Axillary lymph node dissection US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Axillary lymph node dissection. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Axillary lymph node dissection US Medical PG Question 1: A 32-year-old man comes to the emergency department because of a wound in his foot. Four days ago, he stepped on a nail while barefoot at the beach. Examination of the plantar surface of his right foot shows a purulent puncture wound at the base of his second toe with erythema and tenderness of the surrounding skin. The afferent lymphatic vessels from the site of the lesion drain directly into which of the following groups of regional lymph nodes?
- A. Popliteal
- B. Deep inguinal
- C. Anterior tibial
- D. Superficial inguinal (Correct Answer)
- E. External iliac
Axillary lymph node dissection Explanation: ***Superficial inguinal***
- Lymph from the **plantar surface of the foot** (including the base of the toes) drains into the **superficial inguinal lymph nodes**.
- The **medial and central plantar surfaces** specifically follow the medial superficial lymphatic vessels that accompany the great saphenous vein system to reach these nodes.
- These nodes are the **primary drainage site** and crucial in the initial immune response to infections of the lower limb.
*Popliteal*
- The **popliteal lymph nodes** primarily drain lymph from the **lateral foot and heel**, posterior leg, and knee.
- They are located within the popliteal fossa and would not be the direct drainage site for a wound on the plantar surface of the second toe.
*Deep inguinal*
- **Deep inguinal lymph nodes** receive lymph from the superficial inguinal nodes, as well as from deeper structures of the thigh and glans penis/clitoris.
- They are considered a **secondary drainage site** and not the primary destination for superficial foot infections.
*Anterior tibial*
- There are no well-defined major lymph nodes specifically termed "anterior tibial" that serve as a primary drainage site for the foot.
- Lymphatics generally follow venous drainage patterns, and the anterior tibial vessels drain superiorly, not to a specific nodal group at this level.
*External iliac*
- **External iliac lymph nodes** receive lymph primarily from the deep inguinal nodes and pelvic organs.
- They are a more **proximal group** in the lymphatic chain and not the direct initial drainage site for a foot infection.
Axillary lymph node dissection US Medical PG Question 2: A 29-year-old woman, gravida 1, para 1, comes to the physician for the evaluation of a painful mass in her left breast for several days. She has no fevers or chills. She has not noticed any changes in the right breast. She has no history of serious illness. Her last menstrual period was 3 weeks ago. She appears anxious. Her temperature is 37°C (98.6°F), pulse is 80/min, respirations are 13/min, and blood pressure is 130/75 mm Hg. Examination shows a palpable, mobile, tender mass in the left upper quadrant of the breast. Ultrasound shows a 1.75-cm, well-circumscribed anechoic mass with posterior acoustic enhancement. The patient says that she is very concerned that she may have breast cancer and wishes further diagnostic testing. Which of the following is the most appropriate next step in the management of this patient?
- A. Core needle biopsy
- B. MRI scan of the left breast
- C. Reassurance and clinical follow-up
- D. Fine needle aspiration (Correct Answer)
- E. Mammogram
Axillary lymph node dissection Explanation: ***Fine needle aspiration***
- This patient presents with a **palpable, mobile, tender mass** in the breast, and ultrasound reveals a **well-circumscribed anechoic mass with posterior acoustic enhancement**, which is highly suggestive of a **simple cyst**.
- **Fine needle aspiration** is the most appropriate next step for a symptomatic simple cyst; it can be both diagnostic and therapeutic, relieving patient anxiety and pain.
*Core needle biopsy*
- **Core needle biopsy** is typically reserved for lesions that are suspicious for malignancy, such as solid masses with **irregular margins** or **architectural distortion**, which are not present in this case.
- Performing a core needle biopsy on a likely simple cyst is excessively invasive and carries risks like bleeding and infection without clear indication.
*MRI scan of the left breast*
- An **MRI scan** is generally used for screening high-risk patients, evaluating the extent of known cancer, or further characterizing complex lesions not clearly defined by mammography and ultrasound.
- It is not indicated for a lesion that is highly characteristic of a **simple cyst** on ultrasound, as it would be an unnecessary and costly procedure.
