ATLS protocols

On this page
🚨 ATLS Command Center: The Trauma Response Blueprint
You'll master the systematic approach that transforms chaotic trauma scenes into controlled, life-saving sequences. This lesson builds your command of ATLS protocols from initial triage decisions through primary survey execution, secondary assessment, and evidence-based resuscitation strategies. You'll learn why the ABCDE sequence prevents missed injuries, how to prioritize competing threats, and when protocols demand deviation. By integrating these frameworks, you'll develop the clinical judgment to manage multi-system trauma with precision and confidence under pressure.
📌 Remember: ABCDE - Airway with C-spine, Breathing, Circulation, Disability (neuro), Exposure/Environment. Each step must be completed before advancing to the next, with immediate intervention for any life-threatening findings.
The ATLS framework operates on three fundamental principles: treat the greatest threat to life first, lack of a definitive diagnosis never impedes treatment, and detailed history is not essential to begin evaluation. These principles guide decision-making when multiple injuries compete for attention and time is critical.
- Primary Survey Components
- Airway assessment with C-spine protection (<30 seconds)
- Breathing evaluation and ventilation support (<60 seconds)
- Circulation with hemorrhage control (<90 seconds)
- Blood pressure maintenance above 90 mmHg systolic
- Heart rate monitoring for shock indicators
- Immediate vascular access with 2 large-bore IVs
- Disability assessment using Glasgow Coma Scale
- GCS ≤8 indicates severe brain injury
- Pupil examination for herniation signs
- Exposure with environmental control
- Complete undressing for full examination
- Temperature maintenance above 36°C
⭐ Clinical Pearl: The "Golden Hour" concept emphasizes that 60% of preventable trauma deaths occur within the first hour. ATLS protocols maximize survival by ensuring systematic evaluation within 10-15 minutes of arrival.
| ATLS Component | Time Target | Critical Threshold | Intervention Priority | |---|---|---|---|---| | Airway Assessment | <30 seconds | Obstruction/Stridor | Immediate intubation | | Breathing Evaluation | <60 seconds | RR <10 or >29 | Ventilatory support | | Circulation Check | <90 seconds | SBP <90 mmHg | Fluid resuscitation | | Disability Screen | <2 minutes | GCS ≤8 | Neuroprotection | | Exposure Complete | <5 minutes | Temp <36°C | Warming measures |> 💡 Master This: ATLS success depends on simultaneous assessment and treatment. Unlike medical scenarios where diagnosis precedes treatment, trauma care requires immediate intervention for life threats while continuing evaluation. This parallel processing approach reduces mortality by 15-20% compared to sequential evaluation methods.
The protocol's strength lies in its reproducible methodology that functions regardless of provider experience level. Studies demonstrate that ATLS-trained physicians identify 95% of life-threatening injuries during primary survey, compared to 78% identification rates with non-standardized approaches.
Connect this systematic foundation through secondary survey principles to understand comprehensive trauma evaluation patterns.
🚨 ATLS Command Center: The Trauma Response Blueprint
⚡ The Trauma Triage Matrix: Sorting Life and Death
📌 Remember: PAMP - Physiological first (vital signs), Anatomical second (injury patterns), Mechanism third (energy transfer), Patient factors last (age, comorbidities). This hierarchy ensures the most critically injured receive immediate attention.
Physiological Triage Criteria represent the most sensitive predictors of severe injury, with 85-90% correlation with need for immediate intervention:
- Cardiovascular Indicators
- Systolic blood pressure <90 mmHg (shock threshold)
- Heart rate >120 bpm in adults
- Pulse pressure <25 mmHg (narrow pulse pressure)
- Indicates significant blood loss (>30% blood volume)
- Requires immediate fluid resuscitation
- Predicts need for blood transfusion in 75% of cases
- Respiratory Parameters
- Respiratory rate <10 or >29 breaths/minute
- Oxygen saturation <90% on room air
- Need for ventilatory support or intubation
- Neurological Assessment
- Glasgow Coma Scale ≤13
- Paralysis or neurological deficit
- Penetrating injury to head, neck, torso, extremities
⭐ Clinical Pearl: The Revised Trauma Score (RTS) combines GCS, systolic BP, and respiratory rate with weighted values. An RTS <7.84 indicates 90% probability of requiring immediate surgical intervention and correlates with 25% mortality risk.
