Trauma imaging principles US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Trauma imaging principles. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
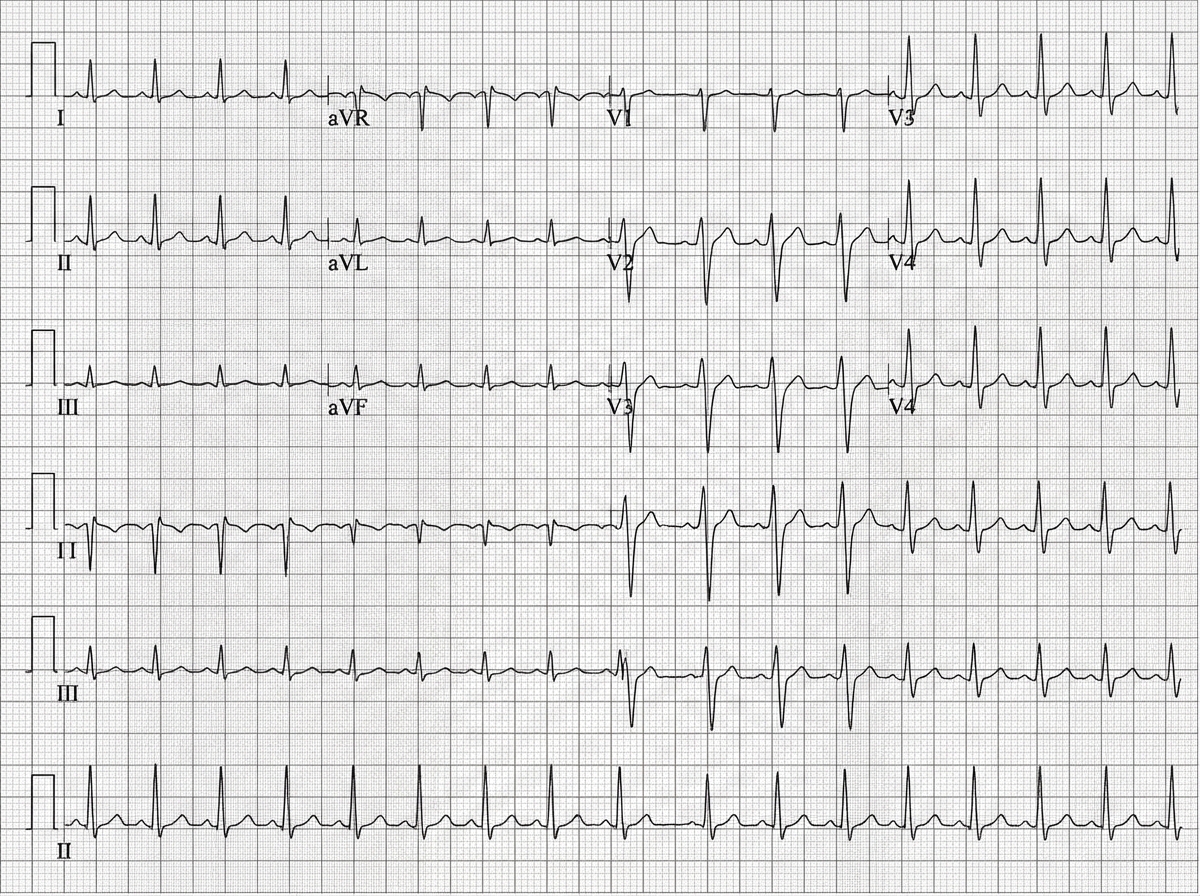
Trauma imaging principles US Medical PG Question 1: A 45-year-old man is brought to the emergency department after a car accident with pain in the middle of his chest and some shortness of breath. He has sustained injuries to his right arm and leg. He did not lose consciousness. His temperature is 37°C (98.6°F), pulse is 110/min, respirations are 18/min, and blood pressure is 90/60 mm Hg. He is alert and oriented to person, place, and time. Examination shows several injuries to the upper extremities and chest. There are jugular venous pulsations 10 cm above the sternal angle. Heart sounds are faint on cardiac examination. The lungs are clear to auscultation. An ECG is shown. Which of the following is the most appropriate next step in management?
