Perioperative respiratory management US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Perioperative respiratory management. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Perioperative respiratory management US Medical PG Question 1: A 21-year-old man undergoes orthopedic surgery for a leg fracture that he has sustained in a motorbike accident. After induction of anesthesia with desflurane, the patient's respiratory minute ventilation decreases notably. Which of the following additional effects is most likely to occur in response to this drug?
- A. Decreased seizure threshold
- B. Increased intracranial pressure (Correct Answer)
- C. Increased skeletal muscle tonus
- D. Increased cerebral metabolic rate
- E. Increased glomerular filtration rate
Perioperative respiratory management Explanation: ***Increased intracranial pressure***
- **Desflurane**, like other volatile anesthetics, causes **cerebral vasodilation**, leading to increased cerebral blood flow and consequently **increased intracranial pressure (ICP)**.
- This effect is particularly pronounced with desflurane and is a key concern, especially in patients with pre-existing elevated ICP.
*Decreased seizure threshold*
- While some anesthetics can lower the seizure threshold, **desflurane** is generally considered to be **seizure-neutral** or even anticonvulsant at higher concentrations.
- **Enflurane** is an example of an inhaled anesthetic known to reliably induce epileptiform activity.
*Increased skeletal muscle tonus*
- **Volatile anesthetics** generally cause **skeletal muscle relaxation**, which is why they are often used with neuromuscular blockers during surgery.
- An increase in skeletal muscle tonus is seen in conditions like **malignant hyperthermia**, which can be triggered by desflurane, but this is a rare, life-threatening genetic disorder, not a typical effect of the drug.
*Increased cerebral metabolic rate*
- **Desflurane** typically causes a **dose-dependent reduction in the cerebral metabolic rate for oxygen (CMRO2)**, indicating a decrease in brain activity.
- This is often beneficial during anesthesia, providing **neuroprotection**, despite the concurrent cerebral vasodilation.
*Increased glomerular filtration rate*
- **Volatile anesthetics**, including desflurane, tend to cause a **dose-dependent decrease in renal blood flow and glomerular filtration rate (GFR)** due to systemic vasodilation and decreased cardiac output.
- Renal function is generally preserved in healthy individuals, but the GFR does not increase with the use of desflurane.
