Disability assessment (neurological status) US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Disability assessment (neurological status). These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Disability assessment (neurological status) US Medical PG Question 1: A previously healthy 10-year-old boy is brought to the emergency department for the evaluation of one episode of vomiting and severe headache since this morning. His mother says he also had difficulty getting dressed on his own. He has not had any trauma. The patient appears nervous. His temperature is 37°C (98.6°F), pulse is 100/min, and blood pressure is 185/125 mm Hg. He is confused and oriented only to person. Ophthalmic examination shows bilateral optic disc swelling. There is an abdominal bruit that is best heard at the right costovertebral angle. A complete blood count is within normal limits. Which of the following is most likely to confirm the diagnosis?
- A. Serum IGF-I level
- B. Oral sodium loading test
- C. Echocardiography
- D. CT angiography (Correct Answer)
- E. High-dose dexamethasone suppression test
Disability assessment (neurological status) Explanation: ***CT angiography***
- The patient presents with **malignant hypertension** (BP 185/125 mmHg, confusion, optic disc swelling) and an **abdominal bruit** especially at the **right costovertebral angle**, pointing strongly towards **renovascular hypertension** due to **renal artery stenosis**.
- **CT angiography** is the most appropriate imaging modality to confirm **renal artery stenosis** by visualizing the renal arteries and identifying any narrowing.
*Serum IGF-I level*
- This test is used to screen for **growth hormone disorders** like **acromegaly** or **gigantism**, which are not indicated by the patient's symptoms.
- The patient's presentation is focused on acute severe hypertension and neurological changes, rather than chronic growth disturbances.
*Oral sodium loading test*
- This test is used to confirm the diagnosis of **primary aldosteronism**, where **aldosterone levels** fail to suppress after a sodium load.
- While primary aldosteronism can cause hypertension, it typically doesn't present with an **abdominal bruit** or the acute, severe neurological symptoms seen here.
*Echocardiography*
- **Echocardiography** assesses the heart's structure and function, which could show signs of **hypertensive heart disease** (e.g., left ventricular hypertrophy) due to long-standing uncontrolled hypertension.
- However, it does not identify the underlying cause of the hypertension in this acute setting, especially when an **abdominal bruit** suggests a vascular origin.
*High-dose dexamethasone suppression test*
- This test is used to differentiate between **Cushing's disease** (pituitary ACTH-dependent) and other causes of **Cushing's syndrome** (e.g., ectopic ACTH production, adrenal tumor) due to excess cortisol.