- A. Contrast-enhanced CT angiography
- B. Transthoracic echocardiography (Correct Answer)
- C. X-ray of the chest
- D. CT scan of the brain
- E. Contrast esophagram with gastrografin
Trauma imaging principles Explanation: ***Transthoracic echocardiography***
- The patient's presentation with **chest pain**, shortness of breath, **hypotension**, **elevated jugular venous pressure (JVP)**, and **faint heart sounds** after trauma strongly suggests **Beck's triad**, which is classic for **cardiac tamponade**.
- **Transthoracic echocardiography** is the fastest and most accurate method to diagnose cardiac tamponade by visualizing pericardial fluid and its hemodynamic effects.
*Contrast-enhanced CT angiography*
- While CT angiography can detect vascular injuries or aortic dissection, it is not the initial diagnostic test for suspected cardiac tamponade.
- The patient's **hemodynamic instability** requires a rapid diagnostic tool to identify life-threatening conditions like tamponade.
*X-ray of the chest*
- A chest X-ray might show a **widened mediastinum** or **cardiomegaly** if there's a large effusion, but it is not sensitive enough to detect smaller effusions causing tamponade or to assess their hemodynamic impact.
- It does not provide real-time visualization of the heart and pericardium, which is crucial in this emergent setting.
*CT scan of the brain*
- A CT scan of the brain is indicated for suspected head injuries or neurological deficits, but the patient is alert and oriented, and his immediate life threat is clearly thoracic.
- Addressing the signs of cardiac tamponade takes precedence over evaluating the brain given his stable neurological status.
*Contrast esophagram with gastrografin*
- This study is used to diagnose **esophageal perforations**. While possible in significant trauma, the patient's symptoms of **Beck's triad** point specifically to cardiac tamponade, making esophageal perforation a less likely primary diagnosis and this investigation less urgent.
- It would not address the immediate, life-threatening cardiovascular compromise.
Trauma imaging principles US Medical PG Question 2: A 56-year-old man is brought to the emergency department 25 minutes after he was involved in a high-speed motor vehicle collision where he was the unrestrained passenger. He has severe lower abdominal and pelvic pain. On arrival, he is alert and oriented. His pulse is 95/min, respirations are 22/min, and blood pressure is 106/62 mm Hg. Examination shows severe tenderness to palpation over the lower abdomen and over the left anterior superior iliac spine. There is no limb length discrepancy. Application of downward pressure over the pelvis shows no springy resistance or instability. Rectal examination is unremarkable. A focused assessment with sonography shows no free fluid in the abdomen. There is no blood at the urethral meatus. Placement of a Foley catheter shows gross hematuria. An x-ray of the pelvis shows a fracture of the left pelvic edge. Which of the following is the most appropriate next step in management?
- A. Intravenous pyelography
- B. External fixation of the pelvis
- C. Cystoscopy
- D. Retrograde urethrography
- E. Retrograde cystography (Correct Answer)
Trauma imaging principles Explanation: ***Retrograde cystography***
- The presence of **gross hematuria** in a patient with a **pelvic fracture** necessitates ruling out **bladder injury**. A retrograde cystography directly visualizes the bladder and can detect extravasation of contrast if a bladder rupture is present.
- This imaging study specifically investigates the bladder using retrograde contrast filling, which is crucial for diagnosing **intraperitoneal** or **extraperitoneal bladder rupture**.
*Intravenous pyelography*
- This study evaluates the **kidneys** and **ureters** for injury, but the primary concern with gross hematuria and pelvic fracture is the bladder.
- An IV pyelogram provides less detailed imaging of the bladder compared to a retrograde cystogram and is less effective for detecting bladder rupture.
*External fixation of the pelvis*
- While the patient has a pelvic fracture, the immediate priority in a hemodynamically stable patient with gross hematuria is to identify and manage potential **life-threatening urologic injuries** before definitive orthopedic repair.
