Trauma scoring systems US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Trauma scoring systems. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Trauma scoring systems US Medical PG Question 1: A 27-year-old male presents to the Emergency Room as a code trauma after being shot in the neck. En route, the patient's blood pressure is 127/73 mmHg, pulse is 91/min, respirations are 14/min, and oxygen saturation is 100% on room air with GCS of 15. On physical exam, the patient is in no acute distress; however, there is an obvious entry point with oozing blood near the left lateral neck above the cricoid cartilage with a small hematoma that is non-pulsatile and stable since arrival. The rest of the physical exam is unremarkable. Rapid hemoglobin returns back at 14.1 g/dL. After initial resuscitation, what is the next best step in management?
- A. Bedside neck exploration
- B. Conventional angiography
- C. MRI
- D. Plain radiography films
- E. CT angiography (Correct Answer)
Trauma scoring systems Explanation: ***CT angiography***
- **CT angiography** is the most appropriate next step for **stable patients** with penetrating neck trauma, like this patient, to evaluate for vascular and airway injuries.
- It offers **rapid, non-invasive assessment** of the extent of injury and helps guide further management.
*Bedside neck exploration*
- **Bedside neck exploration** is typically reserved for patients with **hard signs** of vascular injury (e.g., active hemorrhage, expanding hematoma, pulsatile hematoma) or **signs of airway compromise**, which are absent here.
- This patient is **hemodynamically stable** and has a non-expanding hematoma.
*Conventional angiography*
- **Conventional angiography** is more **invasive** and time-consuming than CTA, carrying risks such as arterial dissection or stroke.
- It is usually reserved for **diagnostic confirmation** or **therapeutic intervention** (e.g., embolization) after initial imaging, especially when CTA findings are equivocal or reveal treatable lesions.
*MRI*
- **MRI** is generally **contraindicated** in acute trauma situations, especially when the presence of metallic foreign bodies (e.g., bullet fragments) is a concern.
- Its **longer acquisition time** and **lack of immediate availability** in the emergency setting make it less suitable for initial evaluation of penetrating neck trauma.
*Plain radiography films*
- **Plain radiographs** can identify **bony fractures** and the general location of foreign bodies, but they offer **limited information** regarding soft tissue and vascular structures.
- They are insufficient for comprehensively evaluating potential vascular or airway injuries in penetrating neck trauma.
Trauma scoring systems US Medical PG Question 2: Group of 100 medical students took an end of the year exam. The mean score on the exam was 70%, with a standard deviation of 25%. The professor states that a student's score must be within the 95% confidence interval of the mean to pass the exam. Which of the following is the minimum score a student can have to pass the exam?
- A. 45%
- B. 63.75%
- C. 67.5%
- D. 20%
- E. 65% (Correct Answer)
Trauma scoring systems Explanation: ***65%***
- To find the **95% confidence interval (CI) of the mean**, we use the formula: Mean ± (Z-score × Standard Error). For a 95% CI, the Z-score is approximately **1.96**.
- The **Standard Error (SE)** is calculated as SD/√n, where n is the sample size (100 students). So, SE = 25%/√100 = 25%/10 = **2.5%**.
- The 95% CI is 70% ± (1.96 × 2.5%) = 70% ± 4.9%. The lower bound is 70% - 4.9% = **65.1%**, which rounds to **65%** as the minimum passing score.
*45%*
- This value is significantly lower than the calculated lower bound of the 95% confidence interval (approximately 65.1%).
- It would represent a score far outside the defined passing range.
*63.75%*
- This value falls below the calculated lower bound of the 95% confidence interval (approximately 65.1%).
- While close, this score would not meet the professor's criterion for passing.
*67.5%*
- This value is within the 95% confidence interval (65.1% to 74.9%) but is **not the minimum score**.
- Lower scores within the interval would still qualify as passing.
*20%*
- This score is extremely low and falls significantly outside the 95% confidence interval for a mean of 70%.
- It would indicate performance far below the defined passing threshold.
