Postoperative anesthesia complications US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Postoperative anesthesia complications. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Postoperative anesthesia complications US Medical PG Question 1: A 56-year-old previously healthy woman with no other past medical history is post-operative day one from an open reduction and internal fixation of a fractured right radius and ulna after a motor vehicle accident. What is one of the primary ways of preventing postoperative pneumonia in this patient?
- A. Shallow breathing exercises
- B. Incentive spirometry (Correct Answer)
- C. Outpatient oral antibiotics
- D. Hyperbaric oxygenation
- E. In-hospital intravenous antibiotics
Postoperative anesthesia complications Explanation: ***Incentive spirometry***
- **Incentive spirometry** is a cornerstone of postoperative care, actively encouraging patients to take slow, deep breaths. This expands the lungs and prevents the collapse of alveoli, reducing the risk of **atelectasis** and subsequent **pneumonia**.
- Its effectiveness lies in promoting lung aeration and clearing secretions, which are crucial after anesthesia and surgery, especially in patients with reduced mobility or pain.
*Shallow breathing exercises*
- **Shallow breathing** is insufficient for adequate lung expansion and can actually contribute to **atelectasis** and the pooling of secretions in the lungs.
- Effective pulmonary hygiene requires **deep breaths** to maximize alveolar recruitment and prevent respiratory complications.
*Outpatient oral antibiotics*
- **Prophylactic antibiotics** are typically given around the time of surgery to prevent surgical site infections, not primarily to prevent postoperative pneumonia in an outpatient setting.
- Administering antibiotics without a diagnosed infection can lead to **antibiotic resistance** and is not a standard practice for preventing pneumonia unless a specific risk factor or existing infection is identified.
*Hyperbaric oxygenation*
- **Hyperbaric oxygenation** involves breathing 100% oxygen in a pressurized chamber and is used for conditions like **decompression sickness**, non-healing wounds, or severe infections.
- It is not a standard or primary method for preventing postoperative pneumonia, as its mechanism of action is unrelated to common pulmonary hygiene techniques.
*In-hospital intravenous antibiotics*
- While antibiotics can treat pneumonia, their routine, **prophylactic use** intravenously in-hospital solely for preventing postoperative pneumonia is generally unwarranted and can contribute to **antibiotic resistance**.
- Antibiotics are indicated if there is evidence of an active infection, but the primary prevention of pneumonia focuses on mechanical lung expansion and airway clearance.
Postoperative anesthesia complications US Medical PG Question 2: A man is brought into the emergency department by police. The patient was found somnolent in the park and did not respond to questioning. The patient's past medical history is unknown, and he is poorly kempt. The patient's personal belongings include prescription medications and illicit substances such as alprazolam, diazepam, marijuana, cocaine, alcohol, acetaminophen, and a baggie containing an unknown powder. His temperature is 97.0°F (36.1°C), blood pressure is 117/58 mmHg, pulse is 80/min, respirations are 9/min, and oxygen saturation is 91% on room air. Physical exam reveals pupils that do not respond to light bilaterally, and a somnolent patient who only withdraws his limbs to pain. Which of the following is the best next step in management?
- A. N-acetylcysteine
- B. Supportive therapy, thiamine, and dextrose
- C. Naloxone (Correct Answer)
- D. Intubation
- E. Flumazenil
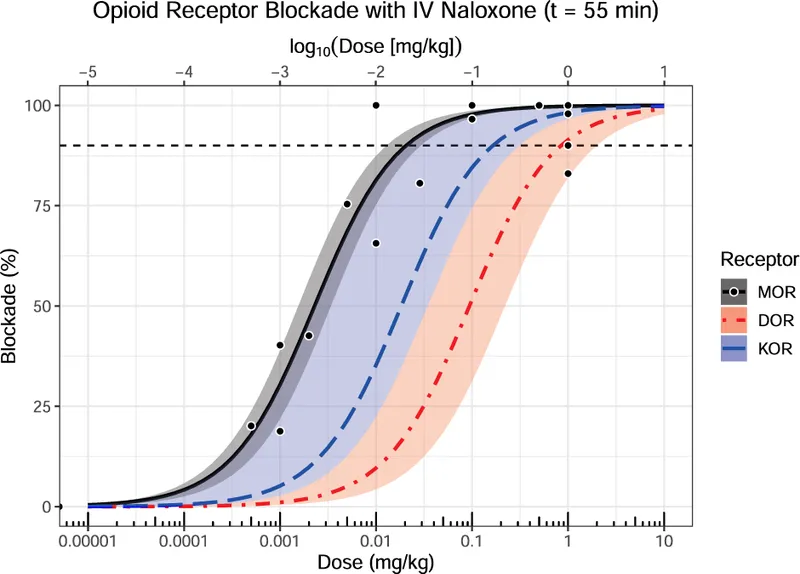
Postoperative anesthesia complications Explanation: ***Naloxone***
- The patient exhibits classic signs of **opioid overdose** including **respiratory depression** (bradypnea, SpO2 91%), **miosis** (though noted as non-reactive, pinpoint pupils are common in opioid overdose), and altered mental status (somnolence, withdrawal to pain).