*Reassurance and clinical follow-up*
- While the ultrasound findings are reassuring, her symptoms (painful mass) and anxiety warrant intervention. **Reassurance alone** is insufficient, as aspiration would confirm the diagnosis and relieve symptoms.
- Dismissing the patient's concerns without further action, especially with a symptomatic mass, is not the best practice and may cause undue stress.
*Mammogram*
- A **mammogram** would be less helpful in this young woman with dense breast tissue, and ultrasound has already characterized the lesion as a cyst.
- Furthermore, for a clearly cystic lesion, mammography provides little additional diagnostic information and exposes the patient to unnecessary radiation.
Axillary lymph node dissection US Medical PG Question 3: A 59-year-old woman presents to her primary care provider with a 6-month history of progressive left-arm swelling. Two years ago she had a partial mastectomy and axillary lymph node dissection for left breast cancer. She was also treated with radiotherapy at the time. Upon further questioning, she denies fever, pain, or skin changes, but reports difficulty with daily tasks because her hand feels heavy and weak. She is bothered by the appearance of her enlarged extremity and has stopped playing tennis. On physical examination, nonpitting edema of the left arm is noted with hyperkeratosis, papillomatosis, and induration of the skin. Limb elevation, exercise, and static compression bandaging are started. If the patient has no improvement, which of the following will be the best next step?
- A. Diethylcarbamazine
- B. Low molecular weight heparin
- C. Endovascular stenting
- D. Vascularized lymph node transfer (Correct Answer)
- E. Antibiotics
Axillary lymph node dissection Explanation: ***Vascularized lymph node transfer***
- This patient presents with **secondary lymphedema** due to axillary dissection and radiotherapy, which has not responded to conservative management.
- **Vascularized lymph node transfer** is a surgical option that involves transplanting healthy lymph nodes to the affected area to re-establish lymphatic drainage pathways, offering a more definitive solution for refractory cases.
*Diethylcarbamazine*
- **Diethylcarbamazine** is an anti-filarial drug used to treat lymphedema caused by **parasitic infections**, specifically filariasis.
- The patient's lymphedema is secondary to breast cancer treatment, not parasitic infection, making this a **misdirected treatment**.
*Low molecular weight heparin*
- **Low molecular weight heparin** is an anticoagulant used to prevent or treat **venous thromboembolism (VTE)**.
- While patients with cancer are at increased risk for VTE, her symptoms are consistent with lymphedema and not thrombosis, which would typically present with more acute pain and swelling, making this an inappropriate treatment.
*Endovascular stenting*
- **Endovascular stenting** is a procedure used to open blocked or narrowed **blood vessels**, such as in peripheral artery disease or venous obstruction.
- Her condition is specifically lymphedema, a lymphatic circulation issue, not a vascular obstruction, so stenting would not address the underlying problem.
*Antibiotics*
- **Antibiotics** are used to treat **bacterial infections**, which can complicate lymphedema (e.g., cellulitis).
- While chronic lymphedema causes skin changes (hyperkeratosis, papillomatosis, induration), the patient shows no signs of **acute infection** such as fever, pain, erythema, or warmth, making empirical antibiotics unnecessary at this stage.
Axillary lymph node dissection US Medical PG Question 4: A 40-year-old man presents with a painless firm mass in the right breast. Examination shows retraction of the nipple and the skin is fixed to the underlying mass. The axillary nodes are palpable. Which of the following statements is FALSE regarding the above condition?
- A. Lobular cancer is the most common breast cancer in males (Correct Answer)
- B. BRCA2 mutations are associated with increased risk
- C. These are positive for estrogen receptor
- D. Endocrine therapy plays an important role in treatment
- E. Gynecomastia may be caused by certain medications
Axillary lymph node dissection Explanation: ***Lobular cancer is the most common breast cancer in males***
- This statement is **FALSE** and is the correct answer. The most common type of breast cancer in males is **invasive ductal carcinoma (IDC)**, accounting for about 80-90% of cases.
- **Invasive lobular carcinoma** is rare in men because men have very few lobules in their breast tissue.
*Gynecomastia may be caused by certain medications*
- This statement is **TRUE**. Medications such as spironolactone, cimetidine, finasteride, antipsychotics, and anabolic steroids can cause gynecomastia.