- **Pelvic external fixation** is primarily indicated for **unstable pelvic fractures** or those causing significant hemorrhage, neither of which is explicitly described as an immediate concern requiring intervention before urologic evaluation.
*Cystoscopy*
- **Cystoscopy** is an endoscopic procedure that allows direct visualization of the bladder's interior. While it can identify bladder injuries, it is generally considered after imaging studies like **retrograde cystography** to confirm findings or address specific issues like clot evacuation or stent placement.
- The initial diagnostic step should focus on assessing for rupture via contrast study, which is often less invasive than a direct endoscopic procedure in the acute trauma setting.
*Retrograde urethrography*
- **Retrograde urethrography (RUG)** is used to evaluate for **urethral injury**, especially when there is blood at the urethral meatus, a high-riding prostate, or an inability to pass a Foley catheter.
- The patient's Foley catheter was successfully placed, and there was **no blood at the urethral meatus**, making urethral injury less likely and thus RUG a lower priority as the initial step compared to assessing for bladder injury.
Trauma imaging principles US Medical PG Question 3: A 67-year-old woman has fallen from the second story level of her home while hanging laundry. She was brought to the emergency department immediately and presented with severe abdominal pain. The patient is anxious, and her hands and feet feel very cold to the touch. There is no evidence of bone fractures, superficial skin wounds, or a foreign body penetration. Her blood pressure is 102/67 mm Hg, respirations are 19/min, pulse is 87/min, and temperature is 36.7°C (98.0°F). Her abdominal exam reveals rigidity and severe tenderness. A Foley catheter and nasogastric tube are inserted. The central venous pressure (CVP) is 5 cm H2O. The medical history is significant for hypertension. Which of the following is best indicated for the evaluation of this patient?
- A. X-Ray
- B. Ultrasound
- C. Peritoneal lavage
- D. CT scan (Correct Answer)
- E. Diagnostic laparotomy
Trauma imaging principles Explanation: ***CT scan***
- A **CT scan of the abdomen and pelvis** is the most indicated imaging modality for evaluating blunt abdominal trauma due to its high sensitivity and specificity in detecting solid organ injuries, free fluid, and active bleeding.
- Given the patient's severe abdominal pain, rigidity, and tenderness after a significant fall, a CT scan will provide detailed anatomical information crucial for guiding further management.
*X-Ray*
- An **X-ray** is useful for detecting bone fractures, but it has limited utility in assessing soft tissue and organ injuries within the abdomen.
- It would not effectively visualize internal bleeding or organ damage, which are primary concerns in this patient given the mechanism of injury and symptoms.
*Ultrasound*
- An **ultrasound (FAST exam)** is effective for rapid detection of free fluid in the abdomen (indicating bleeding or fluid leakage) and can be done at the bedside.
- However, it is operator-dependent and less sensitive than CT for identifying specific organ injuries, retroperitoneal hematomas, or the source of bleeding.
*Peritoneal lavage*
- **Diagnostic peritoneal lavage (DPL)** is an invasive procedure primarily used to detect intra-abdominal bleeding in hemodynamically unstable patients, but it has largely been replaced by ultrasound and CT in stable patients.
- While it can detect blood, it is less specific for identifying the source of bleeding and does not provide anatomical detail, and carries risks of complications like bowel perforation.
*Diagnostic laparotomy*
- **Diagnostic laparotomy** is a surgical procedure to directly visualize abdominal contents and is indicated in cases of clear signs of peritonitis, hemodynamic instability with confirmed intra-abdominal bleeding, or evisceration.
- It is an invasive intervention and would not be the initial diagnostic step in a hemodynamically stable patient without clear indication for immediate surgery.
Trauma imaging principles US Medical PG Question 4: A 36-year-old male is taken to the emergency room after jumping from a building. Bilateral fractures to the femur were stabilized at the scene by emergency medical technicians. The patient is lucid upon questioning and his vitals are stable. Pain only at his hips was elicited. Cervical exam was not performed. What is the best imaging study for this patient?