Trauma scoring systems US Medical PG Question 3: A surgeon is interested in studying how different surgical techniques impact the healing of tendon injuries. In particular, he will compare 3 different types of suture repairs biomechanically in order to determine the maximum load before failure of the tendon 2 weeks after repair. He collects data on maximum load for 90 different repaired tendons from an animal model. Thirty tendons were repaired using each of the different suture techniques. Which of the following statistical measures is most appropriate for analyzing the results of this study?
- A. Chi-squared
- B. Wilcoxon rank sum
- C. Pearson r coefficient
- D. Student t-test
- E. ANOVA (Correct Answer)
Trauma scoring systems Explanation: ***ANOVA***
- **ANOVA (Analysis of Variance)** is appropriate here because it compares the means of **three or more independent groups** (the three different suture techniques) on a continuous dependent variable (maximum load before failure).
- The study has three distinct repair techniques, each with 30 tendons, making ANOVA suitable for determining if there are statistically significant differences among their mean failure loads.
*Chi-squared*
- The **Chi-squared test** is used for analyzing **categorical data** (frequencies or proportions) to determine if there is an association between two nominal variables.
- This study involves quantitative measurement (maximum load), not categorical data, making Chi-squared inappropriate.
*Wilcoxon rank sum*
- The **Wilcoxon rank sum test** (also known as Mann-Whitney U test) is a **non-parametric test** used to compare two independent groups when the data is not normally distributed or is ordinal.
- While the study has independent groups, it involves three groups, and the dependent variable is continuous, making ANOVA a more powerful and appropriate choice assuming normal distribution.
*Pearson r coefficient*
- The **Pearson r coefficient** measures the **strength and direction of a linear relationship between two continuous variables**.
- This study aims to compare means across different groups, not to determine the correlation between two continuous variables.
*Student t-test*
- The **Student t-test** is used to compare the means of **exactly two groups** (either independent or paired) on a continuous dependent variable.
- This study involves comparing three different suture techniques, not just two, making the t-test unsuitable.
Trauma scoring systems US Medical PG Question 4: A 15-year-old boy is brought to the emergency department one hour after sustaining an injury during football practice. He collided head-on into another player while wearing a mouthguard and helmet. Immediately after the collision he was confused but able to use appropriate words. He opened his eyes spontaneously and followed commands. There was no loss of consciousness. He also had a headache with dizziness and nausea. He is no longer confused upon arrival. He feels well. Vital signs are within normal limits. He is fully alert and oriented. His speech is organized and he is able to perform tasks demonstrating full attention, memory, and balance. Neurological examination shows no abnormalities. There is mild tenderness to palpation over the crown of his head but no signs of skin break or fracture. Which of the following is the most appropriate next step?
- A. Discharge without activity restrictions
- B. Discharge and refrain from all physical activity for one week
- C. Observe for 6 hours in the ED and refrain from contact sports for one week (Correct Answer)
- D. Administer prophylactic levetiracetam and observe for 24 hours
- E. Administer prophylactic phenytoin and observe for 24 hours
Trauma scoring systems Explanation: ***Observe for 6 hours in the ED and refrain from contact sports for one week***
- This patient experienced a brief period of **confusion, headache, dizziness**, and **nausea** immediately after a head injury, which are symptoms consistent with a **mild traumatic brain injury (mTBI)** or **concussion**.
- Although his symptoms have resolved at presentation, observation in the ED for a few hours is prudent to ensure no delayed onset of more severe symptoms, and he should **refrain from contact sports** for at least one week as part of concussion management.
*Discharge without activity restrictions*
- Discharging without activity restrictions is unsafe given the initial symptoms of **confusion** and the potential for delayed symptom presentation or complications from a concussion.
- Concussion management requires a period of **physical and cognitive rest** to allow the brain to heal and prevent **second impact syndrome**.
*Discharge and refrain from all physical activity for one week*
- While refraining from all physical activity for one week is part of concussion management, discharging immediately without any observation period after initial neurological symptoms could be risky.
- An observation period allows for monitoring of any **worsening neurological signs** or symptoms that might indicate a more serious injury.