- However, the clinical presentation described (firm mass, nipple retraction, skin fixation, axillary nodes) is consistent with **malignancy**, not gynecomastia.
*BRCA2 mutations are associated with increased risk*
- This statement is **TRUE**. Male breast cancer is strongly associated with **BRCA2 mutations** (and less commonly BRCA1), which are hereditary.
- Men with BRCA2 mutations have a 5-10% lifetime risk of developing breast cancer, compared to less than 0.1% in the general male population.
*These are positive for estrogen receptor*
- This statement is **TRUE**. A vast majority (over 90%) of male breast cancers are **estrogen receptor (ER) positive**, which makes them responsive to endocrine therapy.
- This high rate of ER positivity is even greater than in female breast cancers.
*Endocrine therapy plays an important role in treatment*
- This statement is **TRUE**. Given the high prevalence of ER positivity (over 90%), endocrine therapy such as **tamoxifen** or aromatase inhibitors is a cornerstone of treatment for male breast cancer.
- Endocrine therapy is used in both adjuvant and metastatic settings for hormone receptor-positive disease.
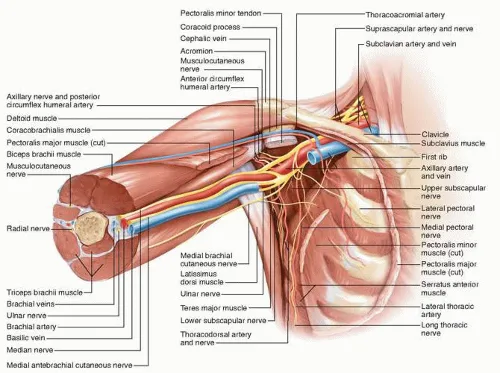
Axillary lymph node dissection US Medical PG Question 5: A 61-year-old woman comes to the physician for a follow-up examination 1 week after undergoing right-sided radical mastectomy and axillary lymph node dissection for breast cancer. She says that she has been unable to comb her hair with her right hand since the surgery. Physical examination shows shoulder asymmetry. She is unable to abduct her right arm above 90 degrees. When she pushes against a wall, there is protrusion of the medial aspect of the right scapula. Injury to which of the following nerves is the most likely cause of this patient's condition?
- A. Long thoracic nerve (Correct Answer)
- B. Thoracodorsal nerve
- C. Axillary nerve
- D. Suprascapular nerve
- E. Upper trunk of the brachial plexus
Axillary lymph node dissection Explanation: ***Long thoracic nerve***
- Injury to the **long thoracic nerve** leads to paralysis of the **serratus anterior muscle**, causing **scapular winging** (protrusion of the medial scapula) especially when pushing against a wall.
- The serratus anterior is crucial for **scapular protraction** and stabilizing the scapula during **abduction of the arm above 90 degrees**, explaining her inability to comb her hair.
*Thoracodorsal nerve*
- The **thoracodorsal nerve** innervates the **latissimus dorsi muscle**, which is responsible for **adduction**, extension, and internal rotation of the arm.
- Injury to this nerve would primarily affect these movements, not shoulder abduction above 90 degrees or scapular winging.
*Axillary nerve*
- The **axillary nerve** innervates the **deltoid muscle** and **teres minor**.
- Damage would primarily result in impaired **arm abduction up to 90 degrees** and loss of sensation over the lateral shoulder, but not scapular winging.
*Suprascapular nerve*
- The **suprascapular nerve** supplies the **supraspinatus** and **infraspinatus muscles**, which are involved in the initiation of arm abduction and external rotation, respectively.
- Injury would cause weakness in these movements and shoulder pain, but not scapular winging.
*Upper trunk of the brachial plexus*
- Injury to the **upper trunk of the brachial plexus** (C5-C6) affects several nerves and muscles, leading to conditions like **Erb's palsy**.
- While it can impair shoulder function and abduction, the specific finding of scapular winging points more directly to long thoracic nerve damage rather than a generalized upper trunk injury, as the long thoracic nerve (C5-C7) is often spared in classic Erb's palsy.
