Airway management in trauma US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Airway management in trauma. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Airway management in trauma US Medical PG Question 1: A 52-year-old obese man is brought to the emergency department 30 minutes after he was involved in a high-speed motor vehicle collision. He was the unrestrained driver. On arrival, he is lethargic. His pulse is 112/min, respirations are 10/min and irregular, and blood pressure is 94/60 mm Hg. Pulse oximetry on room air shows an oxygen saturation of 91%. The pupils are equal and react sluggishly to light. He withdraws his extremities to pain. There are multiple bruises over his face, chest, and abdomen. Breath sounds are decreased over the left lung base. Two large bore peripheral venous catheters are inserted and 0.9% saline infusion is begun. Rapid sequence intubation is initiated and endotracheal intubation is attempted without success. Bag and mask ventilation is continued. Pulse oximetry shows an oxygen saturation of 84%. The patient has no advance directive and family members have not arrived. Which of the following is the most appropriate next step in the management of this patient?
- A. Nasotracheal intubation
- B. Video laryngoscopy
- C. Cricothyrotomy (Correct Answer)
- D. Comfort measures only
- E. Tracheostomy
Airway management in trauma Explanation: ***Cricothyrotomy***
- In a trauma patient with **failed endotracheal intubation** and declining oxygen saturation (from 91% to 84% despite bag-mask ventilation), an emergent cricothyrotomy is indicated for **immediate airway control**.
- This procedure provides a definitive airway in a **can't intubate/can't ventilate** scenario, preventing further hypoxia and potential brain damage.
*Nasotracheal intubation*
- **Nasotracheal intubation** is generally contraindicated in patients with suspected **facial or skull base fractures** due to the risk of intracranial intubation.
- Given the high-speed collision and facial bruises, such fractures are possible, making this a less safe option compared to cricothyrotomy.
*Video laryngoscopy*
- While **video laryngoscopy** can be helpful for difficult airways, it was already implied that intubation was attempted and failed, suggesting the issue might be with visualization or access, not just technique.
- Critically, the patient's oxygen saturation is dropping rapidly, requiring a quicker, more definitive solution than another attempt at orotracheal intubation.
*Comfort measures only*
- The patient has **no advance directive**, and family members have not arrived to make decisions regarding end-of-life care.
- Despite the severity of his injuries, the patient is still alive and does not have clear indications for **comfort measures only** at this stage; resuscitative efforts are warranted.
*Tracheostomy*
- **Tracheostomy** is a surgical procedure for establishing a long-term airway and is not suitable for **emergent airway management** in a rapidly decompensating trauma patient.
- It typically requires specialized surgical expertise and takes longer to perform than a cricothyrotomy, which is a faster, life-saving measure in this acute situation.
Airway management in trauma US Medical PG Question 2: A 21-year-old woman comes to the physician for the evaluation of dry cough and some chest tightness for the past several weeks. The cough is worse at night and while playing volleyball. She frequently has a runny nose and nasal congestion. Her mother has systemic lupus erythematosus. The patient has smoked one pack of cigarettes daily for the last 5 years. She does not drink alcohol. Her only medication is cetirizine. Her vital signs are within normal limits. Pulse oximetry on room air shows an oxygen saturation of 98%. The remainder of the examination shows no abnormalities. Which of the following is the most appropriate next step in management?
- A. CT scan of the chest
- B. Spirometry (Correct Answer)
- C. Laboratory studies
- D. Methacholine challenge test
- E. Blood gas analysis
Airway management in trauma Explanation: ***Spirometry***
- The patient's symptoms (dry cough, chest tightness, worse at night and with activity) are highly suggestive of **asthma**.
- **Spirometry** is the initial recommended diagnostic test to assess for reversible airway obstruction, which is characteristic of asthma.
*CT scan of the chest*
- A CT scan of the chest is generally reserved for evaluating structural lung diseases, persistent or atypical symptoms, or when other diagnoses (e.g., malignancy, interstitial lung disease) are suspected.
- Given the classic asthma-like symptoms, a **less invasive and more direct physiological test** is indicated first.
*Laboratory studies*
- Routine laboratory studies are typically **not helpful** in the initial diagnosis of asthma.
- While allergy testing or inflammatory markers might be considered later, they do not directly assess airway function to confirm asthma.