Perioperative respiratory management US Medical PG Question 2: A 56-year-old previously healthy woman with no other past medical history is post-operative day one from an open reduction and internal fixation of a fractured right radius and ulna after a motor vehicle accident. What is one of the primary ways of preventing postoperative pneumonia in this patient?
- A. Shallow breathing exercises
- B. Incentive spirometry (Correct Answer)
- C. Outpatient oral antibiotics
- D. Hyperbaric oxygenation
- E. In-hospital intravenous antibiotics
Perioperative respiratory management Explanation: ***Incentive spirometry***
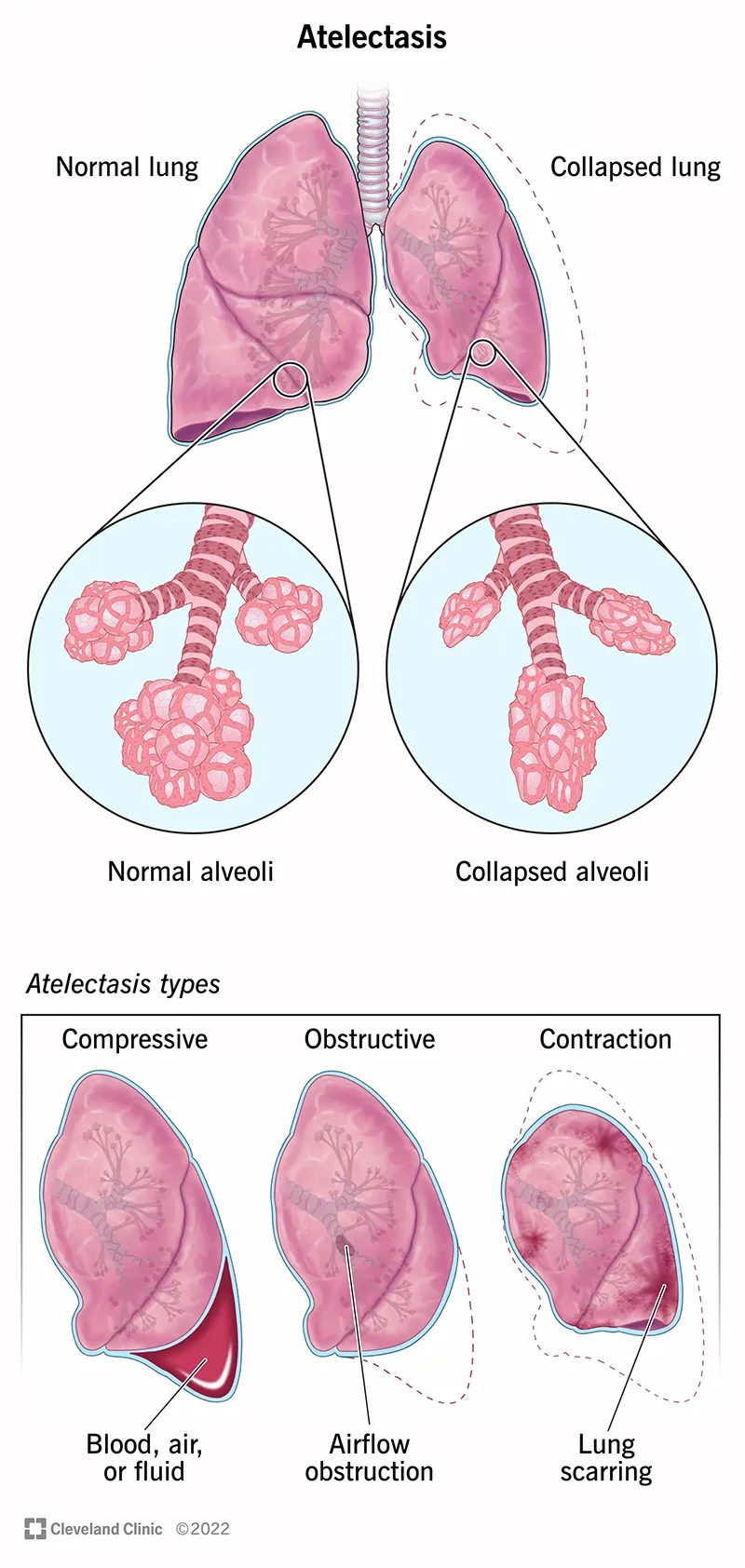
- **Incentive spirometry** is a cornerstone of postoperative care, actively encouraging patients to take slow, deep breaths. This expands the lungs and prevents the collapse of alveoli, reducing the risk of **atelectasis** and subsequent **pneumonia**.
- Its effectiveness lies in promoting lung aeration and clearing secretions, which are crucial after anesthesia and surgery, especially in patients with reduced mobility or pain.
*Shallow breathing exercises*
- **Shallow breathing** is insufficient for adequate lung expansion and can actually contribute to **atelectasis** and the pooling of secretions in the lungs.
- Effective pulmonary hygiene requires **deep breaths** to maximize alveolar recruitment and prevent respiratory complications.
*Outpatient oral antibiotics*
- **Prophylactic antibiotics** are typically given around the time of surgery to prevent surgical site infections, not primarily to prevent postoperative pneumonia in an outpatient setting.
- Administering antibiotics without a diagnosed infection can lead to **antibiotic resistance** and is not a standard practice for preventing pneumonia unless a specific risk factor or existing infection is identified.
*Hyperbaric oxygenation*
- **Hyperbaric oxygenation** involves breathing 100% oxygen in a pressurized chamber and is used for conditions like **decompression sickness**, non-healing wounds, or severe infections.
- It is not a standard or primary method for preventing postoperative pneumonia, as its mechanism of action is unrelated to common pulmonary hygiene techniques.
*In-hospital intravenous antibiotics*
- While antibiotics can treat pneumonia, their routine, **prophylactic use** intravenously in-hospital solely for preventing postoperative pneumonia is generally unwarranted and can contribute to **antibiotic resistance**.