Axillary lymph node dissection US Medical PG Question 6: A 61-year-old woman presents to a surgical oncologist for consideration of surgical removal of biopsy-confirmed breast cancer. The mass is located in the tail of Spence along the superolateral aspect of the left breast extending into the axilla. The surgical oncologist determines that the optimal treatment for this patient involves radical mastectomy including removal of the axillary lymph nodes. The patient undergoes all appropriate preoperative tests and is cleared for surgery. During the operation, multiple enlarged axillary lymph nodes are present along the superolateral chest wall. While exposing the lymph nodes, the surgeon accidentally nicks a nerve. Which of the following physical examination findings will most likely be seen in this patient following the operation?
- A. Internal rotation, adduction, and extension of the arm
- B. Weakness in arm flexion at the elbow and numbness over the lateral forearm
- C. Weakness in shoulder abduction and numbness over the lateral shoulder
- D. Scapular protrusion while pressing against a wall (Correct Answer)
- E. Weakness in wrist extension and numbness over the dorsal hand
Axillary lymph node dissection Explanation: ***Scapular protrusion while pressing against a wall***
- Damage to the **long thoracic nerve** during axillary dissection (common in radical mastectomy) paralyzes the **serratus anterior muscle**.
- Paralysis of the serratus anterior causes **scapular winging** (protrusion) and inability to effectively protract the scapula, especially when pushing against a wall.
*Internal rotation, adduction, and extension of the arm*
- This constellation of findings, sometimes called **"policeman's tip"**, is characteristic of an **Erb's palsy**, involving the C5-C6 roots of the brachial plexus.
- Erb's palsy typically results from birth trauma or severe shoulder injury, not commonly from axillary lymph node dissection.
*Weakness in arm flexion at the elbow and numbness over the lateral forearm*
- This symptom complex indicates injury to the **musculocutaneous nerve**, affecting the biceps brachii and brachialis muscles and sensation to the lateral forearm.
- While theoretically possible in deep axillary dissection, it is less common than long thoracic nerve injury during routine axillary node removal.
*Weakness in shoulder abduction and numbness over the lateral shoulder*
- This presentation suggests damage to the **axillary nerve**, which innervates the deltoid and teres minor muscles and provides sensation over the "regimental badge" area of the shoulder.
- The axillary nerve is located more inferiorly and posteriorly in the axilla and is less prone to injury during standard anterior axillary lymph node dissection compared to the long thoracic nerve.
*Weakness in wrist extension and numbness over the dorsal hand*
- These are signs of **radial nerve injury**, which affects the extensor muscles of the wrist and fingers and sensation over the dorsal hand.
- The radial nerve runs more posteriorly in the axilla and arm, making it less susceptible to injury during an anterior axillary lymph node dissection.
Axillary lymph node dissection US Medical PG Question 7: A 57-year-old nulliparous woman comes to the physician 2 weeks after noticing a lump in her right breast. Her last mammogram was performed 4 years ago and showed no abnormalities. Menopause began 2 years ago, during which time the patient was prescribed hormone replacement therapy for severe hot flashes and vaginal dryness. Vital signs are within normal limits. Examination of the right breast shows a firm, nontender mass close to the nipple. There are no changes in the skin or nipple, and there is no palpable axillary adenopathy. The abdomen is soft and nontender; there is no organomegaly. Mammography shows a suspicious 2-cm mass adjacent to the nipple. Which of the following is the most appropriate next step in management?
- A. Mastectomy
- B. Measurement of serum CA 15–3
- C. Core needle biopsy (Correct Answer)
- D. Fine needle aspiration
- E. Bone scan
Axillary lymph node dissection Explanation: ***Core needle biopsy***
- A **core needle biopsy** is the most appropriate next step to obtain a definitive diagnosis for a suspicious breast mass identified on mammography and clinical exam.
- It provides **tissue for histopathological examination**, allowing for precise classification of the tumor (e.g., invasive ductal carcinoma, lobular carcinoma), grading, and receptor status analysis (estrogen, progesterone, HER2), which are crucial for treatment planning.
*Mastectomy*
- **Mastectomy** is a surgical procedure for breast cancer removal but should only be performed **after a definitive diagnosis** has been established through biopsy.
- Proceeding directly to mastectomy without a biopsy risks unnecessary surgery if the mass proves to be benign.