Anatomical Criteria focus on injury patterns that typically require specialized care, regardless of initial vital signs:
- High-Energy Transfer Injuries
- Penetrating injuries to head, neck, torso, extremities proximal to elbow/knee
- Chest wall instability or flail chest
- Two or more proximal long-bone fractures
- Femur fractures can cause 1-2 liter blood loss
- Pelvic fractures may result in 3-4 liter hemorrhage
- Multiple fractures increase mortality by 40%
- Crush and Amputation Injuries
- Crushed, degloved, or mangled extremity
- Amputation proximal to wrist or ankle
- Pelvic fractures with hemodynamic instability
💡 Master This: Mechanism of injury provides crucial information about energy transfer and potential occult injuries. High-energy mechanisms (>40 mph motor vehicle crashes, >20 foot falls) can cause significant internal injuries despite normal initial vital signs. 15-20% of patients with high-energy mechanisms develop delayed complications requiring intervention.
| Triage Level | Response Time | Team Composition | Survival Benefit | |---|---|---|---|---| | Level 1 (Red) | <5 minutes | Full trauma team (8-12 providers) | 35% mortality reduction | | Level 2 (Yellow) | <15 minutes | Partial team (4-6 providers) | 20% mortality reduction | | Level 3 (Green) | <30 minutes | Physician + nurse | 10% mortality reduction | | Level 4 (Blue) | <60 minutes | Standard ED evaluation | Baseline comparison |The triage system's effectiveness depends on over-triage and under-triage balance. Optimal systems maintain over-triage rates of 25-35% (ensuring no critical cases are missed) while keeping under-triage below 5% (preventing delayed care for severe injuries).
Connect these triage principles through primary survey methodology to understand systematic trauma evaluation approaches.
⚡ The Trauma Triage Matrix: Sorting Life and Death
🎯 The Primary Survey Precision Protocol: ABCDE Mastery
Airway with C-spine Protection forms the foundation of trauma evaluation, as airway compromise can cause death within 3-4 minutes:
- Assessment Techniques
- Look: Facial trauma, foreign bodies, vomit, blood
- Listen: Stridor, gurgling, hoarseness, voice changes
- Feel: Air movement, subcutaneous emphysema, tracheal deviation
- Stridor indicates >50% airway obstruction
- Hoarseness suggests laryngeal injury in 85% of cases
- Subcutaneous emphysema indicates pneumothorax in 90% of presentations
- C-spine Considerations
- Maintain neutral alignment during all airway maneuvers
- 15% of cervical spine injuries occur without neurological deficit
- High-risk mechanisms require immobilization until cleared
📌 Remember: LEMON assessment for difficult airway - Look externally, Evaluate 3-3-2 rule, Mallampati score, Obstruction signs, Neck mobility. Any positive finding increases intubation difficulty by 300-400%.
Breathing and Ventilation assessment identifies immediately life-threatening thoracic injuries requiring intervention within 5-10 minutes:
- Life-Threatening Conditions
- Tension pneumothorax: Immediate needle decompression at 2nd intercostal space, midclavicular line
- Open pneumothorax: Three-sided occlusive dressing, monitor for tension development
- Flail chest: ≥3 consecutive ribs fractured in ≥2 places, requires positive pressure ventilation
- Associated with 25-30% mortality
- 50% develop respiratory failure
- Underlying pulmonary contusion in 75% of cases
- Massive hemothorax: >1500 mL blood loss or >200 mL/hour drainage
⭐ Clinical Pearl: Respiratory rate >29 or <10 breaths/minute indicates severe respiratory compromise requiring immediate intervention. Normal respiratory rate with poor air movement suggests tension pneumothorax or massive hemothorax in 85% of trauma cases.
