Perioperative cardiovascular management US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Perioperative cardiovascular management. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Perioperative cardiovascular management US Medical PG Question 1: A 56-year-old man comes to the emergency department complaining of substernal chest pain that radiates to the left shoulder. Electrocardiogram (EKG) demonstrates ST-elevations in leads II, III, and aVF. The patient subsequently underwent catheterization with drug-eluting stent placement with stabilization of his condition. On post-operative day 3, the patient experiences stabbing chest pain that is worse with inspiration, diaphoresis, and general distress. His temperature is 98.7°F (37.1°C), blood pressure is 145/97mmHg, pulse is 110/min, and respirations are 23/min. EKG demonstrates diffuse ST-elevations. What is the best treatment for this patient?
- A. Lisinopril
- B. Surgery
- C. Needle thoracotomy
- D. Atorvastatin
- E. Aspirin (Correct Answer)
Perioperative cardiovascular management Explanation: ***Aspirin***
- The patient's symptoms (stabbing chest pain worse with inspiration, diffuse ST-elevations) on **post-operative day 3** following a myocardial infarction and stent placement are highly suggestive of **early post-MI pericarditis** (also called acute pericarditis or epistenocardiac pericarditis).
- This occurs within the **first few days** after MI due to direct inflammatory response from myocardial necrosis, distinguished from **Dressler's syndrome** which is a delayed autoimmune phenomenon occurring **1-6 weeks** post-MI.
- **Aspirin** is the first-line treatment for post-MI pericarditis (both early and late forms), as it effectively reduces inflammation while being safer than other NSAIDs in the post-MI setting.
*Lisinopril*
- **Lisinopril** is an ACE inhibitor used for **hypertension**, heart failure, and post-MI remodeling, but it does not address the acute inflammatory process of pericarditis.
- While beneficial for long-term cardiac health post-MI, it is not the immediate treatment for these new inflammatory symptoms.
*Surgery*
- **Surgery** (e.g., pericardiectomy) is reserved for severe, recurrent, or constrictive pericarditis that is refractory to medical therapy.
- It is an invasive procedure and not the initial treatment for an acute episode of post-MI pericarditis.
*Needle thoracotomy*
- A **needle thoracotomy** (needle decompression) is an emergency procedure used to treat a **tension pneumothorax**, which involves air accumulation in the pleural space causing hemodynamic compromise.
- The patient's symptoms and EKG findings of diffuse ST-elevations are consistent with pericarditis, not tension pneumothorax.
*Atorvastatin*
- **Atorvastatin** is a statin used to lower cholesterol and prevent further cardiovascular events.
- While important for secondary prevention after an MI, it does not provide acute relief or treatment for the inflammatory chest pain this patient is experiencing.
Perioperative cardiovascular management US Medical PG Question 2: A patient presents with periods of severe headaches and flushing however every time they have come to the physician they have not experienced any symptoms. The only abnormal finding is a blood pressure of 175 mmHg/100 mmHg. It is determined that the optimal treatment for this patient is surgical. Prior to surgery which of the following noncompetitive inhibitors should be administered?
- A. Phentolamine
- B. Isoproterenol
- C. Atropine
- D. Propranolol
- E. Phenoxybenzamine (Correct Answer)
Perioperative cardiovascular management Explanation: ***Phenoxybenzamine***
- This patient likely has a **pheochromocytoma**, which explains the episodic headaches, flushing, and hypertension. **Phenoxybenzamine** is a **non-competitive, irreversible alpha-adrenergic blocker** that is crucial for preoperative preparation to prevent a **hypertensive crisis** during surgery.
- Its **irreversible binding** provides sustained alpha blockade, essential to control blood pressure and avoid catecholamine-induced surges during tumor manipulation.
*Phentolamine*
- **Phentolamine** is a **competitive alpha-adrenergic blocker** used to manage acute hypertensive episodes, but it has a shorter duration of action.
- It is not preferred for sustained preoperative alpha blockade due to its **reversible nature** and potential for drug washout during surgery, which could lead to catecholamine surges.
*Isoproterenol*
- **Isoproterenol** is a **beta-adrenergic agonist** that increases heart rate and contractility, and causes bronchodilation.
- It would be contraindicated in a patient with pheochromocytoma as it could worsen hypertension and cardiac symptoms by stimulating beta receptors that are already overly sensitive to endogenous catecholamines.