*Measurement of serum CA 15–3*
- **CA 15-3** is a tumor marker that may be elevated in some patients with **advanced breast cancer**, but it is generally *not* sensitive or specific enough for diagnosis or initial staging.
- Its utility is primarily in **monitoring treatment response** or recurrence in patients with known metastatic disease, not for initial evaluation of a suspicious mass.
*Fine needle aspiration*
- **Fine needle aspiration** (FNA) can differentiate between solid and cystic masses and *may* provide cytological diagnosis, but it often does not provide enough tissue to determine invasiveness or perform complete receptor status analysis.
- A **core needle biopsy** is preferred as it yields more tissue for comprehensive pathology, which is critical for treatment decisions.
*Bone scan*
- A **bone scan** is used to detect **bone metastases** in patients with established breast cancer, particularly those with higher stages or symptoms suggestive of bone involvement.
- It is **not indicated as an initial diagnostic step** for a suspicious breast mass before a definitive diagnosis of cancer has been made and staging initiated.
Axillary lymph node dissection US Medical PG Question 8: A 49-year-old man comes to the physician for evaluation of several painless, pruritic lesions on his left forearm that he first noticed 4 days ago. They were initially pink marks that progressed into blisters before ulcerating. He has also had a headache for 1 week. His temperature is 38.1°C (100.6°F). A photograph of one of the lesions is shown. There is pronounced edema of the surrounding skin and painless swelling of the left axillary lymph nodes. Which of the following is the greatest risk factor for this patient's condition?
- A. Pool swimming
- B. Wool handling (Correct Answer)
- C. Sexual contact
- D. Cat scratch
- E. Spider bite
Axillary lymph node dissection Explanation: ***Wool handling***
- The patient's lesion, described as a **painless, pruritic ulcerating blister** on the forearm along with surrounding edema, axillary lymphadenopathy, and systemic symptoms like fever and headache, is highly suggestive of **cutaneous anthrax**.
- **Wool handling** exposes individuals to spores of *Bacillus anthracis*, which are commonly found in animal products, making it a significant risk factor for anthrax, especially the cutaneous form (also known as **wool sorter's disease**).
*Pool swimming*
- Pool swimming is associated with skin infections like **folliculitis** (from *Pseudomonas aeruginosa*) or **verrucae** (warts), which do not present with the characteristic features of a painless ulcer with a black eschar.
- While skin infections can occur, they do not typically cause the systemic symptoms and characteristic lesion shown.
*Sexual contact*
- Sexual contact is associated with sexually transmitted infections, such as **syphilis** (chancre), **herpes simplex virus** (vesicles), or **chancroid** (painful ulcers).
- These conditions have distinctly different lesion characteristics and clinical presentations compared to the described condition.
*Cat scratch*
- **Cat scratch disease**, caused by *Bartonella henselae*, typically presents with **papules or pustules at the scratch site** and regional lymphadenopathy, but the primary lesion does not evolve into a painless ulcer with a distinctive black eschar.
- The initial lesion in cat scratch disease is often a small, red papule or vesicle, not a blister that progresses to an ulcer with a black necrotic center.
*Spider bite*
- Spider bites can cause various skin reactions, from mild irritation to **necrotic lesions** (e.g., from a **brown recluse spider**).
- However, spider bites usually involve a sudden onset of a painful lesion, which often has a central necrotic area, but they don't typically present with a preceding blister and the specific progression to a painless, pruritic ulcer with pronounced edema and associated systemic symptoms as seen in this case of cutaneous anthrax.
Axillary lymph node dissection US Medical PG Question 9: An excisional biopsy is performed and the diagnosis of superficial spreading melanoma is confirmed. The lesion is 1.1 mm thick. Which of the following is the most appropriate next step in management?
- A. Surgical excision with 0.5-1 cm safety margins only
- B. Surgical excision with 1 cm safety margins only
- C. Surgical excision with 1-2 cm safety margins only
- D. Surgical excision with 0.5-1 cm safety margins and sentinel lymph node study
- E. Surgical excision with 1-2 cm safety margins and sentinel lymph node study (Correct Answer)
Axillary lymph node dissection Explanation: ***Surgical excision with 1-2 cm safety margins and sentinel lymph node study***
- A melanoma with a **Breslow thickness between 1.01 mm and 2.0 mm** (like this 1.1 mm lesion) requires a recommended surgical margin of **1 to 2 cm**.