Circulation with Hemorrhage Control addresses the leading cause of preventable trauma death:
- Shock Recognition
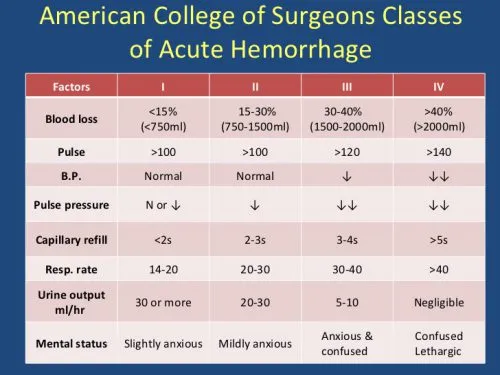
- Class I: <15% blood loss, normal vital signs
- Class II: 15-30% loss, tachycardia >100 bpm, narrow pulse pressure
- Class III: 30-40% loss, hypotension, altered mental status
- Class IV: >40% loss, severe hypotension, obtunded
- Class III-IV require immediate blood transfusion
- Mortality increases exponentially with each class
- Lactate >4 mmol/L indicates severe shock
💡 Master This: Permissive hypotension maintains systolic BP 80-90 mmHg in penetrating trauma until surgical control achieved. Aggressive fluid resuscitation can increase mortality by 15-20% by disrupting clot formation and causing dilutional coagulopathy.
| Assessment Component | Normal Values | Intervention Threshold | Immediate Action | |---|---|---|---|---| | Airway Patency | Clear, audible speech | Stridor, obstruction | Definitive airway | | Respiratory Rate | 12-20/min | <10 or >29/min | Ventilatory support | | Oxygen Saturation | >95% | <90% | Supplemental O2 | | Systolic BP | >90 mmHg | <90 mmHg | Fluid resuscitation | | Heart Rate | 60-100 bpm | >120 bpm | Volume replacement | | Glasgow Coma Scale | 15 | ≤13 | Neuroprotection |Connect this systematic assessment approach through secondary survey techniques to understand comprehensive trauma evaluation methodology.
🎯 The Primary Survey Precision Protocol: ABCDE Mastery
🔍 The Secondary Survey Architecture: Systematic Discovery
Head-to-Toe Examination Sequence follows anatomical progression to ensure complete evaluation:
- Head and Maxillofacial Assessment
- Scalp: Lacerations, hematomas, depressed skull fractures
- Eyes: Pupil reactivity, visual acuity, extraocular movements
- Anisocoria >2mm suggests intracranial pressure elevation
- Raccoon eyes indicate basilar skull fracture in 75% of cases
- Battle's sign appears 12-24 hours post-injury
- Ears: Hemotympanum, CSF otorrhea, hearing assessment
- Nose: Deformity, epistaxis, CSF rhinorrhea
- Mouth: Dental trauma, tongue lacerations, airway foreign bodies
📌 Remember: SCALP layers for head injury assessment - Skin, Connective tissue, Aponeurosis, Loose connective tissue, Pericranium. Injuries to aponeurosis require layered closure to prevent gaping wounds and cosmetic deformity.
Cervical Spine and Neck Evaluation requires systematic palpation and neurological assessment:
- NEXUS Criteria for cervical spine clearance (all must be present):
- No posterior midline cervical tenderness
- No evidence of intoxication
- Normal level of alertness
- No focal neurological deficit
- No painful distracting injuries
- 99.6% sensitivity for clinically significant injuries
- Reduces imaging by 25-30% in appropriate patients
- False negative rate <0.1% when properly applied
Thoracic Examination identifies potentially life-threatening injuries missed during primary survey:
- Inspection and Palpation
- Chest wall: Contusions, abrasions, penetrating wounds
- Respiratory pattern: Symmetry, depth, accessory muscle use
- Subcutaneous emphysema: Indicates pneumothorax or airway injury
- Present in 60-70% of pneumothoraces
- May indicate tracheobronchial injury if extensive
- Can compromise airway if severe
- Auscultation Findings
- Decreased breath sounds: Pneumothorax, hemothorax, contusion
- Heart sounds: Muffled sounds suggest pericardial tamponade
- Bowel sounds in chest: Diaphragmatic rupture
⭐ Clinical Pearl: Potentially life-threatening thoracic injuries include pulmonary contusion (most common), aortic disruption (90% mortality if untreated), esophageal rupture (high morbidity), and diaphragmatic injury (often missed initially). These require high index of suspicion and appropriate imaging.