- A. AP and lateral radiographs of hips
- B. Lateral radiograph (x-ray) of hips
- C. Magnetic resonance imaging (MRI) of hips, knees, lumbar, and cervical area
- D. Anterior-posterior (AP) and lateral radiographs of hips, knees, lumbar, and cervical area
- E. Computed tomography (CT) scan of cervical spine, hips, and lumbar area (Correct Answer)
Trauma imaging principles Explanation: ***Computed tomography (CT) scan of cervical spine, hips, and lumbar area***
- In **high-energy trauma** (fall from height), a CT scan is the **gold standard** for evaluating the **spine and pelvis**, providing detailed cross-sectional images superior to plain radiographs.
- Since the **cervical exam was not performed**, cervical spine imaging is **mandatory** per ATLS (Advanced Trauma Life Support) protocols. High-energy falls carry significant risk of **cervical spine injury** even without obvious neurological symptoms.
- CT allows comprehensive assessment of **hip fractures, pelvic injuries, and the entire spine** (cervical, thoracic, lumbar), identifying both obvious and **subtle fractures** that may be missed on plain films.
- This approach provides the most **efficient and thorough evaluation** in the acute trauma setting, allowing for appropriate surgical planning and ruling out life-threatening spinal instability.
*AP and lateral radiographs of hips*
- Plain radiographs provide **limited detail** and may **miss subtle fractures**, particularly in complex areas like the pelvis and acetabulum.
- This option **fails to address cervical spine clearance**, which is essential in all high-energy trauma patients, especially when cervical exam has not been performed.
- Radiographs are insufficient for **comprehensive trauma evaluation** after a fall from height.
*Lateral radiograph (x-ray) of hips*
- A single lateral view is **grossly insufficient** for evaluating hip and pelvic fractures, providing only a **two-dimensional perspective** that can miss significant injuries.
- This option **completely neglects spinal evaluation**, which is dangerous in an uncleared trauma patient with a high-energy mechanism.
*Magnetic resonance imaging (MRI) of hips, knees, lumbar, and cervical area*
- While MRI excels at evaluating **soft tissues, ligaments, and bone marrow**, it is **not the initial imaging modality** for acute bony trauma due to longer scan times and lower sensitivity for acute fractures compared to CT.
- MRI is **time-consuming and impractical** in the emergency setting for initial fracture assessment, potentially delaying definitive treatment.
- CT is superior for evaluating **acute skeletal injuries** in the trauma bay.
*Anterior-posterior (AP) and lateral radiographs of hips, knees, lumbar, and cervical area*
- Multiple plain radiographs have **limited sensitivity** for complex or non-displaced fractures, particularly in the **spine and pelvis**, making them inadequate for high-energy trauma evaluation.
- Obtaining multiple radiographic views requires **numerous patient repositionings**, which risks further injury if **spinal instability** is present.
- Plain films provide significantly **less diagnostic information** than CT scanning for trauma assessment.
Trauma imaging principles US Medical PG Question 5: A 29-year-old woman presents to a medical office complaining of fatigue, nausea, and vomiting for 1 week. Recently, the smell of certain foods makes her nauseous. Her symptoms are more pronounced in the mornings. The emesis is clear-to-yellow without blood. She has had no recent travel out of the country. The medical history is significant for peptic ulcer, for which she takes pantoprazole. The blood pressure is 100/60 mm Hg, the pulse is 70/min, and the respiratory rate is 12/min. The physical examination reveals pale mucosa and conjunctiva, and bilateral breast tenderness. The LMP was 9 weeks ago. What is the most appropriate next step in the management of this patient?
- A. Beta-HCG levels and a transvaginal ultrasound (Correct Answer)
- B. Beta-HCG levels and a transabdominal ultrasound
- C. Beta-HCG levels and a pelvic CT
- D. Abdominal x-ray
- E. Abdominal CT with contrast
Trauma imaging principles Explanation: ***Beta-HCG levels and a transvaginal ultrasound***
- The patient's symptoms (fatigue, nausea, vomiting, morning sickness, breast tenderness, and **amenorrhea** for 9 weeks) strongly suggest **early pregnancy**.
