Regional anesthesia techniques US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Regional anesthesia techniques. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Regional anesthesia techniques US Medical PG Question 1: A 4-year-old boy is brought to the emergency department by his mother after cutting his buttock on a piece of broken glass. There is a 5-cm curvilinear laceration over the patient's right buttock. His vital signs are unremarkable. The decision to repair the laceration is made. Which of the following will offer the longest anesthesia for the laceration repair?
- A. Lidocaine
- B. Lidocaine mixed with bupivacaine
- C. Bupivacaine with epinephrine (Correct Answer)
- D. Lidocaine with epinephrine
- E. Bupivacaine
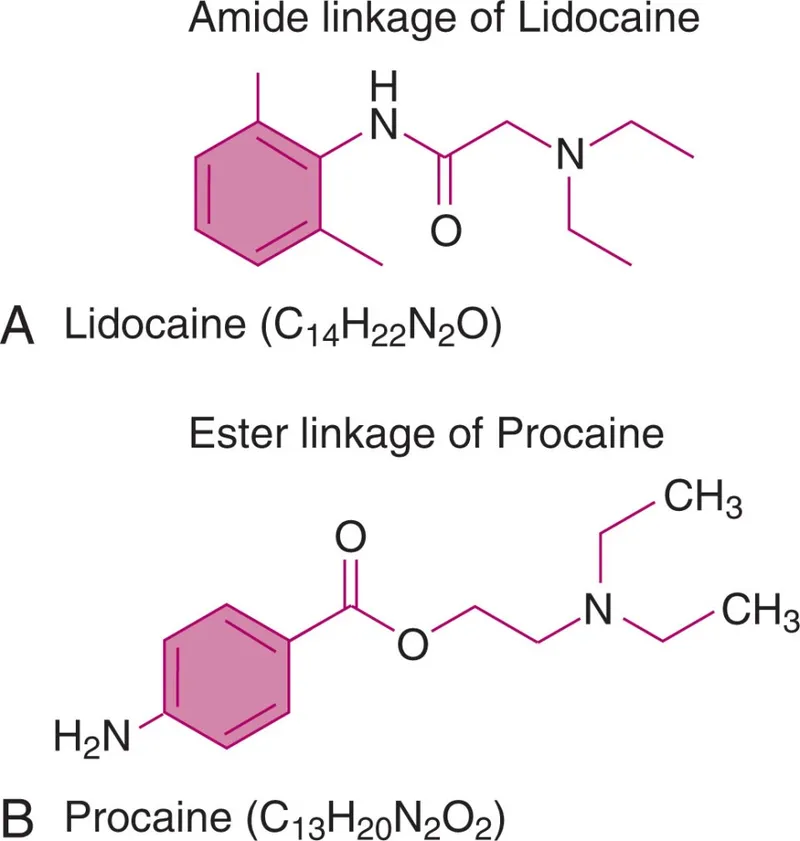
Regional anesthesia techniques Explanation: ***Bupivacaine with epinephrine***
- **Bupivacaine** is a long-acting local anesthetic, and adding **epinephrine** to it further prolongs its duration of action by causing vasoconstriction, which slows systemic absorption.
- This combination would provide the **longest duration of anesthesia** suitable for a laceration repair that requires extended pain control.
*Lidocaine*
- **Lidocaine** is an intermediate-acting local anesthetic with a relatively shorter duration of action compared to bupivacaine.
- While effective for initial anesthesia, its effect would likely wear off sooner than desired for a comprehensive repair.
*Lidocaine mixed with bupivacaine*
- Mixing lidocaine with bupivacaine can provide a **faster onset of action** (due to lidocaine) and a longer duration (due to bupivacaine) as compared to lidocaine alone.
- However, the overall duration would typically still be *shorter* than bupivacaine with epinephrine due to the lack of vasoconstriction from epinephrine, leading to faster systemic absorption.
*Lidocaine with epinephrine*
- Adding **epinephrine** to **lidocaine** prolongs its duration of action by inducing vasoconstriction.
- While this is a practical choice for many procedures, bupivacaine inherently has a longer duration than lidocaine, making *bupivacaine with epinephrine* the longest-acting option among those given.
