Exposure and environmental control US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Exposure and environmental control. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Exposure and environmental control US Medical PG Question 1: A 34-year-old male is brought to the emergency department by fire and rescue following a motor vehicle accident in which the patient was an unrestrained driver. The paramedics report that the patient was struck from behind by a drunk driver. He was mentating well at the scene but complained of pain in his abdomen. The patient has no known past medical history. In the trauma bay, his temperature is 98.9°F (37.2°C), blood pressure is 86/51 mmHg, pulse is 138/min, and respirations are 18/min. The patient is somnolent but arousable to voice and pain. His lungs are clear to auscultation bilaterally. He is diffusely tender to palpation on abdominal exam with bruising over the left upper abdomen. His distal pulses are thready, and capillary refill is delayed bilaterally. Two large-bore peripheral intravenous lines are placed to bolus him with intravenous 0.9% saline. Chest radiograph shows multiple left lower rib fractures.
Which of the following parameters is most likely to be seen in this patient?
- A. Increased cardiac output
- B. Increased mixed venous oxygen saturation
- C. Decreased pulmonary capillary wedge pressure (Correct Answer)
- D. Decreased systemic vascular resistance
- E. Increased right atrial pressure
Exposure and environmental control Explanation: ***Decreased pulmonary capillary wedge pressure***
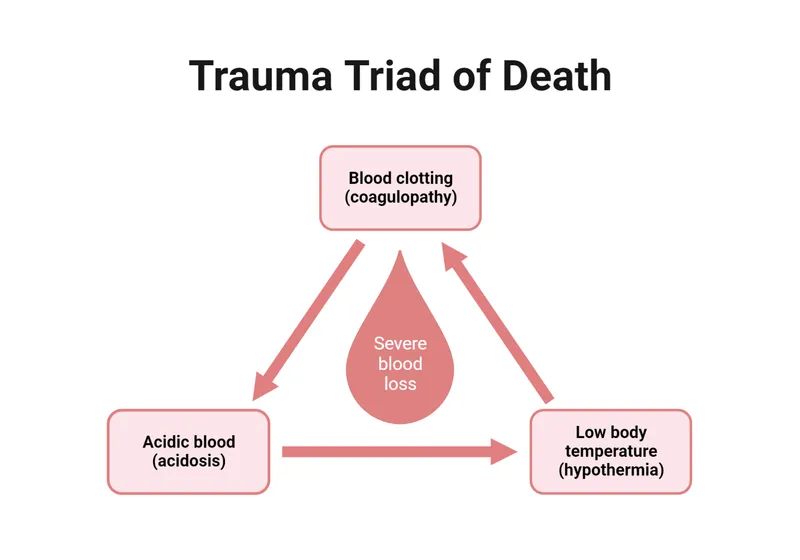
- The patient presents with classic signs of **hemorrhagic shock** (hypotension, tachycardia, somnolence, abdominal bruising, thready pulses) due to trauma, likely involving the spleen or kidney given the left upper abdominal bruising and rib fractures.
- **Decreased pulmonary capillary wedge pressure (PCWP)** is expected in hypovolemic shock because it reflects left atrial and left ventricular end-diastolic pressure, which will be low due to reduced venous return and intravascular volume.
*Increased cardiac output*
- In **hemorrhagic shock**, the body attempts to compensate by increasing heart rate, but overall **cardiac output is typically decreased** due to profound reduction in preload (venous return) from blood loss.
- While heart rate is elevated, the stroke volume is severely diminished, leading to a net decrease in cardiac output despite compensatory efforts.
*Increased mixed venous oxygen saturation*
- **Mixed venous oxygen saturation (SvO2)** is generally **decreased in hemorrhagic shock** due to increased oxygen extraction by tissues.
- Inadequate oxygen delivery to the tissues forces them to extract more oxygen from the blood, leading to a lower SvO2.