- Antibiotics are indicated if there is evidence of an active infection, but the primary prevention of pneumonia focuses on mechanical lung expansion and airway clearance.
Perioperative respiratory management US Medical PG Question 3: Five minutes after arriving in the postoperative care unit following total knee replacement under general anesthesia, a 55-year-old woman is acutely short of breath. The procedure was uncomplicated. Postoperatively, prophylactic treatment with cefazolin was begun and the patient received morphine and ketorolac for pain management. She has generalized anxiety disorder. Her only other medication is escitalopram. She has smoked one pack of cigarettes daily for 25 years. Her temperature is 37°C (98.6°F), pulse is 108/min, respirations are 26/min, and blood pressure is 95/52 mm Hg. A flow-volume loop obtained via pulmonary function testing is shown. Which of the following is the most likely underlying cause of this patient's symptoms?
- A. Decreased central respiratory drive
- B. Neuromuscular blockade
- C. Bronchial hyperresponsiveness
- D. Rupture of an alveolar bleb
- E. Type I hypersensitivity reaction (Correct Answer)
Perioperative respiratory management Explanation: ***Type I hypersensitivity reaction***
- The patient's acute shortness of breath, **tachycardia (pulse 108/min)**, **hypotension (95/52 mm Hg)**, and tachypnea (respirations 26/min) immediately post-surgery are highly suggestive of **anaphylaxis**, which is a severe, systemic type I hypersensitivity reaction.
- The sudden onset shortly after general anesthesia and initiation of prophylactic cefazolin points to a potential allergic reaction to a medication administered during this period (e.g., **antibiotics**, **neuromuscular blockers**, anesthetics).
*Decreased central respiratory drive*
- This would typically lead to **bradypnea** or hypopnea rather than the tachypnea seen in this patient.
- While opioids like morphine can depress respiratory drive, the patient's respiratory rate of 26/min indicates an *increased* drive.
*Neuromuscular blockade*
- Residual neuromuscular blockade would cause respiratory muscle weakness, leading to **shallow breathing** and potentially hypoventilation, but not typically the acute onset of shortness of breath with tachypnea and systemic hemodynamic instability observed here.
- The immediate onset of symptoms also points away from persistent effects of intraoperative neuromuscular blockers, which are usually reversed before emergence.
*Bronchial hyperresponsiveness*
- While the patient is a smoker, which can predispose to respiratory issues, **bronchial hyperresponsiveness** (e.g., asthma exacerbation) typically presents with **wheezing**, prolonged expiration, and often hypoxemia, which are not described.
- The severe hypotension and acute onset of systemic symptoms are not typical features of an isolated asthma flare-up.
*Rupture of an alveolar bleb*
- A ruptured bleb can cause a **pneumothorax**, leading to sudden shortness of breath and chest pain.
- However, it would not typically cause **systemic hypotension** or tachycardia to this degree without other signs of tension pneumothorax (e.g., tracheal deviation, absent breath sounds).
Perioperative respiratory management US Medical PG Question 4: A 57-year-old man presents to the clinic for a chronic cough over the past 4 months. The patient reports a productive yellow/green cough that is worse at night. He denies any significant precipitating event prior to his symptoms. He denies fever, chest pain, palpitations, weight changes, or abdominal pain, but endorses some difficulty breathing that waxes and wanes. He denies alcohol usage but endorses a 35 pack-year smoking history. A physical examination demonstrates mild wheezes, bibasilar crackles, and mild clubbing of his fingertips. A pulmonary function test is subsequently ordered, and partial results are shown below:
Tidal volume: 500 mL
Residual volume: 1700 mL
Expiratory reserve volume: 1500 mL
Inspiratory reserve volume: 3000 mL
What is the functional residual capacity of this patient?