*Bupivacaine*
- **Bupivacaine** alone provides longer anesthesia than lidocaine alone.
- However, without **epinephrine**, its duration is not as long as it could be, as epinephrine would delay its absorption and prolong its local effect.
Regional anesthesia techniques US Medical PG Question 2: A 34-year-old man presents to the outpatient clinic with a complaint of right-sided jaw pain. The onset of pain was approx. 1 month ago and he is experiencing symptoms 2–3 times a day. Each episode of pain lasts for about 30 seconds. He describes the pain as severe (9 out of 10) with an electric and sharp quality. He denies having tear production or conjunctival injection on the affected side during attacks. What is the mechanism of action for the drug that will best treat this patient’s condition?
- A. Increase the time of Cl- channel opening
- B. Prevention of Na+ influx (Correct Answer)
- C. Decrease the excitatory effects of glutamic acid
- D. Decrease in the Ca2+ influx
- E. Increase the frequency of Cl- channel opening
Regional anesthesia techniques Explanation: ***Prevention of Na+ influx***
- The patient's symptoms (right-sided jaw pain, severe, electric, sharp quality, short duration, triggered by daily activities like chewing/talking) are highly consistent with **trigeminal neuralgia**.
- **Carbamazepine**, a sodium channel blocker, is the first-line treatment for trigeminal neuralgia, and its mechanism of action involves **preventing Na+ influx** in neural membranes, thus stabilizing the excited nerve.
*Increase the time of Cl- channel opening*
- This mechanism is associated with **benzodiazepines**, which act on GABA-A receptors to enhance the inhibitory effects of GABA by **increasing the duration of Cl- channel opening**.
- While benzodiazepines can have anticonvulsant properties, they are not the primary treatment for trigeminal neuralgia because **carbamazepine is more effective** at specifically targeting the hyperexcitability of the trigeminal nerve.
*Decrease the excitatory effects of glutamic acid*
- This mechanism is characteristic of drugs like **memantine** (used in Alzheimer's disease) or some antiglutamatergic agents in epilepsy.
- While glutamatergic overactivity can contribute to pain, **inhibiting glutamate receptors** is not the primary or most effective strategy for the acute symptomatic relief in trigeminal neuralgia.
*Decrease in the Ca2+ influx*
- This mechanism is seen with **calcium channel blockers** like gabapentin and pregabalin, which can be used as second-line treatments for neuropathic pain including trigeminal neuralgia.
- However, **sodium channel blockade** (e.g., carbamazepine) is considered more direct and effective for the high-frequency firing characteristic of trigeminal neuralgia.
*Increase the frequency of Cl- channel opening*
- This mechanism also involves **GABA-A receptor agonists** like benzodiazepines, but specifically some agents might increase the frequency of chloride channel opening rather than duration or both.
- Similar to increasing the time of Cl- channel opening, this mechanism aims to enhance GABAergic inhibition but is **not the primary mechanism of action** for the most effective drug in trigeminal neuralgia.
Regional anesthesia techniques US Medical PG Question 3: A 47-year-old man with alcoholic cirrhosis is brought to the emergency department by ambulance 20 minutes after being involved in a high-speed motor vehicle collision. His pulse is 120/min, respirations are 28/min and labored, and blood pressure is 70/40 mm Hg. Physical examination shows ecchymoses over the trunk and abdomen. In preparation for an exploratory laparotomy, atracurium is administered as an anesthetic. Which of the following characteristics is the most likely reason that this drug was chosen over other drugs in the same class?
- A. Quickest onset of action
- B. Highest potency
- C. Prolonged depolarization
- D. Organ-independent elimination (Correct Answer)
- E. Low risk of bleeding
Regional anesthesia techniques Explanation: ***Organ-independent elimination***
- **Atracurium** is metabolized by **Hofmann elimination** and **ester hydrolysis**, which are independent of renal or hepatic function.
- This is crucial for a patient with **alcoholic cirrhosis** and **hemodynamic instability**, where liver and kidney function may be compromised, preventing drug accumulation.
*Quickest onset of action*
- While a rapid onset is desirable in an emergency, atracurium does not have the **quickest onset of action** among neuromuscular blockers; **succinylcholine** is faster.