*Methacholine challenge test*
- A **methacholine challenge test** is used to diagnose **asthma** when spirometry results are normal but asthma is still strongly suspected.
- It is often considered if initial spirometry with bronchodilator reversal is inconclusive, rather than as a first-line diagnostic step.
*Blood gas analysis*
- Blood gas analysis measures oxygen and carbon dioxide levels in the blood and is used to assess the severity of respiratory failure or acid-base status.
- It is **not a primary diagnostic tool for asthma**, especially in a patient with normal vital signs and pulse oximetry.
Airway management in trauma US Medical PG Question 3: A 19-year-old man is rushed to the emergency department 30 minutes after diving head-first into a shallow pool of water from a cliff. He was placed on a spinal board and a rigid cervical collar was applied by the emergency medical technicians. On arrival, he is unconscious and withdraws all extremities to pain. His temperature is 36.7°C (98.1°F), pulse is 70/min, respirations are 8/min, and blood pressure is 102/70 mm Hg. Pulse oximetry on room air shows an oxygen saturation of 96%. The pupils are equal and react sluggishly to light. There is a 3-cm (1.2-in) laceration over the forehead. The lungs are clear to auscultation. Cardiac examination shows no abnormalities. The abdomen is soft and nontender. There is a step-off palpated over the cervical spine. Which of the following is the most appropriate next step in management?
- A. Rapid sequence intubation (Correct Answer)
- B. CT scan of the spine
- C. X-ray of the cervical spine
- D. MRI of the spine
- E. Rectal tone assessment
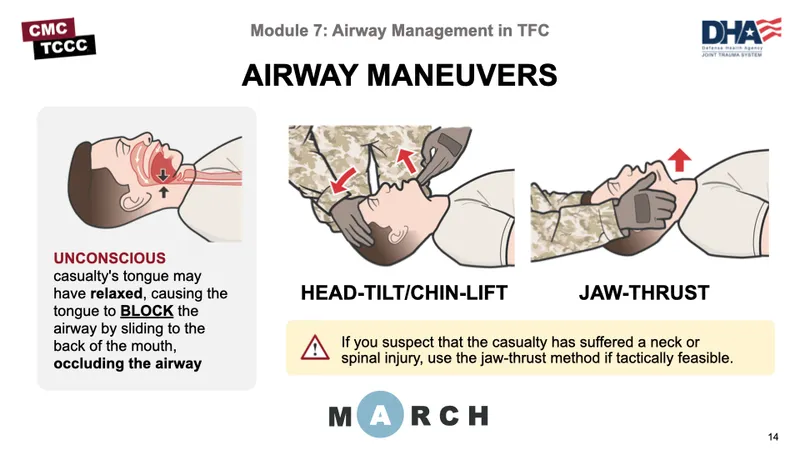
Airway management in trauma Explanation: ***Rapid sequence intubation***
- The patient has a **compromised airway** due to very shallow respirations (8/min), indicating impending respiratory failure, which is prioritized in the management of trauma patients.
- Due to the high suspicion of a **cervical spine injury** (diving into a shallow pool, step-off palpable over the cervical spine), **rapid sequence intubation** is the safest way to secure the airway while maintaining **cervical spine immobilization**.
*CT scan of the spine*
- Imaging studies of the spine are important for diagnosis but must be performed **after securing the airway** and stabilizing vital functions.
- While a CT scan is the preferred imaging modality for evaluating bony spinal trauma, it does not address the immediate life-threatening issue of respiratory insufficiency.
*X-ray of the cervical spine*
- X-rays are less sensitive for detecting all types of cervical spine injuries, especially ligamentous damage, compared to CT or MRI.
- As with other imaging, it should be done **after airway management** is secured.
*MRI of the spine*
- MRI is excellent for evaluating **soft tissue structures** like spinal cord, ligaments, and discs, and is generally performed after initial stabilization and CT for bony injury.
- It is not an immediate diagnostic priority when the patient's airway and breathing are acutely compromised.
*Rectal tone assessment*
- This assessment is part of the neurological examination to evaluate for spinal cord injury, specifically involving the **sacral segments**.
- While important for comprehensive neurological assessment, it is not the most appropriate *next step* when the patient has critical airway and breathing compromise.
