Circulation assessment and hemorrhage control US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Circulation assessment and hemorrhage control. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Circulation assessment and hemorrhage control US Medical PG Question 1: A 28-year-old research assistant is brought to the emergency department for severe chemical burns 30 minutes after accidentally spilling hydrochloric acid on himself. The burns cover both hands and forearms. His temperature is 37°C (98.6°F), pulse is 112/min, respirations are 20/min, and blood pressure is 108/82 mm Hg. Initial stabilization and resuscitation is begun, including respiratory support, fluid resuscitation, and cardiovascular stabilization. The burned skin is irrigated with saline water to remove the chemical agent. Which of the following is the most appropriate method to verify adequate fluid infusion in this patient?
- A. The Parkland formula
- B. Blood pressure
- C. Pulmonary capillary wedge pressure
- D. Heart rate
- E. Urinary output (Correct Answer)
Circulation assessment and hemorrhage control Explanation: ***Urinary output***
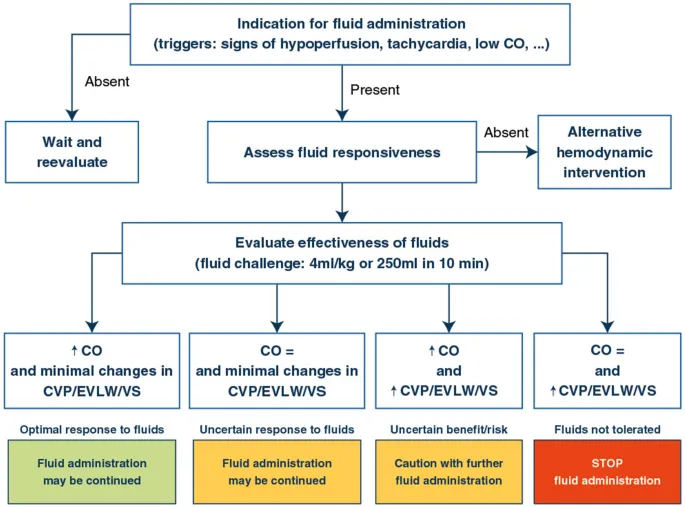
- Maintaining a specific **urinary output** (e.g., adult with major burns: 0.5-1.0 mL/kg/hr or 30-50 mL/hr) is the most reliable clinical indicator of adequate fluid resuscitation in burn patients.
- This ensures sufficient end-organ perfusion and avoids both under-resuscitation (leading to shock and organ damage) and over-resuscitation (risk of compartment syndrome and pulmonary edema).
*The Parkland formula*
- The **Parkland formula** is used to *calculate* the initial fluid volume needed, but it does not *verify* the adequacy of the infusion once started.
- This formula provides a starting point for fluid administration, which then needs to be adjusted based on the patient's response.
*Blood pressure*
- **Blood pressure** can be misleading in burn patients; it may remain deceptively normal due to compensatory mechanisms even with significant fluid deficits.
- It is a late indicator of hypovolemic shock, and relying solely on it can lead to under-resuscitation.
*Pulmonary capillary wedge pressure*
- **Pulmonary capillary wedge pressure (PCWP)** requires invasive monitoring via a pulmonary artery catheter, which is rarely indicated for routine fluid management in burn patients due to its invasiveness and associated risks.
- Less invasive and equally effective methods, like urinary output, are preferred for monitoring resuscitation.
*Heart rate*
- **Heart rate** is a sensitive but non-specific indicator of fluid status; it can be elevated due to pain, anxiety, or infection, not solely hypovolemia.
- While a decreasing heart rate can indicate improved fluid status, it is not as reliable or direct an indicator of end-organ perfusion as urinary output.
Circulation assessment and hemorrhage control US Medical PG Question 2: A 27-year-old man is brought to the emergency department after a motor vehicle accident. He was the unrestrained driver in a head on collision. The patient is responding incoherently and is complaining of being in pain. He has several large lacerations and has been impaled with a piece of metal. IV access is unable to be obtained and a FAST exam is performed. His temperature is 98.2°F (36.8°C), blood pressure is 90/48 mmHg, pulse is 150/min, respirations are 13/min, and oxygen saturation is 98% on room air. Which of the following is the best next step in management?