*Administer prophylactic levetiracetam and observe for 24 hours*
- **Prophylactic anticonvulsants** like levetiracetam are typically not recommended for routine management of **mild traumatic brain injury** or concussion.
- Their use is generally reserved for patients with more severe injuries, evolving conditions, or those who have had **seizures post-trauma**.
*Administer prophylactic phenytoin and observe for 24 hours*
- Similar to levetiracetam, **phenytoin** is an anticonvulsant and its prophylactic use is not indicated for **mild head injuries** or concussions.
- Anticonvulsant prophylaxis is associated with potential side effects and is reserved for specific high-risk scenarios, such as **severe TBI** or **penetrating head trauma**.
Trauma scoring systems US Medical PG Question 5: A 24-year-old man presents to the emergency department after a motor vehicle collision. He was in the front seat and unrestrained driver in a head on collision. His temperature is 99.2°F (37.3°C), blood pressure is 90/65 mmHg, pulse is 152/min, respirations are 16/min, and oxygen saturation is 100% on room air. Physical exam is notable for a young man who opens his eyes spontaneously and is looking around. He answers questions with inappropriate responses but discernible words. He withdraws from pain but does not have purposeful movement. Which of the following is this patient's Glasgow coma scale?
- A. 9
- B. 15
- C. 7
- D. 11 (Correct Answer)
- E. 13
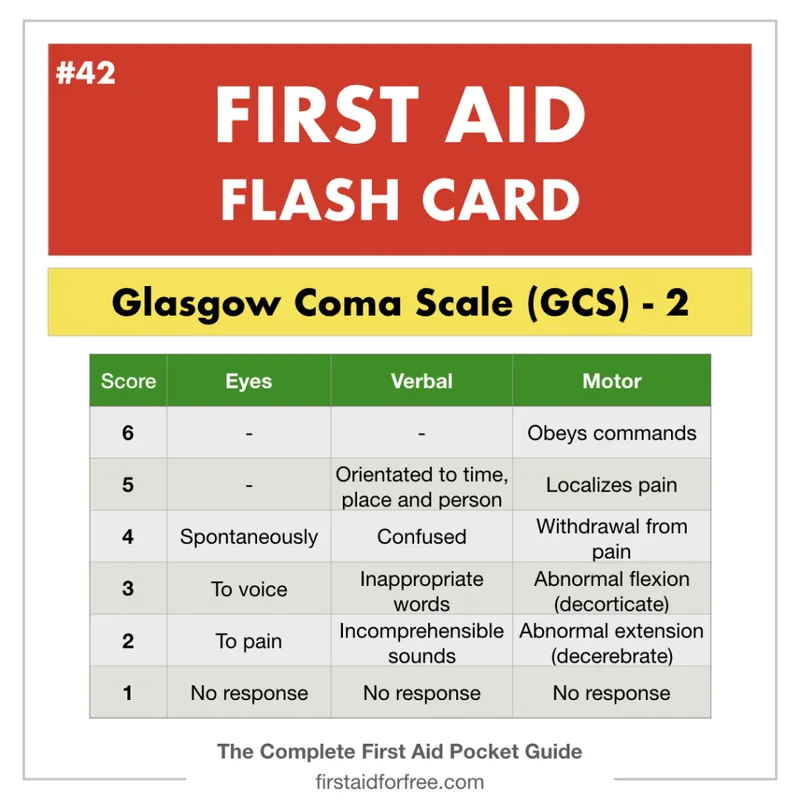
Trauma scoring systems Explanation: ***11***
- **Eye-opening (E)**: The patient opens his eyes spontaneously, scoring **E4**.
- **Verbal response (V)**: He gives inappropriate responses but discernible words, scoring **V3**.
- **Motor response (M)**: He withdraws from pain but does not have purposeful movement, scoring **M4**.
- Therefore, the total Glasgow Coma Scale (GCS) score is **E4 + V3 + M4 = 11**.
*9*
- This score would imply a lower verbal or motor response, such as **incomprehensible sounds (V2)** or **abnormal flexion (M3)**, which is not consistent with the patient's presentation.