*Atropine*
- **Atropine** is a **muscarinic acetylcholine receptor antagonist** that blocks parasympathetic effects, like bradycardia and salivation.
- It has no role in managing hypertension or the catecholamine excess seen in pheochromocytoma.
*Propranolol*
- **Propranolol** is a **non-selective beta-adrenergic blocker** that can be used to control tachycardia and arrhythmias in pheochromocytoma, but only *after* adequate alpha-blockade has been established.
- Using **propranolol alone** or before alpha-blockade can lead to **unopposed alpha-adrenergic stimulation**, resulting in a severe, life-threatening hypertensive crisis.
Perioperative cardiovascular management US Medical PG Question 3: A 60-year-old woman presents to the emergency room with chest pain that started 20 minutes ago while watching television at home. The pain is substernal and squeezing in nature. She rates the pain as 6/10 and admits to having similar pain in the past with exertion. Her past medical history is significant for diabetes mellitus that is controlled with metformin. The physical examination is unremarkable. An electrocardiogram (ECG) shows ST-segment depression in the lateral leads. She is started on aspirin, nitroglycerin, metoprolol, unfractionated heparin, and insulin. She is asked not to take metformin while at the hospital. Three sets of cardiac enzymes are negative.
Lab results are given below:
Serum glucose 88 mg/dL
Sodium 142 mEq/L
Potassium 3.9 mEq/L
Chloride 101 mEq/L
Serum creatinine 1.2 mg/dL
Blood urea nitrogen 22 mg/dL
Cholesterol, total 170 mg/dL
HDL-cholesterol 40 mg/dL
LDL-cholesterol 80 mg/dL
Triglycerides 170 mg/dL
Hematocrit 38%
Hemoglobin 13 g/dL
Leucocyte count 7,500/mm3
Platelet count 185,000 /mm3
Activated partial thromboplastin time (aPTT) 30 seconds
Prothrombin time (PT) 12 seconds
Urinalysis
Glucose negative
Ketones negative
Leucocytes negative
Nitrites negative
Red blood cells (RBC) negative
Casts negative
An echocardiogram reveals left ventricular wall motion abnormalities. With the pain subsiding, she was admitted and the medications were continued. A coronary angiography is planned in 4 days. In addition to regular blood glucose testing, which of the following should be closely monitored in this patient?
- A. Activated partial thromboplastin time (aPTT) alone
- B. Prothrombin time alone
- C. aPTT and platelet count (Correct Answer)
- D. Platelet count alone
- E. Prothrombin time and platelet count
Perioperative cardiovascular management Explanation: ***aPTT and platelet count***
- The patient is receiving **unfractionated heparin**, which requires monitoring of **aPTT** to ensure therapeutic anticoagulation and prevent bleeding complications.
- Heparin can also induce **heparin-induced thrombocytopenia (HIT)**, necessitating close monitoring of the **platelet count**.
*Activated partial thromboplastin time (aPTT) alone*
- While **aPTT** monitoring is crucial for unfractionated heparin, it does not account for the risk of **heparin-induced thrombocytopenia (HIT)**.
- Monitoring platelet count is equally important alongside aPTT in patients receiving heparin.
*Prothrombin time alone*
- **Prothrombin time (PT)** is used to monitor **warfarin** therapy, not unfractionated heparin.
- Monitoring PT in this context would be inappropriate and would not provide information about the efficacy or safety of the prescribed heparin.
*Platelet count alone*
- Monitoring **platelet count** is important for detecting **heparin-induced thrombocytopenia (HIT)**, but it does not assess the therapeutic effect of heparin.
- **aPTT** monitoring is essential to ensure adequate anticoagulation and prevent thrombotic events.
*Prothrombin time and platelet count*
- **Prothrombin time (PT)** is irrelevant for unfractionated heparin monitoring, as it measures the extrinsic pathway and is used for warfarin.
- Although **platelet count** monitoring is important, relying on PT is incorrect for unfractionated heparin management.