Abdominal Assessment challenges clinicians due to subtle presentation of serious injuries:
- Physical Examination Limitations
- Sensitivity only 65-70% for intra-abdominal injury
- False negative rate 15-20% in conscious patients
- Unreliable in presence of altered mental status, spinal cord injury, intoxication
- Diagnostic Adjuncts
- FAST exam: 95% specificity for hemoperitoneum, 85% sensitivity
- CT abdomen/pelvis: 98% accuracy for organ injury
- Diagnostic peritoneal lavage: >95% sensitivity but invasive
💡 Master This: Seat belt sign (abdominal wall contusion from restraint) indicates 15-20% risk of intra-abdominal injury, particularly bowel and mesenteric injuries that may not appear on initial CT. These patients require serial examinations and 24-48 hour observation for delayed presentation.
| Body Region | Key Assessment Points | Critical Findings | Missed Injury Rate | |---|---|---|---|---| | Head/Face | GCS, pupils, facial stability | Anisocoria >2mm, CSF leak | 5-8% | | C-spine | NEXUS criteria, palpation | Midline tenderness, deficit | 2-3% | | Chest | Breath sounds, wall integrity | Asymmetry, subcutaneous air | 10-15% | | Abdomen | Tenderness, distension | Seat belt sign, rigidity | 15-20% | | Pelvis | Stability, rectal exam | Instability, blood at meatus | 8-12% | | Extremities | Pulses, motor/sensory | Absent pulse, deformity | 12-18% |Connect this comprehensive evaluation methodology through adjunctive studies and monitoring to understand complete trauma assessment protocols.
🔍 The Secondary Survey Architecture: Systematic Discovery
⚖️ The Resuscitation Command Matrix: Evidence-Based Interventions
Damage Control Resuscitation represents the paradigm shift toward early blood product administration and permissive hypotension:
- Massive Transfusion Protocol (MTP) activation criteria:
- Systolic BP <90 mmHg with penetrating torso injury
- Systolic BP <70 mmHg with any mechanism
- Heart rate >120 bpm with clinical signs of shock
- Positive FAST with hemodynamic instability
- Early activation reduces mortality by 35-40%
- 1:1:1 ratio (RBC:FFP:Platelets) improves survival
- Tranexamic acid within 3 hours reduces bleeding deaths by 15%
Fluid Resuscitation Strategies balance tissue perfusion with hemorrhage control:
- Permissive Hypotension targets:
- Penetrating trauma: SBP 80-90 mmHg until surgical control
- Blunt trauma: SBP 90-100 mmHg (higher target due to potential TBI)
- Traumatic brain injury: SBP >100 mmHg to maintain cerebral perfusion
- Aggressive resuscitation can increase bleeding by 200-300%
- Clot disruption occurs with SBP >100 mmHg in uncontrolled hemorrhage
- Mortality increases 15-20% with over-resuscitation
📌 Remember: CRASH-2 study demonstrated tranexamic acid 1g IV within 3 hours of injury reduces bleeding deaths by 15% without increasing thrombotic complications. Give 1g over 10 minutes, then 1g over 8 hours.