- For example, E4 + V2 + M3 would equal 9.
*15*
- A GCS of 15 indicates **normal neurological function**, meaning the patient would be fully oriented, obey commands, and open eyes spontaneously, which is not the case here.
- This score is for a patient who is fully conscious and responsive.
*7*
- A GCS of 7 suggests a **severe brain injury**, which would typically present with a much poorer response, such as **no verbal response (V1)** or **abnormal extension (M2)**.
- For example, E4 + V1 + M2 would equal 7.
*13*
- This score would mean a higher level of consciousness, such as **confused conversation (V4)** or **localizing pain (M5)**, which is better than the patient's described responses.
- For example, E4 + V4 + M5 would equal 13.
Trauma scoring systems US Medical PG Question 6: A 44-year-old man is brought to the emergency department 25 minutes after falling off the roof of a house. He was cleaning the roof when he slipped and fell. He did not lose consciousness and does not have any nausea. On arrival, he is alert and oriented and has a cervical collar on his neck. His pulse is 96/min, respirations are 18/min, and blood pressure is 118/78 mm Hg. Examination shows multiple bruises over the forehead and right cheek. The pupils are equal and reactive to light. There is a 2-cm laceration below the right ear. Bilateral ear canals show no abnormalities. The right wrist is swollen and tender; range of motion is limited by pain. The lungs are clear to auscultation. There is no midline cervical spine tenderness. There is tenderness along the 2nd and 3rd ribs on the right side. The abdomen is soft and nontender. Neurologic examination shows no focal findings. Two peripheral venous catheters are placed. Which of the following is the most appropriate next step in management?
- A. CT scan of the cervical spine (Correct Answer)
- B. Focused Assessment with Sonography in Trauma
- C. X-ray of the neck
- D. X-ray of the chest
- E. X-ray of the right wrist
Trauma scoring systems Explanation: ***CT scan of the cervical spine***
- This patient suffered a significant fall from a height, which is a **high-risk mechanism of injury** for cervical spine trauma, even without immediate neurologic deficits or midline tenderness.
- Due to the high-energy trauma and the potential for severe consequences from an unstable cervical spine injury, a **CT scan** is the preferred imaging modality as it offers superior detail compared to plain X-rays, especially in complex anatomy.
- The patient is **hemodynamically stable** with a benign abdominal exam, and the cervical collar is already in place, indicating that spinal precautions are the immediate priority before any further movement or transfers.
*Focused Assessment with Sonography in Trauma (FAST)*
- FAST exam is primarily used to detect **free fluid (hemorrhage)** in the pericardial, perihepatic, perisplenic, and pelvic spaces in trauma patients.
- While important in trauma evaluation, this patient is **hemodynamically stable** (normal blood pressure, normal pulse) with a **soft, nontender abdomen**, making urgent FAST less critical than clearing the cervical spine.
- The primary concern in a patient with a significant fall mechanism and cervical collar in place is ruling out **cervical spine instability** before further interventions or movement.
*X-ray of the neck*
- While an X-ray can assess the cervical spine, a **CT scan** is generally superior for detecting subtle fractures, ligamentous injuries, and malalignments, especially in patients with high-energy trauma.
- Given the patient's mechanism of injury, an X-ray might miss critical injuries that a CT would identify, leading to potential delays in diagnosis and treatment.
*X-ray of the chest*
- A chest X-ray would be appropriate to assess the patient's **rib fractures** and potential associated injuries like pneumothorax or hemothorax.
- However, the most immediate life-threatening injury in this context, after airway and breathing are secured, is an unstable cervical spine injury, which takes precedence in a stable patient with high-risk mechanism.
*X-ray of the right wrist*
- An X-ray of the right wrist is indicated to evaluate the **swollen and tender wrist** for a fracture or dislocation.
- While important for comprehensive trauma management, it is not the most immediate or life-threatening concern compared to potential cervical spine injury from a high-impact fall.