- A. 4500 mL
- B. 2000 mL
- C. 2200 mL
- D. 3200 mL (Correct Answer)
- E. 3500 mL
Perioperative respiratory management Explanation: ***3200 mL***
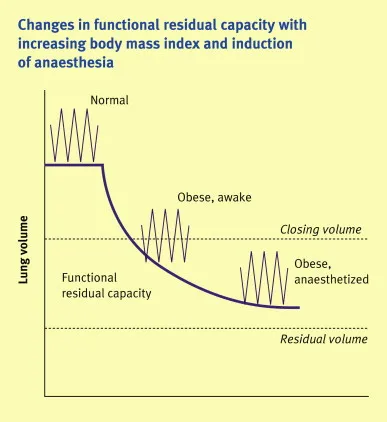
- The **functional residual capacity (FRC)** is the volume of air remaining in the lungs after a normal expiration.
- It is calculated as the sum of the **expiratory reserve volume (ERV)** and the **residual volume (RV)**. In this case, 1500 mL (ERV) + 1700 mL (RV) = 3200 mL.
*4500 mL*
- This value represents the sum of the **inspiratory reserve volume (3000 mL)** and the **residual volume (1700 mL)**, which does not correspond to a standard lung volume or capacity.
- It does not logically relate to the definition of functional residual capacity.
*2000 mL*
- This value represents the sum of the **tidal volume (500 mL)** and the **expiratory reserve volume (1500 mL)**, which is incorrect for FRC.
- This would represent the inspiratory capacity minus the inspiratory reserve volume, which is not a standard measurement used in pulmonary function testing.
*2200 mL*
- This value could be obtained by incorrectly adding the **tidal volume (500 mL)** and the **residual volume (1700 mL)**, which is not the correct formula for FRC.
- This calculation represents a miscombination of lung volumes that does not correspond to any standard pulmonary capacity measurement.
*3500 mL*
- This value is the sum of the **tidal volume (500 mL)**, the **expiratory reserve volume (1500 mL)**, and the **residual volume (1700 mL)**.
- This would represent the FRC plus the tidal volume, which is not a standard measurement and does not represent the functional residual capacity.
Perioperative respiratory management US Medical PG Question 5: A 23-year-old man is admitted to the intensive care unit with acute respiratory distress syndrome (ARDS) due to influenza A. He has no history of serious illness and does not smoke. An x-ray of the chest shows diffuse bilateral infiltrates. Two weeks later, his symptoms have improved. Pulmonary examination on discharge shows inspiratory crackles at both lung bases. This patient is most likely to develop which of the following long-term complications?
- A. Panacinar emphysema
- B. Asthma
- C. Pulmonary embolism
- D. Interstitial lung disease (Correct Answer)
- E. Spontaneous pneumothorax
Perioperative respiratory management Explanation: ***Interstitial lung disease***
- Patients who recover from **acute respiratory distress syndrome (ARDS)**, especially severe cases like that induced by influenza A, often develop **pulmonary fibrosis** leading to interstitial lung disease.
- The presence of **inspiratory crackles at both lung bases** after recovery from ARDS strongly suggests residual fibrotic changes.
*Panacinar emphysema*
- This condition is typically associated with **alpha-1 antitrypsin deficiency** or long-term smoking history, neither of which is indicated in this patient.
- Emphysema involves destruction of alveoli, not typically a direct long-term consequence of ARDS.
*Asthma*
- Asthma is a chronic inflammatory airway disease characterized by **reversible airflow obstruction**, usually with a history of recurrent episodes, not necessarily a direct sequela of ARDS.
- This patient's previous lack of serious illness and the nature of ARDS recovery make new-onset asthma unlikely as a long-term complication.
*Pulmonary embolism*
- While ARDS patients are at increased risk of **venous thromboembolism** during the acute phase due to immobility and inflammation, it is an acute complication, not a typical long-term sequela.
- Long-term complications are more related to lung parenchymal damage rather than persistent embolic risk.
*Spontaneous pneumothorax*
- Although ARDS can be complicated by **barotrauma** and pneumothorax during mechanical ventilation, a spontaneous pneumothorax as a long-term complication after recovery is less common.
- It does not explain the persistent bilateral basal crackles.