- A. Reattempt intravenous access
- B. Obtain intraosseous access (Correct Answer)
- C. Place a central line
- D. Administer oral fluids
- E. Exploratory laparotomy
Circulation assessment and hemorrhage control Explanation: ***Obtain intraosseous access***
- The patient is in **hypotensive shock** (BP 90/48 mmHg, HR 150/min) after a severe trauma, and **IV access cannot be obtained**. **Intraosseous (IO) access** provides a rapid and reliable route for fluid and medication administration in emergent situations when peripheral IV access is difficult or impossible.
- While central line placement is also a viable option, **IO access is generally faster and easier to establish** in an emergency setting by a wide range of providers, making it the **best initial step** when peripheral IV fails.
*Reattempt intravenous access*
- Although obtaining IV access is critical, the question states that it "is unable to be obtained," implying initial attempts have failed or are proving too difficult/time-consuming given the patient's critical state.
- Persisting with repeated attempts risks significant delay in resuscitation, which is detrimental for a patient in shock.
*Place a central line*
- A central line provides reliable access for fluid and medication, but its placement is generally **more time-consuming** and technically challenging than IO access, especially in an agitated, unstable patient in a chaotic emergency setting.
- The immediate priority is rapid access for fluids to address the patient's shock, for which IO is superior in terms of speed of establishment.
*Administer oral fluids*
- The patient is **unstable**, **incoherently responding**, and likely has significant internal injuries given the mechanism of injury (head-on collision, impalement).
- Oral fluids would be **ineffective** and potentially dangerous (risk of aspiration) in this critical, hemodynamically unstable patient who requires immediate intravenous fluid resuscitation.
*Exploratory laparotomy*
- While the patient likely has significant internal injuries requiring surgical intervention (impalement, hypovolemic shock), an **exploratory laparotomy** is a definitive treatment step, not the *best next step in management* for immediate resuscitation.
- **Hemodynamic stabilization** with fluid resuscitation must occur *before* or *simultaneously with* definitive surgical intervention to improve survival chances.
Circulation assessment and hemorrhage control US Medical PG Question 3: A 33-year-old pilot is transported to the emergency department after she was involved in a cargo plane crash during a military training exercise in South Korea. She is conscious but confused. She has no history of serious illness and takes no medications. Physical examination shows numerous lacerations and ecchymoses over the face, trunk, and upper extremities. The lower extremities are cool to the touch. There is continued bleeding despite the application of firm pressure to the sites of injury. The first physiologic response to develop in this patient was most likely which of the following?
- A. Increased respiratory rate
- B. Increased capillary refill time
- C. Decreased systolic blood pressure
- D. Decreased urine output
- E. Increased heart rate (Correct Answer)
Circulation assessment and hemorrhage control Explanation: ***Increased heart rate***
- **Tachycardia** is often the first physiological response to **hypovolemia** (due to hemorrhage, such as that stemming from multiple lacerations). The heart attempts to compensate for reduced circulating blood volume by increasing its pumping rate.
- This sympathetic nervous system response aims to maintain **cardiac output** and tissue perfusion as **blood pressure** and **venous return** start to fall.
*Increased respiratory rate*
- An increased respiratory rate, or **tachypnea**, typically occurs later as the body attempts to compensate for decreased oxygen delivery and metabolic acidosis that can result from sustained hypoperfusion and shock.
- While significant, it usually follows the initial hemodynamic adjustments of the heart.
*Increased capillary refill time*
- **Increased capillary refill time** indicates impaired peripheral perfusion and is a sign of more significant **hypovolemic shock**, often occurring after initial compensatory mechanisms have been activated.
- This reflects **peripheral vasoconstriction**, a later compensatory mechanism, rather than the very first physiological response.
*Decreased systolic blood pressure*
- **Decreased systolic blood pressure** (hypotension) is a later sign of shock and indicates a failure of the body's compensatory mechanisms to maintain adequate blood volume and perfusion, often reflecting a loss of more than 30-40% of blood volume.