Trauma scoring systems US Medical PG Question 7: A 27-year-old man is brought to the emergency department by emergency medical services. The patient was an unrestrained passenger in a head-on collision that occurred 15 minutes ago and is currently unresponsive. His temperature is 99.5°F (37.5°C), blood pressure is 60/33 mmHg, pulse is 180/min, respirations are 17/min, and oxygen saturation is 95% on room air. A FAST exam demonstrates fluid in Morrison’s pouch. Laboratory values are drawn upon presentation to the ED and sent off. The patient is started on IV fluids and an initial trauma survey is started. Twenty minutes later, his blood pressure is 95/65 mmHg, and his pulse is 110/min. The patient is further stabilized and is scheduled for emergency surgery. Which of the following best represents this patient’s most likely initial laboratory values?
- A. Hemoglobin: 10 g/dL, Hematocrit: 30%, MCV: 110 µm^3
- B. Hemoglobin: 19 g/dL, Hematocrit: 55%, MCV: 95 µm^3
- C. Hemoglobin: 7 g/dL, Hematocrit: 21%, MCV: 75 µm^3
- D. Hemoglobin: 11 g/dL, Hematocrit: 33%, MCV: 88 µm^3 (Correct Answer)
- E. Hemoglobin: 15 g/dL, Hematocrit: 45%, MCV: 90 µm^3
Trauma scoring systems Explanation: ***Hemoglobin: 11 g/dL, Hematocrit: 33%, MCV: 88 µm^3***
- The patient experienced significant trauma and is experiencing **hemorrhagic shock**, as evidenced by his initial **hypotension** (BP 60/33 mmHg), **tachycardia** (pulse 180/min), and positive **FAST exam** for fluid in Morrison's pouch, indicating intra-abdominal bleeding.
- The initial hemoglobin and hematocrit could be mildly decreased due to acute blood loss, but significant drops are often *not immediately apparent* as plasma volume has not yet moved into the intravascular compartment to dilute the remaining red blood cells. A hemoglobin of 11 g/dL and hematocrit of 33% are consistent with **acute blood loss** before significant hemodilution occurs. MCV of 88 µm^3 is within the normal range for **normocytic anemia** seen in acute hemorrhage.
*Hemoglobin: 10 g/dL, Hematocrit: 30%, MCV: 110 µm^3*
- While a hemoglobin of 10 g/dL and hematocrit of 30% are consistent with anemia due to blood loss, an **MCV of 110 µm^3** (macrocytic) is not typically seen in acute hemorrhage.
- Macrocytic anemia usually results from conditions like **B12 or folate deficiency**, alcoholism, or liver disease, which are not suggested by the acute traumatic scenario.
*Hemoglobin: 19 g/dL, Hematocrit: 55%, MCV: 95 µm^3*
- This indicates **polycythemia** (abnormally high red blood cell count), which is the opposite of what would be expected in a patient experiencing acute hemorrhagic shock.
- These values would suggest conditions like **polycythemia vera** or severe dehydration, which are not relevant in this acute trauma setting.
*Hemoglobin: 7 g/dL, Hematocrit: 21%, MCV: 75 µm^3*
- While a hemoglobin of 7 g/dL and hematocrit of 21% represent significant anemia consistent with major blood loss, these values are typically seen *later* as **hemodilution** occurs, or in cases of chronic blood loss.
- An **MCV of 75 µm^3** (microcytic) is generally indicative of **iron deficiency anemia** or thalassemia, which develops over time and is not characteristic of acute traumatic blood loss.
*Hemoglobin: 15 g/dL, Hematocrit: 45%, MCV: 90 µm^3*
- These values are within the **normal range** for hemoglobin and hematocrit, which would not be expected in a patient presenting with signs of **hemorrhagic shock** and a positive FAST exam indicating significant internal bleeding.
- This would suggest either very minor blood loss or that the values were taken before any bleeding had occurred or before hemodilution had a chance to manifest.
Trauma scoring systems US Medical PG Question 8: A 54-year-old man is brought to the emergency department 30 minutes after being hit by a car while crossing the street. He had a left-sided tonic-clonic seizure and one episode of vomiting while being transported to the hospital. On arrival, he is not oriented to person, place, or time. Physical examination shows flaccid paralysis of all extremities. A CT scan of the head is shown. This patient's symptoms are most likely the result of a hemorrhage in which of the following structures?
