Secondary survey principles US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Secondary survey principles. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Secondary survey principles US Medical PG Question 1: A 67-year-old woman has fallen from the second story level of her home while hanging laundry. She was brought to the emergency department immediately and presented with severe abdominal pain. The patient is anxious, and her hands and feet feel very cold to the touch. There is no evidence of bone fractures, superficial skin wounds, or a foreign body penetration. Her blood pressure is 102/67 mm Hg, respirations are 19/min, pulse is 87/min, and temperature is 36.7°C (98.0°F). Her abdominal exam reveals rigidity and severe tenderness. A Foley catheter and nasogastric tube are inserted. The central venous pressure (CVP) is 5 cm H2O. The medical history is significant for hypertension. Which of the following is best indicated for the evaluation of this patient?
- A. X-Ray
- B. Ultrasound
- C. Peritoneal lavage
- D. CT scan (Correct Answer)
- E. Diagnostic laparotomy
Secondary survey principles Explanation: ***CT scan***
- A **CT scan of the abdomen and pelvis** is the most indicated imaging modality for evaluating blunt abdominal trauma due to its high sensitivity and specificity in detecting solid organ injuries, free fluid, and active bleeding.
- Given the patient's severe abdominal pain, rigidity, and tenderness after a significant fall, a CT scan will provide detailed anatomical information crucial for guiding further management.
*X-Ray*
- An **X-ray** is useful for detecting bone fractures, but it has limited utility in assessing soft tissue and organ injuries within the abdomen.
- It would not effectively visualize internal bleeding or organ damage, which are primary concerns in this patient given the mechanism of injury and symptoms.
*Ultrasound*
- An **ultrasound (FAST exam)** is effective for rapid detection of free fluid in the abdomen (indicating bleeding or fluid leakage) and can be done at the bedside.
- However, it is operator-dependent and less sensitive than CT for identifying specific organ injuries, retroperitoneal hematomas, or the source of bleeding.
*Peritoneal lavage*
- **Diagnostic peritoneal lavage (DPL)** is an invasive procedure primarily used to detect intra-abdominal bleeding in hemodynamically unstable patients, but it has largely been replaced by ultrasound and CT in stable patients.
- While it can detect blood, it is less specific for identifying the source of bleeding and does not provide anatomical detail, and carries risks of complications like bowel perforation.
*Diagnostic laparotomy*
- **Diagnostic laparotomy** is a surgical procedure to directly visualize abdominal contents and is indicated in cases of clear signs of peritonitis, hemodynamic instability with confirmed intra-abdominal bleeding, or evisceration.
- It is an invasive intervention and would not be the initial diagnostic step in a hemodynamically stable patient without clear indication for immediate surgery.
Secondary survey principles US Medical PG Question 2: A 36-year-old male is taken to the emergency room after jumping from a building. Bilateral fractures to the femur were stabilized at the scene by emergency medical technicians. The patient is lucid upon questioning and his vitals are stable. Pain only at his hips was elicited. Cervical exam was not performed. What is the best imaging study for this patient?
- A. AP and lateral radiographs of hips
- B. Lateral radiograph (x-ray) of hips
- C. Magnetic resonance imaging (MRI) of hips, knees, lumbar, and cervical area
- D. Anterior-posterior (AP) and lateral radiographs of hips, knees, lumbar, and cervical area
- E. Computed tomography (CT) scan of cervical spine, hips, and lumbar area (Correct Answer)
Secondary survey principles Explanation: ***Computed tomography (CT) scan of cervical spine, hips, and lumbar area***
- In **high-energy trauma** (fall from height), a CT scan is the **gold standard** for evaluating the **spine and pelvis**, providing detailed cross-sectional images superior to plain radiographs.
- Since the **cervical exam was not performed**, cervical spine imaging is **mandatory** per ATLS (Advanced Trauma Life Support) protocols. High-energy falls carry significant risk of **cervical spine injury** even without obvious neurological symptoms.
- CT allows comprehensive assessment of **hip fractures, pelvic injuries, and the entire spine** (cervical, thoracic, lumbar), identifying both obvious and **subtle fractures** that may be missed on plain films.
- This approach provides the most **efficient and thorough evaluation** in the acute trauma setting, allowing for appropriate surgical planning and ruling out life-threatening spinal instability.