Perioperative respiratory management US Medical PG Question 6: A 63-year-old man undergoes workup for nocturnal dyspnea and what he describes as a "choking" sensation while sleeping. He also endorses fatigue and dyspnea on exertion. Physical exam reveals a normal S1, loud P2, and a neck circumference of 17 inches (43 cm) (normal < 14 inches (< 35 cm)). His temperature is 98.8°F (37°C), blood pressure is 128/82 mmHg, pulse is 86/min, and respirations are 19/min. He undergoes spirometry, which is unrevealing, and polysomnography, which shows 16 hypopneic and apneic events per hour. Mean pulmonary arterial pressure is 30 mmHg. Which of the following complications is this patient most at risk for?
- A. Left ventricular failure
- B. Right ventricular failure (Correct Answer)
- C. Pulmonary embolism
- D. Aspiration pneumonia
- E. Chronic obstructive pulmonary disease
Perioperative respiratory management Explanation: ***Right ventricular failure***
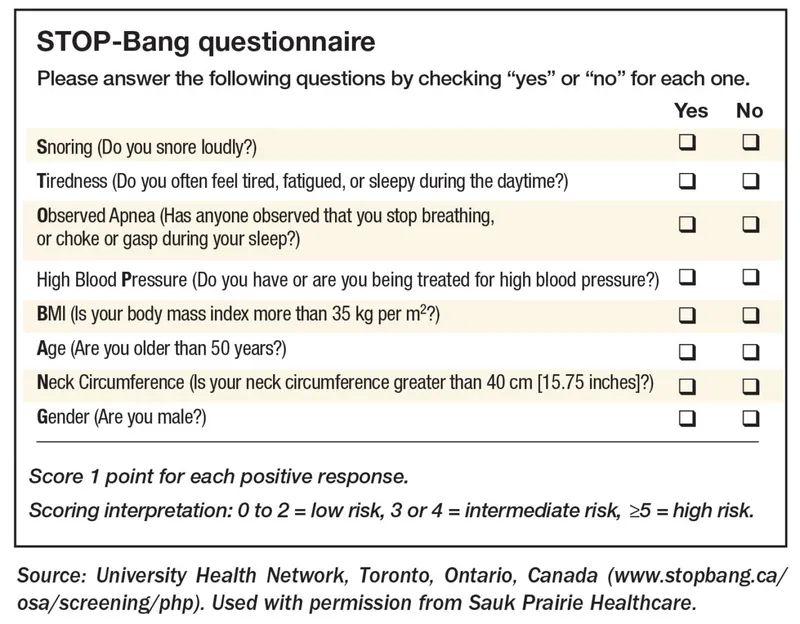
- The patient's symptoms (nocturnal dyspnea, choking sensation, fatigue, exertional dyspnea), risk factors (large neck circumference), and polysomnography results (16 hypopneic/apneic events/hour) are consistent with **obstructive sleep apnea (OSA)**.
- OSA leads to **chronic intermittent hypoxia** and hypercapnia, causing **pulmonary vasoconstriction** and increased pulmonary arterial pressure (mean PAP 30 mmHg), which can result in **pulmonary hypertension** and eventually **right ventricular failure**.
*Left ventricular failure*
- While OSA can exacerbate cardiovascular conditions, the primary cardiac complication directly resulting from ongoing pulmonary hypertension due to OSA is typically right-sided, not primarily left-sided, failure.
- There are no specific findings in the description (e.g., S3 gallop, crackles) that strongly point to left ventricular dysfunction as the most immediate and direct complication.
*Pulmonary embolism*
- Although obesity (suggested by large neck circumference) is a risk factor for pulmonary embolism, there are no acute symptoms (e.g., sudden onset dyspnea, pleuritic chest pain, hemoptysis) or signs (e.g., tachycardia, hypoxemia) to suggest a pulmonary embolism.
- The patient's symptoms are chronic and related to sleep-disordered breathing and pulmonary hypertension.
*Aspiration pneumonia*
- While a "choking" sensation could potentially lead to aspiration, there's no evidence of infection (e.g., fever, productive cough, crackles) or recurrent aspiration events.
- The primary respiratory pathology is clearly defined by the polysomnography and elevated pulmonary pressures.
*Chronic obstructive pulmonary disease*
- Spirometry was reported as "unrevealing," which rules out significant airflow limitation characteristic of COPD.