- A. Between the dura mater and the arachnoid mater
- B. Into the cerebral parenchyma
- C. Between the skull and the dura mater
- D. Between the arachnoid mater and the pia mater (Correct Answer)
- E. Into the ventricular system
Trauma scoring systems Explanation: ***Between the arachnoid mater and the pia mater (Correct)***
- The CT scan demonstrates diffuse high-density (white) material within the sulci and basal cisterns, indicative of a **subarachnoid hemorrhage**. This space is located between the arachnoid mater and the pia mater.
- The patient's presentation with altered mental status, seizures, vomiting, and flaccid paralysis following trauma is consistent with the severe neurological impact of a **traumatic subarachnoid hemorrhage**.
*Between the dura mater and the arachnoid mater (Incorrect)*
- Hemorrhage in this location is known as a **subdural hematoma**, which typically appears as a crescent-shaped collection of blood.
- While possible in trauma, the CT image shows blood primarily filling the sulci, not a subdural collection.
*Into the cerebral parenchyma (Incorrect)*
- This would be an **intraparenchymal hemorrhage**, appearing as a focal area of high density within the brain tissue itself.
- Although there might be some associated parenchymal injury in severe trauma, the predominant pattern seen on the CT is diffuse blood in the subarachnoid space.
*Between the skull and the dura mater (Incorrect)*
- This describes an **epidural hematoma**, often characterized by a lenticular (lens-shaped) collection of blood due to its confinement by dural attachments.
- The CT image does not show a lenticular collection of blood in this space.
*Into the ventricular system (Incorrect)*
- **Intraventricular hemorrhage** would show blood filling the cerebral ventricles.
- While subarachnoid hemorrhage can sometimes extend into the ventricles, the primary finding on this CT is diffuse blood in the subarachnoid space, not isolated ventricular blood.
Trauma scoring systems US Medical PG Question 9: A 36-year-old male is taken to the emergency room after jumping from a building. Bilateral fractures to the femur were stabilized at the scene by emergency medical technicians. The patient is lucid upon questioning and his vitals are stable. Pain only at his hips was elicited. Cervical exam was not performed. What is the best imaging study for this patient?
- A. AP and lateral radiographs of hips
- B. Lateral radiograph (x-ray) of hips
- C. Magnetic resonance imaging (MRI) of hips, knees, lumbar, and cervical area
- D. Anterior-posterior (AP) and lateral radiographs of hips, knees, lumbar, and cervical area
- E. Computed tomography (CT) scan of cervical spine, hips, and lumbar area (Correct Answer)
Trauma scoring systems Explanation: ***Computed tomography (CT) scan of cervical spine, hips, and lumbar area***
- In **high-energy trauma** (fall from height), a CT scan is the **gold standard** for evaluating the **spine and pelvis**, providing detailed cross-sectional images superior to plain radiographs.
- Since the **cervical exam was not performed**, cervical spine imaging is **mandatory** per ATLS (Advanced Trauma Life Support) protocols. High-energy falls carry significant risk of **cervical spine injury** even without obvious neurological symptoms.
- CT allows comprehensive assessment of **hip fractures, pelvic injuries, and the entire spine** (cervical, thoracic, lumbar), identifying both obvious and **subtle fractures** that may be missed on plain films.
- This approach provides the most **efficient and thorough evaluation** in the acute trauma setting, allowing for appropriate surgical planning and ruling out life-threatening spinal instability.
*AP and lateral radiographs of hips*
- Plain radiographs provide **limited detail** and may **miss subtle fractures**, particularly in complex areas like the pelvis and acetabulum.
- This option **fails to address cervical spine clearance**, which is essential in all high-energy trauma patients, especially when cervical exam has not been performed.
- Radiographs are insufficient for **comprehensive trauma evaluation** after a fall from height.
*Lateral radiograph (x-ray) of hips*
- A single lateral view is **grossly insufficient** for evaluating hip and pelvic fractures, providing only a **two-dimensional perspective** that can miss significant injuries.