- The patient's symptoms are inconsistent with Cushing's syndrome, and the **abdominal bruit** points away from this diagnosis.
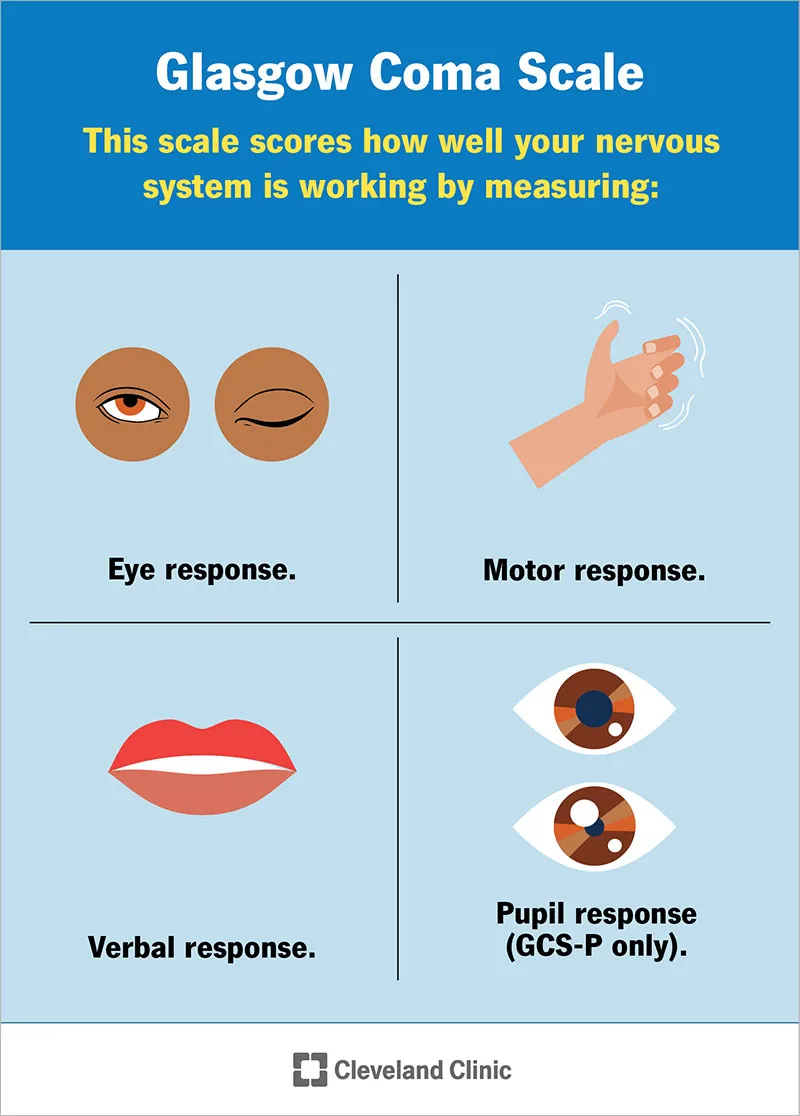
Disability assessment (neurological status) US Medical PG Question 2: A 22-year-old man is brought to the emergency department by ambulance 1 hour after a motor vehicle accident. He did not require any circulatory resuscitation at the scene, but he was intubated because he was unresponsive. He has no history of serious illnesses. He is on mechanical ventilation with no sedation. His blood pressure is 121/62 mm Hg, the pulse is 68/min, and the temperature is 36.5°C (97.7°F). His Glasgow coma scale (GCS) is 3. Early laboratory studies show no abnormalities. A search of the state donor registry shows that he has registered as an organ donor. Which of the following is the most appropriate next step in evaluation?
- A. Evaluation of brainstem reflexes (Correct Answer)
- B. Brain MRI
- C. Electroencephalography
- D. Cerebral angiography
- E. Apnea test
Disability assessment (neurological status) Explanation: ***Evaluation of brainstem reflexes***
- In a patient with a **Glasgow Coma Scale (GCS) of 3** and no response to noxious stimuli/sedation, assessment of **brainstem reflexes** is a critical step in determining brain death.
- This evaluation includes checking for pupillary light reflex, corneal reflex, vestibulo-ocular reflex (doll's eyes), oculocephalic reflex, and gag/cough reflexes to ascertain the complete absence of brainstem function.
*Brain MRI*
- While a brain MRI can provide detailed anatomical information regarding brain injury, it is **not the primary diagnostic test** for determining brain death.
- Brain death is a **clinical diagnosis** based on the irreversible loss of brain and brainstem function, which can be confirmed rapidly by clinical examination.
*Electroencephalography*
- **EEG** measures electrical activity in the brain and can show electrocerebral silence, which is consistent with brain death.
- However, EEG is **not always required** for the diagnosis of brain death and is often used as a confirmatory test in specific situations, such as when clinical examination is inconclusive or legal requirements necessitate it.
*Cerebral angiography*
- **Cerebral angiography** can demonstrate the absence of cerebral blood flow, which is a criterion for brain death.
- This is an **invasive procedure** and is generally reserved for situations where clinical examination tests are difficult to perform or interpret (e.g., severe facial trauma, drug intoxication), and is not the initial step.
*Apnea test*
- The **apnea test** is a critical component of the brain death evaluation, confirming the absence of spontaneous breathing response to hypercapnia.
- It is performed **after the absence of brainstem reflexes** has been established and all confounding factors (e.g., hypothermia, hypotension, sedatives) have been ruled out.