- The patient's symptoms are more indicative of sleep-disordered breathing and its cardiovascular consequences rather than an intrinsic obstructive lung disease like COPD.
Perioperative respiratory management US Medical PG Question 7: A 34-year-old man comes to the physician for a follow-up examination. He has a 3-month history of a nonproductive cough. He has been treated with diphenhydramine since his last visit 2 weeks ago, but his symptoms have persisted. He does not smoke. He drinks 3 beers on the weekends. He is 177 cm (5 ft 10 in) tall and weighs 100 kg (220.46 lbs); BMI is 35.1 kg/m2. His temperature is 37.1°C (98.8°F), pulse is 78/min, respirations are 14/min, and blood pressure is 130/80 mm Hg. Pulse oximetry on room air shows an oxygen saturation of 97%. Physical examination and an x-ray of the chest show no abnormalities. Which of the following is the most appropriate next step in management?
- A. Azithromycin therapy
- B. Pulmonary function testing
- C. CT scan of the chest
- D. Omeprazole therapy (Correct Answer)
- E. Oral corticosteroid therapy
Perioperative respiratory management Explanation: ***Omeprazole therapy***
- The patient's **obesity** (BMI 35.1), **nonproductive cough** lasting 3 months, and persistent symptoms despite antihistamines strongly suggest **gastroesophageal reflux disease (GERD)** as the cause.
- **Proton pump inhibitors (PPIs)** like omeprazole are the first-line treatment for GERD.
*Azithromycin therapy*
- Azithromycin is an **antibiotic** used to treat bacterial infections. There is no evidence of infection (e.g., fever, abnormal chest X-ray, purulent sputum) in this patient.
- Empiric antibiotic use for a nonproductive cough without signs of infection is generally inappropriate and can contribute to **antibiotic resistance**.
*Pulmonary function testing*
- Pulmonary function testing (PFTs) would be appropriate if there were concerns for **asthma**, **COPD**, or other intrinsic lung diseases, which are not suggested by the normal chest X-ray, oxygen saturation, and absence of wheezing or dyspnea.
- The patient's lack of smoking history also makes COPD less likely.
*CT scan of the chest*
- A CT scan of the chest would be indicated for persistent cough if the **chest X-ray were abnormal** or if there were suspicion of a malignancy, interstitial lung disease, or bronchiectasis.
- Given the normal chest X-ray and 3-month duration, a CT scan is not the initial next step, especially when there's a strong alternative diagnosis like GERD.
*Oral corticosteroid therapy*
- Oral corticosteroids are used to treat inflammatory conditions like asthma or COPD exacerbations.
- There is no indication of airflow obstruction, allergic reaction, or significant inflammation based on the clinical presentation and normal chest X-ray, making corticosteroids inappropriate.
Perioperative respiratory management US Medical PG Question 8: A 63-year-old man presents to the clinic complaining of burning bilateral leg pain which has been increasing gradually over the past several months. It worsens when he walks but improves with rest. His past medical and surgical history are significant for hypertension, hyperlipidemia, diabetes, and a 40-pack-year smoking history. His temperature is 99.0°F (37.2°C), blood pressure is 167/108 mm Hg, pulse is 88/min, respirations are 13/min, and oxygen saturation is 95% on room air. Physical exam of the lower extremities reveals palpable but weak posterior tibial and dorsalis pedis pulses bilaterally. Which of the following is the best initial treatment for this patient's symptoms?
- A. Exercise and smoking cessation (Correct Answer)
- B. Lovenox and atorvastatin
- C. Lisinopril and atorvastatin
- D. Balloon angioplasty with stenting
- E. Femoral-popliteal bypass
Perioperative respiratory management Explanation: ***Exercise and smoking cessation***
- This patient presents with symptoms highly suggestive of **peripheral artery disease (PAD)**, characterized by **intermittent claudication** (leg pain worsening with activity and improving with rest), and risk factors like diabetes, hypertension, hyperlipidemia, and smoking.