Airway management in trauma US Medical PG Question 4: A 28-year-old soldier is brought back to a military treatment facility 45 minutes after sustaining injuries in a building fire from a mortar attack. He was trapped inside the building for around 20 minutes. On arrival, he is confused and appears uncomfortable. He has a Glasgow Coma Score of 13. His pulse is 113/min, respirations are 18/min, and blood pressure is 108/70 mm Hg. Pulse oximetry on room air shows an oxygen saturation of 96%. Examination shows multiple second-degree burns over the chest and bilateral upper extremities and third-degree burns over the face. There are black sediments seen within the nose and mouth. The lungs are clear to auscultation. Cardiac examination shows no abnormalities. The abdomen is soft and nontender. Intravenous fluid resuscitation is begun. Which of the following is the most appropriate next step in management?
- A. Insertion of nasogastric tube and enteral nutrition
- B. Intravenous antibiotic therapy
- C. Intubation and mechanical ventilation (Correct Answer)
- D. Immediate bronchoscopy
- E. Intravenous corticosteroid therapy
Airway management in trauma Explanation: ***Intubation and mechanical ventilation***
- The patient exhibits several signs of impending **airway compromise** due to **inhalation injury**, including perioral burns, black sediments in the nose and mouth, and being trapped in a fire.
- While current oxygen saturation is 96%, **airway edema** can rapidly worsen, leading to respiratory failure. **Early intubation** is crucial to secure the airway before it becomes obstructed.
*Insertion of nasogastric tube and enteral nutrition*
- A nasogastric tube is often placed in burn patients to decompress the stomach and provide nutritional support, but it is **not the immediate priority** when there is a risk of airway obstruction.
- **Enteral nutrition** is important but should be initiated only after airway control is established and the patient is stable for feeding.
*Intravenous antibiotic therapy*
- **Prophylactic antibiotics** are generally **not recommended** in the immediate management of burn patients unless there is clear evidence of infection, which is not present here.
- Unnecessary antibiotic use can lead to **antibiotic resistance** and fungal infections.
*Immediate bronchoscopy*
- While **bronchoscopy** can confirm the extent of inhalation injury, it is not the primary immediate step. **Securing the airway** through intubation takes precedence over diagnostic procedures when airway compromise is imminent.
- Bronchoscopy can be considered *after* intubation to assess the lower airway for damage and guide further management.
*Intravenous corticosteroid therapy*
- **Corticosteroids** are typically **contraindicated** in the management of inhalation injury because they can **impair immune function** and increase the risk of infection in burn patients.
- Evidence does not support the routine use of corticosteroids to reduce inflammation in inhalation injury, and they may worsen outcomes.
Airway management in trauma US Medical PG Question 5: A 24-year-old man is brought to the emergency department 30 minutes after being involved in a high-speed motor vehicle collision in which he was a restrained driver. On arrival, he is alert and oriented. His pulse is 112/min, respirations are 29/min, and blood pressure is 100/60 mm Hg. The pupils are equal and reactive to light. There is a 3-cm laceration over the forehead and multiple bruises over the trunk. The lungs are clear to auscultation. Cardiac examination shows no abnormalities. The abdomen is soft and nontender. The right knee is swollen and tender; range of motion is limited by pain. Infusion of 0.9% saline is begun and intravenous acetaminophen is administered. Two hours later, blood-tinged fluid spontaneously drains from both nostrils, and is made worse by leaning forward. On a piece of gauze, it shows up as a rapidly-expanding clear ring of fluid surrounding blood. Further evaluation of this patient is most likely to show which of the following?
- A. Numbness of upper cheek area
- B. Retroauricular ecchymosis
- C. Bilateral periorbital ecchymosis (Correct Answer)
- D. Cranial nerve XII palsy
- E. Carotid artery dissection
Airway management in trauma Explanation: **Bilateral periorbital ecchymosis**
- The clinical presentation, including head trauma from a **high-speed motor vehicle collision**, neurological symptoms like **blood-tinged fluid draining from both nostrils with a halo sign**, and hemodynamic instability (tachycardia and hypotension), points towards a **basilar skull fracture**.
- **Bilateral periorbital ecchymosis** (raccoon eyes) is a classic sign of a basilar skull fracture, particularly one involving the **anterior cranial fossa**, indicating extravasation of blood into the periorbital tissues.