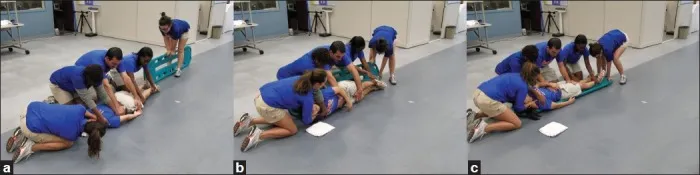
Disability assessment (neurological status) US Medical PG Question 3: A 74-year-old male is brought to the emergency department 1 hour after he fell from the top of the staircase at home. He reports pain in his neck as well as weakness of his upper extremities. He is alert and immobilized in a cervical collar. He has hypertension treated with hydrochlorothiazide. His pulse is 90/min and regular, respirations are 18/min, and blood pressure is 140/70 mmHg. Examination shows bruising and midline cervical tenderness. Neurologic examination shows diminished strength and sensation to pain and temperature in the upper extremities, particularly in the hands. Upper extremity deep tendon reflexes are absent. Strength, sensation, and reflexes in the lower extremities are intact. Anal sensation and tone are present. Babinski's sign is absent bilaterally. Which of the following is most likely to confirm the cause of this patient's neurologic examination findings?
- A. CT angiography of the neck
- B. MRI of the cervical spine without contrast (Correct Answer)
- C. X-ray of the cervical spine
- D. CT of the cervical spine with contrast
- E. Cervical myelography
Disability assessment (neurological status) Explanation: ***MRI of the cervical spine without contrast***
- This patient presents with symptoms consistent with **central cord syndrome**, characterized by greater weakness in the upper extremities than the lower extremities, often following a hyperextension injury in older adults with pre-existing cervical spondylosis. **MRI is the gold standard for visualizing soft tissue injuries**, including spinal cord compression, edema, or hemorrhage, which are typical causes of central cord syndrome.
- Given the primary concern for spinal cord injury and the detailed neurological deficits indicating specific cord involvement, **MRI** offers the best resolution for evaluating the extent of cord damage, disc herniation, ligamentous injury, and pre-existing degenerative changes.
*CT angiography of the neck*
- **CT angiography** primarily evaluates the **vascular structures** of the neck (e.g., carotid and vertebral arteries) for dissection, stenosis, or occlusion.
- While vascular injury could occur in trauma, the patient's neurological findings (disproportionate upper extremity weakness, pain and temperature sensation loss) point more directly to **spinal cord pathology** rather than isolated vascular compromise as the primary cause.
*X-ray of the cervical spine*
- **X-rays** are useful for initial screening of **bony fractures** and significant dislocations but offer limited information about soft tissues, such as the spinal cord, ligaments, or intervertebral discs.
- They cannot adequately visualize the spinal cord damage responsible for the patient's specific neurological deficits, making it insufficient for confirming the cause of central cord syndrome.
*CT of the cervical spine with contrast*
- **CT scans** excel at visualizing **bony structures** and acute fractures, but even with contrast, they provide less detail of the **spinal cord parenchyma** and soft tissue ligaments compared to MRI.
- **Contrast** is typically used to highlight vascular structures, inflammatory processes, or tumors, which are not the primary diagnostic concerns suggested by this patient's acute post-traumatic presentation of central cord syndrome.
*Cervical myelography*
- **Myelography** involves injecting contrast into the subarachnoid space, followed by X-ray or CT imaging, to outline the spinal cord and nerve roots.
- While it can identify **spinal cord compression**, it is an **invasive procedure** with risks (e.g., headache, seizures) and has largely been replaced by the non-invasive and superior soft tissue imaging capabilities of MRI, especially in acute trauma.