- The body initially tries to maintain blood pressure through increased heart rate and vasoconstriction before it drops.
*Decreased urine output*
- **Decreased urine output** (oliguria) is a renal compensatory mechanism in response to reduced renal perfusion and increased antidiuretic hormone (ADH) release, aiming to conserve fluid.
- This response takes time to manifest and is not typically the very first physiological change after acute blood loss.
Circulation assessment and hemorrhage control US Medical PG Question 4: A 71-year-old woman is brought to the emergency department following a syncopal episode. Earlier in the day, the patient had multiple bowel movements that filled the toilet bowl with copious amounts of bright red blood. Minutes later, she felt dizzy and lightheaded and collapsed into her daughter's arms. The patient has a medical history of diabetes mellitus and hypertension. Her temperature is 99.0°F (37.2°C), blood pressure is 155/94 mmHg, pulse is 82/min, respirations are 15/min, and oxygen saturation is 99% on room air. The patient's exam is notable for fecal occult blood positivity on rectal exam; however, the patient is no longer having bloody bowel movements. The patient's lungs are clear to auscultation and her abdomen is soft and nontender. Labs are ordered as seen below.
Hemoglobin: 7.1 g/dL
Hematocrit: 25%
Leukocyte count: 5,300/mm^3 with normal differential
Platelet count: 182,500/mm^3
Two large bore IV's are placed and the patient is given normal saline. What is the best next step in management?
- A. Packed red blood cells
- B. Type and screen (Correct Answer)
- C. Fresh frozen plasma
- D. CT abdomen
- E. Colonoscopy
Circulation assessment and hemorrhage control Explanation: ***Type and screen***
- The patient has experienced a **significant colonic bleed** with associated **syncopal episode** and a **hemoglobin drop** to 7.1 g/dL. Before administering blood products, **blood typing and cross-matching** must be performed to ensure compatibility.
- This step is critical for **patient safety** to prevent transfusion reactions, especially given the likelihood of needing a transfusion soon.
- In the **sequence of acute blood loss management**, type and screen must be completed **before** packed red blood cells can be safely administered, making it the immediate next step after initial resuscitation with IV fluids.
*Packed red blood cells*
- While the patient will likely need **packed red blood cells (PRBCs)** due to severe anemia (Hb 7.1 g/dL) and hemodynamic instability (syncopal episode), PRBCs cannot be administered safely without first performing a **type and screen** to ensure compatibility.
- Administering PRBCs before compatibility testing is generally reserved for **life-threatening emergencies** with ongoing massive hemorrhage where there is no time for even an immediate cross-match (in which case O-negative blood would be used).
- This patient, while anemic, is currently **hemodynamically stable** (normal BP and pulse), allowing time for proper type and screen.
*Fresh frozen plasma*
- **Fresh frozen plasma (FFP)** is used to replace clotting factors in patients with **coagulopathies** or significant bleeding, often observed in massive transfusions or liver disease.
- This patient's **platelet count is normal** and there is no information to suggest a coagulopathy, thus FFP is not indicated as the immediate next step.
*CT abdomen*
- A **CT scan of the abdomen** may be useful later to identify the cause of the lower GI bleed, such as diverticulosis or angiodysplasia.
- However, the immediate priority is to **stabilize the patient hemodynamically** and address the acute blood loss before pursuing diagnostic imaging.
*Colonoscopy*
- A **colonoscopy** is the definitive diagnostic and potentially therapeutic procedure for a lower GI bleed.
- However, before performing a colonoscopy, the patient must be **hemodynamically stable**, which includes addressing their **anemia** and ensuring adequate blood product availability.
Circulation assessment and hemorrhage control US Medical PG Question 5: A 72-year-old man presents to the emergency department after a fall. The patient was found lying down on the floor in his room in his retirement community. The patient has a past medical history of Alzheimer dementia and a prosthetic valve. His current medications include donepezil and warfarin. His temperature is 97.7°F (36.5°C), blood pressure is 85/50 mmHg, pulse is 160/min, respirations are 13/min, and oxygen saturation is 97% on room air. The patient is started on IV fluids and a type and screen is performed. Laboratory values are ordered as seen below.