Perioperative cardiovascular management US Medical PG Question 4: A 66-year-old man comes to the emergency department because of a 1-day history of chest pain, palpitations, and dyspnea on exertion. He had a similar episode 3 days ago and was diagnosed with an inferior wall myocardial infarction. He was admitted and a percutaneous transluminal coronary angioplasty was successfully done that day. A fractional flow reserve test during the procedure showed complete resolution of the stenosis. Laboratory tests including serum glucose, lipids, and blood count were within normal limits. He was discharged the day after the procedure on a drug regimen of aspirin, simvastatin, and isosorbide dinitrate. At the time of discharge, he had no chest pain or dyspnea. Presently, his vitals are normal and ECG at rest shows new T-wave inversion. Which of the following is the most reliable test for rapidly establishing the diagnosis in this patient?
- A. Creatine kinase MB
- B. Lactate dehydrogenase
- C. Copeptin
- D. Aspartate aminotransferase
- E. Cardiac troponin T (Correct Answer)
Perioperative cardiovascular management Explanation: ***Cardiac troponin T***
- **Cardiac troponin T** is a highly sensitive and specific biomarker for **myocardial injury**, making it the most reliable test for rapidly diagnosing acute coronary syndrome or re-infarction.
- Its elevation indicates ongoing **myocardial necrosis**, even after a recent MI, and is crucial for guiding immediate management.
*Creatine kinase MB*
- While CK-MB is used for diagnosing myocardial infarction, its levels can also be elevated in cases of **skeletal muscle injury** or **after cardiac procedures**, reducing its specificity in this context.
- CK-MB also has a **shorter window of elevation** compared to troponins, potentially missing later presentations of myocardial injury.
*Lactate dehydrogenase*
- **LDH** is a relatively **nonspecific marker** that can elevate due to various conditions affecting different organs (e.g., liver disease, hemolysis, renal injury).
- Its elevation onset is **slower** and its diagnostic window is longer, making it less suitable for rapid diagnosis of acute myocardial injury.
*Copeptin*
- **Copeptin** is a marker of **endogenous stress** and is often used in conjunction with troponins to rule out NSTEMI, especially at early presentation.
- However, it is not a direct marker of myocardial necrosis itself and is **not as specific** as troponin for diagnosing a re-infarction.
*Aspartate aminotransferase*
- **AST** is a **nonspecific enzyme** found in various tissues, including the liver, skeletal muscle, and heart.
- Elevated AST levels are frequently seen in **liver damage** and are not a primary biomarker for diagnosing acute myocardial infarction or re-infarction.
Perioperative cardiovascular management US Medical PG Question 5: A 41-year-old man presents to his primary care provider because of chest pain with activity for the past 6 months. Past medical history is significant for appendectomy at age 12 and hypertension, and diabetes mellitus type 2 that is poorly controlled. He takes metformin and lisinopril but admits that he is bad at remembering to take them everyday. His father had a heart attack at 41 and 2 stents were placed in his heart. His mother is healthy. He drinks alcohol occasionally and smokes a half of a pack of cigarettes a day. He is a sales executive and describes his work as stressful. Today, the blood pressure is 142/85 and the body mass index (BMI) is 28.5 kg/m2. A coronary angiogram shows > 75% narrowing of the left anterior descending coronary artery. Which of the following is most significant in this patient?
- A. Obesity
- B. Family history
- C. Hypertension
- D. Smoking
- E. Diabetes mellitus (Correct Answer)
Perioperative cardiovascular management Explanation: ***Diabetes mellitus***
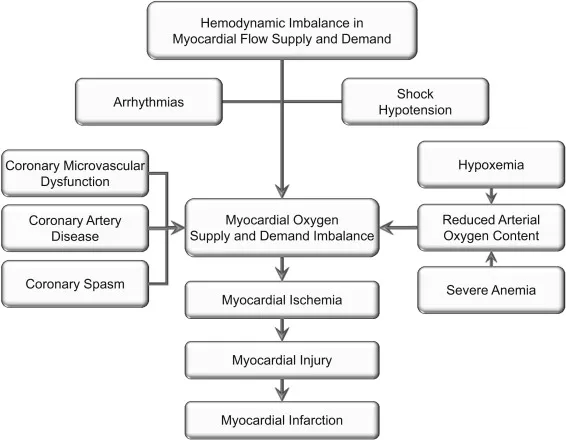
- **Diabetes mellitus** is a significant risk factor for **atherosclerosis** and contributes to accelerated progression of **coronary artery disease (CAD)**, often leading to more widespread and severe disease.