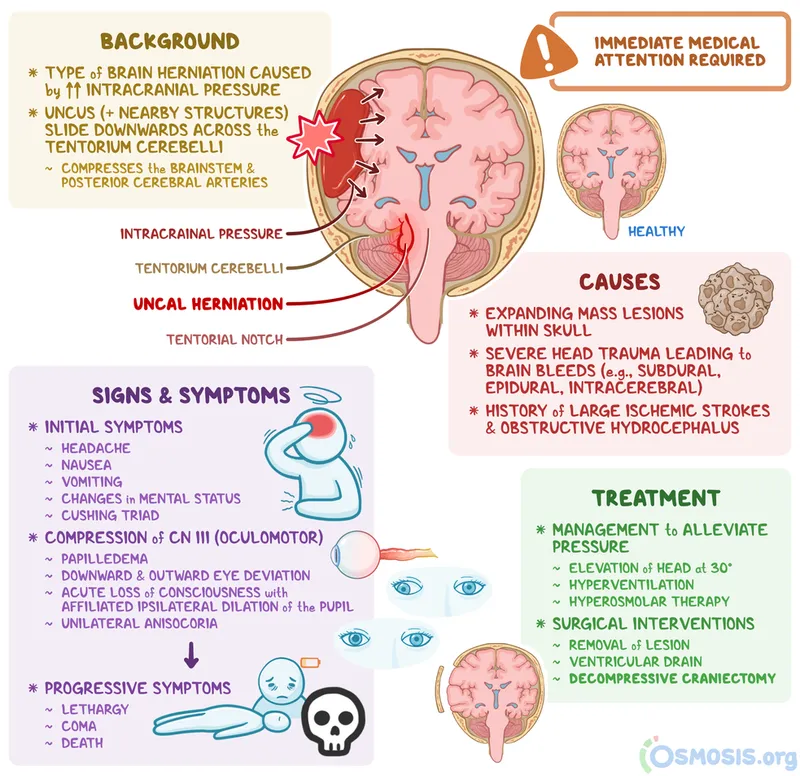
Disability assessment (neurological status) US Medical PG Question 4: A 37-year-old man is presented to the emergency department by paramedics after being involved in a serious 3-car collision on an interstate highway while he was driving his motorcycle. On physical examination, he is responsive only to painful stimuli and his pupils are not reactive to light. His upper extremities are involuntarily flexed with hands clenched into fists. The vital signs include temperature 36.1°C (97.0°F), blood pressure 80/60 mm Hg, and pulse 102/min. A non-contrast computed tomography (CT) scan of the head shows a massive intracerebral hemorrhage with a midline shift. Arterial blood gas (ABG) analysis shows partial pressure of carbon dioxide in arterial blood (PaCO2) of 68 mm Hg, and the patient is put on mechanical ventilation. His condition continues to decline while in the emergency department and it is suspected that this patient is brain dead. Which of the following results can be used to confirm brain death and legally remove this patient from the ventilator?
- A. Electrocardiogram
- B. Apnea test (Correct Answer)
- C. Lumbar puncture and CSF culture
- D. Electromyography with nerve conduction studies
- E. CT scan
Disability assessment (neurological status) Explanation: ***Correct: Apnea test***
- The **apnea test** is a **mandatory component** of brain death determination according to American Academy of Neurology (AAN) guidelines
- It directly confirms the **irreversible absence of brainstem function** by demonstrating no respiratory drive despite adequate stimulus (PaCO2 ≥60 mm Hg or 20 mm Hg rise from baseline)
- This patient already has a PaCO2 of 68 mm Hg, making the apnea test particularly relevant for confirmation
- Brain death requires both **clinical examination** (absent brainstem reflexes, coma) and a **positive apnea test** to legally declare death and discontinue mechanical ventilation
- The apnea test is performed by disconnecting the ventilator, providing supplemental oxygen, and observing for any respiratory effort while PaCO2 rises to adequate levels
*Incorrect: CT scan*
- While a **CT scan showing massive intracerebral hemorrhage with midline shift** provides anatomical evidence of severe, irreversible structural brain damage, it is **NOT sufficient to confirm brain death**
- CT imaging is used to establish the **etiology** and rule out reversible causes, but does not directly test brainstem function
- Brain death is a **clinical and functional diagnosis**, not purely an anatomical one—imaging alone cannot confirm cessation of all brain function
- A patient can have devastating structural damage on CT but still retain some brainstem reflexes
*Incorrect: Electrocardiogram*
- An **electrocardiogram (ECG)** measures cardiac electrical activity and provides no information about brain or brainstem function
- Cardiac activity commonly persists after brain death due to the heart's intrinsic automaticity
- ECG findings are irrelevant to brain death determination
*Incorrect: Lumbar puncture and CSF culture*
- **Lumbar puncture and CSF culture** are used to diagnose CNS infections (meningitis, encephalitis) or inflammatory conditions
- These tests are **completely irrelevant** for brain death diagnosis, which is based on irreversible cessation of all brain function, not infection
- In this trauma case with known intracerebral hemorrhage, LP would be contraindicated due to increased intracranial pressure and risk of herniation
*Incorrect: Electromyography with nerve conduction studies*
- **EMG and nerve conduction studies** assess peripheral nerve and muscle function, used for diagnosing neuromuscular disorders
- These tests provide no information about brain or brainstem function
- They are not part of brain death determination protocols
Disability assessment (neurological status) US Medical PG Question 5: A 56-year-old man comes to the physician because of worsening double vision and drooping of the right eyelid for 2 days. He has also had frequent headaches over the past month. Physical examination shows right eye deviation laterally and inferiorly at rest. The right pupil is dilated and does not react to light or with accommodation. The patient's diplopia improves slightly on looking to the right. Which of the following is the most likely cause of this patient’s findings?