Hemoglobin: 13 g/dL
Hematocrit: 39%
Leukocyte count: 5,500 cells/mm^3 with normal differential
Platelet count: 225,000/mm^3
INR: 2.5
AST: 10 U/L
ALT: 12 U/L
A chest radiograph and EKG are performed and are within normal limits. A full physical exam is within normal limits. The patient's vitals are repeated. His temperature is 99.5°F (37.5°C), blood pressure is 110/70 mmHg, pulse is 90/min, respirations are 10/min, and oxygen saturation is 98% on room air. Which of the following is the best next step in management?
- A. CT scan (Correct Answer)
- B. Urgent blood transfusion
- C. Fresh frozen plasma
- D. Exploratory laparoscopy
- E. Exploratory laparotomy
Circulation assessment and hemorrhage control Explanation: ***CT scan***
- A patient with a **prosthetic valve** on **warfarin** and a fall is at high risk for **intracranial hemorrhage**, even without focal neurological deficits.
- While initial vitals improved after IV fluids, the mechanism of injury (fall) and medication profile warrant a **CT scan** of the head to rule out serious internal injury, especially given the history of dementia which might mask symptoms.
*Urgent blood transfusion*
- The patient's **hemoglobin (13 g/dL)** and **hematocrit (39%)** are within normal limits, indicating no acute need for blood transfusion due to hemorrhage.
- Transfusions are typically reserved for patients with significant blood loss or severe symptomatic anemia.
*Fresh frozen plasma*
- The patient's **INR of 2.5** is within the therapeutic range for a patient with a prosthetic valve on warfarin.
- There is no evidence of active bleeding or supratherapeutic anticoagulation that would necessitate the administration of **fresh frozen plasma (FFP)** to reverse anticoagulation.
*Exploratory laparoscopy*
- There are no clinical signs or symptoms, such as abdominal pain, distension, or evidence of intra-abdominal bleeding (e.g., declining hemoglobin, peritoneal signs), to suggest an indication for an **exploratory laparoscopy**.
- The patient's physical exam was described as normal.
*Exploratory laparotomy*
- Similar to laparoscopy, there is no clinical evidence of acute abdominal injury or hemorrhage, which would necessitate an **exploratory laparotomy**.
- This invasive procedure is reserved for cases with strong suspicion of significant intra-abdominal pathology or trauma.
Circulation assessment and hemorrhage control US Medical PG Question 6: A 35-year-old male is brought into the emergency department for a trauma emergency. The emergency medical services states that the patient was wounded with a knife on his upper left thigh near the inguinal ligament. Upon examination in the trauma bay, the patient is awake and alert. His physical exam and FAST exam is normal other than the knife wound. Large bore intravenous lines are inserted into the patient for access and fluids are being administered. Pressure on the knife wound is being held by one of the physicians with adequate control of the bleeding, but the physician notices the blood was previously extravasating in a pulsatile manner. His vitals are BP 100/50, HR 110, T 97.8, RR 22. What is the next best step for this patient?