*AP and lateral radiographs of hips*
- Plain radiographs provide **limited detail** and may **miss subtle fractures**, particularly in complex areas like the pelvis and acetabulum.
- This option **fails to address cervical spine clearance**, which is essential in all high-energy trauma patients, especially when cervical exam has not been performed.
- Radiographs are insufficient for **comprehensive trauma evaluation** after a fall from height.
*Lateral radiograph (x-ray) of hips*
- A single lateral view is **grossly insufficient** for evaluating hip and pelvic fractures, providing only a **two-dimensional perspective** that can miss significant injuries.
- This option **completely neglects spinal evaluation**, which is dangerous in an uncleared trauma patient with a high-energy mechanism.
*Magnetic resonance imaging (MRI) of hips, knees, lumbar, and cervical area*
- While MRI excels at evaluating **soft tissues, ligaments, and bone marrow**, it is **not the initial imaging modality** for acute bony trauma due to longer scan times and lower sensitivity for acute fractures compared to CT.
- MRI is **time-consuming and impractical** in the emergency setting for initial fracture assessment, potentially delaying definitive treatment.
- CT is superior for evaluating **acute skeletal injuries** in the trauma bay.
*Anterior-posterior (AP) and lateral radiographs of hips, knees, lumbar, and cervical area*
- Multiple plain radiographs have **limited sensitivity** for complex or non-displaced fractures, particularly in the **spine and pelvis**, making them inadequate for high-energy trauma evaluation.
- Obtaining multiple radiographic views requires **numerous patient repositionings**, which risks further injury if **spinal instability** is present.
- Plain films provide significantly **less diagnostic information** than CT scanning for trauma assessment.
Secondary survey principles US Medical PG Question 3: A 15-year-old boy is brought to the emergency department one hour after sustaining an injury during football practice. He collided head-on into another player while wearing a mouthguard and helmet. Immediately after the collision he was confused but able to use appropriate words. He opened his eyes spontaneously and followed commands. There was no loss of consciousness. He also had a headache with dizziness and nausea. He is no longer confused upon arrival. He feels well. Vital signs are within normal limits. He is fully alert and oriented. His speech is organized and he is able to perform tasks demonstrating full attention, memory, and balance. Neurological examination shows no abnormalities. There is mild tenderness to palpation over the crown of his head but no signs of skin break or fracture. Which of the following is the most appropriate next step?
- A. Discharge without activity restrictions
- B. Discharge and refrain from all physical activity for one week
- C. Observe for 6 hours in the ED and refrain from contact sports for one week (Correct Answer)
- D. Administer prophylactic levetiracetam and observe for 24 hours
- E. Administer prophylactic phenytoin and observe for 24 hours
Secondary survey principles Explanation: ***Observe for 6 hours in the ED and refrain from contact sports for one week***
- This patient experienced a brief period of **confusion, headache, dizziness**, and **nausea** immediately after a head injury, which are symptoms consistent with a **mild traumatic brain injury (mTBI)** or **concussion**.
- Although his symptoms have resolved at presentation, observation in the ED for a few hours is prudent to ensure no delayed onset of more severe symptoms, and he should **refrain from contact sports** for at least one week as part of concussion management.
*Discharge without activity restrictions*
- Discharging without activity restrictions is unsafe given the initial symptoms of **confusion** and the potential for delayed symptom presentation or complications from a concussion.
- Concussion management requires a period of **physical and cognitive rest** to allow the brain to heal and prevent **second impact syndrome**.
*Discharge and refrain from all physical activity for one week*
- While refraining from all physical activity for one week is part of concussion management, discharging immediately without any observation period after initial neurological symptoms could be risky.
- An observation period allows for monitoring of any **worsening neurological signs** or symptoms that might indicate a more serious injury.
*Administer prophylactic levetiracetam and observe for 24 hours*
- **Prophylactic anticonvulsants** like levetiracetam are typically not recommended for routine management of **mild traumatic brain injury** or concussion.
- Their use is generally reserved for patients with more severe injuries, evolving conditions, or those who have had **seizures post-trauma**.
*Administer prophylactic phenytoin and observe for 24 hours*
- Similar to levetiracetam, **phenytoin** is an anticonvulsant and its prophylactic use is not indicated for **mild head injuries** or concussions.