- Naloxone is an **opioid antagonist** that can rapidly reverse these effects and is indicated in suspected opioid overdose to improve breathing and consciousness.
*N-acetylcysteine*
- This is the antidote for **acetaminophen overdose**, which is possible given the presence of acetaminophen among the patient's belongings.
- However, the patient's acute symptoms of **severe respiratory and CNS depression** are not typical of acute acetaminophen toxicity and require more immediate intervention.
*Supportive therapy, thiamine, and dextrose*
- **Supportive therapy** (e.g., airway management) is crucial, and **thiamine and dextrose** are often given empirically to patients with altered mental status to address potential **Wernicke's encephalopathy** or **hypoglycemia**.
- While important general measures, these do not specifically target the immediate life-threatening respiratory depression and CNS depression so highly suggestive of opioid overdose.
*Intubation*
- While the patient has respiratory depression, **intubation** is an invasive procedure and should be considered if naloxone fails to improve respiratory status or if persistent airway compromise exists.
- The first step in suspected opioid overdose is typically to administer naloxone, as it may avoid the need for intubation.
*Flumazenil*
- **Flumazenil** is an antagonist for **benzodiazepine overdose**, and alprazolam and diazepam were found in the patient's possession.
- However, flumazenil can precipitate **withdrawal seizures** in chronic benzodiazepine users and is generally avoided in undifferentiated comatose patients, especially when mixed ingestions are suspected.
Postoperative anesthesia complications US Medical PG Question 3: A 25-year-old man is brought to the emergency department after his girlfriend discovered him at home in a minimally responsive state. He has a history of drinking alcohol excessively and using illicit drugs. On arrival, he does not respond to commands but withdraws all extremities to pain. His pulse is 90/min, respirations are 8/min, and blood pressure is 130/90 mm Hg. Pulse oximetry while receiving bag-valve-mask ventilation shows an oxygen saturation of 95%. Examination shows cool, dry skin, with scattered track marks on his arms and legs. The pupils are pinpoint and react sluggishly to light. His serum blood glucose level is 80 mg/dL. The most appropriate next step in management is intravenous administration of which of the following?
- A. Fomepizole
- B. Naltrexone
- C. Methadone
- D. Naloxone (Correct Answer)
- E. Phentolamine
Postoperative anesthesia complications Explanation: ***Naloxone***
- The patient presents with classic signs of **opioid overdose**: altered mental status, **respiratory depression** (8/min), and **pinpoint pupils**.
- **Naloxone** is an opioid antagonist that rapidly reverses the effects of opioid toxicity and is the most appropriate first-line treatment in this scenario.
*Fomepizole*
- This medication is used as an antidote for **methanol** and **ethylene glycol poisoning**, which typically present with metabolic acidosis and renal failure, not pinpoint pupils and respiratory depression.
- There are no clinical signs in this patient indicative of methanol or ethylene glycol ingestion.
*Naltrexone*
- **Naltrexone** is an opioid antagonist used for long-term management of opioid use disorder or alcohol dependence, but it is not used in acute overdose resuscitation due to its slower onset and formulation (oral or long-acting injectable).
- Its primary role is to prevent relapse, not to reverse acute respiratory depression.
*Methadone*
- **Methadone** is a long-acting opioid agonist used for opioid replacement therapy and chronic pain management.
- Administering methadone would worsen the patient's opioid-induced respiratory depression and central nervous system depression.
*Phentolamine*
- **Phentolamine** is an alpha-adrenergic blocker used to treat hypertensive crises, particularly those caused by pheochromocytoma or extravasation of vasopressors.
- It has no role in managing opioid overdose and could lead to hypotension in this patient.