- For melanomas **≥0.8 mm thickness** (or those with ulceration), a **sentinel lymph node biopsy (SLNB)** is recommended to assess for micrometastasis, as it helps in staging and prognosis.
*Surgical excision with 0.5-1 cm safety margins only*
- A 0.5 cm margin is typically reserved for melanoma *in situ* or extremely thin melanomas (less than or equal to 0.5 mm), and 1 cm for lesions 0.51 to 1.0 mm, which is too narrow for a 1.1 mm lesion.
- This option incorrectly omits the **sentinel lymph node study**, which is indicated for a melanoma of this thickness.
*Surgical excision with 1 cm safety margins only*
- While 1 cm is a common margin for lesions up to 1.0 mm, a 1.1 mm melanoma usually warrants a slightly wider margin, ideally 1-2 cm.
- This option also fails to include the **sentinel lymph node study**, which is crucial for staging melanomas ≥0.8 mm thickness.
*Surgical excision with 0.5-1 cm safety margins and sentinel lymph node study*
- The recommended surgical margin for a 1.1 mm melanoma is at least **1 cm, preferably between 1 and 2 cm**, making a 0.5-1 cm range insufficient.
- Although it correctly includes the sentinel lymph node study, the **surgical margin is inadequate** for the given Breslow thickness.
*Surgical excision with 1-2 cm safety margins only*
- While the **1-2 cm surgical margin** is appropriate for a 1.1 mm melanoma, this option **incorrectly excludes the sentinel lymph node study**.
- The sentinel lymph node biopsy is a critical part of the staging and management plan for melanomas of this thickness to detect potential nodal involvement.
Axillary lymph node dissection US Medical PG Question 10: A 63-year-old female with known breast cancer presents with progressive motor weakness in bilateral lower extremities and difficulty ambulating. Physical exam shows 4 of 5 motor strength in her legs and hyper-reflexia in her patellar tendons. Neurologic examination 2 weeks prior was normal. Imaging studies, including an MRI, show significant spinal cord compression by the metastatic lesion and complete erosion of the T12 vertebrae. She has no metastatic disease to the visceral organs and her oncologist reports her life expectancy to be greater than one year. What is the most appropriate treatment?
- A. Palliative pain management consultation
- B. Surgical decompression and postoperative radiotherapy (Correct Answer)
- C. High-dose corticosteroids and clinical observation
- D. Radiation therapy alone
- E. Chemotherapy alone
Axillary lymph node dissection Explanation: ***Surgical decompression and postoperative radiotherapy***
- There is **spinal cord compression** by a metastatic lesion in a patient with a good prognosis (>1 year life expectancy) and rapidly progressive neurological deficits. **Surgical decompression** offers immediate relief of compression, while **postoperative radiotherapy** helps local tumor control.
- This combined approach is superior in preserving neurological function and improving quality of life for patients with **epidural spinal cord compression (ESCC)** in this clinical context.
*Palliative pain management consultation*
- While pain management is important in cancer care, this option alone does not address the **progressive neurological deficits** due to spinal cord compression.
- This patient's condition requires active treatment to prevent further neurological compromise and is not solely focused on comfort measures at this stage given her prognosis.
*Spinal dose corticosteroids and clinical observation*
- **Corticosteroids** can temporarily reduce edema around the spinal cord, but they do not resolve the mechanical compression caused by the eroded T12 vertebrae.
- **Clinical observation** without definitive intervention risks irreversible neurological damage given the rapid progression of symptoms.
*Radiation therapy alone*
- While radiation therapy is effective for local tumor control, it may not provide **rapid enough decompression** for acute or rapidly progressing neurological deficits due to significant mechanical compression.
- In cases of severe compression, such as bone erosion and cord involvement, surgery is usually needed prior to or in combination with radiation.
*Chemotherapy alone*
- **Chemotherapy** for breast cancer is a systemic treatment and may take time to reduce tumor burden, which is not suitable for urgent relief of **spinal cord compression**.
- It does not provide immediate mechanical decompression and is generally not the primary treatment for acute ESCC, especially with bone involvement.
More Axillary lymph node dissection US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.