- A. Demyelination of the medial longitudinal fasciculus
- B. Aneurysm of the posterior communicating artery (Correct Answer)
- C. Infarction of the midbrain
- D. Enlarging pituitary adenoma
- E. Thrombosis of the cavernous sinus
Disability assessment (neurological status) Explanation: ***Aneurysm of the posterior communicating artery***
- The combination of **third nerve palsy** (drooping eyelid, dilated pupil, eye deviated down and out) with **pupillary involvement** (dilated and unreactive) is a hallmark of **compressive lesions** affecting the oculomotor nerve, such as a PComm artery aneurysm.
- Frequent headaches over the past month can suggest a progressively enlarging lesion that is starting to exert pressure.
*Demyelination of the medial longitudinal fasciculus*
- This would cause **internuclear ophthalmoplegia (INO)**, characterized by impaired adduction of one eye and nystagmus of the abducting eye on attempted lateral gaze.
- It does not typically cause **pupillary dilation** or **ptosis** as seen in this patient.
*Infarction of the midbrain*
- A midbrain infarction could cause an **ischemic third nerve palsy**, but this usually **spares the pupil** because the parasympathetic fibers are located peripherally on the nerve and are more susceptible to compression than ischemia.
- The patient's **mydriasis** (dilated pupil) is a key feature pointing away from an ischemic cause.
*Enlarging pituitary adenoma*
- While a large pituitary adenoma can cause **vision changes** or **headaches**, it typically compresses the **optic chiasm** leading to **bitemporal hemianopsia**.
- Direct third nerve palsy with pupillary involvement is **uncommon** unless the mass is unusually large and extends significantly laterally.
*Thrombosis of the cavernous sinus*
- Cavernous sinus thrombosis presents more acutely with severe headache, fever, and involves **multiple cranial nerves** (**III, IV, V1, V2, VI**), often unilaterally.
- This patient's symptoms are primarily localized to the third nerve, and there are no signs of widespread cranial nerve involvement or systemic infection.
Disability assessment (neurological status) US Medical PG Question 6: A 57-year-old man was brought into the emergency department unconscious 2 days ago. His friends who were with him at that time say he collapsed on the street. Upon arrival to the ED, he had a generalized tonic seizure. At that time, he was intubated and is being treated with diazepam and phenytoin. A noncontrast head CT revealed hemorrhages within the pons and cerebellum with a mass effect and tonsillar herniation. Today, his blood pressure is 110/65 mm Hg, heart rate is 65/min, respiratory rate is 12/min (intubated, ventilator settings: tidal volume (TV) 600 ml, positive end-expiratory pressure (PEEP) 5 cm H2O, and FiO2 40%), and temperature is 37.0°C (98.6°F). On physical examination, the patient is in a comatose state. Pupils are 4 mm bilaterally and unresponsive to light. Cornea reflexes are absent. Gag reflex and cough reflex are also absent. Which of the following is the next best step in the management of this patient?