- Anticonvulsant prophylaxis is associated with potential side effects and is reserved for specific high-risk scenarios, such as **severe TBI** or **penetrating head trauma**.
Secondary survey principles US Medical PG Question 4: The medical student on the pediatric cardiology team is examining a 9-year-old girl who was referred by her primary care physician for unexplained hypertension. She is accompanied by her mother who reveals that the child is generally well but has been significantly less active than her peers for the past year. On exam, the medical student notes a thin girl in no apparent distress appearing slightly younger than stated age. Vital signs reveal a BP is 160/80, HR 80, RR 16. Physical exam is notable only for a clicking sound is noted around the time of systole but otherwise the cardiac exam is normal. Pedal pulses could not be palpated. Which of the following physical exam findings was most likely missed by both the medical student and primary care physician?
- A. Long philtrum
- B. Prominent occiput
- C. Webbed neck (Correct Answer)
- D. Cleft palate
- E. Single palmar crease
Secondary survey principles Explanation: ***Webbed neck***
- The combination of **hypertension** with **unpalpable pedal pulses** and a **systolic click** in a pediatric patient strongly suggests **coarctation of the aorta**.
- **Webbed neck** (or **pterygium colli**) is a classic phenotypic feature associated with **Turner syndrome**, which frequently co-occurs with coarctation of the aorta.
*Long philtrum*
- A **long philtrum** is a craniofacial feature sometimes associated with certain genetic syndromes like **fetal alcohol syndrome** or **Marfan syndrome**, but it is not specifically linked to coarctation of the aorta or Turner syndrome.
- While these syndromes can have cardiovascular manifestations, a long philtrum does not directly point to the specific findings presented.
*Prominent occiput*
- A **prominent occiput** is a non-specific finding that can be seen in various conditions, including some **chromosomal abnormalities** or **skeletal dysplasias**.
- It is not a characteristic feature of **Turner syndrome** or **coarctation of the aorta**.
*Cleft palate*
- **Cleft palate** is a birth defect affecting the roof of the mouth, often associated with a wide range of genetic or environmental factors.
- While patients with cleft palate can have associated congenital heart defects, it is not a direct or common association with **Turner syndrome** or **coarctation of the aorta**.
*Single palmar crease*
- A **single palmar crease** (simian crease) is a dermatoglyphic feature often associated with **Down syndrome** (Trisomy 21).
- While Down syndrome is associated with various congenital heart defects (e.g., AV septal defect), it is not typically associated with **coarctation of the aorta** or **Turner syndrome**.
Secondary survey principles US Medical PG Question 5: A 78-year-old man is brought in to the emergency department by ambulance after his wife noticed that he began slurring his speech and had developed facial asymmetry during dinner approximately 30 minutes ago. His past medical history is remarkable for hypertension and diabetes. His temperature is 99.1°F (37.3°C), blood pressure is 154/99 mmHg, pulse is 89/min, respirations are 12/min, and oxygen saturation is 98% on room air. Neurologic exam reveals right upper and lower extremity weakness and an asymmetric smile. Which of the following is the next best step in management?
- A. Alteplase
- B. MRI brain
- C. CT head (Correct Answer)
- D. Aspirin
- E. CTA head
Secondary survey principles Explanation: ***CT head***
- A **non-contrast CT head** is the immediate priority to differentiate between ischemic and hemorrhagic stroke, which is critical for guiding subsequent treatment decisions.
- Given the patient's acute neurological deficits (slurred speech, facial asymmetry, weakness) and vascular risk factors (hypertension, diabetes), **stroke is highly suspected**, and identifying intracerebral hemorrhage is crucial before considering thrombolytic therapy.
*Alteplase*
- **Alteplase** (tPA) is a thrombolytic agent used for acute ischemic stroke, but its administration is **contraindicated in hemorrhagic stroke**.
- Initiating alteplase without first ruling out hemorrhage with a CT scan could lead to catastrophic bleeding.
*MRI brain*
- While an **MRI brain** can provide more detailed imaging of stroke, it is typically **not the initial imaging modality** in the emergency setting due to longer acquisition times and limited availability, especially when emergent differentiation between ischemic and hemorrhagic stroke is needed.
- Its use is usually reserved for cases where the CT is inconclusive or for later evaluation.