- A. CT lower extremities
- B. Radiograph lower extremities
- C. Coagulation studies and blood typing/crossmatch
- D. Tourniquet of proximal lower extremity
- E. Emergent surgery (Correct Answer)
Circulation assessment and hemorrhage control Explanation: ***Emergent surgery***
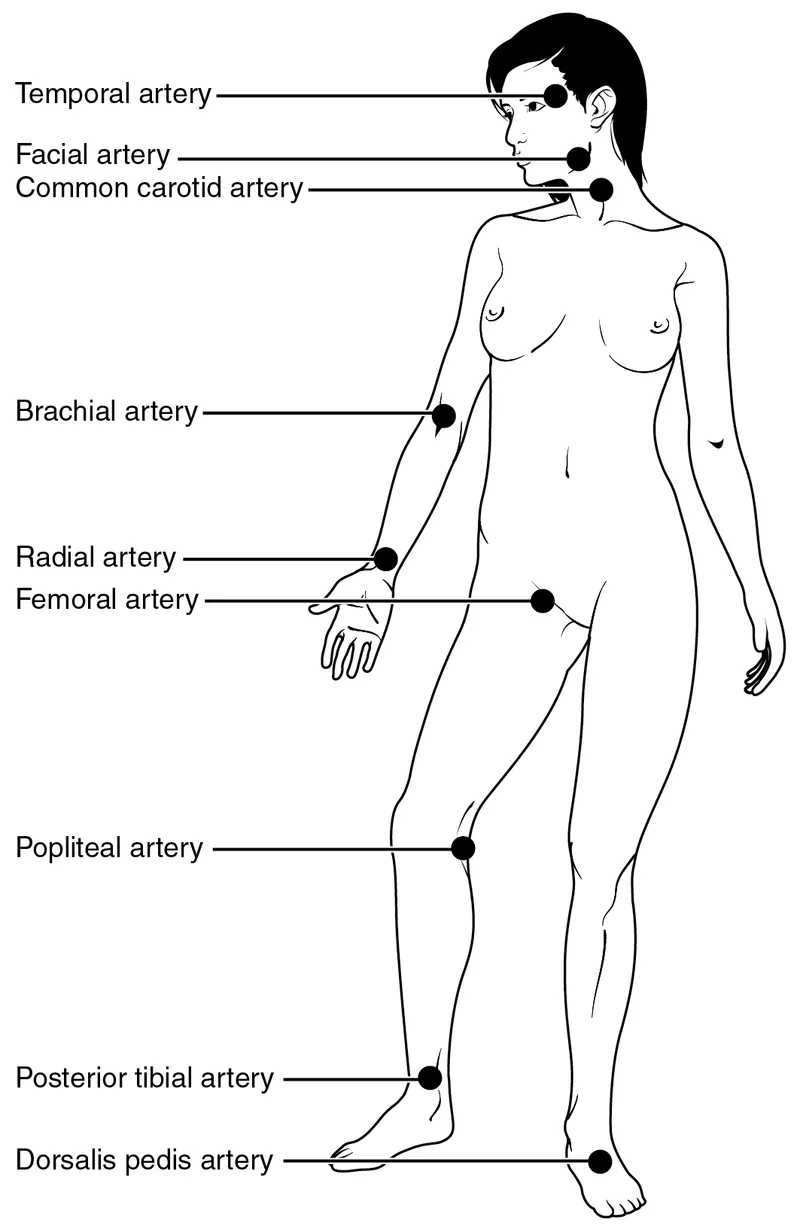
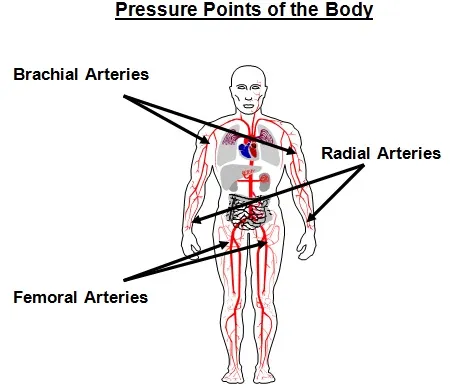
- The pulsatile bleeding from a thigh wound near the inguinal ligament is highly suggestive of a major arterial injury, such as to the **femoral artery**.
- Given the potential for rapid blood loss and hemodynamic instability, **emergent surgical exploration and repair** are necessary to control the bleeding and prevent further compromise.
*CT lower extremities*
- While CT angiography could further delineate vascular injury, the presence of **active pulsatile bleeding** necessitates immediate surgical intervention rather than delaying for imaging.
- Delaying surgery for imaging risks **exsanguination** and worsening patient outcomes, especially with a blood pressure of **100/50 mmHg** and a heart rate of **110 bpm**, indicating early shock.
*Radiograph lower extremities*
- A radiograph would primarily visualize bone structures and foreign bodies but would not provide adequate information regarding the **vascular injury** and active bleeding.
- It would not change the urgent need for **surgical exploration** to address the pulsatile hemorrhage.
*Coagulation studies and blood typing/crossmatch*
- These are important preparatory steps for major surgery involving significant blood loss, but they should be carried out **concurrently with preparations for emergent surgery**, not instead of it.