*Numbness of upper cheek area*
- **Numbness of the upper cheek area** is associated with injury to the **infraorbital nerve**, which often occurs with **maxillary (Le Fort II or III) fractures** or **orbital floor fractures**.
- While midface fractures can occur in severe trauma, the **halo sign** from the nostrils is more indicative of a **CSF leak** associated with a **basilar skull fracture**, rather than isolated maxillary injury.
*Retroauricular ecchymosis*
- **Retroauricular ecchymosis** (Battle's sign) is also a sign of a **basilar skull fracture**, but it specifically indicates a fracture involving the **middle cranial fossa** and the **temporal bone**.
- While possible, the spontaneous draining of CSF from the nostrils (rhinorrhea) is more directly linked to an **anterior cranial fossa fracture** and involvement of the **cribriform plate**, making bilateral periorbital ecchymosis a more likely and specific finding in this context.
*Cranial nerve XII palsy*
- **Cranial nerve XII (hypoglossal) palsy** would result in **tongue deviation** and weakness, typically associated with injuries to the **posterior cranial fossa** or the **neck**.
- This is not a common finding with the presented symptoms of **rhinorrhea with a halo sign**, which points to an **anterior cranial fossa fracture**.
*Carotid artery dissection*
- **Carotid artery dissection** can occur after significant trauma and may present with headaches, neck pain, and focal neurological deficits such as **hemiparesis** or **cranial nerve deficits (e.g., Horner's syndrome)**.
- While trauma increases the risk, the specific symptom of **CSF rhinorrhea with a halo sign** is not characteristic of a carotid dissection but rather indicative of a **communication between the subarachnoid space and the nasal cavity** due to a skull base fracture.
Airway management in trauma US Medical PG Question 6: An obese 52-year-old man is brought to the emergency department because of increasing shortness of breath for the past 8 hours. Two months ago, he noticed a mass on the right side of his neck and was diagnosed with laryngeal cancer. He has smoked two packs of cigarettes daily for 27 years. He drinks two pints of rum daily. He appears ill. He is oriented to person, place, and time. His temperature is 37°C (98.6°F), pulse is 111/min, respirations are 34/min, and blood pressure is 140/90 mm Hg. Pulse oximetry on room air shows an oxygen saturation of 89%. Examination shows a 9-cm, tender, firm subglottic mass on the right side of the neck. Cervical lymphadenopathy is present. His breathing is labored and he has audible inspiratory stridor but is able to answer questions. The lungs are clear to auscultation. Arterial blood gas analysis on room air shows:
pH 7.36
PCO2 45 mm Hg
PO2 74 mm Hg
HCO3- 25 mEq/L
He has no advanced directive. Which of the following is the most appropriate next step in management?
- A. Comfort care measures
- B. Cricothyroidotomy (Correct Answer)
- C. Tracheostomy
- D. Intramuscular epinephrine
- E. Tracheal stenting
Airway management in trauma Explanation: ***Correct: Cricothyroidotomy***
- This patient has **impending complete airway obstruction** evidenced by inspiratory stridor, severe tachypnea (34/min), hypoxia (O2 sat 89%), and a large obstructing laryngeal mass
- **Cricothyroidotomy** is the emergent surgical airway procedure of choice when there is **imminent or actual complete upper airway obstruction** and endotracheal intubation cannot be safely performed
- The subglottic mass makes endotracheal intubation **extremely dangerous** - instrumentation could precipitate complete obstruction and inability to ventilate
- Cricothyroidotomy provides **immediate airway access** (can be performed in 30-60 seconds) below the level of obstruction, making it life-saving in this emergency
- In the "cannot intubate, cannot ventilate" scenario, cricothyroidotomy is the definitive emergency intervention per ATLS and airway management guidelines
*Incorrect: Tracheostomy*
- While tracheostomy provides definitive airway management, it is a **controlled, elective procedure** typically performed in the OR that takes 20-30 minutes
- This patient requires **immediate airway access** - waiting for OR setup and performing tracheostomy risks complete airway collapse and death
- Tracheostomy may be performed later as a planned procedure once the airway is secured with cricothyroidotomy
- The presence of stridor indicates **critical airway narrowing** requiring emergency intervention, not elective surgery
*Incorrect: Comfort care measures*
- The patient is **alert and oriented** without an advanced directive indicating wishes for comfort care only