*Decreased systemic vascular resistance*
- In **hemorrhagic shock**, the body activates compensatory mechanisms, including generalized **vasoconstriction**, to maintain blood pressure and prioritize blood flow to vital organs.
- This leads to an **increased systemic vascular resistance (SVR)**, not decreased, as reflected by the thready distal pulses and delayed capillary refill.
*Increased right atrial pressure*
- **Right atrial pressure (RAP)**, representing CVP, is typically **decreased in hemorrhagic shock** due to reduced circulating blood volume.
- A lower RAP indicates decreased venous return to the heart, a hallmark of hypovolemia.
Exposure and environmental control US Medical PG Question 2: A trauma 'huddle' is called. Morphine is administered for pain. Low-flow oxygen is begun. A traumatic diaphragmatic rupture is suspected. Infusion of 0.9% saline is begun. Which of the following is the most appropriate next step in management?
- A. Chest fluoroscopy
- B. Barium study
- C. CT of the chest, abdomen, and pelvis (Correct Answer)
- D. MRI chest and abdomen
- E. ICU admission and observation
Exposure and environmental control Explanation: ***CT of the chest, abdomen, and pelvis***
- A suspected **traumatic diaphragmatic rupture** requires a comprehensive imaging study to assess the diaphragm, surrounding organs, and potential associated injuries.
- **CT scan** of the chest, abdomen, and pelvis provides detailed anatomical information, can identify herniated abdominal contents, and is essential for surgical planning in trauma settings.
*Chest fluoroscopy*
- While fluoroscopy can detect diaphragmatic motion, it is **less sensitive** for identifying tears or herniated contents in the **acute trauma setting**.
- It does not provide the comprehensive view of surrounding organs and associated injuries often needed in trauma.
*Barium study*
- A barium study is primarily used to evaluate the **gastrointestinal tract**, but it is generally **not the initial imaging modality** for diaphragmatic rupture due to its limited ability to visualize the diaphragm itself or other solid organ injuries.
- It would be performed after suspicion is increased or for very specific indications, not as a primary diagnostic tool.
*MRI chest and abdomen*
- While MRI offers excellent soft tissue contrast, its use in **acute trauma** is limited by **longer acquisition times**, potential contraindications with metallic implants (though less common in acute trauma), and lower availability compared to CT.
- CT remains the **gold standard** for rapid, comprehensive imaging in unstable trauma patients.
*ICU admission and observation*
- While observation in the ICU is important for monitoring and supportive care, it is **not the next step for diagnosis** of a suspected diaphragmatic rupture.
- Definitive diagnosis through imaging (CT) is crucial before determining specific management strategies, including potential surgical intervention.
Exposure and environmental control US Medical PG Question 3: A 78-year-old woman is brought to the emergency ward by her son for lethargy and generalized weakness. The patient speaks in short utterances and does not make eye contact with the provider or her son throughout the interview and examination. You elicit that the patient lives with her son and daughter-in-law, and she reports vague weakness for the last couple days. The emergency room provider notices 3-4 healing bruises on the patient's upper extremities; otherwise, examination is not revealing. Routine chemistries and blood counts are unremarkable; non-contrast head CT demonstrates normal age-related changes. Which of the following is the most appropriate next step in management?
- A. Ask the patient's son to leave the room (Correct Answer)
- B. Question the patient's son regarding the home situation
- C. Call Adult Protective Services to report the patient's son
- D. Perform lumbar puncture
- E. Question the patient regarding abuse or neglect
Exposure and environmental control Explanation: ***Ask the patient's son to leave the room***
- The patient's **lethargy**, **non-engagement**, and **healing bruises** raise strong suspicions for elder abuse or neglect. Removing the son allows for a private interview, which is crucial for her to feel safe enough to disclose information.
- In situations of suspected abuse, it is paramount to prioritize the **patient's safety and ability to speak freely** without the presence of the suspected abuser.
*Question the patient's son regarding the home situation*
- Questioning the son directly at this point may escalate the situation or make the patient even less likely to disclose abuse, as she is likely **frightened or coerced**.