- A. Second opinion from a neurologist
- B. Withdraw ventilation support and mark time of death
- C. Electroencephalogram
- D. Repeat examination in several hours
- E. Apnea test (Correct Answer)
Disability assessment (neurological status) Explanation: ***Apnea test***
- The patient exhibits classic signs of **brain death**, including a **coma**, fixed and dilated pupils, and absent brainstem reflexes (corneal, gag, cough). The next step is to perform an apnea test to confirm the absence of spontaneous respiratory drive.
- An apnea test confirms brain death by demonstrating the **absence of respiratory effort** despite a rising pCO2, provided that spinal cord reflexes are not mistaken for respiratory efforts.
*Second opinion from a neurologist*
- While consulting a neurologist is often helpful in complex neurological cases, the current clinical picture presents such clear signs of brain death that **further confirmatory testing** for brain death (like the apnea test) is more immediately indicated before seeking additional opinions on diagnosis.
- A second opinion would typically be sought to confirm the diagnosis or guide management, but establishing brain death requires a specific protocol which is incomplete without the apnea test.
*Withdraw ventilation support and mark time of death*
- It is **premature to withdraw ventilation** before brain death is unequivocally confirmed by all necessary clinical and confirmatory tests, including the apnea test.
- Withdrawing support without full confirmation could lead to ethical and legal issues, as the patient might still have residual brainstem function, however minimal.
*Electroencephalogram*
- An **EEG** can show absent electrical activity, supporting brain death, but it is **not a mandatory part of the core brain death criteria** in many protocols, especially when clinical signs are clear and an apnea test can be performed.
- The primary diagnostic criteria for brain death usually prioritize clinical examination and the apnea test for proving irreversible cessation of all brain functions.
*Repeat examination in several hours*
- Repeating the examination in several hours is typically done if there are **confounding factors** (e.g., severe hypothermia, drug intoxication) that might mimic brain death, or if the initial assessment is incomplete.
- In this case, there are no mentioned confounding factors, and the immediate priority is to complete the brain death protocol with an apnea test, given the current clear clinical picture.
Disability assessment (neurological status) US Medical PG Question 7: A 27-year-old man presents to the emergency department after being hit by a car while riding his bike. The patient was brought in with his airway intact, vitals stable, and with a C-collar on. Physical exam is notable for bruising over the patient’s head and a confused man with a Glasgow coma scale of 11. It is noticed that the patient has a very irregular pattern of breathing. Repeat vitals demonstrate his temperature is 97.5°F (36.4°C), blood pressure is 172/102 mmHg, pulse is 55/min, respirations are 22/min and irregular, and oxygen saturation is 94% on room air. Which of the following interventions are most likely to improve this patient's vital signs?
- A. Head elevation, sedation, hypertonic saline, hypoventilation
- B. Lower head, sedation, hypertonic saline, hypoventilation
- C. Head elevation, sedation, mannitol, hyperventilation (Correct Answer)
- D. Head elevation, norepinephrine, mannitol, hyperventilation
- E. Lower head, sedation, hypertonic saline, hyperventilation
Disability assessment (neurological status) Explanation: ***Head elevation, sedation, mannitol, hyperventilation***
- This patient presents with signs of **increased intracranial pressure (ICP)**, indicated by **Cushing's triad** (hypertension, bradycardia, irregular respirations) and a decreased Glasgow Coma Scale (GCS) after head trauma. **Head elevation** to 30 degrees promotes venous outflow from the brain, reducing ICP.
- **Sedation** lowers metabolic demand and reduces agitation, which can otherwise increase ICP. **Mannitol** is an osmotic diuretic that rapidly draws fluid from the brain, decreasing cerebral edema. **Hyperventilation** temporarily reduces ICP by causing cerebral vasoconstriction through decreased pCO2.
*Head elevation, sedation, hypertonic saline, hypoventilation*
- While **head elevation**, **sedation**, and **hypertonic saline** (an alternative osmotic agent to mannitol) are appropriate for ICP management, **hypoventilation** would increase pCO2, causing cerebral vasodilation and worsening ICP.