- The primary selection criterion here relates to the patient's underlying liver pathology and the drug's elimination profile.
*Highest potency*
- **Potency** refers to the dose required to produce a given effect, and while important, it is not the **most critical factor** in selecting atracurium for this patient.
- The patient's severe medical condition necessitates drug selection based on **metabolic profile** to minimize adverse effects.
*Prolonged depolarization*
- Atracurium is a **non-depolarizing neuromuscular blocker**, meaning it does not cause prolonged depolarization.
- **Succinylcholine** is a depolarizing agent, and its use might be contraindicated or require careful consideration in trauma patients with potential electrolyte imbalances.
*Low risk of bleeding*
- The risk of bleeding is generally not a direct characteristic of **neuromuscular blocking agents** themselves.
- The patient's **cirrhosis** and **trauma** are the primary factors contributing to a high risk of bleeding, which is managed independently of muscle relaxant choice.
Regional anesthesia techniques US Medical PG Question 4: An investigator is studying a local anesthetic that causes increased sympathetic activity. When given intravenously, it causes euphoria and pupillary dilation. Which of the following is the most likely effect of this drug at the synaptic cleft?
- A. Increased release of norepinephrine
- B. Decreased reuptake of norepinephrine (Correct Answer)
- C. Decreased release of acetylcholine
- D. Increased release of serotonin
- E. Decreased breakdown of norepinephrine
Regional anesthesia techniques Explanation: ***Decreased reuptake of norepinephrine***
- This drug causes **euphoria** and **pupillary dilation**, which are classic signs of increased **sympathetic nervous system** activity and **CNS stimulation**, consistent with enhanced **noradrenergic transmission**.
- Decreasing the **reuptake of norepinephrine** would increase its concentration in the **synaptic cleft**, leading to more prolonged activation of **alpha and beta adrenergic receptors**.
*Increased release of norepinephrine*
- While increased release would also elevate **norepinephrine** in the **synaptic cleft**, reuptake inhibition is a more common mechanism for drugs producing similar effects like **cocaine** and **amphetamine-like stimulants**.
- Without specific information, **reuptake inhibition** aligns better with the broad activation of **adrenergic receptors** and central effects described.
*Decreased release of acetylcholine*
- This would primarily affect **cholinergic systems**, and while some interactions exist, it does not directly explain the intense **adrenergic activation**, **euphoria**, and **pupillary dilation** observed.
- **Acetylcholine** primarily mediates **parasympathetic responses** and **skeletal muscle contraction**, not the sympathetic effects seen here.
*Increased release of serotonin*
- Increased **serotonin** release is associated with hallucinogenic effects and mood modulation, but it does not directly lead to the pronounced **pupillary dilation** and widespread **alpha/beta adrenergic receptor activation** described.
- The drug explicitly affects **adrenergic receptors**, making an effect on **norepinephrine** more direct.
*Decreased breakdown of norepinephrine*
- This mechanism, typically involving **MAO inhibitors**, would increase **norepinephrine** levels but is described as activating both **alpha and beta adrenergic receptors**, which points more towards a direct increase in synaptic availability rather than metabolic inhibition.
- While it prolongs the action of **norepinephrine**, the primary mechanism described for such a general stimulant often involves **reuptake inhibition** or **enhanced release**.
Regional anesthesia techniques US Medical PG Question 5: A 25-year-old man presents to the emergency department with a severe pulsatile headache for an hour. He says that he is having palpitations as well. He adds that he has had several episodes of headache in the past which resolved without seeking medical attention. He is a non-smoker and does not drink alcohol. He denies use of any illicit drugs. He looks scared and anxious. His temperature is 37°C (98.6°F), respirations are 25/min, pulse is 107/min, and blood pressure is 221/161 mm Hg. An urgent urinalysis reveals elevated plasma metanephrines. What is the next best step in the management of this patient?
- A. Hydralazine
- B. Amlodipine
- C. Phenoxybenzamine followed by propranolol (Correct Answer)
- D. Propranolol followed by phenoxybenzamine
- E. Emergent surgery
Regional anesthesia techniques Explanation: ***Phenoxybenzamine followed by propranolol***
- This patient presents with symptoms highly suggestive of a **pheochromocytoma crisis**, including **severe headache**, **palpitations**, **hypertension**, **tachycardia**, and **anxiety**, along with elevated **plasma metanephrines**. The initial management for a pheochromocytoma crisis is **alpha-blockade** (e.g., with phenoxybenzamine) to control the severe hypertension, followed by **beta-blockade** (e.g., with propranolol) to manage tachycardia and prevent unopposed alpha-agonist effects.