Coagulopathy Management addresses the lethal triad of hypothermia, acidosis, and coagulopathy:
- Acute Traumatic Coagulopathy occurs in 25-30% of severely injured patients:
- Tissue factor release activates coagulation cascade
- Protein C activation causes anticoagulation
- Fibrinolysis activation breaks down clots
- Develops within minutes of injury
- Independent predictor of mortality
- Worsened by crystalloid dilution and hypothermia
- Point-of-Care Testing guides targeted therapy:
- TEG/ROTEM provides real-time coagulation assessment
- Fibrinogen <150 mg/dL requires cryoprecipitate
- Platelet count <50,000 requires platelet transfusion
⭐ Clinical Pearl: Hypothermia develops rapidly in trauma patients, with core temperature dropping 1-2°C within 30 minutes of exposure. Temperature <35°C increases mortality by 100% and impairs coagulation function by 50%. Aggressive warming measures are essential.
Hemodynamic Monitoring guides resuscitation endpoints:
- Traditional Endpoints (blood pressure, heart rate) are insensitive indicators:
- Young patients compensate until 30-40% blood loss
- Elderly patients decompensate with 15-20% loss
- Medications (beta-blockers) mask tachycardic response
- Advanced Monitoring provides earlier detection:
- Base deficit >-6 indicates significant shock
- Lactate >4 mmol/L suggests inadequate perfusion
- ScvO2 <70% indicates ongoing oxygen debt
💡 Master This: Damage control surgery focuses on controlling hemorrhage and contamination rather than definitive repair. Abbreviated procedures reduce operative time by 60-70% and improve survival in critically injured patients by allowing physiological optimization before definitive repair.
| Resuscitation Component | Target Parameter | Evidence Level | Mortality Benefit | |---|---|---|---|---| | Blood Pressure | SBP 80-90 mmHg (penetrating) | Level I | 15-20% reduction | | Transfusion Ratio | 1:1:1 (RBC:FFP:PLT) | Level I | 25-30% reduction | | Tranexamic Acid | 1g within 3 hours | Level I | 15% bleeding death reduction | | Temperature | Core temp >36°C | Level II | 50% coagulopathy improvement | | Base Deficit | >-6 mEq/L | Level II | Early shock detection | | Lactate | <4 mmol/L | Level II | Perfusion adequacy marker |Connect these resuscitation principles through definitive care planning to understand comprehensive trauma management strategies.
⚖️ The Resuscitation Command Matrix: Evidence-Based Interventions
🔗 The Integration Command Center: Multi-System Trauma Mastery
Polytrauma Scoring Systems quantify injury severity and predict outcomes:
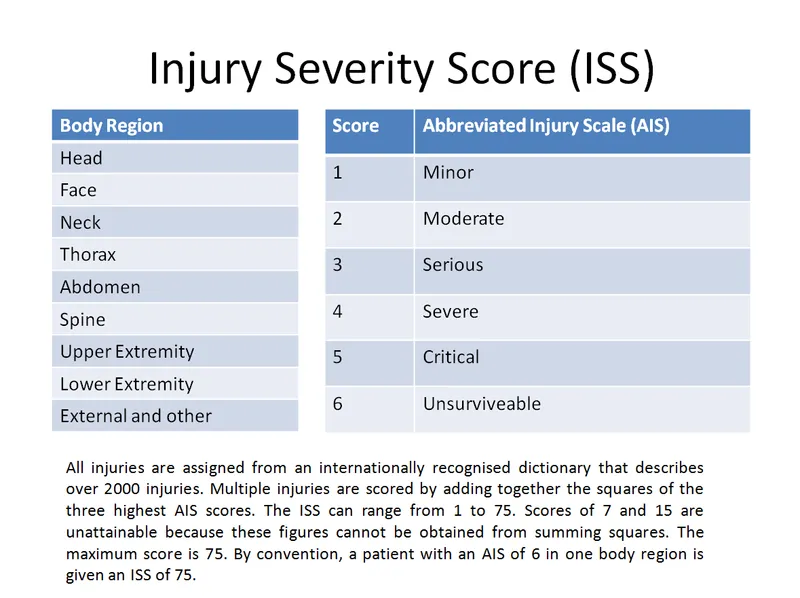
- Injury Severity Score (ISS) calculation:
- Sum of squares of three highest AIS scores from different body regions
- ISS >15 defines major trauma (10% mortality)
- ISS >25 indicates severe trauma (25% mortality)
- ISS >40 suggests critical trauma (50% mortality)
- Maximum score 75 (incompatible with life)
- Correlates strongly with length of stay and resource utilization
- Underestimates mortality in elderly patients
Systems Integration Challenges require coordinated decision-making:
- Competing Surgical Priorities require systematic approach:
- Immediate life threats: Hemorrhage control, airway management
- Urgent interventions: Intracranial pressure control, compartment syndrome
- Semi-urgent procedures: Open fracture fixation, vascular repair
- Delayed interventions: Reconstructive procedures, rehabilitation
- Damage control principles guide initial management
- Physiological optimization before definitive repair
- Staged procedures reduce complications by 30-40%
📌 Remember: ATLS priorities remain constant in polytrauma - treat the greatest threat to life first. Hemorrhage control takes precedence over fracture fixation, and airway management supersedes neurological intervention if both are immediately life-threatening.