- This step is premature and should only occur after a private interview with the patient, and potentially with the involvement of Protective Services.
*Call Adult Protective Services to report the patient's son*
- While reporting to **Adult Protective Services** is a critical step if abuse is confirmed, it is not the immediate first action until a private interview with the patient has been conducted to gather more information.
- Making a report without attempting to speak with the patient alone first can hinder the investigation and potentially jeopardize her safety if the abuser is alerted prematurely.
*Perform lumbar puncture*
- A lumbar puncture is an invasive procedure generally performed to diagnose **central nervous system infections** or **inflammatory conditions**.
- There are no clinical indications (e.g., fever, meningeal signs, focal neurological deficits) to suggest a need for a lumbar puncture, especially given the history and physical findings that point towards abuse.
*Question the patient regarding abuse or neglect*
- While it's important to question the patient about abuse, it must be done in a **safe and private environment** where she feels comfortable speaking freely.
- Questioning her while the suspected abuser (her son) is present would likely yield unhelpful responses due to fear or intimidation, as seen by her lack of eye contact and short utterances.
Exposure and environmental control US Medical PG Question 4: A 45-year-old man is found deceased in his bedroom. Time of death needs to be established for legal purposes. The body temperature is 32°C (89.6°F), and the ambient temperature is 20°C (68°F). Rigor mortis is complete in all muscle groups. Assuming normal conditions, which of the following best estimates the postmortem interval?
- A. 24-26 hours
- B. 6-8 hours
- C. 12-14 hours (Correct Answer)
- D. 2-4 hours
Exposure and environmental control Explanation: ***12-14 hours***
- **Complete rigor mortis** in all muscle groups typically occurs between **12-18 hours** postmortem.
- The body temperature of 32°C (89.6°F) with an ambient temperature of 20°C (68°F) indicates significant cooling, suggesting a **postmortem interval of several hours**, consistent with the stages of rigor mortis.
- This timeframe represents the peak of complete rigor mortis across all muscle groups.
*24-26 hours*
- By **24-36 hours**, rigor mortis would typically be **passing or completely absent** due to autolysis and decomposition.
- The body temperature would also be closer to the ambient temperature at this stage, unless other factors were involved.
*6-8 hours*
- At 6-8 hours, rigor mortis would typically be **developing or fully established in smaller muscles** (like the face and neck), but likely **not complete in all muscle groups**.
- Body temperature would be higher than 32°C, as a significant drop to 32°C would take longer.
*2-4 hours*
- At this early stage, rigor mortis would likely be **absent** or only just beginning to develop in the smallest muscles.
- The body temperature would also be much closer to normal body temperature (37°C or 98.6°F), with only a slight drop.
Exposure and environmental control US Medical PG Question 5: A 28-year-old male presents to his primary care physician with complaints of intermittent abdominal pain and alternating bouts of constipation and diarrhea. His medical chart is not significant for any past medical problems or prior surgeries. He is not prescribed any current medications. Which of the following questions would be the most useful next question in eliciting further history from this patient?
- A. "Does the diarrhea typically precede the constipation, or vice-versa?"
- B. "Is the diarrhea foul-smelling?"
- C. "Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life"
- D. "Are the symptoms worse in the morning or at night?"
- E. "Can you tell me more about the symptoms you have been experiencing?" (Correct Answer)
Exposure and environmental control Explanation: ***Can you tell me more about the symptoms you have been experiencing?***
- This **open-ended question** encourages the patient to provide a **comprehensive narrative** of their symptoms, including details about onset, frequency, duration, alleviating/aggravating factors, and associated symptoms, which is crucial for diagnosis.
- In a patient presenting with vague, intermittent symptoms like alternating constipation and diarrhea, allowing them to elaborate freely can reveal important clues that might not be captured by more targeted questions.
*Does the diarrhea typically precede the constipation, or vice-versa?*
- While knowing the sequence of symptoms can be helpful in understanding the **pattern of bowel dysfunction**, it is a very specific question that might overlook other important aspects of the patient's experience.