Postoperative anesthesia complications US Medical PG Question 4: A 68-year-old woman presents to the hospital for an elective right hemicolectomy. She is independently mobile and does her own shopping. She has had type 2 diabetes mellitus for 20 years, essential hypertension for 15 years, and angina on exertion for 6 years. She has a 30-pack-year history of smoking. The operation was uncomplicated. On post-op day 5, she becomes confused. She has a temperature of 38.5°C (101.3°F), respiratory rate of 28/min, and oxygen saturation of 92% on 2 L of oxygen. She is tachycardic at 118/min and her blood pressure is 110/65 mm Hg. On chest auscultation, she has coarse crackles in the right lung base. Her surgical wound appears to be healing well, and her abdomen is soft and nontender. Which of the following is the most likely diagnosis?
- A. Malignant hyperthermia
- B. Drug-induced fever
- C. Multiple organ dysfunction syndrome
- D. Sepsis (Correct Answer)
- E. Non-infectious systemic inflammatory response syndrome (SIRS)
Postoperative anesthesia complications Explanation: ***Sepsis***
- The patient exhibits several signs of **systemic inflammatory response syndrome (SIRS)** (fever, tachycardia, tachypnea) coupled with evidence of infection (coarse crackles in the lung base suggests **pneumonia**).
- The combination of **SIRS criteria** and a likely infection source in a postoperative patient strongly points to sepsis, a life-threatening organ dysfunction caused by a dysregulated host response to infection.
*Malignant hyperthermia*
- This is a rare, life-threatening condition typically triggered by **volatile anesthetic agents** or **succinylcholine** during surgery.
- It usually presents **intraoperatively or immediately postoperatively** with rapid onset of hyperthermia, muscle rigidity, and metabolic acidosis, which is not consistent with a presentation on post-op day 5.
*Drug-induced fever*
- While drug-induced fever is possible, particularly in polymedicated patients, it would be a **diagnosis of exclusion** when other more likely causes of fever, such as infection, are present.
- There are no specific clinical features in this case that strongly suggest a drug as the singular cause of fever and the systemic inflammatory response.
*Multiple organ dysfunction syndrome*
- **MODS** is the progressive failure of two or more organ systems and is often a **complication of severe sepsis or septic shock**, rather than an initial diagnosis.
- While the patient is unwell, her current presentation describes a potential precursor (sepsis) rather than established multi-organ dysfunction.
*Non-infectious systemic inflammatory response syndrome (SIRS)*
- SIRS caused by non-infectious etiologies (e.g., pancreatitis, trauma, burns) can occur, but the presence of **localized lung crackles** and a **postoperative fever** makes an infectious etiology much more likely.
- Postoperative SIRS can occur due to surgical stress, but the signs of infection (especially respiratory) shift the diagnosis towards sepsis.
Postoperative anesthesia complications US Medical PG Question 5: Two hours after undergoing elective cholecystectomy with general anesthesia, a 41-year-old woman is evaluated for decreased mental status. BMI is 36.6 kg/m2. Respirations are 18/min and blood pressure is 126/73 mm Hg. Physical examination shows the endotracheal tube in normal position. She does not respond to sternal rub and gag reflex is absent. Arterial blood gas analysis on room air shows normal PO2 and PCO2 levels. Which of the following anesthetic properties is the most likely cause of these findings?
- A. Low blood solubility
- B. High lipid solubility (Correct Answer)
- C. Low brain-blood partition coefficient
- D. High minimal alveolar concentration
- E. Low cytochrome P450 activity
Postoperative anesthesia complications Explanation: ***High lipid solubility***
- Anesthetics with **high lipid solubility** accumulate in **adipose tissue** and are slowly released, prolonging their effect, especially in obese patients.
- The patient's **obesity (BMI 36.6 kg/m2)** contributes to a larger reservoir for lipid-soluble drugs, leading to delayed recovery and decreased mental status.
*Low blood solubility*
- **Low blood solubility** implies a rapid equilibrium between the lungs and the blood, leading to a **faster onset and offset** of anesthetic action.
- This property would result in a quicker recovery from anesthesia, which contradicts the patient's prolonged unconsciousness.
*Low brain-blood partition coefficient*
- A **low brain-blood partition coefficient** means the anesthetic does not accumulate significantly in brain tissue relative to blood.