*Aspirin*
- **Aspirin** is an antiplatelet agent used in the management of ischemic stroke, but it should **not be given until a hemorrhagic stroke has been ruled out** via CT head.
- Administering aspirin in the context of an intracerebral hemorrhage could worsen bleeding.
*CTA head*
- A **CT angiography (CTA) head** is used to visualize the cerebral vasculature and identify large vessel occlusions, which can guide thrombectomy decisions in ischemic stroke.
- However, performing a **non-contrast CT head is a prerequisite** to rule out hemorrhage before proceeding with CTA or any other advanced imaging or therapeutic interventions.
Secondary survey principles US Medical PG Question 6: A 27-year-old soldier is brought to the emergency department of a military hospital 20 minutes after being involved in a motor vehicle accident during a training exercise. He was an unrestrained passenger. On arrival, he has shortness of breath and chest pain. He appears pale and anxious. His temperature is 37°C (98.6°F), pulse is 110/min, respirations are 20/min, and blood pressure is 100/65 mm Hg. He is alert and oriented to person, place, and time. Examination shows pale conjunctivae and mucous membranes. There is bruising on the chest, extremities, and abdomen. The lungs are clear to auscultation. He has normal heart sounds and flat neck veins. The abdomen is flat, soft, and mildly tender. The remainder of the physical examination shows no abnormalities. High-flow oxygen is applied, and intravenous fluid resuscitation is begun. A chest x-ray is obtained. Which of the following is the most appropriate next step in management?
- A. Placement of a chest tube
- B. Pericardiocentesis
- C. Abdominal ultrasonography
- D. Intubation with positive pressure ventilation
- E. CT scan of the chest with contrast (Correct Answer)
Secondary survey principles Explanation: ***CT scan of the chest with contrast***
- The patient has suffered a **blunt chest trauma** with symptoms including shortness of breath, chest pain, and signs of potential internal bleeding (pale, anxious, tachycardia, mild hypotension).
- A chest X-ray was performed; however, a **CT scan with contrast** is essential to further evaluate for **aortic injury**, **pulmonary contusions**, or other subtle thoracic injuries that may not be evident on plain radiographs, especially given the mechanism of injury (unrestrained passenger in a MVA).
*Placement of a chest tube*
- This intervention is indicated for conditions like **pneumothorax** or **hemothorax**, which would typically present with **diminished breath sounds** on the affected side or characteristic X-ray findings.
- The patient's lungs are described as **clear to auscultation**, and no specific X-ray findings are mentioned that would necessitate immediate chest tube placement.
*Pericardiocentesis*
- This procedure is performed for **cardiac tamponade**, which would manifest with muffled heart sounds, jugular venous distention, and pulsus paradoxus.
- The patient has **normal heart sounds** and **flat neck veins**, making cardiac tamponade less likely.
*Abdominal ultrasonography*
- While the patient has bruising and mild tenderness in the abdomen, suggesting potential **abdominal injury**, the primary life-threatening concerns based on his presentation (shortness of breath, chest pain, chest X-ray ordered) are thoracic.
- A **Focused Assessment with Sonography for Trauma (FAST) exam** would be appropriate if the abdominal tenderness was more pronounced or if there were signs of active intra-abdominal bleeding, but the immediate priority is to rule out life-threatening thoracic injuries.
*Intubation with positive pressure ventilation*
- This is indicated for patients with **respiratory failure** or an inability to protect their airway. The patient's respiratory rate is 20/min (within normal limits), and he is **alert and oriented**.
- While high-flow oxygen and fluid resuscitation have been initiated, there is no indication of impending respiratory collapse that would necessitate immediate intubation.
Secondary survey principles US Medical PG Question 7: A 65-year-old man presents to his primary-care doctor for a 2-month history of dizziness. He describes feeling unsteady on his feet or like he's swaying from side-to-side; he's also occasionally had a room-spinning sensation. He first noticed it when he was in the front yard playing catch with his grandson, and he now also reliably gets it when throwing the frisbee with his dog. The dizziness only happens during these times, and it goes away after a couple of minutes of rest. His medical history is notable for type 2 diabetes mellitus treated with metformin. His vital signs are within normal limits in the office. The physical exam is unremarkable. Which of the following is the next best test for this patient?