- Poorly controlled diabetes can cause **endothelial dysfunction**, increasing oxidative stress and inflammation, which are key processes in **plaque formation** and destabilization.
*Obesity*
- **Obesity** (BMI 28.5 kg/m2) is a risk factor for **CAD** but often acts through associated conditions like **hypertension**, **diabetes**, and **dyslipidemia**.
- While it contributes to overall cardiovascular risk, it is less directly pathogenic than diabetes which independently accelerates **atherosclerosis**.
*Family history*
- The patient's father had a **heart attack at 41**, which is a significant risk factor for **early-onset CAD**.
- However, the patient has multiple modifiable risk factors (smoking, hypertension, diabetes) that are independently and more directly contributing to his current presentation.
*Hypertension*
- **Hypertension** (142/85 mmHg) is a major modifiable risk factor that causes **endothelial damage** and promotes **atherosclerosis**.
- While important, the patient's **poorly controlled diabetes mellitus** often creates a more aggressive environment for plaque formation and progression compared to hypertension alone.
*Smoking*
- **Smoking** is a potent, modifiable risk factor that causes direct vascular injury, promotes **thrombogenesis**, and contributes to **atherosclerosis**.
- Although highly detrimental, smoking is one of several significant risk factors; **diabetes mellitus**, with its systemic metabolic impact, can be considered more broadly influential in the severity and diffuse nature of **CAD**.
Perioperative cardiovascular management US Medical PG Question 6: A 66-year-old female with hypertension and a recent history of acute ST-elevation myocardial infarction (STEMI) 6 days previous, treated with percutaneous transluminal angioplasty (PTA), presents with sudden onset chest pain, shortness of breath, diaphoresis, and syncope. Vitals are temperature 37°C (98.6°F), blood pressure 80/50 mm Hg, pulse 125/min, respirations 12/min, and oxygen saturation 92% on room air. On physical examination, the patient is pale and unresponsive. Cardiac exam reveals tachycardia and a pronounced holosystolic murmur loudest at the apex and radiates to the back. Lungs are clear to auscultation. Chest X-ray shows cardiomegaly with clear lung fields. ECG is significant for ST elevations in the precordial leads (V2-V4) and low-voltage QRS complexes. Emergency transthoracic echocardiography shows a left ventricular wall motion abnormality along with a significant pericardial effusion. The patient is intubated, and aggressive fluid resuscitation is initiated. What is the next best step in management?
- A. Immediate cardiac catheterization
- B. Immediate transfer to the operating room (Correct Answer)
- C. Emergency pericardiocentesis
- D. Intra-aortic balloon counterpulsation
- E. Administer dobutamine 5-10 mcg/kg/min IV
Perioperative cardiovascular management Explanation: ***Immediate transfer to the operating room***
- The patient's presentation with sudden onset chest pain, shortness of breath, profound cardiogenic shock, and a new **holosystolic murmur at the apex radiating to the back** in the context of a recent **STEMI**, strongly suggests **acute papillary muscle rupture** causing severe mitral regurgitation. This is a surgical emergency requiring immediate intervention.
- The holosystolic murmur at the apex is pathognomonic for acute mitral regurgitation, distinguishing this from ventricular free wall rupture (which would present with tamponade physiology without a murmur).
- The patient requires urgent surgical repair (mitral valve replacement or repair) to address this mechanical complication of **myocardial infarction (MI)**, which is causing severe hemodynamic compromise.
*Immediate cardiac catheterization*
- While cardiac catheterization is essential for diagnosing coronary artery disease and revascularization, in this emergent situation with profound shock and a mechanical complication (papillary muscle rupture), the primary issue is structural cardiac damage requiring surgical repair, not ongoing ischemia alone.
- Delaying surgical intervention for catheterization in this hemodynamically unstable patient would be detrimental and potentially fatal.
*Emergency pericardiocentesis*
- Although there is a **pericardial effusion** on echocardiography, the patient's presentation with a new holosystolic murmur and profound shock after STEMI indicates **papillary muscle rupture with acute mitral regurgitation**, not cardiac tamponade.
- The presence of a loud murmur excludes ventricular free wall rupture as the primary cause. The effusion is likely reactive or incidental.
- Pericardiocentesis would not address the underlying mitral valve pathology causing the hemodynamic collapse.