- **Urine or serum beta-HCG** confirms pregnancy, and a **transvaginal ultrasound** is crucial for confirming an **intrauterine pregnancy**, estimating gestational age, and ruling out complications like ectopic pregnancy, especially at this early stage when transabdominal ultrasound might not provide clear images.
*Beta-HCG levels and a transabdominal ultrasound*
- While beta-HCG levels are appropriate, a **transabdominal ultrasound** may not be sufficient to visualize an early intrauterine pregnancy at 9 weeks due to limited resolution compared to transvaginal ultrasound.
- A definitive confirmation of **intrauterine pregnancy** is critical to rule out an **ectopic pregnancy**, which is better achieved with transvaginal imaging in early gestation.
*Beta-HCG levels and a pelvic CT*
- **CT scans** expose the patient to significant **ionizing radiation**, which is **contraindicated in pregnancy** unless absolutely necessary for life-threatening conditions.
- While it could identify some pelvic pathologies, it is **not the primary imaging modality** for confirming or evaluating early pregnancy due to radiation risks and inferior soft tissue resolution for early gestational sacs compared to ultrasound.
*Abdominal x-ray*
- An **abdominal X-ray** involves **ionizing radiation** and offers very limited diagnostic value for early pregnancy, as it cannot visualize the gestational sac, fetus, or fetal heart activity.
- It is **contraindicated** in suspected pregnancy due to the risk of fetal harm.
*Abdominal CT with contrast*
- **Abdominal CT with contrast** involves both **ionizing radiation** and **contrast agents**, both of which pose significant risks to a developing fetus.
- It is an **inappropriate initial step** for suspected pregnancy and offers no specific diagnostic benefits for confirming or characterizing early gestation.
Trauma imaging principles US Medical PG Question 6: A 33-year-old man is brought to the emergency department because of trauma from a motor vehicle accident. His pulse is 122/min and rapid and thready, the blood pressure is 78/37 mm Hg, the respirations are 26/min, and the oxygen saturation is 90% on room air. On physical examination, the patient is drowsy, with cold and clammy skin. Abdominal examination shows ecchymoses in the right flank. The external genitalia are normal. No obvious external wounds are noted, and the rest of the systemic examination values are within normal limits. Blood is sent for laboratory testing and urinalysis shows 6 RBC/HPF. Hematocrit is 22% and serum creatinine is 1.1 mg/dL. Oxygen supplementation and IV fluid resuscitation are started immediately, but the hypotension persists. The focused assessment with sonography in trauma (FAST) examination shows a retroperitoneal fluid collection. What is the most appropriate next step in management?
- A. Perform an MRI scan of the abdomen and pelvis
- B. CT of the abdomen and pelvis with contrast
- C. Obtain a retrograde urethrogram
- D. Take the patient to the OR for an exploratory laparotomy (Correct Answer)
- E. Perform a diagnostic peritoneal lavage
Trauma imaging principles Explanation: ***Take the patient to the OR for an exploratory laparotomy***
- The patient is **hemodynamically unstable** (BP 78/37 mm Hg, pulse 122/min) with signs of hemorrhagic shock (cold and clammy skin, drowsy, tachycardia) and **hypotension persists despite IV fluid resuscitation**.
- FAST examination shows **retroperitoneal fluid collection** (presumed blood), flank ecchymoses (Grey Turner sign), and hematocrit of 22% indicating **significant blood loss**.
- According to **ATLS (Advanced Trauma Life Support) protocols**, hemodynamically **unstable patients with positive FAST exams require immediate surgical intervention** and should not be delayed for further imaging.
- **Exploratory laparotomy** allows for immediate identification and control of bleeding sources, which is life-saving in this persistently hypotensive patient. The retroperitoneal hematoma can be explored and bleeding vessels ligated or repaired.
*CT of the abdomen and pelvis with contrast*
- CT scan is the **appropriate next step for hemodynamically STABLE trauma patients** or those who **respond to initial resuscitation** to characterize injuries and guide management.