- This option **completely neglects spinal evaluation**, which is dangerous in an uncleared trauma patient with a high-energy mechanism.
*Magnetic resonance imaging (MRI) of hips, knees, lumbar, and cervical area*
- While MRI excels at evaluating **soft tissues, ligaments, and bone marrow**, it is **not the initial imaging modality** for acute bony trauma due to longer scan times and lower sensitivity for acute fractures compared to CT.
- MRI is **time-consuming and impractical** in the emergency setting for initial fracture assessment, potentially delaying definitive treatment.
- CT is superior for evaluating **acute skeletal injuries** in the trauma bay.
*Anterior-posterior (AP) and lateral radiographs of hips, knees, lumbar, and cervical area*
- Multiple plain radiographs have **limited sensitivity** for complex or non-displaced fractures, particularly in the **spine and pelvis**, making them inadequate for high-energy trauma evaluation.
- Obtaining multiple radiographic views requires **numerous patient repositionings**, which risks further injury if **spinal instability** is present.
- Plain films provide significantly **less diagnostic information** than CT scanning for trauma assessment.
Trauma scoring systems US Medical PG Question 10: A 17-year-old boy is brought to the emergency department by his brother after losing consciousness 1 hour ago. The brother reports that the patient was skateboarding outside when he fell on the ground and started to have generalized contractions. There was also some blood coming from his mouth. The contractions stopped after about 1 minute, but he remained unconscious for a few minutes afterward. He has never had a similar episode before. There is no personal or family history of serious illness. He does not smoke or drink alcohol. He does not use illicit drugs. He takes no medications. On arrival, he is confused and oriented only to person and place. He cannot recall what happened and reports diffuse muscle ache, headache, and fatigue. He appears pale. His temperature is 37°C (98.6°F), pulse is 80/min, and blood pressure is 130/80 mm Hg. There is a small wound on the left side of the tongue. A complete blood count and serum concentrations of electrolytes, urea nitrogen, and creatinine are within the reference ranges. Toxicology screening is negative. An ECG shows no abnormalities. Which of the following is the most appropriate next step in management?
- A. Electroencephalography
- B. Lumbar puncture
- C. Lorazepam therapy
- D. Reassurance and follow-up
- E. CT scan of the head (Correct Answer)
Trauma scoring systems Explanation: ***CT scan of the head***
- Given the **first-time seizure** in an adolescent, especially with a history of head trauma (falling while skateboarding) and subsequent confusion, a **CT scan of the head** is crucial to rule out acute structural lesions like hemorrhage, mass, or edema.
- It is vital for identifying **life-threatening causes** of seizure that require immediate intervention, such as an **intracranial hematoma** or **mass lesion**, which could have been precipitated or exacerbated by the fall.
*Electroencephalography*
- **EEG** is appropriate for later evaluation to diagnose and classify seizure disorders, but it is not the *most appropriate initial step* in the emergency setting for a first-time seizure with a possible traumatic etiology.
- An EEG might be normal shortly after a seizure, and it does not rule out acute structural brain pathology that requires urgent management.
*Lumbar puncture*
- A **lumbar puncture** is indicated if there's suspicion of meningoencephalitis (e.g., fever, nuchal rigidity, immunocompromised status), which are not prominent features in this patient.
- The patient's vital signs are stable, and there are no signs of infection, making this a less urgent initial diagnostic step compared to imaging.
*Lorazepam therapy*
- **Lorazepam** is a benzodiazepine used to terminate ongoing seizures (**status epilepticus**), but this patient's generalized contractions have already stopped.
- Administering lorazepam when the seizure has resolved is unnecessary and would only cause further sedation.
*Reassurance and follow-up*
- While reassurance is part of patient care, it is *insufficient* as the sole next step for a **first-time seizure** episode in an adolescent, especially with features suggesting a possible underlying acute cause.
- A thorough diagnostic workup, beginning with neuroimaging, is necessary to ensure there is no serious underlying pathology before considering discharge and follow-up.
More Trauma scoring systems US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.