*Intra-aortic balloon counterpulsation*
- **Intra-aortic balloon pump (IABP)** can improve cardiac output and reduce afterload, which may provide temporary hemodynamic support in cardiogenic shock.
- However, in cases of **papillary muscle rupture** with severe acute mitral regurgitation, IABP provides only temporary support and does not fix the underlying structural problem.
- It could be considered as a bridge to surgery, but the definitive treatment is surgical repair, which should be expedited without delay.
*Administer dobutamine 5-10 mcg/kg/min IV*
- **Dobutamine** is an inotrope that increases cardiac contractility. While it might improve cardiac output in some forms of cardiogenic shock, in the setting of **acute severe mitral regurgitation from papillary muscle rupture**, it cannot resolve the structural valvular incompetence.
- Increasing contractility may paradoxically worsen the regurgitant fraction and further compromise forward cardiac output.
- Medical management alone cannot resolve this mechanical complication, necessitating urgent surgical intervention.
Perioperative cardiovascular management US Medical PG Question 7: A 69-year-old man is scheduled to undergo radical retropubic prostatectomy for prostate cancer in 2 weeks. He had a myocardial infarction at the age of 54 years. He has a history of GERD, unstable angina, hyperlipidemia, and severe osteoarthritis in the left hip. He is unable to climb up stairs or walk fast because of pain in his left hip. He had smoked one pack of cigarettes daily for 30 years but quit 25 years ago. He drinks one glass of wine daily. Current medications include aspirin, metoprolol, lisinopril, rosuvastatin, omeprazole, and ibuprofen as needed. His temperature is 36.4°C (97.5°F), pulse is 90/min, and blood pressure is 136/88 mm Hg. Physical examination shows no abnormalities. A 12-lead ECG shows Q waves and inverted T waves in leads II, III, and aVF. His B-type natriuretic protein is 84 pg/mL (N < 125). Which of the following is the most appropriate next step in management to assess this patient's perioperative cardiac risk?
- A. No further testing
- B. 24-hour ambulatory ECG monitoring
- C. Radionuclide myocardial perfusion imaging (Correct Answer)
- D. Treadmill stress test
- E. Resting echocardiography
Perioperative cardiovascular management Explanation: ***Radionuclide myocardial perfusion imaging***
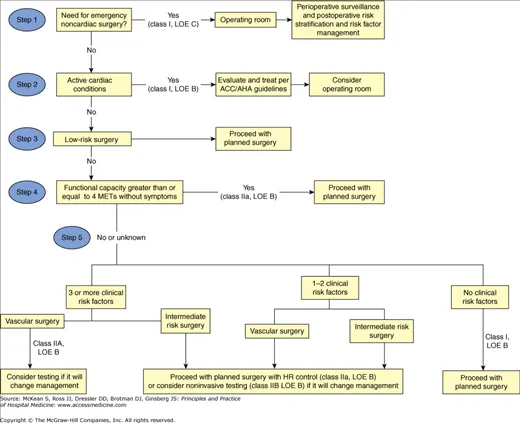
- This patient requires **perioperative cardiac risk assessment** before intermediate-risk surgery (radical prostatectomy).
- Key factors include: history of **myocardial infarction**, current cardiac risk factors, and **inability to exercise** due to severe osteoarthritis.
- Since he cannot perform exercise stress testing, **pharmacologic stress testing** with radionuclide myocardial perfusion imaging (using agents like adenosine, dipyridamole, or regadenoson) is the most appropriate test to assess for **inducible myocardial ischemia**.
- This provides functional assessment of coronary perfusion under pharmacologic stress, helping guide perioperative risk stratification and management.
- *Note: The presence of unstable angina would typically require cardiac stabilization first; this question focuses on selecting the appropriate stress test modality for a patient unable to exercise.*
*No further testing*
- This patient has significant cardiac risk factors including **prior MI**, ongoing cardiac medications, and ECG changes suggesting old infarction.
- Proceeding directly to surgery without functional cardiac assessment would be **inappropriate** given his risk profile and the intermediate-risk nature of the planned surgery.
*24-hour ambulatory ECG monitoring*
- Holter monitoring detects arrhythmias and silent ischemic episodes but does not provide **functional capacity assessment** or evaluation of inducible ischemia under stress conditions.