- This is an **acute, reversible condition** with appropriate emergency airway intervention
- Presumed consent applies in life-threatening emergencies when the patient cannot formally consent but intervention would be life-saving
- Comfort care would be inappropriate without documented patient wishes or irreversible terminal condition
*Incorrect: Intramuscular epinephrine*
- Epinephrine is indicated for **anaphylaxis** or angioedema causing airway edema from allergic/inflammatory mechanisms
- This patient has **mechanical obstruction** from a solid tumor mass, which will not respond to epinephrine
- Epinephrine causes vasoconstriction and reduces mucosal edema but cannot reduce tumor mass
- Would delay definitive airway management and not address the underlying problem
*Incorrect: Tracheal stenting*
- Tracheal stenting requires **bronchoscopy** in a controlled setting and is used for palliation of tracheal narrowing
- Cannot be performed emergently in an unstable patient with impending airway obstruction
- The obstruction is at the **laryngeal/subglottic level**, not typically amenable to emergency stenting
- Requires time for procedure setup and sedation, which this patient cannot afford given the critical airway emergency
Airway management in trauma US Medical PG Question 7: A 17-year-old boy is brought to the emergency department by his brother after losing consciousness 1 hour ago. The brother reports that the patient was skateboarding outside when he fell on the ground and started to have generalized contractions. There was also some blood coming from his mouth. The contractions stopped after about 1 minute, but he remained unconscious for a few minutes afterward. He has never had a similar episode before. There is no personal or family history of serious illness. He does not smoke or drink alcohol. He does not use illicit drugs. He takes no medications. On arrival, he is confused and oriented only to person and place. He cannot recall what happened and reports diffuse muscle ache, headache, and fatigue. He appears pale. His temperature is 37°C (98.6°F), pulse is 80/min, and blood pressure is 130/80 mm Hg. There is a small wound on the left side of the tongue. A complete blood count and serum concentrations of electrolytes, urea nitrogen, and creatinine are within the reference ranges. Toxicology screening is negative. An ECG shows no abnormalities. Which of the following is the most appropriate next step in management?
- A. Electroencephalography
- B. Lumbar puncture
- C. Lorazepam therapy
- D. Reassurance and follow-up
- E. CT scan of the head (Correct Answer)
Airway management in trauma Explanation: ***CT scan of the head***
- Given the **first-time seizure** in an adolescent, especially with a history of head trauma (falling while skateboarding) and subsequent confusion, a **CT scan of the head** is crucial to rule out acute structural lesions like hemorrhage, mass, or edema.
- It is vital for identifying **life-threatening causes** of seizure that require immediate intervention, such as an **intracranial hematoma** or **mass lesion**, which could have been precipitated or exacerbated by the fall.
*Electroencephalography*
- **EEG** is appropriate for later evaluation to diagnose and classify seizure disorders, but it is not the *most appropriate initial step* in the emergency setting for a first-time seizure with a possible traumatic etiology.
- An EEG might be normal shortly after a seizure, and it does not rule out acute structural brain pathology that requires urgent management.
*Lumbar puncture*
- A **lumbar puncture** is indicated if there's suspicion of meningoencephalitis (e.g., fever, nuchal rigidity, immunocompromised status), which are not prominent features in this patient.
- The patient's vital signs are stable, and there are no signs of infection, making this a less urgent initial diagnostic step compared to imaging.
*Lorazepam therapy*
- **Lorazepam** is a benzodiazepine used to terminate ongoing seizures (**status epilepticus**), but this patient's generalized contractions have already stopped.
- Administering lorazepam when the seizure has resolved is unnecessary and would only cause further sedation.
*Reassurance and follow-up*
- While reassurance is part of patient care, it is *insufficient* as the sole next step for a **first-time seizure** episode in an adolescent, especially with features suggesting a possible underlying acute cause.
- A thorough diagnostic workup, beginning with neuroimaging, is necessary to ensure there is no serious underlying pathology before considering discharge and follow-up.