- The combination of effective and ineffective ICP-reducing strategies makes this an incorrect option.
*Lower head, sedation, hypertonic saline, hypoventilation*
- **Lowering the head** would impede venous drainage from the brain and increase ICP, which is detrimental in this scenario.
- As mentioned, **hypoventilation** is contraindicated as it exacerbates cerebral edema and elevated ICP.
*Head elevation, norepinephrine, mannitol, hyperventilation*
- While **head elevation**, **mannitol**, and **hyperventilation** are appropriate, **norepinephrine** is primarily used to treat hypotension and maintain cerebral perfusion pressure (CPP) if blood pressure is dangerously low.
- In this case, the patient is hypertensive (**blood pressure 172/102 mmHg**), so norepinephrine would further increase blood pressure and ICP.
*Lower head, sedation, hypertonic saline, hyperventilation*
- **Lowering the head** is contraindicated as it directly increases ICP by hindering venous outflow from the brain.
- Although **sedation**, **hypertonic saline**, and **hyperventilation** are useful for ICP control, the incorrect positioning makes this option less suitable.
Disability assessment (neurological status) US Medical PG Question 8: One day after undergoing surgery for a traumatic right pelvic fracture, a 73-year-old man has pain over his buttocks and scrotum and urinary incontinence. Physical examination shows right-sided perineal hypesthesia and absence of anal sphincter contraction when the skin around the anus is touched. This patient is most likely to have which of the following additional neurological deficits?
- A. Impaired hip flexion
- B. Paralysis of hip adductors
- C. Absent cremasteric reflex
- D. Impaired psychogenic erection
- E. Absent reflex erection (Correct Answer)
Disability assessment (neurological status) Explanation: ***Absent reflex erection***
- The patient's symptoms (buttock/scrotal pain, perineal hypesthesia, urinary incontinence, absent anal sphincter contraction) suggest **damage to the sacral plexus and pudendal nerve**, consistent with a **cauda equina syndrome**.
- **Reflex erections** are primarily mediated by the **sacral parasympathetic outflow (S2-S4)**, which are likely compromised given the other sacral nerve deficits.
*Impaired hip flexion*
- **Hip flexion** is primarily controlled by the **L1-L3 nerve roots** (e.g., iliopsoas muscle), and while a severe pelvic fracture could cause widespread nerve damage, the current symptoms localize more strongly to the sacral region.
- The described symptoms are more indicative of **sacral nerve involvement** rather than higher lumbar segments that govern hip flexion.
*Paralysis of hip adductors*
- **Hip adduction** is mainly innervated by the **obturator nerve (L2-L4)**.
- The patient's symptoms point to **S2-S4 nerve dysfunction** (perineal sensation, anal sphincter, bladder), which are distinct from the obturator nerve's primary innervations.
*Absent cremasteric reflex*
- The **cremasteric reflex** is mediated by the **genitofemoral nerve (L1-L2)**.
- The symptoms presented are more consistent with **sacral nerve damage**, specifically S2-S4, rather than the higher lumbar segments responsible for the cremasteric reflex.
*Impaired psychogenic erection*
- **Psychogenic erections** are initiated by **supraspinal input** descending through the thoracolumbar spinal cord (T10-L2) to activate sympathetic pathways.
- While sacral nerve damage can affect the final efferent pathway for all erections, the direct impairment of psychogenic initiation is linked to higher centers and **thoracolumbar sympathetic outflow**, not purely sacral damage.
Disability assessment (neurological status) US Medical PG Question 9: A 25-year-old male presents to his primary doctor with difficulty sleeping. On exam, he is noted to have impaired upgaze bilaterally, although the rest of his ocular movements are intact. On pupillary exam, both pupils accommodate, but do not react to light. What is the most likely cause of his symptoms?
- A. Melanoma with temporal lobe metastasis
- B. Craniopharyngioma
- C. Pinealoma (Correct Answer)
- D. Spinal cord ependymoma
- E. Frontal lobe cavernoma
Disability assessment (neurological status) Explanation: **Pinealoma**
- The constellation of **impaired upgaze** (Parinaud syndrome) and **pupils that accommodate but do not react to light** (Argyll Robertson-like pupils) is highly suggestive of a lesion in the **dorsal midbrain**, a classic presentation of a **pinealoma**.