- Delaying surgery to await these results would be inappropriate when facing **active arterial bleeding**.
*Tourniquet of proximal lower extremity*
- While a tourniquet can be used for temporary hemorrhage control, especially in an uncontrolled external hemorrhage, the current bleeding is being controlled by **direct pressure**.
- Applying a tourniquet could cause **ischemic damage** to the extremity if applied for too long, and for a deep stab wound, direct compression is often effective until surgical control can be achieved.
Circulation assessment and hemorrhage control US Medical PG Question 7: A 24-year-old woman is brought to the emergency department after being assaulted. The paramedics report that the patient was found conscious and reported being kicked many times in the torso. She is alert and able to respond to questions. She denies any head trauma. She has a past medical history of endometriosis and a tubo-ovarian abscess that was removed surgically two years ago. Her only home medication is oral contraceptive pills. Her temperature is 98.5°F (36.9°C), blood pressure is 82/51 mmHg, pulse is 136/min, respirations are 24/min, and SpO2 is 94%. She has superficial lacerations to the face and severe bruising over her chest and abdomen. Her lungs are clear to auscultation bilaterally and her abdomen is soft, distended, and diffusely tender to palpation. Her skin is cool and clammy. Her FAST exam reveals fluid in the perisplenic space.
Which of the following is the next best step in management?
- A. Emergency laparotomy (Correct Answer)
- B. Abdominal radiograph
- C. Abdominal CT
- D. Fluid resuscitation
- E. Diagnostic peritoneal lavage
Circulation assessment and hemorrhage control Explanation: ***Emergency laparotomy***
- The patient presents with **hemodynamic instability** (BP 82/51 mmHg, HR 136/min) and a **positive FAST exam** showing fluid in the perisplenic space, indicating intra-abdominal hemorrhage.
- According to **ATLS guidelines**, a hemodynamically unstable patient with a positive FAST exam requires **immediate operative intervention** to control bleeding. This is the definitive management for ongoing hemorrhage.
- While fluid resuscitation is initiated simultaneously (en route to OR), **surgical control of the bleeding source** is the priority and should not be delayed.
*Fluid resuscitation*
- Fluid resuscitation with IV crystalloids is essential and should be started immediately in this patient with hypovolemic shock.
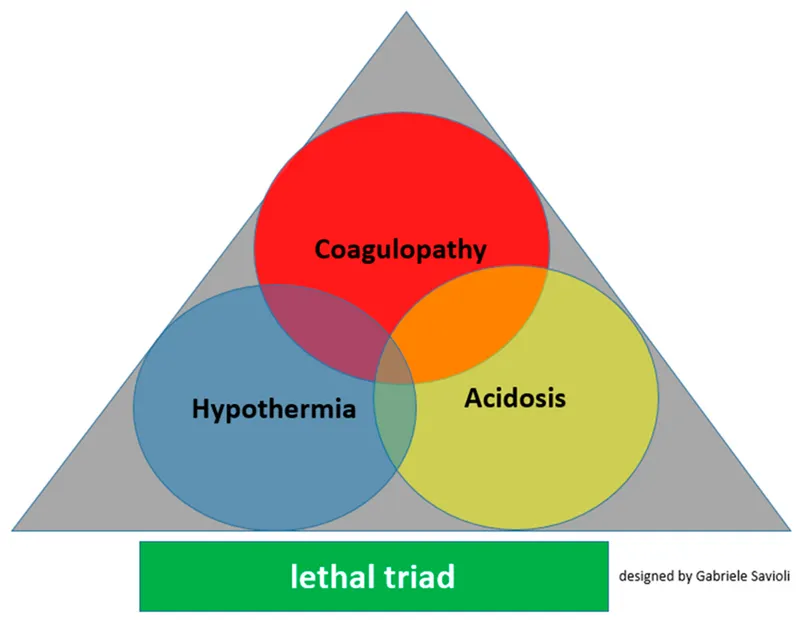
- However, in a patient with **uncontrolled intra-abdominal hemorrhage** (positive FAST, hemodynamic instability), fluids alone will not stop the bleeding. Continued fluid resuscitation without surgical intervention can lead to dilutional coagulopathy and worsening outcomes.