Airway management in trauma US Medical PG Question 8: A 47-year-old man is admitted to the emergency room after a fight in which he was hit in the head with a hammer. The witnesses say that the patient initially lost consciousness, but regained consciousness by the time emergency services arrived. On admission, the patient complained of a diffuse headache. He opened his eyes spontaneously, was verbally responsive, albeit confused, and was able to follow commands. He could not elevate his left hand and leg. He did not remember the events prior to the loss of consciousness and had difficulty remembering information, such as the names of nurses or doctors. His airway was not compromised. The vital signs are as follows: blood pressure, 180/100 mm Hg; heart rate, 59/min; respiratory rate, 12/min; temperature 37.0℃ (98.6℉); and SaO2, 96% on room air. The examination revealed bruising in the right frontotemporal region. The pupils are round, equal, and show a poor response to light. The neurologic examination shows hyperreflexia and decreased power in the left upper and lower limbs. There is questionable nuchal rigidity, but no Kernig and Brudzinski signs. The CT scan is shown in the image. Which of the following options is recommended for this patient?
- A. Lumbar puncture
- B. Decompressive craniectomy
- C. Administration of levetiracetam
- D. Administration of methylprednisolone
- E. Surgical evacuation of the clots (Correct Answer)
Airway management in trauma Explanation: ***Surgical evacuation of the clots***
- The CT scan image shows a **biconvex (lenticular) hyperdensity** consistent with an **epidural hematoma (EDH)**, which typically results from arterial bleeding (often from the **middle meningeal artery**). This patient's **"lucid interval"** (initial loss of consciousness, regain consciousness, then deterioration) is classic for EDH.
- Given the patient's neurological deterioration (left-sided weakness, pupillary changes, confusion, memory issues) and signs of increased intracranial pressure (hypertension, bradycardia - part of Cushing's triad), urgent surgical evacuation of the hematoma is indicated to relieve pressure and prevent herniation.
*Lumbar puncture*
- A lumbar puncture is **contraindicated** in the setting of suspected or confirmed **increased intracranial pressure (ICP)**, as it can precipitate **cerebral herniation**.
- The CT scan clearly demonstrates a space-occupying lesion, making a lumbar puncture unnecessary and potentially dangerous.
*Decompressive craniectomy*
- While decompressive craniectomy is a neurosurgical procedure used to reduce ICP, it is generally considered when other measures have failed or in cases of **diffuse brain swelling** or large **intracerebral hematomas** not amenable to simple evacuation.
- In this case of a localized epidural hematoma with a clear surgical target, direct evacuation is the primary and most effective intervention.
*Administration of levetiracetam*
- Levetiracetam is an **anticonvulsant** used to prevent seizures. While seizures can occur after traumatic brain injury, there is no indication that the patient is currently seizing.
- Prophylactic anticonvulsants are sometimes used in severe TBI, but addressing the life-threatening hematoma takes **precedence** over seizure prophylaxis.
*Administration of methylprednisolone*
- **Corticosteroids** like methylprednisolone are generally **contraindicated** in traumatic brain injury (TBI) as studies have shown **worse outcomes** and increased mortality.
- They are primarily used for their **anti-inflammatory effects** in conditions like spinal cord injury or vasogenic edema from tumors, not for acute head trauma with hematoma.
Airway management in trauma US Medical PG Question 9: A mass casualty incident occurs with 25 casualties arriving simultaneously at a community hospital emergency department. The trauma team has limited resources with 2 operating rooms available and 4 surgeons present. Among the arriving patients: Patient A has traumatic amputation of forearm with tourniquet in place and stable vitals; Patient B has flail chest, respiratory distress, and unstable vitals; Patient C is in cardiac arrest with penetrating chest wound; Patient D has a femur fracture with stable vitals; Patient E has GCS 4 with bilateral blown pupils. Evaluate the triage priority according to ATLS mass casualty protocols.
- A. Priority order: C, E, B, A, D - treat most severely injured first
- B. Priority order: B, A, D, with E and C designated expectant (Correct Answer)
- C. Priority order: A, D, B, E, C - treat all patients equally regardless of prognosis
- D. Priority order: B, A, E, D, C - based on severity alone
- E. Immediate evacuation of all patients to a higher level trauma center
Airway management in trauma Explanation: ***Priority order: B, A, D, with E and C designated expectant***
- In a **mass casualty incident (MCI)** with limited resources, the goal is to provide the **greatest good for the greatest number**; Patient B has life-threatening but **salvageable** injuries (respiratory distress) making them the top priority.
- Patients C (cardiac arrest) and E (GCS 4, blown pupils) are classified as **expectant (black tag)** because their survival probability is minimal and resuscitating them would exhaust resources needed for salvageable patients.
