surgical excision with 1-2 cm safety margins and sentinel lymph node study (Correct Answer)
Breast biopsy techniques Explanation: ***Surgical excision with 1-2 cm safety margins and sentinel lymph node study***
- A melanoma with a **Breslow thickness between 1.01 mm and 2.0 mm** (like this 1.1 mm lesion) requires a recommended surgical margin of **1 to 2 cm**.
- For melanomas **≥0.8 mm thickness** (or those with ulceration), a **sentinel lymph node biopsy (SLNB)** is recommended to assess for micrometastasis, as it helps in staging and prognosis.
*Surgical excision with 0.5-1 cm safety margins only*
- A 0.5 cm margin is typically reserved for melanoma *in situ* or extremely thin melanomas (less than or equal to 0.5 mm), and 1 cm for lesions 0.51 to 1.0 mm, which is too narrow for a 1.1 mm lesion.
- This option incorrectly omits the **sentinel lymph node study**, which is indicated for a melanoma of this thickness.
*Surgical excision with 1 cm safety margins only*
- While 1 cm is a common margin for lesions up to 1.0 mm, a 1.1 mm melanoma usually warrants a slightly wider margin, ideally 1-2 cm.
- This option also fails to include the **sentinel lymph node study**, which is crucial for staging melanomas ≥0.8 mm thickness.
*Surgical excision with 0.5-1 cm safety margins and sentinel lymph node study*
- The recommended surgical margin for a 1.1 mm melanoma is at least **1 cm, preferably between 1 and 2 cm**, making a 0.5-1 cm range insufficient.
- Although it correctly includes the sentinel lymph node study, the **surgical margin is inadequate** for the given Breslow thickness.
*Surgical excision with 1-2 cm safety margins only*
- While the **1-2 cm surgical margin** is appropriate for a 1.1 mm melanoma, this option **incorrectly excludes the sentinel lymph node study**.
- The sentinel lymph node biopsy is a critical part of the staging and management plan for melanomas of this thickness to detect potential nodal involvement.
Breast biopsy techniques US Medical PG Question 9: A 37-year-old man presents to the emergency department after he cut his hand while working on his car. The patient has a past medical history of antisocial personality disorder and has been incarcerated multiple times. His vitals are within normal limits. Physical exam is notable for a man covered in tattoos with many bruises over his face and torso. Inspection of the patient's right hand reveals 2 deep lacerations on the dorsal aspects of the second and third metacarpophalangeal (MCP) joints. The patient is given a tetanus vaccination, and the wound is irrigated. Which of the following is appropriate management for this patient?
- A. Closure of the wound with sutures
- B. Clindamycin and topical erythromycin
- C. Ciprofloxacin and topical erythromycin
- D. Surgical irrigation, debridement, and amoxicillin-clavulanic acid (Correct Answer)
- E. No further management necessary
Breast biopsy techniques Explanation: ***Surgical irrigation, debridement, and amoxicillin-clavulanic acid***
- The presence of deep lacerations over the metacarpophalangeal joints, combined with an injury mechanism suggestive of a **fight bite** (laceration from striking another person's teeth), mandates **aggressive surgical management**.
- **Amoxicillin-clavulanic acid** is the appropriate antibiotic choice for **human bite wounds** due to its broad spectrum covering common oral flora like *Eikenella corrodens*, *Streptococci*, and anaerobes.
*Closure of the wound with sutures*
- **Primary closure** of human bite wounds, especially those on the hand, is strongly **contraindicated** due to the high risk of severe infection.
- These wounds should be left open to drain and heal by **secondary intention** following thorough debridement.
*Clindamycin and topical erythromycin*
- **Clindamycin** has good anaerobic coverage but lacks sufficient coverage for common aerobes found in human bites like *Eikenella corrodens*.
- **Topical erythromycin** is ineffective for deep soft tissue infections and does not provide systemic protection against the likely pathogens.
*Ciprofloxacin and topical erythromycin*
- **Ciprofloxacin** has limited activity against many oral anaerobes and *Eikenella corrodens*, making it a poor choice for human bite prophylaxis.
- As mentioned, **topical antibiotics** are insufficient for preventing serious infections in deep bite wounds.
*No further management necessary*
- This patient has sustained a **deep, contaminated wound** with a high risk of serious infection, potentially involving joints or tendons.
- Failing to provide further management, including surgical exploration and appropriate antibiotics, would likely lead to severe complications such as **osteomyelitis** or **septic arthritis**.
Breast biopsy techniques US Medical PG Question 10: A 58-year-old woman underwent mastectomy for multicentric DCIS. Final pathology shows high-grade DCIS with comedonecrosis, margins negative by 3 mm, no invasion identified in 40 tissue blocks examined. Sentinel lymph node biopsy shows isolated tumor cells (0.1 mm cluster) positive for cytokeratin. The medical oncologist requests input on systemic therapy. Evaluate the significance of the nodal finding and recommendations.
- A. Upstage to invasive cancer, recommend chemotherapy and endocrine therapy
- B. Perform completion axillary dissection to assess additional nodal involvement
- C. Consider isolated tumor cells clinically insignificant, node-negative staging, endocrine therapy only if ER-positive (Correct Answer)
- D. Recommend axillary radiation and systemic chemotherapy
- E. Repeat pathology review to identify occult invasion
Breast biopsy techniques Explanation: ***Consider isolated tumor cells clinically insignificant, node-negative staging, endocrine therapy only if ER-positive***
- Per AJCC guidelines, **isolated tumor cells (ITCs)** (clusters ≤ 0.2 mm or < 200 cells) are staged as **pN0(i+)**, which is considered node-negative disease.
- In the setting of pure **DCIS**, ITCs do not warrant staging as invasive cancer nor do they justify **systemic chemotherapy**; management depends solely on the tumor's **ER-status** for endocrine therapy.
*Upstage to invasive cancer, recommend chemotherapy and endocrine therapy*
- Staging cannot be upgraded to invasive cancer unless a **pathological focus of invasion** is identified in the breast tissue (T category).
- **Chemotherapy** is never indicated for pure DCIS, regardless of high-grade features or the presence of ITCs in the lymph nodes.
*Perform completion axillary dissection to assess additional nodal involvement*
- **Completion axillary lymph node dissection (ALND)** is not indicated for ITCs, as they do not carry the same prognostic weight as macro-metastases.
- In pure DCIS, the presence of ITCs is often attributed to **mechanical transport** of cells during biopsy rather than true metastatic potential.
*Recommend axillary radiation and systemic chemotherapy*
- **Axillary radiation** is reserved for patients with significant nodal burden and is inappropriate for **pN0(i+)** status.
- Because DCIS is a non-invasive, **pre-cancerous lesion** contained within the basement membrane, systemic chemotherapy provides no benefit and unnecessary toxicity.
*Repeat pathology review to identify occult invasion*
- While high-grade DCIS increases the risk of occult invasion, the examination of **40 tissue blocks** is considered exhaustive and standard for ruling out invasion.
- Persistent searching for micro-invasion after comprehensive sampling is unlikely to change the clinical management dictated by the **pN0(i+)** finding.
More Breast biopsy techniques US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.