- It prematurely narrows the focus without first obtaining a broad understanding of the patient's overall symptomatic picture.
*Is the diarrhea foul-smelling?*
- Foul-smelling diarrhea can indicate **malabsorption** or **bacterial overgrowth**, which are important to consider in some gastrointestinal conditions.
- However, this is a **specific symptom inquiry** that should follow a more general exploration of the patient's symptoms, as it may not be relevant if other crucial details are missed.
*Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life*
- Quantifying pain intensity is useful for assessing the **severity of discomfort** and monitoring changes over time.
- However, for a patient with intermittent rather than acute, severe pain, understanding the **character, location, and triggers** of the pain is often more diagnostically valuable than just a numerical rating initially.
*Are the symptoms worse in the morning or at night?*
- Diurnal variation can be relevant in certain conditions, such as inflammatory bowel diseases where nocturnal symptoms might be more concerning, or functional disorders whose symptoms might be stress-related.
- This is another **specific question** that should come after gathering a more complete initial picture of the patient's symptoms to ensure no key information is overlooked.
Exposure and environmental control US Medical PG Question 6: A 25-year-old man is admitted to the emergency department because of an episode of acute psychosis with suicidal ideation. He has no history of serious illness and currently takes no medications. Despite appropriate safety precautions, he manages to leave the examination room unattended. Shortly afterward, he is found lying outside the emergency department. A visitor reports that she saw the patient climbing up the facade of the hospital building. He does not respond to questions but points to his head when asked about pain. His pulse is 131/min, respirations are 22/min, and blood pressure is 95/61 mm Hg. Physical examination shows a 1-cm head laceration and an open fracture of the right tibia. He opens his eyes spontaneously. Pupils are equal, round, and reactive to light. Breath sounds are decreased over the right lung field, and the upper right hemithorax is hyperresonant to percussion. Which of the following is the most appropriate next step in management?
- A. Obtain a chest x-ray
- B. Perform a needle thoracostomy (Correct Answer)
- C. Perform an endotracheal intubation
- D. Apply a cervical collar
- E. Perform an open reduction of the tibia fracture
Exposure and environmental control Explanation: ***Perform a needle thoracostomy***
- The patient presents with **clinical signs of tension pneumothorax**: hypotension (95/61 mm Hg), tachycardia (131/min), decreased breath sounds, and hyperresonance over the right hemithorax following significant trauma from a fall.
- According to **ATLS (Advanced Trauma Life Support) principles**, the primary survey follows the **ABC priority**: Airway, Breathing, Circulation. A **tension pneumothorax is an immediately life-threatening condition** that compromises both breathing and circulation (obstructive shock).
- **Needle thoracostomy (needle decompression)** is the immediate, life-saving intervention for tension pneumothorax and must be performed **before** or concurrent with other interventions. This takes precedence over spinal immobilization when there is an immediate life threat.
- The clinical presentation strongly suggests tension physiology requiring immediate decompression; waiting for imaging would be inappropriate and potentially fatal.
*Apply a cervical collar*
- While **cervical spine protection** is important in this polytrauma patient with head injury and fall mechanism, it does **not take precedence over treating immediately life-threatening conditions** like tension pneumothorax.
- C-spine can be protected with **manual in-line stabilization** during the needle thoracostomy procedure.
- Modern trauma protocols emphasize that **life threats to airway, breathing, and circulation must be addressed immediately**, even if it requires brief spinal movement with appropriate precautions.
*Obtain a chest x-ray*
- **Tension pneumothorax is a clinical diagnosis** that requires immediate intervention without waiting for imaging confirmation.
- The combination of hypotension, tachycardia, decreased breath sounds, and hyperresonance in a trauma patient is sufficient to warrant emergent needle decompression.
- Delaying treatment for imaging in a hemodynamically unstable patient would be dangerous and violates patient safety principles.