- This patient has **persistent hypotension despite resuscitation**, making him too unstable to safely transport to the CT scanner. Delaying surgery for imaging in an unstable patient increases mortality risk.
- The principle is: **"Blood pressure is better than pictures"** - unstable patients need operative hemorrhage control, not diagnostic imaging.
*Perform an MRI scan of the abdomen and pelvis*
- **MRI has no role in acute trauma evaluation** due to long acquisition time (30-60 minutes), limited availability, and inability to adequately monitor critically ill patients in the MRI suite.
- This would be an inappropriate and potentially fatal delay in a patient with ongoing hemorrhage and hemodynamic instability.
*Perform a diagnostic peritoneal lavage*
- **Diagnostic peritoneal lavage (DPL)** has been largely replaced by FAST examination for detecting intraperitoneal hemorrhage in the modern trauma algorithm.
- While DPL can detect intra-abdominal blood, the **FAST has already identified retroperitoneal fluid**, and the patient's persistent instability mandates immediate surgical intervention rather than additional diagnostic procedures.
- DPL also does not evaluate the retroperitoneum well and would not change management in this unstable patient.
*Obtain a retrograde urethrogram*
- **Retrograde urethrogram (RUG)** is indicated when urethral injury is suspected (blood at meatus, high-riding prostate, perineal hematoma, inability to void).
- This patient has **normal external genitalia** and only microscopic hematuria (6 RBC/HPF), which is nonspecific in blunt trauma.
- The immediate life-threatening issue is **hemorrhagic shock from retroperitoneal bleeding**, not potential urethral injury. RUG would be an inappropriate delay in management and can be performed later if clinically indicated.
Trauma imaging principles US Medical PG Question 7: A trauma 'huddle' is called. Morphine is administered for pain. Low-flow oxygen is begun. A traumatic diaphragmatic rupture is suspected. Infusion of 0.9% saline is begun. Which of the following is the most appropriate next step in management?
- A. Chest fluoroscopy
- B. Barium study
- C. CT of the chest, abdomen, and pelvis (Correct Answer)
- D. MRI chest and abdomen
- E. ICU admission and observation
Trauma imaging principles Explanation: ***CT of the chest, abdomen, and pelvis***
- A suspected **traumatic diaphragmatic rupture** requires a comprehensive imaging study to assess the diaphragm, surrounding organs, and potential associated injuries.
- **CT scan** of the chest, abdomen, and pelvis provides detailed anatomical information, can identify herniated abdominal contents, and is essential for surgical planning in trauma settings.
*Chest fluoroscopy*
- While fluoroscopy can detect diaphragmatic motion, it is **less sensitive** for identifying tears or herniated contents in the **acute trauma setting**.
- It does not provide the comprehensive view of surrounding organs and associated injuries often needed in trauma.
*Barium study*
- A barium study is primarily used to evaluate the **gastrointestinal tract**, but it is generally **not the initial imaging modality** for diaphragmatic rupture due to its limited ability to visualize the diaphragm itself or other solid organ injuries.
- It would be performed after suspicion is increased or for very specific indications, not as a primary diagnostic tool.
*MRI chest and abdomen*
- While MRI offers excellent soft tissue contrast, its use in **acute trauma** is limited by **longer acquisition times**, potential contraindications with metallic implants (though less common in acute trauma), and lower availability compared to CT.
- CT remains the **gold standard** for rapid, comprehensive imaging in unstable trauma patients.
*ICU admission and observation*
- While observation in the ICU is important for monitoring and supportive care, it is **not the next step for diagnosis** of a suspected diaphragmatic rupture.
- Definitive diagnosis through imaging (CT) is crucial before determining specific management strategies, including potential surgical intervention.
Trauma imaging principles US Medical PG Question 8: A 45-year-old female presents to the emergency room as a trauma after a motor vehicle accident. The patient was a restrained passenger who collided with a drunk driver traveling approximately 45 mph. Upon impact, the passenger was able to extricate herself from the crushed car and was sitting on the ground at the scene of the accident. Her vitals are all stable. On physical exam, she is alert and oriented, speaking in complete sentences with a GCS of 15. She has a cervical spine collar in place and endorses exquisite cervical spine tenderness on palpation. Aside from her superficial abrasions on her right lower extremity, the rest of her examination including FAST exam is normal. Rapid hemoglobin testing is within normal limits. What is the next best step in management of this trauma patient?