- **Smoking cessation** is the single most important modifiable risk factor, and a supervised **exercise program** (walking to the point of claudication) is the most effective initial treatment to improve walking distance and quality of life for PAD patients.
*Lovenox and atorvastatin*
- **Atorvastatin** is appropriate for dyslipidemia and cardiovascular risk reduction in PAD patients, but **Lovenox (low molecular weight heparin)** is an anticoagulant typically used for acute thrombotic events or VTE prophylaxis, not initial management of chronic stable claudication.
- While statins are important for secondary prevention, Lovenox does not directly address the primary management of claudication symptoms or underlying atherosclerotic progression in this stable setting.
*Lisinopril and atorvastatin*
- **Lisinopril** is an ACE inhibitor suitable for hypertension, which is important for overall cardiovascular health but not the primary initial treatment for claudication symptoms.
- While both medications address risk factors, they do not directly target the improvement of walking function and symptom relief as effectively as exercise and smoking cessation in the initial phase.
*Balloon angioplasty with stenting*
- Invasive revascularization procedures like **balloon angioplasty with stenting** are typically reserved for patients with more severe symptoms (e.g., rest pain, non-healing ulcers, critical limb ischemia) or those who have failed conservative management like exercise therapy.
- This is not the **best initial treatment** for a patient with stable claudication.
*Femoral-popliteal bypass*
- **Femoral-popliteal bypass** is a surgical revascularization procedure indicated for more severe PAD, particularly in cases of critical limb ischemia or long-segment occlusions that are not amenable to endovascular repair.
- Like angioplasty, it is a more aggressive intervention and not the **initial treatment of choice** for intermittent claudication.
Perioperative respiratory management US Medical PG Question 9: An obese 52-year-old man is brought to the emergency department because of increasing shortness of breath for the past 8 hours. Two months ago, he noticed a mass on the right side of his neck and was diagnosed with laryngeal cancer. He has smoked two packs of cigarettes daily for 27 years. He drinks two pints of rum daily. He appears ill. He is oriented to person, place, and time. His temperature is 37°C (98.6°F), pulse is 111/min, respirations are 34/min, and blood pressure is 140/90 mm Hg. Pulse oximetry on room air shows an oxygen saturation of 89%. Examination shows a 9-cm, tender, firm subglottic mass on the right side of the neck. Cervical lymphadenopathy is present. His breathing is labored and he has audible inspiratory stridor but is able to answer questions. The lungs are clear to auscultation. Arterial blood gas analysis on room air shows:
pH 7.36
PCO2 45 mm Hg
PO2 74 mm Hg
HCO3- 25 mEq/L
He has no advanced directive. Which of the following is the most appropriate next step in management?
- A. Comfort care measures
- B. Cricothyroidotomy (Correct Answer)
- C. Tracheostomy
- D. Intramuscular epinephrine
- E. Tracheal stenting
Perioperative respiratory management Explanation: ***Correct: Cricothyroidotomy***
- This patient has **impending complete airway obstruction** evidenced by inspiratory stridor, severe tachypnea (34/min), hypoxia (O2 sat 89%), and a large obstructing laryngeal mass
- **Cricothyroidotomy** is the emergent surgical airway procedure of choice when there is **imminent or actual complete upper airway obstruction** and endotracheal intubation cannot be safely performed
- The subglottic mass makes endotracheal intubation **extremely dangerous** - instrumentation could precipitate complete obstruction and inability to ventilate
- Cricothyroidotomy provides **immediate airway access** (can be performed in 30-60 seconds) below the level of obstruction, making it life-saving in this emergency
- In the "cannot intubate, cannot ventilate" scenario, cricothyroidotomy is the definitive emergency intervention per ATLS and airway management guidelines
*Incorrect: Tracheostomy*
- While tracheostomy provides definitive airway management, it is a **controlled, elective procedure** typically performed in the OR that takes 20-30 minutes
- This patient requires **immediate airway access** - waiting for OR setup and performing tracheostomy risks complete airway collapse and death
- Tracheostomy may be performed later as a planned procedure once the airway is secured with cricothyroidotomy
- The presence of stridor indicates **critical airway narrowing** requiring emergency intervention, not elective surgery