Trauma-Induced Coagulopathy complicates multi-system injuries:
- Pathophysiology involves multiple mechanisms:
- Tissue factor release from injured tissues
- Protein C pathway activation causing anticoagulation
- Fibrinolysis enhancement breaking down clots
- Platelet dysfunction from activation and consumption
- Occurs in 25-30% of severely injured patients
- Independent predictor of mortality (OR 4.2)
- Worsened by hypothermia, acidosis, dilution
- Management Strategies:
- Early recognition through point-of-care testing
- Targeted therapy based on specific deficits
- Antifibrinolytic agents (tranexamic acid) within 3 hours
- Factor concentrates for specific deficiencies
⭐ Clinical Pearl: Secondary brain injury from hypotension and hypoxia causes more morbidity than primary brain injury in 60% of TBI patients. Maintaining SBP >100 mmHg and PaO2 >60 mmHg reduces secondary injury and improves neurological outcomes by 25-30%.
Resource Allocation in polytrauma requires strategic planning:
- Operating Room Coordination:
- Multiple teams may require simultaneous access
- Equipment conflicts (C-arm, microscope) need resolution
- Anesthesia considerations for prolonged procedures
- Blood bank coordination for massive transfusion
- Average OR time increases 200-300% with multiple teams
- Complication rates increase with prolonged procedures
- Staged approach reduces overall morbidity
💡 Master This: Tertiary survey performed 24-48 hours after admission identifies 15-20% of missed injuries in polytrauma patients. Systematic re-examination when patient is stable, awake, and cooperative reveals injuries missed during initial evaluation due to distracting injuries and altered mental status.
| System Involvement | Mortality Rate | Key Interventions | Time Sensitivity | |---|---|---|---|---| | Single System | 5-10% | Standard protocols | Routine urgency | | Two Systems | 15-25% | Coordinated care | Urgent priority | | Three Systems | 30-45% | Multidisciplinary approach | Immediate action | | Four+ Systems | 50-70% | Damage control strategy | Life-threatening |Quality Improvement in polytrauma focuses on system-wide optimization:
- Performance Indicators:
- Time to OR for life-threatening hemorrhage (<60 minutes)
- Missed injury rate (<5% for significant injuries)
- Preventable death rate (<2% in Level I centers)
- Functional outcomes at 6 months and 1 year
- Multidisciplinary rounds improve communication
- Standardized protocols reduce variation in care
- Regular case review identifies improvement opportunities
Connect this integrated approach through quality metrics and outcome optimization to understand comprehensive trauma system performance.
🔗 The Integration Command Center: Multi-System Trauma Mastery
🎯 The ATLS Mastery Arsenal: Rapid Response Excellence
Essential ATLS Command Thresholds for immediate clinical application:
📌 Remember: "10-5-2-1" Rule - 10 minutes for primary survey completion, 5 minutes for life-threatening intervention, 2 large-bore IVs, 1 systematic approach. This framework ensures no critical steps are omitted under pressure.