- Giving a beta-blocker before an alpha-blocker can lead to **unopposed alpha-adrenergic stimulation**, which can cause a life-threatening increase in blood pressure due to vasoconstriction.
*Hydralazine*
- While **hydralazine** is a potent direct vasodilator used for hypertensive emergencies, it is generally **not the first-line treatment for pheochromocytoma** crisis.
- It can cause reflex **tachycardia**, which might be detrimental in a patient with excessive catecholamine release.
*Amlodipine*
- **Amlodipine** is a **calcium channel blocker** that can lower blood pressure.
- However, it is **not the preferred initial agent for the acute hypertensive crisis** associated with pheochromocytoma, which requires specific alpha-blockade.
*Propranolol followed by phenoxybenzamine*
- Administering a **beta-blocker** (propranolol) before an **alpha-blocker** (phenoxybenzamine) in a patient with pheochromocytoma is **contraindicated** and potentially dangerous.
- This sequence could lead to **unopposed alpha-adrenergic stimulation**, resulting in profound **vasoconstriction** and an extreme, life-threatening increase in blood pressure.
*Emergent surgery*
- While surgical removal of the tumor (adrenalectomy) is the **definitive treatment** for pheochromocytoma, it is **not the immediate next step** in a hypertensive crisis.
- The patient needs **pharmacological stabilization** of blood pressure and heart rate first to reduce surgical risks.
Regional anesthesia techniques US Medical PG Question 6: A 26-year-old G1P0 woman at 40 weeks estimated gestational age presents after experiencing labor pains. Pregnancy has been uncomplicated so far. Rupture of membranes occurs, and a transvaginal delivery is performed under epidural anesthesia, and the baby is delivered alive and healthy. The patient voids a few hours after the delivery and complains of mild irritation at the injection site on her back. On the second day, she complains of a severe headache over the back of her head. The headache is associated with pain and stiffness in the neck. Her headache is aggravated by sitting up or standing and relieved by lying down. The pain is relieved slightly by acetaminophen and ibuprofen. The patient is afebrile. Her vital signs include: pulse 100/min, respiratory rate 18/min, and blood pressure 128/84 mm Hg. Which of the following statements is the most accurate regarding this patient’s condition?
- A. A blockage of CSF is the cause of this patient’s headache
- B. An infection is present at the epidural injection site
- C. This patient’s condition can resolve on its own (Correct Answer)
- D. Excessive bed rest will worsen this patient’s condition
- E. Immediate intervention is required
Regional anesthesia techniques Explanation: ***This patient’s condition can resolve on its own***
- The symptoms describe a **post-dural puncture headache (PDPH)**, a common complication of epidural anesthesia, which is often **self-limiting** within days to weeks.
- Initial management involves conservative measures like bed rest, hydration, and analgesics, as many cases resolve without specific interventions.
*A blockage of CSF is the cause of this patient’s headache*
- PDPH is caused by a **leakage of cerebrospinal fluid (CSF)** through the dura mater, leading to **intracranial hypotension**, not a blockage of CSF flow.
- The leakage reduces CSF pressure, causing the brain to sag when upright, stretching pain-sensitive structures like meninges and blood vessels.
*An infection is present at the site of epidural injection site*
- While localized irritation is mentioned, there are no signs of infection such as **fever**, **erythema**, or **purulent discharge** at the injection site, making infection less likely.
- The headache characteristics (positional, severe, neck stiffness) are classic for PDPH, not typically seen in local epidural infections, which would also present with systemic signs.
*Excessive bed rest will worsen this patient’s condition*
- **Bed rest** typically **improves** the symptoms of PDPH by reducing the gravitational pull on the intracranial structures, thereby alleviating the headache.
- Prolonged bed rest is generally recommended in the acute phase, often combined with hydration and caffeine, to help manage symptoms, not worsen them.