*Perform an endotracheal intubation*
- While the patient has a **GCS of approximately 10** (eyes open spontaneously = 4, no verbal response = 1-2, localizes pain = 5-6), intubation is not the immediate priority.
- The **tension pneumothorax must be decompressed first** before attempting intubation, as positive pressure ventilation could worsen the tension pneumothorax and cause cardiovascular collapse.
- If intubation is needed, it should occur after needle decompression.
*Perform an open reduction of the tibia fracture*
- While the open tibia fracture requires urgent surgical management, it is **not immediately life-threatening** in the same timeframe as tension pneumothorax.
- According to ATLS principles, **life-threatening injuries are addressed before limb-threatening injuries**.
- The fracture should be stabilized temporarily, and definitive surgical management can occur after the patient is hemodynamically stable.
Exposure and environmental control US Medical PG Question 7: A 67-year-old man is brought to the emergency room after being involved in a traffic accident. He currently complains of bilateral hip pain. His vital signs are within the normal range, and he is hemodynamically stable. The pelvic compression test is positive. External genitalia appears normal, except there is blood at the urethral meatus and a contusion at the base of the scrotum. Digital rectal examination (DRE) shows a high-riding ballotable prostate. An X-ray reveals the presence of a pelvic fracture. Which of the following initial actions is the most appropriate for this patient?
- A. Insert a Foley catheter
- B. Take the patient emergently to the operating room and check for a urethral injury with IV indigo carmine
- C. Obtain a retrograde urethrogram (RUG), including a pre-injection kidney, ureter, and bladder (KUB) film (Correct Answer)
- D. Obtain a urinalysis to detect microscopic hematuria
- E. Perform a suprapubic cystostomy
Exposure and environmental control Explanation: ***Obtain a retrograde urethrogram (RUG), including a pre-injection kidney, ureter, and bladder (KUB) film***
- The combination of **blood at the urethral meatus**, a **high-riding ballotable prostate** on DRE, and a **pelvic fracture** are classic signs of a **urethral injury**, specifically a posterior urethral tear.
- A **retrograde urethrogram (RUG)** is the gold standard diagnostic test to confirm urethral injury and determine its location and extent, which is crucial before any attempt at catheterization.
*Insert a Foley catheter*
- **Insertion of a Foley catheter is contraindicated** in suspected urethral injuries, as it can worsen a partial tear into a complete transection or create a false passage.
- Doing so blindly could lead to further damage, stricture formation, and increased morbidity.
*Take the patient emergently to the operating room and check for a urethral injury with IV indigo carmine*
- This approach is premature before confirming the diagnosis and extent of urethral injury; **indigo carmine is used to assess ureteral integrity**, not urethral injury.
- Surgical exploration for urethral injury as an initial step is typically reserved for cases where RUG cannot be performed or for severe complex injuries with other indications for immediate surgery.
*Obtain a urinalysis to detect microscopic hematuria*
- While microscopic hematuria would likely be present, it is a **nonspecific finding** and does not provide information about the integrity of the urethra itself.
- It would not change the need for a RUG to assess for urethral injury in the presence of more specific signs.
*Perform a suprapubic cystostomy*
- A **suprapubic cystostomy** is the appropriate method for urinary diversion in a patient with a confirmed urethral injury if a Foley catheter cannot be safely placed.
- However, it is an intervention chosen *after* diagnosing the injury with a RUG, not the initial diagnostic step itself.
Exposure and environmental control US Medical PG Question 8: A mass casualty incident occurs with 25 casualties arriving simultaneously at a community hospital emergency department. The trauma team has limited resources with 2 operating rooms available and 4 surgeons present. Among the arriving patients: Patient A has traumatic amputation of forearm with tourniquet in place and stable vitals; Patient B has flail chest, respiratory distress, and unstable vitals; Patient C is in cardiac arrest with penetrating chest wound; Patient D has a femur fracture with stable vitals; Patient E has GCS 4 with bilateral blown pupils. Evaluate the triage priority according to ATLS mass casualty protocols.