- Agents with this property equilibrate quickly and leave the brain rapidly upon discontinuation, resulting in **fast recovery**, which is inconsistent with the patient's persistent decreased mental status.
*High minimal alveolar concentration*
- **High minimal alveolar concentration (MAC)** means that a higher concentration of the anesthetic gas is required to produce immobility in 50% of patients.
- A high MAC describes the **potency** of an anesthetic and does not directly explain prolonged recovery or decreased mental status in an obese patient, but rather indicates that a larger dose or concentration was needed to achieve anesthesia.
*Low cytochrome P450 activity*
- **Low cytochrome P450 activity** would lead to slower metabolism of drugs that are primarily cleared by this system, potentially prolonging their effects.
- While relevant for some drugs, the primary issue for inhaled anesthetics is their **physical distribution and elimination**, not typically metabolic clearance via Cytochrome P450 enzymes.
Postoperative anesthesia complications US Medical PG Question 6: Three days after undergoing laparoscopic colectomy, a 67-year-old man reports swelling and pain in his right leg. He was diagnosed with colon cancer 1 month ago. His temperature is 38.5°C (101.3°F). Physical examination shows swelling of the right leg from the ankle to the thigh. There is no erythema or rash. Which of the following is likely to be most helpful in establishing the diagnosis?
- A. D-dimer level
- B. Compression ultrasonography (Correct Answer)
- C. CT pulmonary angiography
- D. Transthoracic echocardiography
- E. Blood cultures
Postoperative anesthesia complications Explanation: ***Compression ultrasonography***
- This patient's presentation with **unilateral leg swelling and pain** after surgery, especially given his recent **colon cancer diagnosis** (a hypercoagulable state), is highly suspicious for a **deep vein thrombosis (DVT)**.
- **Compression ultrasonography** is the gold standard, non-invasive imaging modality for diagnosing DVT, allowing direct visualization of thrombi and assessing venous compressibility.
*D-dimer level*
- While a **positive D-dimer** indicates recent or ongoing clot formation, it is **non-specific** and can be elevated in many conditions, including surgery, cancer, and infection.
- A normal D-dimer can rule out DVT in low-probability patients, but a high D-dimer in a high-probability patient (like this case) requires further imaging for confirmation, making it less definitive than ultrasound.
*CT pulmonary angiography*
- This imaging is used to diagnose a **pulmonary embolism (PE)**, which is a complication of DVT, but the primary symptoms here are localized to the leg.
- While PE is a concern, diagnosing the source (DVT) in the leg is the immediate priority for treatment and prevention of future complications.
*Transthoracic echocardiography*
- **Echocardiography** evaluates cardiac structure and function and can sometimes detect large clots in the right heart leading to PE, but it is not the primary diagnostic tool for DVT in the leg.
- It would be done if signs of cardiac strain or shunting associated with acute PE were prominent, which is not the case here.
*Blood cultures*
- **Blood cultures** are used to diagnose **bacteremia or sepsis**, which might explain a fever, but the prominent, unilateral leg swelling and pain are not typical for a primary infectious cause in the leg without local signs of cellulitis or abscess.
- While a low-grade fever is present, the absence of erythema or rash makes a primary infectious etiology less likely than DVT given the risk factors.
Postoperative anesthesia complications US Medical PG Question 7: A 37-year-old-woman presents to the emergency room with complaints of fever and abdominal pain. Her blood pressure is 130/74 mmHg, pulse is 98/min, temperature is 101.5°F (38.6°C), and respirations are 23/min. The patient reports that she had a laparoscopic cholecystectomy 4 days ago but has otherwise been healthy. She is visiting her family from Nebraska and just arrived this morning from a 12-hour drive. Physical examination revealed erythema and white discharge from abdominal incisions and tenderness upon palpations at the right upper quadrant. What is the most probable cause of the patient’s fever?
- A. Pulmonary atelectasis
- B. Residual gallstones
- C. Urinary tract infection
- D. Wound infection (Correct Answer)
- E. Pulmonary embolism
Postoperative anesthesia complications Explanation: ***Wound infection***
- The presence of **erythema**, **white discharge from abdominal incisions**, and **fever** 4 days post-laparoscopic cholecystectomy strongly indicates a surgical site infection.
- This is a common complication after surgery, especially with visible signs of local inflammation and purulent discharge.
*Pulmonary atelectasis*
- **Atelectasis** typically presents within **24-48 hours post-op** and usually resolves spontaneously.