- A. Remove the patient’s cervical collar immediately
- B. Discharge home and start physical therapy
- C. Initiate rapid sequence intubation.
- D. Consult neurosurgery immediately
- E. CT cervical spine (Correct Answer)
Trauma imaging principles Explanation: ***CT cervical spine***
- Given the patient's **mechanism of injury** (motor vehicle accident at 45 mph) and **cervical spine tenderness**, a CT cervical spine is the most appropriate next step to rule out a fracture or other significant injury.
- While the patient is alert and stable, the presence of **exquisite tenderness** mandates imaging to ensure no occult injury is missed that could lead to neurological compromise.
*Remove the patient’s cervical collar immediately*
- Removing the cervical collar prematurely in a trauma patient with cervical spine tenderness is dangerous, as it could lead to further damage if an **unstable fracture** is present.
- The collar should remain in place until imaging has ruled out a clinically significant cervical spine injury.
*Discharge home and start physical therapy*
- Discharging a patient with **cervical spine tenderness** after a high-impact motor vehicle accident without imaging is inappropriate and could result in severe consequences if an injury is present.
- Physical therapy would only be considered after a thorough workup has cleared any acute injury.
*Initiate rapid sequence intubation.*
- **Rapid sequence intubation (RSI)** is used for airway management in patients with impending or actual respiratory failure or inability to protect their airway.
- This patient is alert, speaking in complete sentences, has a GCS of 15, and stable vitals, indicating **no immediate need for intubation**.
*Consult neurosurgery immediately*
- While a neurosurgery consult may be necessary if an injury is identified, the immediate next step is to **diagnose the injury** with imaging.
- Consulting neurosurgery without definitive imaging results would be premature in this stable patient.
Trauma imaging principles US Medical PG Question 9: Three days after being admitted to the hospital because of a fall from the roof of a two-story building, a 27-year-old man is being monitored in the intensive care unit. On arrival, the patient was somnolent and not oriented to person, place, or time. A CT scan of the head showed an epidural hemorrhage that was 45 cm3 in size and a midline shift of 7 mm. Emergency surgery was performed with craniotomy and hematoma evacuation on the day of admission. Perioperatively, a bleeding vessel was identified and ligated. Postoperatively, the patient was transferred to the intensive care unit and placed on a ventilator. His temperature is 37°C (98.6°F), pulse is 67/min, and blood pressure is 117/78 mm Hg. The ventilator is set at a FiO2 of 55%, tidal volume of 520 mL, and positive end-expiratory pressure of 5.0 cm H2O. In addition to intravenous administration of fluids, which of the following is the most appropriate next step in managing this patient's nutrition?
- A. Enteral feeding via nasogastric tube (Correct Answer)
- B. Oral feeding
- C. Keep patient NPO
- D. Total parenteral nutrition
- E. Enteral feeding using a percutaneous endoscopic gastrostomy (PEG) tube
Trauma imaging principles Explanation: ***Enteral feeding via nasogastric tube***
- This patient has been **somnolent** and on a ventilator for 3 days after a significant head injury, indicating a prolonged period without oral intake and an inability to protect his airway for oral feeding. **Early enteral nutrition** via a nasogastric tube is preferred in critically ill patients, especially those with head injuries, as it helps maintain gut integrity and reduces complications compared to parenteral nutrition.
- The patient's **hemodynamic stability** (blood pressure and pulse are within a reasonable range for a ventilated patient) suggests he can tolerate enteral feeding, and there are no signs of gut ischemia or ileus that would contraindicate it.
*Enteral feeding using a percutaneous endoscopic gastrostomy (PEG) tube*
- While a PEG tube provides enteral nutrition, it is typically reserved for patients requiring **long-term enteral support** (usually more than 4-6 weeks) or those who cannot tolerate a nasogastric tube.