- Critical Time Targets
- Airway assessment: <30 seconds to decision
- Breathing evaluation: <60 seconds to intervention
- Circulation control: <90 seconds to vascular access
- Disability screen: <2 minutes to GCS documentation
- Exposure complete: <5 minutes to full assessment
- Door-to-CT time: <25 minutes for stable patients
- Door-to-OR time: <60 minutes for hemorrhage control
- Blood availability: <15 minutes for type-specific
Rapid Assessment Decision Matrix for pattern recognition mastery:
| Clinical Finding | Immediate Concern | Intervention | Success Threshold | |---|---|---|---|---| | Stridor + agitation | Airway obstruction | Surgical airway | Air movement restored | | Absent breath sounds + hypotension | Tension pneumothorax | Needle decompression | BP improvement >20 mmHg | | Distended neck veins + muffled heart | Cardiac tamponade | Pericardiocentesis | Pulse pressure >25 mmHg | | Rigid abdomen + hypotension | Hemoperitoneum | Emergency laparotomy | Hemorrhage control | | GCS ≤8 + blown pupil | Herniation syndrome | Hyperventilation + mannitol | ICP <20 mmHg |> ⭐ Clinical Pearl: "Failure to respond to resuscitation" indicates ongoing hemorrhage in 85% of cases. If patient requires >2 liters crystalloid or >4 units PRBC to maintain vital signs, immediate surgical exploration is indicated regardless of imaging results.
ATLS Performance Optimization Strategies:
- Team Communication Protocols
- Closed-loop communication: Confirm all orders verbally
- Role designation: Clear team leader identification
- Information sharing: Systematic handoff protocols
- Decision documentation: Real-time recording of interventions
- Communication failures cause 30% of medical errors
- Structured handoffs reduce errors by 40-50%
- Team training improves performance by 25-30%
💡 Master This: Cognitive aids and checklists reduce error rates by 50-60% in high-stress situations. Memory-based performance degrades under pressure, while systematic protocols maintain consistency regardless of provider experience or stress level.
Advanced ATLS Integration Points:
-
Damage Control Principles
- Stop the bleeding: Hemorrhage control priority
- Prevent contamination: Bowel injury management
- Restore physiology: Temperature, coagulation, acid-base
- Definitive repair: When patient physiologically optimized
- Survival improves 40-50% with damage control approach
- ICU length of stay reduced by 30%
- Complication rates decreased by 25%
-
Quality Metrics for ATLS Excellence
- Primary survey completion: <10 minutes in 95% of cases
- Missed injury rate: <5% for significant injuries
- Preventable death rate: <2% in trauma centers
- Patient satisfaction: >90% with communication and care
- Continuous improvement through case review
- Simulation training maintains skill proficiency
- Outcome tracking identifies system weaknesses
⚠️ Critical Warning: Never proceed to secondary survey until primary survey is complete and vital signs are stable. 15-20% of preventable deaths result from premature advancement through ATLS sequence without addressing life threats.
ATLS Mastery Validation Checklist:
- ✓ Systematic approach maintained under pressure
- ✓ Time targets consistently achieved
- ✓ Team coordination optimized for efficiency
- ✓ Communication protocols followed precisely
- ✓ Quality metrics tracked and improved
- ✓ Continuous learning through case review and simulation
Master these ATLS principles, and you possess the systematic framework that transforms chaotic trauma scenarios into organized, life-saving interventions with measurable outcome improvements and reduced preventable mortality.
🎯 The ATLS Mastery Arsenal: Rapid Response Excellence
Practice Questions: ATLS protocols
Test your understanding with these related questions
A 35-year-old woman with no significant past medical history is brought in by ambulance after a major motor vehicle collision. Temperature is 97.8 deg F (36.5 deg C), blood pressure is 76/40, pulse is 110/min, and respirations are 12/min. She arouses to painful stimuli and makes incomprehensible sounds, but is unable to answer questions. Her abdomen is distended and diffusely tender to palpation. Bedside ultrasound shows blood in the peritoneal cavity. Her husband rushes to the bedside and states she is a Jehovah’s Witness and will refuse blood products. No documentation of blood refusal is available for the patient. What is the most appropriate next step in management?