*Incorrect: Comfort care measures*
- The patient is **alert and oriented** without an advanced directive indicating wishes for comfort care only
- This is an **acute, reversible condition** with appropriate emergency airway intervention
- Presumed consent applies in life-threatening emergencies when the patient cannot formally consent but intervention would be life-saving
- Comfort care would be inappropriate without documented patient wishes or irreversible terminal condition
*Incorrect: Intramuscular epinephrine*
- Epinephrine is indicated for **anaphylaxis** or angioedema causing airway edema from allergic/inflammatory mechanisms
- This patient has **mechanical obstruction** from a solid tumor mass, which will not respond to epinephrine
- Epinephrine causes vasoconstriction and reduces mucosal edema but cannot reduce tumor mass
- Would delay definitive airway management and not address the underlying problem
*Incorrect: Tracheal stenting*
- Tracheal stenting requires **bronchoscopy** in a controlled setting and is used for palliation of tracheal narrowing
- Cannot be performed emergently in an unstable patient with impending airway obstruction
- The obstruction is at the **laryngeal/subglottic level**, not typically amenable to emergency stenting
- Requires time for procedure setup and sedation, which this patient cannot afford given the critical airway emergency
Perioperative respiratory management US Medical PG Question 10: A 47-year-old man is brought to the emergency room by his wife. She states that they were having dinner at a restaurant when the patient suddenly became out of breath. His past medical history is irrelevant but has a 20-year pack smoking history. On evaluation, the patient is alert and verbally responsive but in moderate respiratory distress. His temperature is 37°C (98.6°F), blood pressure is 85/56 mm Hg, pulse is 102/min, and respirations are 20/min. His oxygen saturation is 88% on 2L nasal cannula. An oropharyngeal examination is unremarkable. The trachea is deviated to the left. Cardiopulmonary examination reveals decreased breath sounds on the right lower lung field with nondistended neck veins. Which of the following is the next best step in the management of this patient?
- A. Urgent needle decompression (Correct Answer)
- B. D-dimer levels
- C. Nebulization with albuterol
- D. Chest X-ray
- E. Heimlich maneuver
Perioperative respiratory management Explanation: ***Urgent needle decompression***
- The patient presents with sudden onset **respiratory distress**, **tracheal deviation** to the left (away from the affected right side), **decreased breath sounds** on the right, and **hypotension** with **tachycardia**. These are classic signs of a **tension pneumothorax**, which requires immediate needle decompression.
- This is a life-threatening emergency where air accumulates in the pleural space under positive pressure, collapsing the lung and shifting mediastinal structures, compromising venous return to the heart.
*D-dimer levels*
- While helpful in the workup for pulmonary embolism, **D-dimer levels** are not relevant as the immediate next step for a patient in acute respiratory distress with clear signs of tracheal deviation and decreased breath sounds, which points toward a mechanical lung issue.
- The patient's presentation with acute, severe respiratory symptoms and hemodynamic instability mandates immediate life-saving intervention.
*Nebulization with albuterol*
- **Albuterol** is used for bronchospasm, as seen in asthma or COPD exacerbations. This patient's symptoms are sudden and severe, with clear signs of a **tension pneumothorax**, which would not respond to bronchodilators.
- There is no indication of wheezing or a history of reactive airway disease to suggest this as a primary treatment.
*Chest X-ray*
- A **chest X-ray** would confirm the diagnosis of tension pneumothorax. However, given the patient's severe respiratory distress, hypotension, and classic physical findings (tracheal deviation, absent breath sounds), performing an X-ray would delay life-saving intervention.
- In a true tension pneumothorax, diagnosis is clinical, and immediate intervention takes precedence over imaging.
*Heimlich maneuver*
- The **Heimlich maneuver** is indicated for foreign body airway obstruction. The patient is verbally responsive, which indicates a patent airway, and there are no direct signs of choking on food.
- Although the patient was having dinner, the distinct clinical signs of **tracheal deviation** and unilateral decreased breath sounds do not support an airway obstruction requiring the Heimlich maneuver.
More Perioperative respiratory management US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.