- Given that it has only been 3 days post-injury, a **less invasive method** like a nasogastric tube is initially preferred.
*Oral feeding*
- The patient is described as **somnolent** and on a ventilator, meaning he is not awake enough or able to protect his airway to safely receive oral feeding.
- Attempting oral feeding in this state carries a high risk of **aspiration pneumonia**.
*Keep patient NPO*
- Keeping the patient NPO (nil per os) for an extended period in critical illness is associated with several negative outcomes, including **gut mucosal atrophy, increased infection risk**, and poorer clinical outcomes.
- After 3 days, initiating nutritional support is crucial to prevent these complications.
*Total parenteral nutrition*
- **Total parenteral nutrition (TPN)** is generally considered a last resort when the gastrointestinal tract is non-functional or enteral feeding is contraindicated.
- TPN is associated with a **higher risk of complications**, such as central line infections, liver dysfunction, and metabolic disturbances, compared to enteral feeding.
Trauma imaging principles US Medical PG Question 10: A 24-year-old woman is brought to the emergency department after being assaulted. The paramedics report that the patient was found conscious and reported being kicked many times in the torso. She is alert and able to respond to questions. She denies any head trauma. She has a past medical history of endometriosis and a tubo-ovarian abscess that was removed surgically two years ago. Her only home medication is oral contraceptive pills. Her temperature is 98.5°F (36.9°C), blood pressure is 82/51 mmHg, pulse is 136/min, respirations are 24/min, and SpO2 is 94%. She has superficial lacerations to the face and severe bruising over her chest and abdomen. Her lungs are clear to auscultation bilaterally and her abdomen is soft, distended, and diffusely tender to palpation. Her skin is cool and clammy. Her FAST exam reveals fluid in the perisplenic space.
Which of the following is the next best step in management?
- A. Emergency laparotomy (Correct Answer)
- B. Abdominal radiograph
- C. Abdominal CT
- D. Fluid resuscitation
- E. Diagnostic peritoneal lavage
Trauma imaging principles Explanation: ***Emergency laparotomy***
- The patient presents with **hemodynamic instability** (BP 82/51 mmHg, HR 136/min) and a **positive FAST exam** showing fluid in the perisplenic space, indicating intra-abdominal hemorrhage.
- According to **ATLS guidelines**, a hemodynamically unstable patient with a positive FAST exam requires **immediate operative intervention** to control bleeding. This is the definitive management for ongoing hemorrhage.
- While fluid resuscitation is initiated simultaneously (en route to OR), **surgical control of the bleeding source** is the priority and should not be delayed.
*Fluid resuscitation*
- Fluid resuscitation with IV crystalloids is essential and should be started immediately in this patient with hypovolemic shock.
- However, in a patient with **uncontrolled intra-abdominal hemorrhage** (positive FAST, hemodynamic instability), fluids alone will not stop the bleeding. Continued fluid resuscitation without surgical intervention can lead to dilutional coagulopathy and worsening outcomes.
- Fluid resuscitation occurs **concurrently with preparation for surgery**, not as a separate step that delays definitive management.
*Diagnostic peritoneal lavage*
- DPL is an invasive diagnostic procedure that has largely been replaced by FAST exam in modern trauma care.
- Given that the **FAST is already positive**, DPL would provide no additional useful information and would only **delay definitive surgical management**.
- In hemodynamically unstable patients with positive FAST, proceeding directly to laparotomy is indicated.
*Abdominal radiograph*
- Plain radiographs have **limited sensitivity** for detecting intra-abdominal bleeding or solid organ injury.
- They may show free air (indicating hollow viscus perforation) but cannot assess for fluid or characterize solid organ injuries.
- This would **delay necessary operative intervention** without providing actionable information.
*Abdominal CT*
- CT abdomen is the imaging modality of choice for **hemodynamically stable** trauma patients to characterize injuries and guide management.
- For **unstable patients**, CT is **contraindicated** as it delays definitive treatment and removes the patient from a resuscitation environment where deterioration can be immediately addressed.
More Trauma imaging principles US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.