- Fluid resuscitation occurs **concurrently with preparation for surgery**, not as a separate step that delays definitive management.
*Diagnostic peritoneal lavage*
- DPL is an invasive diagnostic procedure that has largely been replaced by FAST exam in modern trauma care.
- Given that the **FAST is already positive**, DPL would provide no additional useful information and would only **delay definitive surgical management**.
- In hemodynamically unstable patients with positive FAST, proceeding directly to laparotomy is indicated.
*Abdominal radiograph*
- Plain radiographs have **limited sensitivity** for detecting intra-abdominal bleeding or solid organ injury.
- They may show free air (indicating hollow viscus perforation) but cannot assess for fluid or characterize solid organ injuries.
- This would **delay necessary operative intervention** without providing actionable information.
*Abdominal CT*
- CT abdomen is the imaging modality of choice for **hemodynamically stable** trauma patients to characterize injuries and guide management.
- For **unstable patients**, CT is **contraindicated** as it delays definitive treatment and removes the patient from a resuscitation environment where deterioration can be immediately addressed.
Circulation assessment and hemorrhage control US Medical PG Question 8: A 28-year-old male presents to his primary care physician with complaints of intermittent abdominal pain and alternating bouts of constipation and diarrhea. His medical chart is not significant for any past medical problems or prior surgeries. He is not prescribed any current medications. Which of the following questions would be the most useful next question in eliciting further history from this patient?
- A. "Does the diarrhea typically precede the constipation, or vice-versa?"
- B. "Is the diarrhea foul-smelling?"
- C. "Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life"
- D. "Are the symptoms worse in the morning or at night?"
- E. "Can you tell me more about the symptoms you have been experiencing?" (Correct Answer)
Circulation assessment and hemorrhage control Explanation: ***Can you tell me more about the symptoms you have been experiencing?***
- This **open-ended question** encourages the patient to provide a **comprehensive narrative** of their symptoms, including details about onset, frequency, duration, alleviating/aggravating factors, and associated symptoms, which is crucial for diagnosis.
- In a patient presenting with vague, intermittent symptoms like alternating constipation and diarrhea, allowing them to elaborate freely can reveal important clues that might not be captured by more targeted questions.
*Does the diarrhea typically precede the constipation, or vice-versa?*
- While knowing the sequence of symptoms can be helpful in understanding the **pattern of bowel dysfunction**, it is a very specific question that might overlook other important aspects of the patient's experience.
- It prematurely narrows the focus without first obtaining a broad understanding of the patient's overall symptomatic picture.
*Is the diarrhea foul-smelling?*
- Foul-smelling diarrhea can indicate **malabsorption** or **bacterial overgrowth**, which are important to consider in some gastrointestinal conditions.
- However, this is a **specific symptom inquiry** that should follow a more general exploration of the patient's symptoms, as it may not be relevant if other crucial details are missed.
*Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life*
- Quantifying pain intensity is useful for assessing the **severity of discomfort** and monitoring changes over time.
- However, for a patient with intermittent rather than acute, severe pain, understanding the **character, location, and triggers** of the pain is often more diagnostically valuable than just a numerical rating initially.
*Are the symptoms worse in the morning or at night?*
- Diurnal variation can be relevant in certain conditions, such as inflammatory bowel diseases where nocturnal symptoms might be more concerning, or functional disorders whose symptoms might be stress-related.
- This is another **specific question** that should come after gathering a more complete initial picture of the patient's symptoms to ensure no key information is overlooked.
Circulation assessment and hemorrhage control US Medical PG Question 9: An 18-year-old man presents to the emergency department after an automobile accident. His vitals have significantly dropped since admission. Upon examination, his abdomen is slightly distended, the ribs on the right side are tender and appear broken, and breath sounds are diminished at the base of the right lung. An abdominal ultrasound and chest X-ray are ordered. Ultrasound shows fluid in the abdominal cavity and trauma to the liver. X-ray confirmed broken ribs and pleural effusion on the right. Based on these findings, the surgeons recommend immediate surgery. Upon entering the abdomen, an exsanguinating hemorrhage is observed. The Pringle maneuver is used to reduce bleeding. What was clamped during this maneuver?