*Immediate intervention is required*
- While severe PDPH can be debilitating, immediate invasive intervention (like an **epidural blood patch**) is usually reserved for cases that are **severe and refractory to conservative management** after 24-48 hours.
- Many patients experience spontaneous resolution or significant improvement with conservative measures, making immediate invasive intervention typically unnecessary.
Regional anesthesia techniques US Medical PG Question 7: A 21-year-old G1P0 woman presents to the labor and delivery ward at 39 weeks gestation for elective induction of labor. She requests a labor epidural. An epidural catheter is secured at the L4-L5 space. She exhibits no hemodynamic reaction to lidocaine 1.5% with epinephrine 1:200,000. A continuous infusion of bupivacaine 0.0625% is started. After 5 minutes, the nurse informs the anesthesiologist that the patient is hypotensive to 80/50 mmHg with a heart rate increase from 90 bpm to 120 bpm. The patient is asymptomatic and fetal heart rate has not changed significantly from baseline. She says that her legs feel heavy but is still able to move them. What is the most likely cause of the hemodynamic change?
- A. Local anesthetic systemic toxicity
- B. Intrathecal infiltration of local anesthetic
- C. Sympathetic blockade (Correct Answer)
- D. Bainbridge reflex
- E. Spinal anesthesia
Regional anesthesia techniques Explanation: ***Sympathetic blockade***
- **Epidural anesthesia** blocks the **sympathetic nerves**, leading to **vasodilation** and decreased venous return, which results in hypotension and a compensatory tachycardia.
- The patient's symptoms of **hypotension** (80/50 mmHg) and **tachycardia** (120 bpm) following epidural initiation are classic signs of sympathetic blockade.
*Local anesthetic systemic toxicity*
- This condition presents with central nervous system symptoms such as **perioral numbness**, **tinnitus**, **seizures**, or **cardiovascular collapse** (severe arrhythmias, asystole), none of which are described.
- The patient is **asymptomatic** apart from the hemodynamic changes, and her ability to move her legs makes systemic toxicity less likely.
*Intrathecal infiltration of local anesthetic*
- This would cause a rapid onset of a **dense motor and sensory block** with profound hypotension and bradycardia, often within seconds to a few minutes.
- The patient's ability to move her legs and the gradual onset over 5 minutes with only "heavy" legs makes a full intrathecal spread unlikely.
*Bainbridge reflex*
- The Bainbridge reflex occurs with an **increase in central venous pressure**, leading to an increase in heart rate.
- In this case, the patient is experiencing **hypotension**, indicating decreased venous return rather than increased, making this reflex an unlikely cause.
*Spinal anesthesia*
- While spinal anesthesia also causes **sympathetic blockade** and hypotension, it typically results in a **rapid onset** (within minutes) of a **dense motor and sensory block** with inability to move the legs.
- The patient's ability to still move her legs and the more gradual presentation are not typical of a full spinal block.
Regional anesthesia techniques US Medical PG Question 8: A 65-year-old woman is transferred to the intensive care unit after she underwent coronary stenting for a posterior-inferior STEMI. She is known to have allergies to amiodarone and captopril. A few hours after the transfer, she suddenly loses consciousness. The monitor shows ventricular fibrillation. CPR is initiated. After 3 consecutive shocks with a defibrillator, the monitor shows ventricular fibrillation. Which of the following medications should be administered next?
- A. Adrenaline and lidocaine (Correct Answer)
- B. Lidocaine and sotalol
- C. Adrenaline and verapamil
- D. Adrenaline and amiodarone
- E. Amiodarone and lidocaine
Regional anesthesia techniques Explanation: ***Adrenaline and lidocaine***
- **Adrenaline (epinephrine)** is the standard vasopressor in ACLS for cardiac arrest, given at 1 mg IV/IO every 3-5 minutes to increase coronary and cerebral perfusion pressures, improving the chances of return of spontaneous circulation (ROSC).
- **Lidocaine** is the recommended alternative antiarrhythmic for refractory ventricular fibrillation when **amiodarone is contraindicated** (as in this patient with documented amiodarone allergy).
- Per **ACLS guidelines**, after failed defibrillation attempts, continue CPR, administer epinephrine, and give an antiarrhythmic agent (lidocaine 1-1.5 mg/kg when amiodarone cannot be used).