- While it can cause fever, the prominent local wound signs and the timing (4 days post-op) make it less likely to be the primary cause of fever.
*Residual gallstones*
- **Residual gallstones** would typically present with symptoms resembling acute cholecystitis or cholangitis, such as **right upper quadrant pain**, **jaundice**, or **elevated liver enzymes**, without direct signs of wound infection.
- These do not account for the **erythema and discharge from the incision sites**.
*Urinary tract infection*
- A **urinary tract infection (UTI)** would present with **dysuria**, **frequency**, **urgency**, or **suprapubic pain**, and would not explain the local wound findings.
- While surgery can increase the risk of nosocomial UTIs, the clinical presentation is primarily focused on the surgical site.
*Pulmonary embolism*
- A **pulmonary embolism (PE)** would likely cause **dyspnea**, **tachycardia**, **hypoxia**, and **pleuritic chest pain**, which are not reported in this case.
- Though prolonged immobility (e.g., long drive) is a risk factor, the specific local signs of infection are not consistent with PE.
Postoperative anesthesia complications US Medical PG Question 8: Three days after undergoing an open cholecystectomy, a 73-year-old man has fever and abdominal pain. He has hypertension, type 2 diabetes mellitus, chronic obstructive pulmonary disease, and benign prostatic hyperplasia. He had smoked one pack of cigarettes daily for 40 years but quit 1 year ago. He does not drink alcohol. Prior to admission to the hospital, his medications included lisinopril, metformin, ipratropium, and tamsulosin. He appears acutely ill and lethargic. His temperature is 39.5°C (103.1°F), pulse is 108/min, respirations are 18/min, and blood pressure is 110/84 mm Hg. He is oriented only to person. Examination shows a 10-cm subcostal incision that appears dry and non-erythematous. Scattered expiratory wheezing is heard throughout both lung fields. His abdomen is distended with tenderness to palpation over the lower quadrants. Laboratory studies show:
Hemoglobin 10.1 g/dl
Leukocyte count 19,000/mm3
Serum
Glucose 180 mg/dl
Urea Nitrogen 25 mg/dl
Creatinine 1.2 mg/dl
Lactic acid 2.5 mEq/L (N = 0.5 - 2.2 mEq/L)
Urine
Protein 1+
RBC 1–2/hpf
WBC 32–38/hpf
Which of the following is the most likely underlying mechanism of this patient's current condition?
- A. Wound contamination
- B. Peritoneal inflammation
- C. Impaired alveolar ventilation
- D. Intraabdominal abscess formation (Correct Answer)
- E. Bladder outlet obstruction
Postoperative anesthesia complications Explanation: ***Intraabdominal abscess formation***
- The patient presents with **fever**, **leukocytosis**, **abdominal pain** and **distension** three days post-cholecystectomy. These symptoms, coupled with signs of systemic illness (lethargy, altered mental status, tachycardia, elevated lactic acid), are highly suggestive of an **intraabdominal infection** such as an abscess.
- The surgical site incision appears dry and non-erythematous, making a superficial wound infection less likely to explain the systemic symptoms and deep abdominal pain.
*Wound contamination*
- While wound contamination can cause infection, the incision site is described as **dry and non-erythematous**, suggesting that a superficial surgical site infection is not the primary cause of the patient's systemic illness and deep abdominal pain.
- A simple wound infection generally would not lead to such significant systemic symptoms, including **lethargy** and **altered mental status**, within three days post-surgery, especially without local signs of inflammation.
*Peritoneal inflammation*
- Peritoneal inflammation (peritonitis) is a consequence of an intraabdominal process like an abscess or anastomotic leak, rather than the primary underlying mechanism itself.
- The symptoms of **localized tenderness** and **distension** are more indicative of a contained process like an abscess rather than diffuse peritoneal inflammation as the initial cause.
*Impaired alveolar ventilation*
- While the patient has COPD and scattered expiratory wheezing, suggesting some degree of respiratory compromise, **impaired alveolar ventilation** alone does not explain the fever, elevated leukocyte count, abdominal pain, and an elevated lactic acid (though respiratory distress can contribute to lactic acidemia, an infection is a more direct cause here).
- Post-operative pulmonary complications are common, but the abdominal findings and systemic signs of infection point away from a purely respiratory origin for this acute deterioration.