*Priority order: C, E, B, A, D - treat most severely injured first*
- This approach is used in standard trauma situations where resources are ample, but it is incorrect in an **MCI** where resource-heavy, low-prognosis patients are de-prioritized.
- Assigning highest priority to **cardiac arrest (C)** and **severe brain injury (E)** would likely result in the deaths of more salvageable patients like Patient B.
*Priority order: A, D, B, E, C - treat all patients equally regardless of prognosis*
- Treating all patients equally ignores the **ATLS triage categories** (Immediate, Delayed, Minimal, Expectant) and fails to address life-threatening priorities first.
- While A and D have stable vitals and are **Delayed (Yellow tag)**, waiting to treat Patient B's airway/breathing emergency would lead to a preventable death.
*Priority order: B, A, E, D, C - based on severity alone*
- Severity alone does not dictate priority in an MCI; the **likelihood of survival** with the available resources must be considered.
- Patient E, despite being "severe," has a **devastating neurological prognosis** (blown pupils, GCS 4) and should not be prioritized over stable patients with better outcomes like A and D.
*Immediate evacuation of all patients to a higher level trauma center*
- Evacuation is a secondary step; the primary task according to **ATLS protocols** is to perform triage and stabilization at the current facility during the initial influx.
- Attempting to evacuate all 25 casualties simultaneously without triage would overwhelm transport systems and delay life-saving **initial stabilization** for patients like B.
Airway management in trauma US Medical PG Question 10: A 35-year-old pregnant woman at 32 weeks gestation is involved in a motor vehicle collision. She is hemodynamically stable with blood pressure 105/70 mmHg, heart rate 100/min. She has left upper quadrant tenderness and left lower rib fractures. FAST examination shows fluid in the splenorenal recess. Fetal heart tones are 150/min and reassuring. CT scan shows a Grade III splenic laceration. After 6 hours of observation with stable vital signs and hemoglobin, she suddenly develops blood pressure 85/50 mmHg and heart rate 125/min. Evaluate the management priority.
- A. Initiate massive transfusion and reassess after maternal stabilization
- B. Perform emergency cesarean section first, then address splenic injury
- C. Simultaneous laparotomy with splenectomy and obstetric standby for potential cesarean (Correct Answer)
- D. Proceed with splenectomy only, as maternal stabilization is the priority
- E. Perform angioembolization of splenic artery to avoid surgery
Airway management in trauma Explanation: ***Simultaneous laparotomy with splenectomy and obstetric standby for potential cesarean***
- The patient has failed **non-operative management** of a splenic injury and is now **hemodynamically unstable**, necessitating immediate **laparotomy** to control hemorrhage.
- At **32 weeks gestation**, the fetus is viable; therefore, an **obstetric standby** is essential to perform a cesarean section if the mother's condition does not improve or if **fetal distress** occurs during the procedure.
*Initiate massive transfusion and reassess after maternal stabilization*
- While **massive transfusion** is part of trauma resuscitation, delaying surgery in an unstable patient with a known **Grade III splenic laceration** and hemodynamic collapse is inappropriate.
- Definitive **hemorrhage control** (surgery) is the priority once a patient becomes unstable after initial observation.
*Perform emergency cesarean section first, then address splenic injury*
- Performing a cesarean section first in an unstable trauma patient with **intra-abdominal hemorrhage** increases maternal morbidity and can worsen **hypovolemic shock**.
- Maternal stabilization and controlling the source of **bleeding** (splenectomy) is the most critical step to ensure both maternal and fetal survival.
*Proceed with splenectomy only, as maternal stabilization is the priority*
- While maternal stabilization is the priority, ignoring the viable fetus during a major surgical intervention is suboptimal care.
- Failure to involve an **obstetric team** overlooks the risk of **placental abruption** or fetal distress induced by maternal hypotension during surgery.
*Perform angioembolization of splenic artery to avoid surgery*
- **Angioembolization** is only indicated for stable patients; this patient is **hemodynamically unstable** (BP 85/50, HR 125), which is a contraindication for the interventional radiology suite.
- In the setting of active **intraperitoneal hemorrhage** and shock, an emergent **exploratory laparotomy** is the standard of care.
More Airway management in trauma US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.