*Lidocaine and sotalol*
- **Lidocaine** is appropriate as an antiarrhythmic in refractory VF when amiodarone is contraindicated.
- However, this option omits **epinephrine (adrenaline)**, which is a critical vasopressor required during cardiac arrest per ACLS protocols.
- **Sotalol** is a beta-blocker with Class III antiarrhythmic properties, but it is not recommended for acute management of refractory VF in cardiac arrest.
*Adrenaline and verapamil*
- **Adrenaline** is indicated as the vasopressor for cardiac arrest.
- **Verapamil** is a calcium channel blocker used for supraventricular arrhythmias; it is **contraindicated in ventricular fibrillation** due to negative inotropic effects and peripheral vasodilation that can worsen hemodynamic collapse during cardiac arrest.
*Adrenaline and amiodarone*
- While **adrenaline** is indicated and **amiodarone** would typically be the preferred antiarrhythmic for refractory VF, this patient has a **documented allergy to amiodarone**, making it contraindicated.
- Lidocaine must be used as the alternative antiarrhythmic agent.
*Amiodarone and lidocaine*
- **Lidocaine** is appropriate in this scenario.
- However, **amiodarone is contraindicated** due to the patient's known allergy.
- This combination would be dangerous and violates basic principles of avoiding known allergens.
Regional anesthesia techniques US Medical PG Question 9: A 42-year-old man presents to his family physician for evaluation of oral pain. He states that he has increasing pain in a molar on the top left of his mouth. The pain started 1 week ago and has been progressively worsening since then. His medical history is significant for hypertension and type 2 diabetes mellitus, both of which are currently controlled with lifestyle modifications. His blood pressure is 124/86 mm Hg, heart rate is 86/min, and respiratory rate is 14/min. Physical examination is notable for a yellow-black discoloration of the second molar on his left upper mouth. The decision is made to refer him to a dentist for further management of this cavity. The patient has never had any dental procedures and is nervous about what type of sedation will be used. Which of the following forms of anesthesia utilizes solely an oral or intravenous anti-anxiety medication?
- A. Minimal Sedation (Correct Answer)
- B. Dissociation
- C. Regional anesthesia
- D. Epidural anesthesia
- E. Deep sedation
Regional anesthesia techniques Explanation: ***Minimal Sedation***
- This involves using **oral** or **intravenous anti-anxiety medications** to help a patient relax while remaining conscious and responsive.
- The patient can still respond to verbal commands but is in a state of decreased anxiety and awareness.
*Dissociation*
- This is a state induced by certain drugs, like **ketamine**, where the patient feels detached from their body and environment.
- While it can be achieved intravenously, it is not solely an anti-anxiety medication effect and involves a different neurological state.
*Regional anesthesia*
- This involves injecting a **local anesthetic** near nerves to numb a specific part of the body, such as a limb or a jaw section for dental procedures.
- It primarily provides pain relief by blocking nerve signals and does not typically involve anti-anxiety medication as its sole component for sedation.
*Epidural anesthesia*
- This form of regional anesthesia involves injecting a **local anesthetic** into the **epidural space** surrounding the spinal cord to block pain signals.
- It is used for pain control during surgery or childbirth and does not involve oral or intravenous anti-anxiety medication as the primary method of sedation.
*Deep sedation*
- This involves a more profound depression of consciousness than minimal sedation, where the patient may be difficult to arouse but still responds purposefully to repeated or painful stimulation.
- While it can use intravenous medications, it typically involves a combination of sedatives and analgesics to achieve a deeper state of unresponsiveness, beyond just anti-anxiety medication.