*Bladder outlet obstruction*
- The patient has BPH and is on tamsulosin, but his current symptoms of fever, leukocytosis, abdominal pain, and elevated lactic acid are not typical for **bladder outlet obstruction**.
- Although the urine analysis shows pyuria (WBC 32-38/hpf), which could suggest a urinary tract infection (UTI), a UTI alone is less likely to cause this degree of systemic illness with **significant abdominal distension** and **tenderness** in the lower quadrants shortly after abdominal surgery; it's more probable that the pyuria is a secondary finding or contributing factor in a patient with a more severe intraabdominal process.
Postoperative anesthesia complications US Medical PG Question 9: Three days after undergoing coronary artery bypass surgery, a 72-year-old man has severe right upper quadrant pain, fever, nausea, and vomiting. He has type 2 diabetes mellitus, benign prostatic hyperplasia, peripheral vascular disease, and chronic mesenteric ischemia. He had smoked one pack of cigarettes daily for 30 years but quit 10 years ago. He drinks 8 cans of beer a week. His preoperative medications include metformin, aspirin, simvastatin, and finasteride. His temperature is 38.9°C (102°F), pulse is 102/min, respirations are 18/min, and blood pressure is 110/60 mmHg. Auscultation of the lungs shows bilateral inspiratory crackles. Cardiac examination shows no murmurs, rubs or gallops. Abdominal examination shows soft abdomen with tenderness and sudden inspiratory arrest upon palpation in the right upper quadrant. There is no rebound tenderness or guarding. Laboratory studies show the following:
Hemoglobin 13.1 g/dL
Hematocrit 42%
Leukocyte count 15,700/mm3
Segmented neutrophils 65%
Bands 10%
Lymphocytes 20%
Monocytes 3%
Eosinophils 1%
Basophils 0.5%
AST 40 U/L
ALT 100 U/L
Alkaline phosphatase 85 U/L
Total bilirubin 1.5 mg/dL
Direct 0.9 mg/dL
Amylase 90 U/L
Abdominal ultrasonography shows a distended gallbladder, thickened gallbladder wall with pericholecystic fluid, and no stones. Which of the following is the most appropriate next step in management?
- A. Intravenous heparin therapy followed by embolectomy
- B. Careful observation with serial abdominal examinations
- C. Endoscopic retrograde cholangiopancreatography with papillotomy
- D. Intravenous piperacillin-tazobactam therapy and percutaneous cholecystostomy (Correct Answer)
- E. Immediate cholecystectomy
Postoperative anesthesia complications Explanation: ***Intravenous piperacillin-tazobactam therapy and percutaneous cholecystostomy***
- The patient presents with **acalculous cholecystitis**, characterized by severe RUQ pain, fever, leukocytosis, elevated transaminases, and ultrasonographic findings of a distended gallbladder with a thickened wall and pericholecystic fluid, but no stones.
- Given his comorbid conditions (diabetes, PVD, recent CABG) and the severity of his illness, empirical **broad-spectrum antibiotics** (like piperacillin-tazobactam) along with image-guided **percutaneous cholecystostomy** for gallbladder decompression are the most appropriate management, avoiding the high risks of immediate surgery.
*Intravenous heparin therapy followed by embolectomy*
- This approach is indicated for **acute mesenteric ischemia with embolism**, which can present with severe abdominal pain and signs of hypoperfusion.
- While the patient has chronic mesenteric ischemia, his current symptoms and imaging findings are more consistent with cholecystitis, and there is no clear evidence of acute embolic event requiring embolectomy.
*Careful observation with serial abdominal examinations*
- This patient exhibits signs of a severe inflammatory process (fever, leukocytosis, RUQ tenderness, elevated LFTs, and sonographic findings of severe inflammation) and systemic illness, making **conservative observation insufficient** and potentially dangerous.
- **Acalculous cholecystitis** is a serious condition with a high risk of complications like perforation and sepsis, especially in critically ill patients, and requires prompt intervention.
*Endoscopic retrograde cholangiopancreatography with papillotomy*
- **ERCP with papillotomy** is indicated for conditions like **choledocholithiasis** (common bile duct stones) or **cholangitis**, which cause biliary obstruction.
- The ultrasound shows **no stones** and features specific to cholecystitis rather than common bile duct obstruction, making ERCP inappropriate as an initial step.
*Immediate cholecystectomy*
- While cholecystectomy is the definitive treatment for cholecystitis, immediate open or laparoscopic cholecystectomy in a critically ill patient with **acalculous cholecystitis** after recent CABG carries a **very high morbidity and mortality risk**.