- A. Ankle-brachial index
- B. Doppler ultrasound (Correct Answer)
- C. Transthoracic echocardiogram
- D. CT head (noncontrast)
- E. Electrocardiogram
Secondary survey principles Explanation: ***Doppler ultrasound***
- The patient's dizziness occurring specifically during **upper extremity exertion** (playing catch, throwing frisbee) that resolves with rest is classic for **subclavian steal syndrome**.
- In subclavian steal, stenosis of the subclavian artery proximal to the vertebral artery origin causes **reversed flow in the vertebral artery** during arm exercise, "stealing" blood from the posterior circulation and causing vertebrobasilar insufficiency symptoms.
- **Doppler ultrasound** of the subclavian and vertebral arteries is the appropriate initial test to demonstrate reversed vertebral flow and subclavian stenosis. This can be confirmed with provocative maneuvers (arm exercise during the study).
- The patient's diabetes increases his risk for atherosclerotic disease, making this diagnosis more likely.
*CT head (noncontrast)*
- While CT head can evaluate for stroke or structural brain lesions, it would **not visualize the vascular stenosis** causing subclavian steal syndrome.
- The episodic nature triggered by specific arm movements and complete resolution with rest makes an acute structural brain lesion unlikely.
- CT head would be appropriate if symptoms were persistent, progressive, or associated with focal neurological deficits.
*Ankle-brachial index*
- ABI is used to diagnose **peripheral artery disease** affecting the lower extremities, typically presenting with **intermittent claudication** (leg pain with walking).
- This does not evaluate the upper extremity or cerebrovascular circulation relevant to this patient's symptoms.
*Electrocardiogram*
- ECG evaluates cardiac rhythm and ischemia but would not diagnose the **vascular steal phenomenon** causing his symptoms.
- Cardiac arrhythmias typically cause syncope or presyncope rather than positional dizziness triggered by specific arm movements.
- While arrhythmias should be considered in the differential, the clear association with arm exercise points to a vascular steal phenomenon.
*Transthoracic echocardiogram*
- TTE assesses cardiac structure and function (valves, chambers, ejection fraction) but does not evaluate the **extracranial vasculature**.
- Cardiac causes of dizziness (e.g., severe aortic stenosis) would more likely present with exertional syncope rather than dizziness specifically with arm movements.
- The symptom pattern does not suggest primary cardiac pathology.
Secondary survey principles US Medical PG Question 8: A 28-year-old male presents to his primary care physician with complaints of intermittent abdominal pain and alternating bouts of constipation and diarrhea. His medical chart is not significant for any past medical problems or prior surgeries. He is not prescribed any current medications. Which of the following questions would be the most useful next question in eliciting further history from this patient?
- A. "Does the diarrhea typically precede the constipation, or vice-versa?"
- B. "Is the diarrhea foul-smelling?"
- C. "Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life"
- D. "Are the symptoms worse in the morning or at night?"
- E. "Can you tell me more about the symptoms you have been experiencing?" (Correct Answer)
Secondary survey principles Explanation: ***Can you tell me more about the symptoms you have been experiencing?***
- This **open-ended question** encourages the patient to provide a **comprehensive narrative** of their symptoms, including details about onset, frequency, duration, alleviating/aggravating factors, and associated symptoms, which is crucial for diagnosis.
- In a patient presenting with vague, intermittent symptoms like alternating constipation and diarrhea, allowing them to elaborate freely can reveal important clues that might not be captured by more targeted questions.
*Does the diarrhea typically precede the constipation, or vice-versa?*
- While knowing the sequence of symptoms can be helpful in understanding the **pattern of bowel dysfunction**, it is a very specific question that might overlook other important aspects of the patient's experience.
- It prematurely narrows the focus without first obtaining a broad understanding of the patient's overall symptomatic picture.
*Is the diarrhea foul-smelling?*
- Foul-smelling diarrhea can indicate **malabsorption** or **bacterial overgrowth**, which are important to consider in some gastrointestinal conditions.
- However, this is a **specific symptom inquiry** that should follow a more general exploration of the patient's symptoms, as it may not be relevant if other crucial details are missed.
*Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life*
- Quantifying pain intensity is useful for assessing the **severity of discomfort** and monitoring changes over time.
- However, for a patient with intermittent rather than acute, severe pain, understanding the **character, location, and triggers** of the pain is often more diagnostically valuable than just a numerical rating initially.