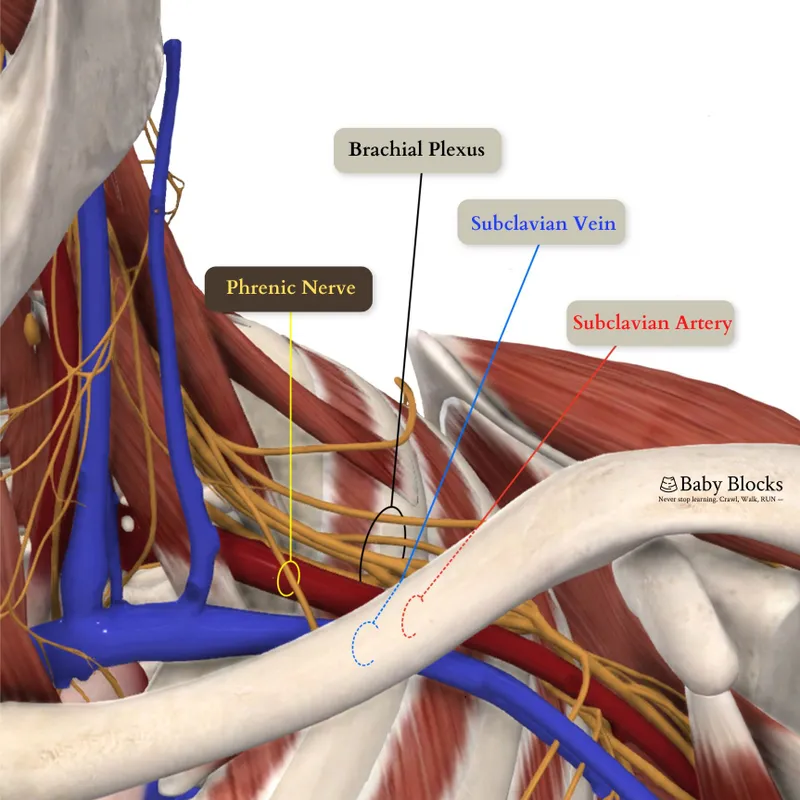
Regional anesthesia techniques US Medical PG Question 10: A 28-year-old man comes to the emergency department for an injury sustained while doing construction. Physical examination shows a long, deep, irregular laceration on the lateral aspect of the left forearm with exposed fascia. Prior to surgical repair of the injury, a brachial plexus block is performed using a local anesthetic. Shortly after the nerve block is performed, he complains of dizziness and then loses consciousness. His radial pulse is faint and a continuous cardiac monitor shows a heart rate of 24/min. Which of the following is the most likely mechanism of action of the anesthetic that was administered?
- A. Activation of acetylcholine receptors
- B. Inactivation of ryanodine receptors
- C. Inactivation of sodium channels (Correct Answer)
- D. Activation of GABA receptors
- E. Inactivation of potassium channels
Regional anesthesia techniques Explanation: ***Inactivation of sodium channels***
- Local anesthetics primarily work by reversibly blocking **voltage-gated sodium channels** in nerves.
- This prevents the influx of sodium ions, inhibiting the generation and propagation of **action potentials**, thus blocking pain signals.
- The clinical presentation of dizziness, loss of consciousness, and bradycardia represents systemic toxicity from intravascular absorption of the local anesthetic.
*Activation of acetylcholine receptors*
- Activation of **nicotinic or muscarinic acetylcholine receptors** is the primary mechanism of action for neuromuscular stimulants or parasympathomimetics, not local anesthetics.
- This would typically lead to muscle contraction or increased parasympathetic activity rather than analgesia and local nerve block.
*Inactivation of ryanodine receptors*
- Inactivation of **ryanodine receptors** primarily affects calcium release from the sarcoplasmic reticulum in muscle cells, crucial for excitation-contraction coupling.
- This mechanism is associated with drugs like dantrolene used for malignant hyperthermia, not local anesthetics.
*Activation of GABA receptors*
- Activation of **GABA-A receptors** is the primary mechanism of action for benzodiazepines and barbiturates, leading to widespread CNS depression and sedation.
- While systemic absorption of local anesthetics can cause CNS effects (as seen in toxicity), their primary therapeutic mechanism for nerve block is sodium channel inactivation, not GABA receptor activation.
*Inactivation of potassium channels*
- Inactivation of **potassium channels** would typically prolong repolarization and increase neuronal excitability or cause arrhythmias, depending on the specific channel.
- This is not the mechanism of action for local anesthetics, which prevent depolarization by blocking sodium channel activation.
More Regional anesthesia techniques US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.
 ⚠️ Bupivacaine has high cardiotoxicity.
⚠️ Bupivacaine has high cardiotoxicity.