- It is not the primary tool for **perioperative cardiac risk stratification** before major surgery.
*Treadmill stress test*
- The patient's **severe osteoarthritis** prevents him from climbing stairs or walking fast, making him unable to achieve adequate exercise workload for a treadmill stress test.
- This functional limitation makes **exercise stress testing contraindicated**; pharmacologic stress testing is required instead.
*Resting echocardiography*
- Resting echocardiography assesses **baseline left ventricular function**, wall motion abnormalities from prior infarction, and valvular disease.
- While useful for structural assessment, it does **not evaluate for exercise-induced or stress-induced ischemia**, which is critical for perioperative risk assessment in patients with coronary artery disease.
- His normal BNP (84 pg/mL) suggests adequate baseline ventricular function, making functional ischemia assessment more relevant than structural evaluation alone.
Perioperative cardiovascular management US Medical PG Question 8: A 72-year-old female presents to the emergency department following a syncopal episode while walking down several flights of stairs. The patient has not seen a doctor in several years and does not take any medications. Your work-up demonstrates that she has symptoms of angina and congestive heart failure. Temperature is 36.8 degrees Celsius, blood pressure is 160/80 mmHg, heart rate is 81/min, and respiratory rate is 20/min. Physical examination is notable for a 3/6 crescendo-decrescendo systolic murmur present at the right upper sternal border with radiation to the carotid arteries. Random blood glucose is 205 mg/dL. Which of the following portends the worst prognosis in this patient?
- A. Hypertension
- B. Angina
- C. Diabetes
- D. Syncope
- E. Congestive heart failure (CHF) (Correct Answer)
Perioperative cardiovascular management Explanation: ***Congestive heart failure (CHF)***
- Once **congestive heart failure** symptoms develop in severe aortic stenosis, the prognosis is very poor, with an average survival of 1.5-2 years if untreated.
- This indicates significant myocardial dysfunction and increased risk of sudden cardiac death.
*Syncope*
- **Syncope** in aortic stenosis, while serious and indicating reduced cerebral perfusion, has a slightly better prognosis than CHF, with an average survival of 2-3 years untreated.
- It often reflects a critical reduction in cardiac output, but the heart muscle itself may still have some compensatory capacity.
*Angina*
- **Angina** is a common symptom of aortic stenosis, reflecting increased myocardial oxygen demand or reduced coronary perfusion.
- Untreated, patients with angina in aortic stenosis have an average survival of 3-5 years, which is better than syncope or CHF.
*Hypertension*
- While **hypertension** is a risk factor for aortic stenosis and can exacerbate symptoms, it is not a direct symptom of severe aortic stenosis itself but rather a co-morbidity.
- Its presence doesn't inherently portend a worse prognosis for aortic stenosis than the severe symptomatic manifestations like syncope or CHF.
*Diabetes*
- **Diabetes** is a systemic disease that can accelerate atherosclerosis and increase cardiovascular risk, but it is a chronic condition rather than an acute symptom of severe aortic stenosis.
- While it complicates management and overall prognosis, its impact is not as immediate or as severe as the development of CHF directly attributable to the aortic stenosis itself.
Perioperative cardiovascular management US Medical PG Question 9: A 71-year-old African American man diagnosed with high blood pressure presents to the outpatient clinic. In the clinic, his blood pressure is 161/88 mm Hg with a pulse of 88/min. He has had similar blood pressure measurements in the past, and you initiate captopril. He presents back shortly after initiation with extremely swollen lips, tongue, and face. After captopril is discontinued, what is the most appropriate step for the management of his high blood pressure?
- A. Initiate a beta-blocker
- B. Switch to ramipril
- C. Initiate a thiazide diuretic (Correct Answer)
- D. Reinitiate captopril
- E. Initiate an ARB
Perioperative cardiovascular management Explanation: ***Initiate a thiazide diuretic***
- The patient experienced **angioedema** after taking **captopril**, which is an **ACE inhibitor**. This is a life-threatening adverse effect, and it indicates that all **ACE inhibitors** should be avoided in the future.
- Due to the risk of angioedema, a different class of antihypertensive should be used. Given his African American ethnicity, a **thiazide diuretic** or **calcium channel blocker** would be an appropriate initial choice for monotherapy if hypertension is stage 1, or combination therapy if stage 2 hypertension, otherwise, a second agent, such as a **calcium channel blocker**, can be added.