- A. Priority order: C, E, B, A, D - treat most severely injured first
- B. Priority order: B, A, D, with E and C designated expectant (Correct Answer)
- C. Priority order: A, D, B, E, C - treat all patients equally regardless of prognosis
- D. Priority order: B, A, E, D, C - based on severity alone
- E. Immediate evacuation of all patients to a higher level trauma center
Exposure and environmental control Explanation: ***Priority order: B, A, D, with E and C designated expectant***
- In a **mass casualty incident (MCI)** with limited resources, the goal is to provide the **greatest good for the greatest number**; Patient B has life-threatening but **salvageable** injuries (respiratory distress) making them the top priority.
- Patients C (cardiac arrest) and E (GCS 4, blown pupils) are classified as **expectant (black tag)** because their survival probability is minimal and resuscitating them would exhaust resources needed for salvageable patients.
*Priority order: C, E, B, A, D - treat most severely injured first*
- This approach is used in standard trauma situations where resources are ample, but it is incorrect in an **MCI** where resource-heavy, low-prognosis patients are de-prioritized.
- Assigning highest priority to **cardiac arrest (C)** and **severe brain injury (E)** would likely result in the deaths of more salvageable patients like Patient B.
*Priority order: A, D, B, E, C - treat all patients equally regardless of prognosis*
- Treating all patients equally ignores the **ATLS triage categories** (Immediate, Delayed, Minimal, Expectant) and fails to address life-threatening priorities first.
- While A and D have stable vitals and are **Delayed (Yellow tag)**, waiting to treat Patient B's airway/breathing emergency would lead to a preventable death.
*Priority order: B, A, E, D, C - based on severity alone*
- Severity alone does not dictate priority in an MCI; the **likelihood of survival** with the available resources must be considered.
- Patient E, despite being "severe," has a **devastating neurological prognosis** (blown pupils, GCS 4) and should not be prioritized over stable patients with better outcomes like A and D.
*Immediate evacuation of all patients to a higher level trauma center*
- Evacuation is a secondary step; the primary task according to **ATLS protocols** is to perform triage and stabilization at the current facility during the initial influx.
- Attempting to evacuate all 25 casualties simultaneously without triage would overwhelm transport systems and delay life-saving **initial stabilization** for patients like B.
Exposure and environmental control US Medical PG Question 9: A 35-year-old pregnant woman at 32 weeks gestation is involved in a motor vehicle collision. She is hemodynamically stable with blood pressure 105/70 mmHg, heart rate 100/min. She has left upper quadrant tenderness and left lower rib fractures. FAST examination shows fluid in the splenorenal recess. Fetal heart tones are 150/min and reassuring. CT scan shows a Grade III splenic laceration. After 6 hours of observation with stable vital signs and hemoglobin, she suddenly develops blood pressure 85/50 mmHg and heart rate 125/min. Evaluate the management priority.
- A. Initiate massive transfusion and reassess after maternal stabilization
- B. Perform emergency cesarean section first, then address splenic injury
- C. Simultaneous laparotomy with splenectomy and obstetric standby for potential cesarean (Correct Answer)
- D. Proceed with splenectomy only, as maternal stabilization is the priority
- E. Perform angioembolization of splenic artery to avoid surgery
Exposure and environmental control Explanation: ***Simultaneous laparotomy with splenectomy and obstetric standby for potential cesarean***
- The patient has failed **non-operative management** of a splenic injury and is now **hemodynamically unstable**, necessitating immediate **laparotomy** to control hemorrhage.
- At **32 weeks gestation**, the fetus is viable; therefore, an **obstetric standby** is essential to perform a cesarean section if the mother's condition does not improve or if **fetal distress** occurs during the procedure.
*Initiate massive transfusion and reassess after maternal stabilization*
- While **massive transfusion** is part of trauma resuscitation, delaying surgery in an unstable patient with a known **Grade III splenic laceration** and hemodynamic collapse is inappropriate.