*Are the symptoms worse in the morning or at night?*
- Diurnal variation can be relevant in certain conditions, such as inflammatory bowel diseases where nocturnal symptoms might be more concerning, or functional disorders whose symptoms might be stress-related.
- This is another **specific question** that should come after gathering a more complete initial picture of the patient's symptoms to ensure no key information is overlooked.
Secondary survey principles US Medical PG Question 9: A 24-year-old man is brought to the emergency department 30 minutes after being involved in a high-speed motor vehicle collision in which he was a restrained driver. On arrival, he is alert and oriented. His pulse is 112/min, respirations are 29/min, and blood pressure is 100/60 mm Hg. The pupils are equal and reactive to light. There is a 3-cm laceration over the forehead and multiple bruises over the trunk. The lungs are clear to auscultation. Cardiac examination shows no abnormalities. The abdomen is soft and nontender. The right knee is swollen and tender; range of motion is limited by pain. Infusion of 0.9% saline is begun and intravenous acetaminophen is administered. Two hours later, blood-tinged fluid spontaneously drains from both nostrils, and is made worse by leaning forward. On a piece of gauze, it shows up as a rapidly-expanding clear ring of fluid surrounding blood. Further evaluation of this patient is most likely to show which of the following?
- A. Numbness of upper cheek area
- B. Retroauricular ecchymosis
- C. Bilateral periorbital ecchymosis (Correct Answer)
- D. Cranial nerve XII palsy
- E. Carotid artery dissection
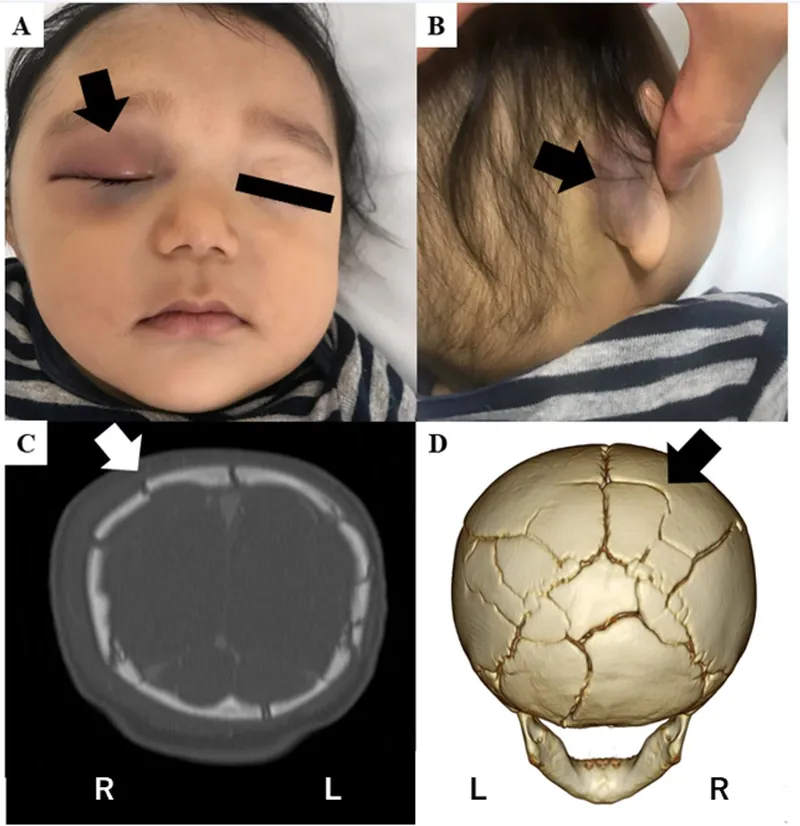
Secondary survey principles Explanation: **Bilateral periorbital ecchymosis**
- The clinical presentation, including head trauma from a **high-speed motor vehicle collision**, neurological symptoms like **blood-tinged fluid draining from both nostrils with a halo sign**, and hemodynamic instability (tachycardia and hypotension), points towards a **basilar skull fracture**.
- **Bilateral periorbital ecchymosis** (raccoon eyes) is a classic sign of a basilar skull fracture, particularly one involving the **anterior cranial fossa**, indicating extravasation of blood into the periorbital tissues.