*Initiate a beta-blocker*
- While beta-blockers are a class of antihypertensive drugs, they are generally not preferred as **first-line monotherapy** for **hypertension**, especially in older African American patients, unless there are specific comorbidities like heart failure or coronary artery disease.
- The most appropriate first-line choice after **ACE inhibitor-induced angioedema** would be a thiazide diuretic or calcium channel blocker, as per ACC/AHA guidelines for primary hypertension.
*Switch to ramipril*
- **Ramipril** is also an **ACE inhibitor**, and the patient experienced **angioedema** with **captopril** (another ACE inhibitor).
- Cross-reactivity and recurrence of angioedema are high with other ACE inhibitors, making this choice extremely dangerous and contraindicated.
*Reinitiate captopril*
- The patient developed **angioedema**, a severe and potentially fatal hypersensitivity reaction, to **captopril**.
- Reinitiating the same drug could lead to recurrent, and potentially more severe, angioedema and is therefore absolutely contraindicated.
*Initiate an ARB*
- **Angiotensin receptor blockers (ARBs)**, while a different class from ACE inhibitors, act on the renin-angiotensin system and carry a **small but significant risk of cross-reactivity** leading to angioedema, especially in patients who have experienced it with an ACE inhibitor.
- Given the life-threatening nature of angioedema, it is generally recommended to avoid ARBs if a patient has a history of ACE inhibitor-induced angioedema.
Perioperative cardiovascular management US Medical PG Question 10: A 55-year-old man with chronic pain on high-dose opioids (120 mg oral morphine equivalents daily) requires major spine surgery. Intraoperatively, he requires escalating doses of fentanyl with poor pain control. Postoperatively, his pain remains severe (10/10) despite maximum conventional multimodal analgesia including IV hydromorphone PCA, acetaminophen, and ketorolac. He becomes increasingly agitated and tachycardic. Evaluate the most comprehensive pain management strategy addressing the underlying pathophysiology.
- A. Increase PCA opioid dose to match home requirements plus surgical pain needs
- B. Transition to methadone for better mu-receptor coverage
- C. Ketamine infusion to address opioid-induced hyperalgesia and NMDA receptor sensitization (Correct Answer)
- D. Epidural analgesia with local anesthetic and low-dose opioid
- E. Regional nerve blocks with liposomal bupivacaine
Perioperative cardiovascular management Explanation: ***Ketamine infusion to address opioid-induced hyperalgesia and NMDA receptor sensitization***
- The patient exhibits **opioid-induced hyperalgesia (OIH)**, where high-dose opioids paradoxically increase pain sensitivity through **NMDA receptor** activation and central sensitization.
- **Ketamine** is an NMDA receptor antagonist that directly targets the underlying pathophysiology to reverse **central sensitization** and reduce the "wind-up" phenomenon.
*Increase PCA opioid dose to match home requirements plus surgical pain needs*
- Simply increasing the opioid dose in a patient with **OIH** can exacerbate the pain sensitization rather than alleviate it.
- This strategy fails to address the down-regulation of **mu-receptors** and the neuroplastic changes associated with chronic high-dose opioid use.
*Transition to methadone for better mu-receptor coverage*
- While **methadone** has NMDA antagonist properties, a rapid transition in the acute postoperative setting is pharmacokinetically complex and lacks the immediate efficacy of a **low-dose ketamine infusion**.
- Methadone titration is challenging due to its long **half-life** and risk of delayed respiratory depression in an agitated, acutely painful patient.
*Epidural analgesia with local anesthetic and low-dose opioid*
- While neuraxial techniques are normally effective, **major spine surgery** often complicates or precludes the placement of an epidural due to surgical site constraints or dural integrity.
- This approach may provide regional relief but does not systemically address the **centralized hyperalgesia** caused by chronic high-dose opioid therapy.
*Regional nerve blocks with liposomal bupivacaine*
- **Regional blocks** for extensive spine surgery may provide inadequate coverage for the broad dermatomal distribution involved in major spinal procedures.
- These blocks target **peripheral nerves** and do not address the **NMDA-mediated sensitization** in the central nervous system that is driving this patient's severe pain.
More Perioperative cardiovascular management US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.