- A. Aorta above celiac axis
- B. Splenic artery only
- C. Hepatic artery only
- D. Hepatic vein only
- E. Hepatoduodenal ligament (Correct Answer)
Circulation assessment and hemorrhage control Explanation: ***Hepatoduodenal ligament***
- The **Pringle maneuver** involves clamping the **hepatoduodenal ligament** to control bleeding from the liver. This ligament contains the **hepatic artery**, **portal vein**, and **bile duct**.
- Clamping the hepatoduodenal ligament effectively stops blood flow into the liver, allowing for temporary control of hemorrhage during hepatic trauma repair.
*Aorta above celiac axis*
- Clamping the **aorta above the celiac axis** would severely compromise blood flow to multiple vital organs, including the stomach, spleen, and most of the intestines, leading to widespread ischemia.
- This is a much more extensive and dangerous clamping maneuver typically reserved for massive intra-abdominal hemorrhage not controllable by other means, rather than liver-specific bleeding.
*Splenic artery only*
- Clamping the **splenic artery** would only stop blood flow to the spleen and would not significantly impact bleeding from the liver.
- The described trauma is to the liver, so addressing the splenic artery would not be the primary intervention for a liver hemorrhage.
*Hepatic artery only*
- While clamping the **hepatic artery** would reduce arterial blood flow to the liver, the liver also receives a significant blood supply from the portal vein.
- Therefore, clamping only the hepatic artery would not completely stop the blood flow into the liver, making it less effective than the Pringle maneuver (which includes the portal vein).
*Hepatic vein only*
- Clamping the **hepatic vein** would obstruct blood outflow from the liver, leading to **hepatic venous congestion**, but it would not stop the inflow of blood from the hepatic artery and portal vein.
- This would worsen rather than control an exsanguinating hemorrhage from a liver injury.
Circulation assessment and hemorrhage control US Medical PG Question 10: A 63-year-old man comes to the physician because of a 1-month history of difficulty swallowing, low-grade fever, and weight loss. He has smoked one pack of cigarettes daily for 30 years. An esophagogastroduodenoscopy shows an esophageal mass just distal to the upper esophageal sphincter. Histological examination confirms the diagnosis of locally invasive squamous cell carcinoma. A surgical resection is planned. Which of the following structures is at greatest risk for injury during this procedure?
- A. Bronchial branch of thoracic aorta
- B. Left gastric artery
- C. Left inferior phrenic artery
- D. Esophageal branch of thoracic aorta
- E. Inferior thyroid artery (Correct Answer)
Circulation assessment and hemorrhage control Explanation: **Inferior thyroid artery**
- The esophageal mass is located just distal to the **upper esophageal sphincter**, which is in the neck, close to the **thyroid gland**.
- During surgery for an esophageal tumor in this region, the **inferior thyroid artery**, which supplies the thyroid and adjacent structures, is at the greatest risk of injury due to its proximity.
*Bronchial branch of thoracic aorta*
- The **bronchial branches** of the thoracic aorta primarily supply the bronchi and lungs.
- These vessels are located deeper in the thorax, away from the **upper esophageal sphincter** and the initial surgical field for an upper esophageal tumor.
*Left gastric artery*
- The **left gastric artery** supplies the stomach and is a branch of the celiac trunk.
- This artery is located in the **abdomen**, far from the surgical site involving an esophageal mass near the upper esophageal sphincter.
*Left inferior phrenic artery*
- The **left inferior phrenic artery** primarily supplies the diaphragm.
- This vessel originates from the aorta in the **abdominal region**, which is distant from the upper esophageal sphincter.
*Esophageal branch of thoracic aorta*
- **Esophageal branches** directly supply the esophagus; however, the question refers to the **thoracic aorta branches**.
- Tumors near the **upper esophageal sphincter** are usually accessed via a cervical incision, making thoracic branches less likely to be injured compared to arteries located in the neck.
More Circulation assessment and hemorrhage control US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.