- **Pinealomas** are tumors of the pineal gland, which is located in the dorsal midbrain area, leading to compression of surrounding structures.
*Melanoma with temporal lobe metastasis*
- **Temporal lobe metastases** typically cause symptoms related to the temporal lobe function, such as **seizures**, memory deficits, or language disturbances.
- It would not specifically explain the characteristic ocular findings of **impaired upgaze** and **light-near dissociation** of the pupils.
*Craniopharyngioma*
- **Craniopharyngiomas** arise from Rathke's pouch and are typically located in the **suprasellar region**, often causing **visual field defects** (bitemporal hemianopsia) due to compression of the optic chiasm.
- While they can cause hydrocephalus and other neurological symptoms, they are not the primary cause of the specific dorsal midbrain syndrome described.
*Spinal cord ependymoma*
- **Spinal cord ependymomas** are tumors of the spinal cord and would present with **spinal cord compression symptoms** like weakness, sensory loss, or bladder dysfunction.
- These tumors do not affect the brainstem or ocular movements and therefore would not explain the patient's symptoms.
*Frontal lobe cavernoma*
- A **frontal lobe cavernoma** is a vascular malformation in the frontal lobe, most commonly presenting with **seizures** or focal neurological deficits related to the frontal lobe function (e.g., personality changes, motor weakness).
- It would not cause the specific set of ocular findings observed in this patient, which point to a midbrain lesion.
Disability assessment (neurological status) US Medical PG Question 10: A 45-year-old female presents to the emergency room as a trauma after a motor vehicle accident. The patient was a restrained passenger who collided with a drunk driver traveling approximately 45 mph. Upon impact, the passenger was able to extricate herself from the crushed car and was sitting on the ground at the scene of the accident. Her vitals are all stable. On physical exam, she is alert and oriented, speaking in complete sentences with a GCS of 15. She has a cervical spine collar in place and endorses exquisite cervical spine tenderness on palpation. Aside from her superficial abrasions on her right lower extremity, the rest of her examination including FAST exam is normal. Rapid hemoglobin testing is within normal limits. What is the next best step in management of this trauma patient?
- A. Remove the patient’s cervical collar immediately
- B. Discharge home and start physical therapy
- C. Initiate rapid sequence intubation.
- D. Consult neurosurgery immediately
- E. CT cervical spine (Correct Answer)
Disability assessment (neurological status) Explanation: ***CT cervical spine***
- Given the patient's **mechanism of injury** (motor vehicle accident at 45 mph) and **cervical spine tenderness**, a CT cervical spine is the most appropriate next step to rule out a fracture or other significant injury.
- While the patient is alert and stable, the presence of **exquisite tenderness** mandates imaging to ensure no occult injury is missed that could lead to neurological compromise.
*Remove the patient’s cervical collar immediately*
- Removing the cervical collar prematurely in a trauma patient with cervical spine tenderness is dangerous, as it could lead to further damage if an **unstable fracture** is present.
- The collar should remain in place until imaging has ruled out a clinically significant cervical spine injury.
*Discharge home and start physical therapy*
- Discharging a patient with **cervical spine tenderness** after a high-impact motor vehicle accident without imaging is inappropriate and could result in severe consequences if an injury is present.
- Physical therapy would only be considered after a thorough workup has cleared any acute injury.
*Initiate rapid sequence intubation.*
- **Rapid sequence intubation (RSI)** is used for airway management in patients with impending or actual respiratory failure or inability to protect their airway.
- This patient is alert, speaking in complete sentences, has a GCS of 15, and stable vitals, indicating **no immediate need for intubation**.
*Consult neurosurgery immediately*
- While a neurosurgery consult may be necessary if an injury is identified, the immediate next step is to **diagnose the injury** with imaging.
- Consulting neurosurgery without definitive imaging results would be premature in this stable patient.
More Disability assessment (neurological status) US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.