- Definitive **hemorrhage control** (surgery) is the priority once a patient becomes unstable after initial observation.
*Perform emergency cesarean section first, then address splenic injury*
- Performing a cesarean section first in an unstable trauma patient with **intra-abdominal hemorrhage** increases maternal morbidity and can worsen **hypovolemic shock**.
- Maternal stabilization and controlling the source of **bleeding** (splenectomy) is the most critical step to ensure both maternal and fetal survival.
*Proceed with splenectomy only, as maternal stabilization is the priority*
- While maternal stabilization is the priority, ignoring the viable fetus during a major surgical intervention is suboptimal care.
- Failure to involve an **obstetric team** overlooks the risk of **placental abruption** or fetal distress induced by maternal hypotension during surgery.
*Perform angioembolization of splenic artery to avoid surgery*
- **Angioembolization** is only indicated for stable patients; this patient is **hemodynamically unstable** (BP 85/50, HR 125), which is a contraindication for the interventional radiology suite.
- In the setting of active **intraperitoneal hemorrhage** and shock, an emergent **exploratory laparotomy** is the standard of care.
Exposure and environmental control US Medical PG Question 10: A 50-year-old helmeted motorcyclist is brought to the trauma bay after a collision at 50 mph. He is unconscious with GCS 6. Initial vitals show blood pressure 160/95 mmHg, heart rate 58/min. Pupils are unequal with the right pupil dilated and minimally reactive. He begins to posture with extension of extremities. He is intubated with in-line stabilization. CT scan cannot be immediately obtained due to scanner malfunction. Evaluate the most appropriate immediate management strategy.
- A. Administer hypertonic saline and wait for CT scanner to be repaired
- B. Start therapeutic hypothermia protocol and await imaging
- C. Administer mannitol, hyperventilate to pCO2 30-35 mmHg, elevate head of bed, and arrange emergent neurosurgical consultation (Correct Answer)
- D. Transport to another facility for immediate CT scan
- E. Perform bilateral burr holes at bedside
Exposure and environmental control Explanation: ***Administer mannitol, hyperventilate to pCO2 30-35 mmHg, elevate head of bed, and arrange emergent neurosurgical consultation***
- This patient exhibits **Cushing's triad** (hypertension, bradycardia) and asymmetric pupil dilation, indicating a life-threatening **transtentorial herniation** and increased **intracranial pressure (ICP)**.
- Immediate medical decompression using **osmotic therapy** (mannitol), **controlled hyperventilation** (causing cerebral vasoconstriction), and **head elevation** is critical to prevent brainstem death while awaiting neurosurgical intervention.
*Administer hypertonic saline and wait for CT scanner to be repaired*
- While **hypertonic saline** is an effective osmotic agent, waiting for a malfunctioning scanner in the setting of active **herniation** is unsafe and delays definitive care.
- Patients with clinical signs of herniation require **immediate neurosurgical consultation** and potentially a transfer if surgery cannot be performed on-site.
*Start therapeutic hypothermia protocol and await imaging*
- **Therapeutic hypothermia** is not a primary or immediate management strategy for acute **traumatic brain injury** with signs of herniation.
- Focus must remain on **ICP reduction** and surgical decompression; hypothermia does not address the acute mass effect evidenced by the blown pupil.
*Transport to another facility for immediate CT scan*
- Transporting an unstable patient with signs of **imminent herniation** without first initiating **ICP-lowering measures** is dangerous and may lead to death during transit.
- **Stabilization** including osmotic therapy and airway protection must be prioritized before considering any inter-facility transfer.
*Perform bilateral burr holes at bedside*
- **Bedside burr holes** are generally reserved for extreme circumstances where neurosurgical support is unavailable and the patient is rapidly deteriorating.
- The priority in a trauma bay setting is focused **medical management** followed by emergent definitive surgery (craniotomy) by a **neurosurgeon**.
More Exposure and environmental control US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.