*Numbness of upper cheek area*
- **Numbness of the upper cheek area** is associated with injury to the **infraorbital nerve**, which often occurs with **maxillary (Le Fort II or III) fractures** or **orbital floor fractures**.
- While midface fractures can occur in severe trauma, the **halo sign** from the nostrils is more indicative of a **CSF leak** associated with a **basilar skull fracture**, rather than isolated maxillary injury.
*Retroauricular ecchymosis*
- **Retroauricular ecchymosis** (Battle's sign) is also a sign of a **basilar skull fracture**, but it specifically indicates a fracture involving the **middle cranial fossa** and the **temporal bone**.
- While possible, the spontaneous draining of CSF from the nostrils (rhinorrhea) is more directly linked to an **anterior cranial fossa fracture** and involvement of the **cribriform plate**, making bilateral periorbital ecchymosis a more likely and specific finding in this context.
*Cranial nerve XII palsy*
- **Cranial nerve XII (hypoglossal) palsy** would result in **tongue deviation** and weakness, typically associated with injuries to the **posterior cranial fossa** or the **neck**.
- This is not a common finding with the presented symptoms of **rhinorrhea with a halo sign**, which points to an **anterior cranial fossa fracture**.
*Carotid artery dissection*
- **Carotid artery dissection** can occur after significant trauma and may present with headaches, neck pain, and focal neurological deficits such as **hemiparesis** or **cranial nerve deficits (e.g., Horner's syndrome)**.
- While trauma increases the risk, the specific symptom of **CSF rhinorrhea with a halo sign** is not characteristic of a carotid dissection but rather indicative of a **communication between the subarachnoid space and the nasal cavity** due to a skull base fracture.
Secondary survey principles US Medical PG Question 10: A 67-year-old man is brought to the emergency room after being involved in a traffic accident. He currently complains of bilateral hip pain. His vital signs are within the normal range, and he is hemodynamically stable. The pelvic compression test is positive. External genitalia appears normal, except there is blood at the urethral meatus and a contusion at the base of the scrotum. Digital rectal examination (DRE) shows a high-riding ballotable prostate. An X-ray reveals the presence of a pelvic fracture. Which of the following initial actions is the most appropriate for this patient?
- A. Insert a Foley catheter
- B. Take the patient emergently to the operating room and check for a urethral injury with IV indigo carmine
- C. Obtain a retrograde urethrogram (RUG), including a pre-injection kidney, ureter, and bladder (KUB) film (Correct Answer)
- D. Obtain a urinalysis to detect microscopic hematuria
- E. Perform a suprapubic cystostomy
Secondary survey principles Explanation: ***Obtain a retrograde urethrogram (RUG), including a pre-injection kidney, ureter, and bladder (KUB) film***
- The combination of **blood at the urethral meatus**, a **high-riding ballotable prostate** on DRE, and a **pelvic fracture** are classic signs of a **urethral injury**, specifically a posterior urethral tear.
- A **retrograde urethrogram (RUG)** is the gold standard diagnostic test to confirm urethral injury and determine its location and extent, which is crucial before any attempt at catheterization.
*Insert a Foley catheter*
- **Insertion of a Foley catheter is contraindicated** in suspected urethral injuries, as it can worsen a partial tear into a complete transection or create a false passage.
- Doing so blindly could lead to further damage, stricture formation, and increased morbidity.
*Take the patient emergently to the operating room and check for a urethral injury with IV indigo carmine*
- This approach is premature before confirming the diagnosis and extent of urethral injury; **indigo carmine is used to assess ureteral integrity**, not urethral injury.
- Surgical exploration for urethral injury as an initial step is typically reserved for cases where RUG cannot be performed or for severe complex injuries with other indications for immediate surgery.
*Obtain a urinalysis to detect microscopic hematuria*
- While microscopic hematuria would likely be present, it is a **nonspecific finding** and does not provide information about the integrity of the urethra itself.
- It would not change the need for a RUG to assess for urethral injury in the presence of more specific signs.
*Perform a suprapubic cystostomy*
- A **suprapubic cystostomy** is the appropriate method for urinary diversion in a patient with a confirmed urethral injury if a Foley catheter cannot be safely placed.
- However, it is an intervention chosen *after* diagnosing the injury with a RUG, not the initial diagnostic step itself.
More Secondary survey principles US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.