- **Percutaneous cholecystostomy** offers a safer, less invasive alternative for source control and stabilizes the patient before potential delayed definitive surgery if needed, once the patient's condition improves.
Postoperative anesthesia complications US Medical PG Question 10: Two hours after undergoing a left femoral artery embolectomy, an obese 63-year-old woman has severe pain, numbness, and tingling of the left leg. The surgery was without complication and peripheral pulses were weakly palpable postprocedure. She has type 2 diabetes mellitus, peripheral artery disease, hypertension, and hypercholesterolemia. Prior to admission, her medications included insulin, enalapril, carvedilol, aspirin, and rosuvastatin. She appears uncomfortable. Her temperature is 37.1°C (99.3°F), pulse is 98/min, and blood pressure is 132/90 mm Hg. Examination shows a left groin surgical incision. The left lower extremity is swollen, stiff, and tender on palpation. Dorsiflexion of her left foot causes severe pain in her calf. Femoral pulses are palpated bilaterally. Pedal pulses are weaker on the left side as compared to the right side. Laboratory studies show:
Hemoglobin 12.1
Leukocyte count 11,300/mm3
Platelet count 189,000/mm3
Serum
Glucose 222 mg/dL
Creatinine 1.1 mg/dL
Urinalysis is within normal limits. Which of the following is the most likely cause of these findings?
- A. Reperfusion injury (Correct Answer)
- B. Cellulitis
- C. Cholesterol embolism
- D. Deep vein thrombosis
- E. Rhabdomyolysis
Postoperative anesthesia complications Explanation: ***Reperfusion injury***
- The patient's symptoms of **severe pain, numbness, and tingling** in the left leg following an embolectomy, along with **swelling, stiffness, and tenderness** of the extremity, and pain on passive dorsiflexion (**pain with passive stretch**), are classic signs of **acute compartment syndrome**.
- In this context, compartment syndrome is caused by **reperfusion injury** following prolonged limb ischemia. When blood flow is restored after prolonged ischemia, the reperfusion causes **oxidative stress, inflammatory mediator release, and increased capillary permeability**, leading to **tissue edema and elevated intracompartmental pressure** that compresses nerves and vessels.
- The **2-hour timeline** post-embolectomy and the clinical triad of pain out of proportion, pain with passive stretch, and paresthesias make reperfusion injury leading to compartment syndrome the most likely diagnosis.
*Cellulitis*
- While cellulitis causes **pain, swelling, and redness**, it typically has a more **gradual onset** and is associated with warmth, erythema, and signs of infection.
- The **acute onset** (2 hours post-surgery), **severe neurologic symptoms** (numbness, tingling), and **pain with passive stretch** are not characteristic of cellulitis.
- The absence of fever, significant leukocytosis, or spreading erythema makes cellulitis unlikely.
*Cholesterol embolism*
- **Cholesterol emboli** can occur after vascular procedures and typically present with **livedo reticularis**, **"blue toe" syndrome**, **renal impairment**, or **eosinophilia**.
- While possible after arterial manipulation, the acute presentation with signs of **elevated compartment pressure** (pain with passive stretch, swelling, paresthesias) points to a pressure-related compartment issue rather than distal microembolization.
*Deep vein thrombosis*
- **DVT** causes **unilateral leg swelling, pain, and tenderness** but typically presents with a more **gradual onset** over hours to days.
- DVT would not explain the **acute severe pain with passive stretch**, **rapid neurologic symptoms** (paresthesias), or the **compartment syndrome findings** seen immediately (2 hours) post-procedure.
- The clinical picture of acute compartment syndrome better fits ischemia-reperfusion injury.
*Rhabdomyolysis*
- **Rhabdomyolysis** involves muscle breakdown due to prolonged ischemia or trauma and is characterized by **elevated creatinine kinase (CK)**, **myoglobinuria**, and potentially **acute kidney injury**.
- While rhabdomyolysis can occur **secondary to** both the initial ischemia and subsequent compartment syndrome, it is a **consequence or complication** rather than the **primary cause** of the acute compartment syndrome findings.
- The immediate clinical presentation (severe pain with passive stretch, paresthesias, swelling) reflects **elevated intracompartmental pressure from reperfusion injury**, not rhabdomyolysis itself.
More Postoperative anesthesia complications US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.